Abstract
Reconstructing predictable and esthetic papilla is the most complex and challenging aspect of implant dentistry. To obtain an esthetic and predictable gingival architecture and implant restoration, interdental papilla plays an important role. The main objective of the surgeon during the second stage of implant treatment should be the creation of interdental papilla prior to prosthetic restoration. The aim of this case report was to demonstrate a novel window technique for developing predictable and esthetic papilla around dental implants, which was followed for 2 years with excellent esthetic results.
KEY WORDS: Incisions, interdental papilla, second stage surgery, soft tissue esthetics
Dental implants have become a day-to-day procedure in the dental office. Restoration of missing teeth alone should not be considered as a success of an implant procedure. Restoration of lost gingival tissues and to create gingiva similar to that in a natural dentition should be considered as ultimate success of an implant by the treating surgeon.
To obtain an esthetic and predictable gingival architecture and implant restoration, interdental papilla plays an important role. The main objective of the surgeon during the second stage of implant treatment should be the creation of interdental papilla prior to prosthetic restoration.
In the classical Branemark system,[1] two stages of surgical procedure are followed, wherein the implant fixture is exposed in the second stage surgical procedure. During 2nd stage, the simplest method that is followed widely is the conventional mid-crestal incision method, which is not capable of generating papilla. To overcome this method, several techniques have been proposed.
It was Professor Palacci[2] of France who advocated different incision procedures for single and multiple teeth restorations. Following his reports several incision designs have been advocated and proposed by various researchers. Various incisions and procedures such as U – design, I – design, horizontal design, using template design, and soft tissue autografts have been reported in the regeneration of interdental papilla around dental implants.
The aim of this case report was to demonstrate a novel window technique for developing predictable and esthetic papilla around dental implants, which was followed for 2 years with excellent esthetic results.
Window Technique
Crestal incision placed about 1.5 mm palatal to the greatest bony height with an angulation of 45° with no. 15 bard parker blade [Figure 1]
A vertical releasing incision placed mesially and distally to the crestal incision without disturbing the adjacent teeth papilla and extending about 3 mm labially [Figure 2]
Soft tissue reflected to expose the cover screw [Figure 3]
Palatal extension of the incision followed closer to the adjacent teeth on both sides, and a release incision made around the palatal portion of the exposed cover screw [Figure 4]
Then healing abutment is placed after thoroughly cleaning the soft tissue around internal hex of the implant [Figure 5]
Soft tissue approximated with 4’0 suture material (vicryl)
Sutures removal has to be done after 10 days
After 2 weeks, second stage prosthetic procedure should be carried out.
Figure 1.
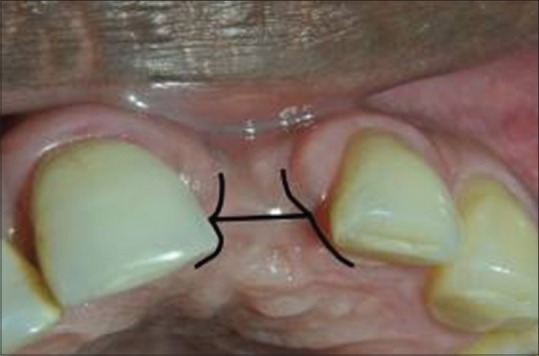
Window incision
Figure 2.

Flap reflection
Figure 3.
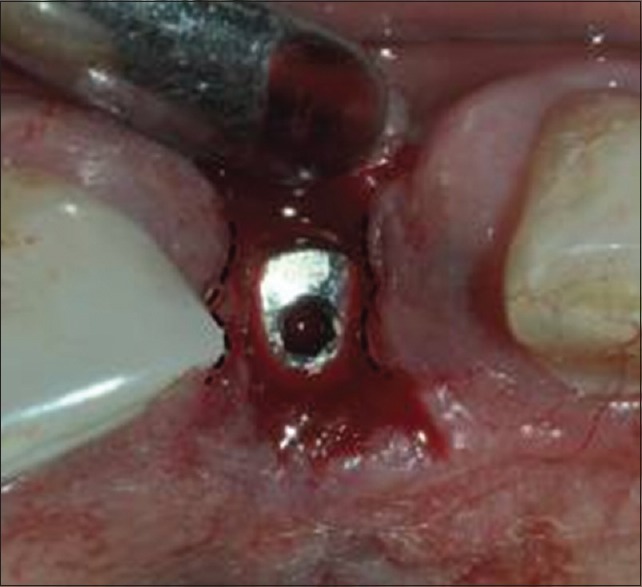
Incision and flap outlined (after reflection)
Figure 4.

Flap reflected
Figure 5.

Flap approximated
Discussion
Interdental papilla is seen in the space between two adjacent teeth. It acts as a biological barrier in the protection of periodontium. More importantly it plays an important and crucial role in an esthetic component of a natural dentition. Hence, it is very vital to maintain the integrity of the papilla during second stage implant surgery. Numerous techniques have been advocated in the regeneration of interdental papilla around implants.
Several methods with unique incisions and suturing designs have been proposed to regenerate interdental papilla around implants. Palacci[3] suggested that a full thickness flap be raised from the buccal and palatal side of the implant on the ridge and rotated 90° to accommodate the interproximal space of the implant. Adriaenssens et al.[4] introduced the “palatal sliding strip flap” to form papilla between implants and natural dentition in the anterior maxilla.
Nemcovsky et al.[5] suggested an U- shaped incision, with opening toward the buccal aspect of the implant site with divergent incisions. Tinti and Benfenati[6] reported a ramp mattress suture design, which pulled the buccal flap coronally, to obtain a papilla between two implants. Misch et al.[7] suggested a split finger surgical method in which three interlacing finger like incisions were made and each of the fingers was sutured over the desired interdental papillary position. Salama et al.[8] proposed a method for papilla regeneration wherein the healing abutment is buried beneath the gingival flap to produce a dead space with expectation of the space being filled by the soft tissue.
Even though these procedures provided papillary height, the results were not predictable. Various factors were involved in the success of any papilla regeneration procedures, such as preservation of blood supply, prevention of scar formation, and more importantly ideal placement of the implant into the bone. This new and innovative surgical technique provided significantly excellent results compared to the conventional mid-crestal technique [Figures 6 and 7].
Figure 6.

Labial view
Figure 7.

Occlusal view
In this case report, in order to overcome the limitations of above-mentioned techniques a novel window technique was followed to regenerate papilla around implants during second stage surgery prior to prosthetic restoration. Unlike most other procedures mentioned above, this technique avoided the labial papilla on the adjacent teeth and involved wholly the palatal papilla, which is considered to be the key element in the success of this technique. Moreover, there is no cross incisions on to the papilla, which may lead to, disturbed wound healing and scar formation. Above all avoiding more invasive surgery is considered one of the best methods of soft tissue regeneration, which is being incorporated in this technique.
The major advantages of this technique, when compared with earlier ones, are minimal invasive incision, less postoperative discomfort, and excellent esthetic and emergence profile obtained. The aim of any soft tissue procedure should be to obtain a resilient and scar less soft tissue. This can be obtained with atraumatic tissue handling, minimal tension during approximation, adequate vascularity, adequate hydration, and expedient surgical procedures that do not compromise blood supply. This case report shows the excellent results following the above requisites to obtain esthetic soft tissue profile.
The results obtained with this technique using the mentioned technique, were phenomenal. The patients were followed for 2 years at regular intervals and still the esthetic results obtained during the surgery and after 2 years were the same [Figure 8]. With above considerations with respect to follow-up and esthetic component, this technique provided the required and desired results.
Figure 8.

Final esthetic result after 2 years
Conclusion
In order to obtain esthetic papillary height and tissue integrity around implants proper and meticulous implant positioning is needed. This case report demonstrates a novel window technique with excellent and predictable results. Being a long term follow-up report this technique can be considered as a simple, minimal invasive procedure, which can be followed during 2nd stage surgery.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
References
- 1.Brånemark PI, Worthington P. Advanced Osseointegration Surgery: Applications in the Maxillofacial Region. Chicago: Quintessence; 1992. pp. 211–32. [Google Scholar]
- 2.Palacci P. Chicago: Quintessence; 1995. Optimal Implant Positioning and Soft Tissue Management for the Brånemark System; pp. 35–9. [Google Scholar]
- 3.Palacci P. Palacci P, Ericsson I, Engstrand P, Rangert B. Optimal Implant Positioning and Soft Tissue Management for Branemark system. Chicago: Quintessence Pub. Co; 1995. Papailla regeneration technique; pp. 59–70. [Google Scholar]
- 4.Adriaenssens P, Hermans M, Ingber A, Prestipino V, Daelemans P, Malevez C. Palatal sliding strip flap: Soft tissue management to restore maxillary anterior esthetics at stage 2 surgery: A clinical report. Int J Oral Maxillofac Implants. 1999;14:30–6. [PubMed] [Google Scholar]
- 5.Nemcovsky CE, Moses O, Artzi Z. Interproximal papillae reconstruction in maxillary implants. J Periodontol. 2000;71:308–14. doi: 10.1902/jop.2000.71.2.308. [DOI] [PubMed] [Google Scholar]
- 6.Tinti C, Benfenati SP. The ramp mattress suture: A new suturing technique combined with a surgical procedure to obtain papillae between implants in the buccal area. Int J Periodontics Restorative Dent. 2002;22:63–9. [PubMed] [Google Scholar]
- 7.Misch CE, Al-Shammari KF, Wang HL. Creation of interimplant papillae through a split-finger technique. Implant Dent. 2004;13:20–7. doi: 10.1097/01.id.0000116368.76369.78. [DOI] [PubMed] [Google Scholar]
- 8.Salama H, Salama M, Garber D, Adar P. Developing optimal peri-implant papillae within the esthetic zone: Guided soft tissue augmentation. J Esthet Dent. 1995;7:125–9. doi: 10.1111/j.1708-8240.1995.tb00729.x. [DOI] [PubMed] [Google Scholar]


