Abstract
Myoepithelioma is a benign salivary gland tumor in the head and neck region, accounting for 1–1.5% of all glandular tumors. The diagnosis is rendered histopathologically, and it includes the proliferation of myoepithelial cells, without chondroid or myxochondroid stroma and ductal components (up to 5% of ductal component is acceptable). In our case report, this lesion has occurred in a 46-year-old female patient, and presented as well defined, nodular growth on the right posterior palatal region. Bony erosion and invasion were observed radiographically, and the lesion was excised surgically, with 1–2 cm of clear margin. The microscopic features included proliferating tumor sheets, composed of bland looking spindle and plasmacytoid shaped myoepithelial cells, and few cells showed clear cytoplasm, which were confirmed immunohistochemically as myoepithelial cells. Thus, the final diagnosis of benign myoepithelioma was rendered and no recurrence had been reported so far in the regular follow-up.
KEY WORDS: Benign salivary gland lesion, myoepithelial cells, myoepithelioma
Myoepithelioma is a benign tumor of the oral cavity, arising predominantly from major and minor salivary glands, and accounting for 1–1.5% of all glandular tumors.[1] Benign myoepitheliomas are mainly composed of myoepithelial cells, which are ectodermally derived cells located between the basal surface of acinar units, basement membrane, and surrounding intercalated duct. Other than salivary glands, these myoepithelial cells are also found in many exocrine tissues including lacrimal glands, breast, prostate, and sweat glands.[1,2,3,4]
Sheldon in 1943 coined the term “myoepithelioma” to describe a group of tumors, histologically composed of solitary myoepithelial cells.[5,6] In the World Health Organization (WHO) classification, benign myoepitheliomas have been defined as “neoplasms without chondroid or myxochondroid stroma” and they may exhibit various growth patterns based on the arrangement of myoepithelial cells. It may vary from solid, reticular pattern of arrangement or some combination of these with different histological appearances of myoepithelial cells (spindle, plasmacytoid in appearance).[7] Malignant myoepithelioma have myoepithelial cells with prominent cellular pleomorphism and atypia.[8]
Clinically, it presents as a painless mass with a peak age of occurrence being in the third to fifth decade. Most frequent sites of involvement are parotid glands and minor salivary glands of the hard palate. The prognosis is excellent and recurrence is rare after complete excision.[1] To our concern, biologic behavior of myoepithelioma is that metastasis may develop in these benign looking lesions.[1] Here, we present a rare case of myoepithelioma of the hard palate causing bony erosion, and we have discussed about the diagnosis and treatment of this lesion with concerned literature reviews.
Case Report
A 46-year-old female patient reported to our hospital and presented with a history of painless mass which had grown over a period of 6 months to the present size of 2 cm × 3 cm. She complained of mild obstruction of nose and thereby changes in her voice. On clinical examination, she had a well circumscribed sessile growth with irregular nodular surface arising from the posterior part of right maxilla [Figure 1]. The lesion extended anteriorly from the mesial aspect of right maxillary premolar region up to the junction of hard and soft palate posteriorly. Medially, the lesion was crossing the midline toward left side by around 2 mm and laterally it had involved the right maxillary alveolar ridge. The lesion was firm in consistency and the color was similar to that of surrounding normal mucosa. No secondary changes like ulceration were seen and no lymph nodes were palpable. On computerized topography examination, there was a well-circumscribed mass causing bony erosion and invasion of hard palate [Figure 2]. Based on these clinical and imaging features, it was provisionally diagnosed as malignant salivary gland tumor, most commonly mucoepidermoid carcinoma, and planned for right subtotal maxillectomy to avoid recurrence in future. The resected mass was well circumscribed and measuring about 2.5 cm × 1.5 cm [Figure 3]. The mucosal cut margin clearance was 1–2 cm, and the depth of clearance was 2.5 cm.
Figure 1.

Intraoral photograph revealing the tumor mass
Figure 2.
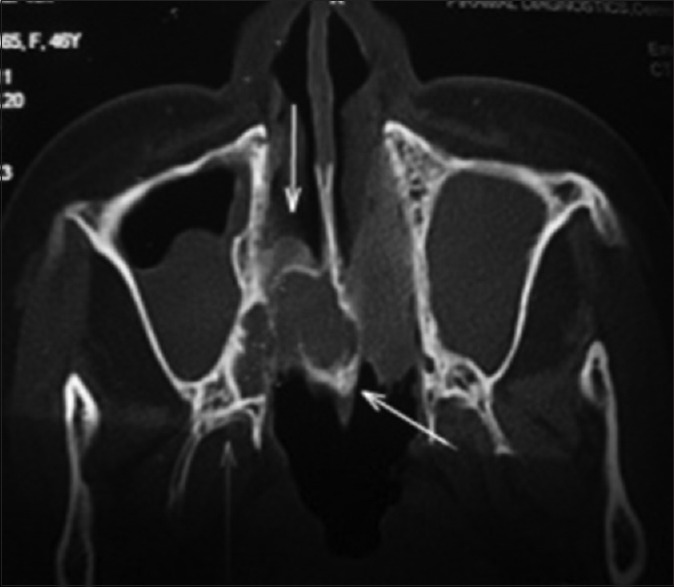
Computerized topography - coronal view showing tumor extension and bony erosion
Figure 3.

Surgical specimen, after resection
On histopathological examination, the multiple sections studied from the hematoxylin and eosin stained slides showed a well-circumscribed tumor mass composed of myoepithelial cells arranged in large lobules, sheets, and large nests. The cells are spindle and plasmacytoid shaped with a moderate amount of clear to pale eosinophilic cytoplasm. Nuclei were round to ovoid in shape and appeared relatively bland [Figure 4]. No ductal structures were evident and cellularity was more with minimal atypia, and without significant pleomorphism. Stromal hyalinization was noted and the overlying mucosa was intact and nonneoplastic. No mucous or intermediate cells were seen, ruling out the possibility of provisional radiological diagnosis, mucoepidermoid carcinoma. Thus, the final histological diagnosis based on these features was benign myoepithelioma.
Figure 4.
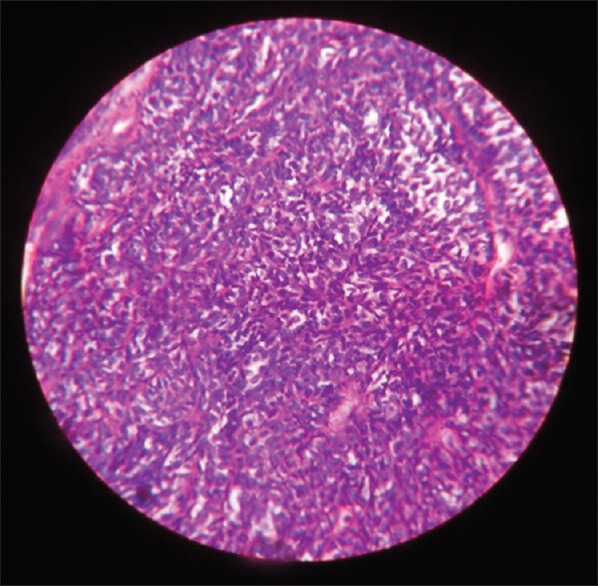
Histopathological picture showing myoepithelial cells with few cells showing clear cytoplasm
Since bony erosion and invasion are uncommon in benign lesions and for academic purpose, immunohistochemistry (IHC) was performed, which revealed a strong and diffuse positive reaction to S100 protein and smooth muscle actin. These IHC findings confirmed that the tumor cells were myoepithelial cells, consistent with the histopathological diagnosis of “benign myoepithelioma” of salivary gland origin.
After the surgery, the patient had been under regular follow-up and no recurrence was observed in this 2 years period of follow-up. The surgical site also revealed the coincidental presence of nasal polyp in the patient during microscopic examination.
Discussion
Myoepitheliomas account for <1.5% of all salivary gland tumors. The most common location of myoepithelioma in the head and neck region are parotid gland (40%) and the palate (2%).[1,9] Myoepithelioma usually presents as asymptomatic, slowly growing masses and is diagnosed histopathologically, rather than clinically. Grossly they may have a solid, white or yellow glistening cut surface. Myoepithelioma of minor salivary glands will not demonstrate capsule whereas those of parotid are usually encapsulated. Microscopically they show four histopathologic subtypes, including plasmacytoid, epitheliod, spindle and clear cells which can be associated with mucoid (or) hyalinized stroma. However, hisopathological subtype has not seemed to influence the clinical or biological behavior of these tumors. The most common subtype has been the spindle cell variant, observed usually in the parotid lesions, whereas plasmacytoid type is commonly seen in the palate. Although some pathologist will not accept any ductal elements in benign myoepitheliomas, others permit upto 1 duct per medium power field or <5% of ducts in the whole section.[10] Till date, more than 200 cases of benign myoepitheliomas have been reported in the English literature.
According to WHO classification of salivary gland tumors, “myoepitheliomas are characterized by a more aggressive growth pattern than pleomorphic adenoma,” but benign myoepithelioma should be carefully differentiated from malignant tissues, such as malignant myoepithelioma, mucoepidermoid carcinoma, and spindle cell squamous carcinoma. Because of varied histopathological features, differential diagnosis will also extend to include adenocarcinoma, basal cell adenoma, leiomyoma, and adenoid cystic carcinoma. However, with the bland cytomorphologic features of tumor cells, and IHC a diagnosis of benign myoepithelioma can be effectively rendered.[3,11]
Curative treatment for the lesion includes excision with 0.5 cm negative margin. Extension into the adjacent bone is rare and can be treated similarly with resection including 0.5 cm of clear margin from the lesion. Although recurrence has been reported rarely, patients will require regular long-term follow-up.
Conclusion
Myoepithelioma in our case report had occurred as a well-defined palatal lesion, showing nodular surface and radiographically, it mimicked malignant salivary gland lesion by causing bony erosion. On histopathological investigation, the solid pattern of bland appearing myoepithelial cells with epithelioid and clear cell component were noted and immunohistochemically, these tumor cells stained positive for myoepithelial cells, confirming the diagnosis of benign myoepithelioma.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
References
- 1.Barnes L, Appel BN, Perez H, El-Attar AM. Myoepithelioma of the head and neck: Case report and review. J Surg Oncol. 1985;28:21–8. doi: 10.1002/jso.2930280107. [DOI] [PubMed] [Google Scholar]
- 2.Kawashima Y, Kobayashi D, Ishikawa N, Kishimoto S. A case of myoepithelioma arising in an accessory parotid gland. J Laryngol Otol. 2002;116:474–6. doi: 10.1258/0022215021911112. [DOI] [PubMed] [Google Scholar]
- 3.Sciubba JJ, Brannon RB. Myoepithelioma of salivary glands: Report of 23 cases. Cancer. 1982;49:562–72. doi: 10.1002/1097-0142(19820201)49:3<562::aid-cncr2820490328>3.0.co;2-6. [DOI] [PubMed] [Google Scholar]
- 4.Morinière S, Robier A, Machet MC, Beutter P, Lescanne E. Massive infra-clinic invasion of the facial nerve by a myoepithelial carcinoma of the parotid. Int J Pediatr Otorhinolaryngol. 2003;67:663–7. doi: 10.1016/s0165-5876(03)00062-4. [DOI] [PubMed] [Google Scholar]
- 5.Sheldon WH. So-called mixed tumors of the salivary glands. Arch Pathol. 1943;35:1–20. [Google Scholar]
- 6.Kanazawa H, Furuya T, Watanabe T, Kato J. Plasmacytoid myoepithelioma of the palate. J Oral Maxillofac Surg. 1999;57:857–60. doi: 10.1016/s0278-2391(99)90830-3. [DOI] [PubMed] [Google Scholar]
- 7.Bolzoni A, Pianta L, Farina D, Nicolai P. Benign myoepithelioma of the lacrimal gland: Report of a case. Eur Arch Otorhinolaryngol. 2005;262:186–8. doi: 10.1007/s00405-004-0787-z. [DOI] [PubMed] [Google Scholar]
- 8.Di Palma S, Guzzo M. Malignant myoepithelioma of salivary glands: Clinicopathological features of ten cases. Virchows Arch A Pathol Anat Histopathol. 1993;423:389–96. doi: 10.1007/BF01607152. [DOI] [PubMed] [Google Scholar]
- 9.Waldron CA. Ellis GL, Auclair PL, Gnepp DR. Surgical Pathology of the Salivary Glands. Philadelphia: WB Saunders; 1991. Mixed tumor (pleomorphic adenoma) and myoepithelioma; pp. 165–86. [Google Scholar]
- 10.Gnepp DR, Brandwein MS, Henley JD. Gnepp DR. Diagnostic Surgical Pathology of the Head and Neck. 2nd ed. Philadelphia, PA: Saunders; 2009. Salivary and lacrimal glands; pp. 449–53. [Google Scholar]
- 11.Dardick I, Thomas MJ, van Nostrand AW. Myoepithelioma - New concepts of histology and classification: A light and electron microscopic study. Ultrastruct Pathol. 1989;13:187–224. doi: 10.3109/01913128909057442. [DOI] [PubMed] [Google Scholar]


