Abstract
Excessive gingival pigmentation is a major esthetic concern for many people. Melanin pigmentation is known to be caused by melanin granules within the gingival epithelium. Smile is determined not only by the shape, the position, and the color of the teeth, but also by the gingival tissues. Gingival health and appearance are essential components of an attractive smile. It is not a medical problem, but it feels unesthetic for the patient and particularly in patients having a very high lip/smile line. Depigmentation is not a clinical indication but a treatment of choice where esthetics is a concern and is desired by the patient. For depigmentation of gingival, different treatment modalities have been reported such as bur abrasion, scraping, partial thickness flap, cryotherapy, electrosurgery, and laser. The present case series describes two simple and effective surgical depigmentation techniques treated with diode laser and electrosurgery.
KEY WORDS: Depigmentation, electrocautery, laser, melanin pigmentation
The harmony of the smile is determined not only by the shape, color, and position of the teeth but also by the gingival tissues.[1] Healthy gingival and its appearance are essential factors for an attractive smile and removal of hyperpigmented gingiva is the necessity for a better and beautiful smile.[2] The pigmentation becomes an esthetic concern in patients with a high smile line. The color of the gingiva, which is the part of many epidemiological evaluations of gingival health ranges from pale pink to deep red or violet. Oral melanin pigmentation is considered to be multifactorial, which can be physiological or pathological and can be caused by a variety of local and/or systemic factors such as tobacco use, genetic, prolonged administration of certain drugs especially antimalarial agents, and tricyclic antidepressants.[3]
The first and foremost indication for depigmentation is the patient demand for improved esthetics. There is no racial or gender predilection for oral pigmentation. The distribution and intensity of racial pigmentation of the oral mucosa varies, not only among races but also between different individuals of the same race and within different areas of the same mouth. The selection of the technique should be based on clinical experience and individuals preferences, which give better results.[4]
Various methods such as gingivectomy with free gingival autografts and acellular dermal matrix allografts, electrosurgery, cryosurgery, abrasion with diamond bur, and laser therapy have been used in the treatment of gingival melanin depigmentation with varied degrees of success.[5]
The cases were selected based on Dummett-Gupta oral pigmentation index (DOPI): (Dummett 1971).[1]
No clinical pigmentation (pink gingiva)
Mild clinical pigmentation (mild light brown color)
Moderate clinical pigmentation (medium brown or mixed pink and brown).
Heavy clinical pigmentation (deep brown or bluish black).
The present case series describes two different techniques for depigmentation in split-mouth design and to compare the clinical outcomes of electrosurgery (left) and laser therapy (right).
Case Reports
Case 1
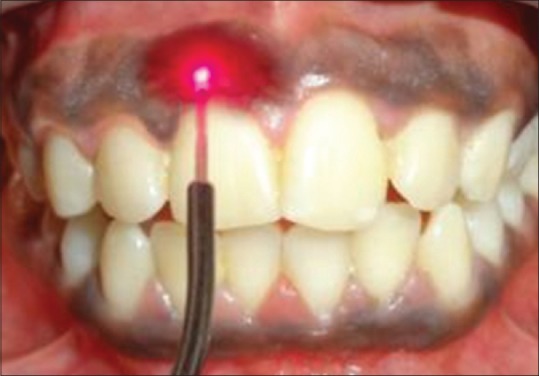
A 24-year-old male patient complaining of heavily pigmented gums visited Department of Periodontics, J.K.K. Nattraja Dental College and Hospital, Komarapalayam. The medical history was non-contributory. Intraoral examination revealed deeply pigmented gingiva with DOPI score of 3, and it was healthy and free of any inflammation. On intraoral examination, his DOPI score was 3 [Figure 1]. The patient had a very high smile line according to Liebart et al. smile line classification.[1] Considering the patients esthetic concern different treatment options were explained and on left side electrocautery [Figure 2] and on right side laser therapy [Figure 3] was planned. Blood investigation was carried out to rule out any contraindication for surgery. To the patient, oral hygiene procedures were performed, and oral hygiene instructions were given. Under topical anesthetic spray, local anesthesia was infiltrated in the maxillary anterior region in a left quadrant from the central incisor to canine. A loop electrode was used for depigmentation of gingiva [Figure 4]. It was used in light brushing strokes. The tip was kept in motion all the time to avoid heat buildup on the tissues and destruction of the tissues. Melanin pigments have been removed completely in the upper left quadrant [Figure 5]. Finally, coe-pak was placed over the surgical area, and oral hygiene instructions and medications were given. The pack was removed after 1-week and the area debrided with saline. 3 months postoperative examination showed well-epithelialized gingiva, which was pink, healthy, and pleasant [Figure 6]. After 1-week, in the maxillary right quadrant from the central incisor to canine, laser therapy was planned. Under topical anesthetic spray, in contact mode diode laser was used [Figure 7]. At 0.8 W in contact mode, the procedure was performed in cervico-apical direction on all pigmented areas. That is, from the central incisor to canine in the first quadrant. During and after laser therapy, there was no pain or bleeding at the surgical site [Figure 8]. Complete healing was seen in 1-week postoperatively. A total of 3 months after laser therapy, the appearance of gingiva was healthy and pink in color.
Figure 1.

Preoperative view showing pigmentation of upper labial gingival [case 1]
Figure 2.

Operative view using electrocautery (left) [case 2]
Figure 3.
Operative view using laser (right) [case 2]
Figure 4.

Operative view using electrocautery (left) [case 1]
Figure 5.

Immediate view after electrotherapy (left) [case 1]
Figure 6.

Operative view using diode laser (right) [case 1]
Figure 7.

Immediate view after laser therapy (right) [case 1]
Figure 8.

Three months postoperative view using laser and electrocautery [case 1]
Case 2
A 20-year-old female patient visited the Department of Periodontics, J.K.K. Nattraja Dental College and Hospital with the chief complaint of deeply and darkly pigmented gums. The medical history was non-contributory. The DOPI score was 3, which also revealed high smile line [Figure 9]. Considering the patients esthetic concern, different treatment options were explained and on left side electrocautery and on right side laser therapy were planned. However, the same procedure as like case 1 was carried out [Figures 10 and 11]. A total of 3 months postoperatively, in both the techniques appearance of gingiva was pink in color and healthy [Figure 12] when compared with cautery fewer pigmented areas can be seen.
Figure 9.

Preoperative view showing melanin pigments of upper labial gingiva [case 2]
Figure 10.

Immediate view after laser therapy (right) [case 2]
Figure 11.

Immediate view after electrocautery (left) [case 2]
Figure 12.

Three months postoperative view showed well-epithelialized gingiva, which is pink and healthy [case 2]
Discussion
Gingival pigmentation appears in the gingiva as early as 3 h after birth, and it is known to be the evidence of pigmentation.[6]
Hyperpigmented gingiva often leads many at times and forces the patient to seek esthetic treatment. Many treatment modalities like simple scalpel technique to advanced lasers have been addressed in the literature. According to Dummett, 1960 the degree of pigmentation relates with the mechanical, chemical, and physical stimuli. The selection of a technique for depigmentation is based on clinician's experience, patient's affordability, and preferences.[7]
Scalpel depigmentation is simple, effective, and economical of all the other techniques. Advantages which include wound healing are faster. Demerits of scalpel technique are excessive bleeding in the operating area, postoperative pain, and discomfort.[7] To overcome these difficulties, electrocautery procedure has been employed in the field of dentistry.
Another technique for depigmentation, which is advanced than scalpel is electrocautery. Electrocautery is effective when compared to the scalpel, and it has been explained through exploding cell theory in the year 1975 by Oringer.[8]
Electrosurgery has a strong influence in the retarding migration of melanin cells from locally situated cells. Electrocautery application for prolonged time leads to accumulation of heat to the tissues with tissue destruction. However, in the present case series no recurrence of pigmentation was seen between electrosurgical technique and laser therapy at 3 months postoperatively. According to Ciçek and Ertas, 2003, electrosurgery has many advantages such as the absence of bleeding and patient discomfort.[4] The prolonged use of cautery induces heat accumulation and tissue destruction and so to overcome the disadvantages of electrocautery, soft tissue lasers have been used in dentistry.
Another recent technique employed in this present case series is by laser therapy.[9] Maiman invented the first laser device in 1960, based on theories derived by Einstein in the early 1900s. The use of lasers for periodontal treatment is beneficial because the periodontium consists of both hard and soft tissues. Lasers have been approved for soft tissue management in periodontium because of their excellent and effective soft tissue ablation and hemostatic features.[6] Advantages of laser therapy include minimal wound contraction, bactericidal effect, greater hemostasis, bloodless field during surgery, and minimum damage to the periosteum and underlying bone. Moreover, dressing is not required for the treated gingiva and mucosa.[10] However, in this case report, due to patient's convenience coe-pak has been given.
In the present case series, two techniques were selected for depigmentation, which included electrosurgery and laser therapy. Following surgical procedure, patients were recalled at 1-week and 3 months postoperatively to evaluate the recurrence of melanin pigments. Wound healing was evaluated as per the list of clinical observations and patient responses prepared by Tal et al.[11]
In both the split-mouth case series, patient treated with laser showed complete healing within the 1-week period and also patient had better compliance, less pain, and no signs of bleeding.
All the techniques showed successful results with good patient satisfaction, and there is no recurrence at 3 months period. However, the laser is more advanced, and it is more effective when compared with electrocautery and patient also satisfied more with laser therapy because of convenience.
Conclusion
Electrocautery and laser therapy showed desirable results with better patient satisfaction, and there was no recurrence 3 months postoperatively. These two techniques have the advantage of the bloodless field during surgery, and technical expertise is required. Both the techniques did not show any postoperative complications. Laser therapy is of high cost, which also needs to be taken into consideration. However, the recurrence was less 3 months postoperatively when compared with electrocautery.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
References
- 1.Liebart ME, Deruelle CF, Santini A, Dillier FL, Corti VM. Smile line and periodontium visibility. Perio. 2004;1:17–25. [Google Scholar]
- 2.Doshi Y, Khandge N, Byakod G, Patil P. Management of gingival pigmentation with diodelaser: Is it a predictive tool? Int J Laser Dent. 2012;2:29–32. [Google Scholar]
- 3.Deepak P, Sunil S, Mishra R, Sheshadri P. Treatment of gingival pigmentation: A case series. Indian J Dent Res. 2005;16:171–6. doi: 10.4103/0970-9290.29901. [DOI] [PubMed] [Google Scholar]
- 4.Ciçek Y, Ertas U. The normal and pathological pigmentation of oral mucous membrane: A review. J Contemp Dent Pract. 2003;4:76–86. [PubMed] [Google Scholar]
- 5.Roshna T, Nandakumar K. Anterior esthetic gingival depigmentation and crown lengthening: Report of a case. J Contemp Dent Pract. 2005;6:139–47. [PubMed] [Google Scholar]
- 6.Cohen RE, Ammons WF. Lasers in periodontics. Report of Research, Science and Therapy Committee, American Academy of Periodontology. J Periodontol. 2002;73:1231. [Google Scholar]
- 7.Kaushik N, Srivastava N, Kaushik M, Gaurav V. Efficacy of different techniques of gingival depigmentation: A comparative evaluation with a case report. Int J Laser Dent. 2013;3:68–72. [Google Scholar]
- 8.Oringer MJ, editor . Electrosurgery in Dentistry. 2nd ed. Philadelphia: W.B. Saunders Co; 1975. [Google Scholar]
- 9.Ishikawa I, Aoki A, Takasaki AA. Potential applications of Erbium: YAG laser in periodontics. J Periodontal Res. 2004;39:275–85. doi: 10.1111/j.1600-0765.2004.00738.x. [DOI] [PubMed] [Google Scholar]
- 10.Atsawasuwan P, Greethong K, Nimmanon V. Treatment of gingival hyperpigmentation for esthetic purposes by Nd: YAG laser: Report of 4 cases. J Periodontol. 2000;71:315–21. doi: 10.1902/jop.2000.71.2.315. [DOI] [PubMed] [Google Scholar]
- 11.Tal H, Oegiesser D, Tal M. Gingival depigmentation by Erbium: YAG laser: Clinical observations and patient responses. J Periodontol. 2003;74:1660–7. doi: 10.1902/jop.2003.74.11.1660. [DOI] [PubMed] [Google Scholar]


