Abstract
Objective
To estimate the numbers and proportions of cancers occurring in Australia in 2010 attributable to modifiable causal factors.
Methods
We estimated the population attributable fraction (PAF) of cancers associated with exposure to 13 causal factors using standard formulae incorporating exposure prevalence and relative risk data. We also calculated the potential impact of changing exposure to some factors.
Results
A total of 32% of all cancers diagnosed in Australia in 2010 (excluding keratinocyte cancers) were attributable to the 13 factors assessed (men 33%; women 31%). Leading factors were tobacco smoke (PAF all cancers: 13.4%), solar radiation (6.2%), inadequate diet (6.1%) and overweight/obesity (3.4%). Factors conferring highest PAFs differed by sex: highest PAFs for men were tobacco smoke (15.8%), solar radiation (7.1%) and alcohol (3.0%); while highest PAFs for women were tobacco smoke (10.1%), solar radiation (5.0%) and overweight/obesity (4.5%). Sites with the highest counts of potentially preventable cancers were lung (8,569), colorectal (7,404), melanoma of the skin (7,220) and breast (3,233).
Conclusions
At least one in three cancers in Australia is attributable to exposure to known modifiable factors.
Implications
Up to 37,000 cancers could be prevented in Australia each year if the population avoided exposure to 13 common factors known or strongly suspected to cause cancer.
Keywords: population attributable fraction, cancer, risk factor, potential impact fraction, prevented fraction
In Australia in 2010, 116,850 people were diagnosed with invasive cancers, not including keratinocyte cancers (basal cell carcinomas (BCC) or squamous cell carcinomas (SCC) of the skin).1 Epidemiologic and experimental evidence accrued over the past five decades has established that many factors to which humans are commonly exposed are causes of cancer. Because exposure to such factors is potentially modifiable, it is important to quantify the proportion of cancers that might be averted if exposure to those factors were removed entirely or reduced to the minimum compatible with optimum health.
We estimated the fraction and numbers of cancers occurring in the Australian population that were attributable to established causal factors that are, at least in theory, able to be modified.2 Using estimates of the prevalence of each exposure in the Australian population and estimates of the relative risk of cancer associated with different levels of exposure, we applied standard formulae to calculate the population attributable fraction (PAF) for cancers associated with exposure to each of 13 factors determined to cause cancer by independent, international cancer agencies (Table 1). The magnitudes of PAF estimates depend heavily on the definition of exposure; Table 1 lists the reference category for each factor that was used to estimate the PAF. For some factors (e.g. tobacco smoking, alcohol, infections), the reference category represents no exposure. Other factors are ubiquitous (e.g. body mass index, dietary factors, sunlight) and so the reference levels for those factors were widely accepted thresholds for optimum health.
Table 1.
Factors declared as modifiable carcinogens: reference levels of exposure for calculating population attributable fractions (PAF) of cancer
| Factor | Reference levela |
|---|---|
| Alcohol consumption | None |
| Breast feeding for 12 months or less among parous women | >12 months breast feedingb |
| Diet – inadequate intake of dietary fibre | >30 g/day for adult malesc |
| >25 g/day for adult femalesc | |
| Diet – inadequate intake of fruit | >300 g/day (∼2 serves/day)c |
| Diet – inadequate intake of non-starchy vegetables | >260 g/day (∼3.5 serves/day)c |
| Diet – red and processed meat consumption | Nonec |
| Hormones – menopausal hormone therapy* | None |
| Hormones – combined oral contraceptives* | None |
| Infectious agents | None |
| Overweight and obesity | BMI ≤25 kg/m2d |
| Insufficient physical activity | ≥300 minutes (5 hours ∼ 30 MET-hours) of moderate activity per weeke |
| Radiation – solar ultraviolet radiation (UVR) | Melanoma incidence in low ambient solar UVR population (UK) |
| Tobacco smoke | None |
* For cancers that have an increased risk
a: the reference level refers either to the category of ‘minimum exposure’ used in epidemiological studies, or where no consensus category exists, the level recommended by Australian or international guidelines for lowest cancer risk or optimum health. Specific agencies are listed below.
b: NHMRC guidelines recommend 12 months breastfeeding for each child. The level used here was determined pragmatically owing to the limited availability of breastfeeding prevalence data in the Australian population.
c: NHMRC Australian dietary guidelines19
d: World Health Organization ‘healthy weight’ category for body mass index
e: Australian guidelines for physical activity and sedentary behaviour20
Proportions of cancers attributable to modifiable exposures
Table 2 summarises the PAF estimates for 26 cancer sites, and for all cancers collectively (excluding BCC and SCC of the skin), for each of the 13 factors appraised. Detailed reports including numbers of cases of cancer attributed to these factors and sensitivity analyses have been reported in companion articles.3–14 In total, we found that 32% of all cancers (approximately 37,000 cases) diagnosed in Australia in 2010 (excluding BCC and SCC of the skin) could be attributed to the 13 factors (33% in men and 31% in women). Overall, tobacco smoke (PAF all cancers: 13.4%) was the leading cause of cancer in 2010, followed by solar radiation (6.2%), inadequate diet (6.1%) and overweight and obesity (3.4%), see Figure 1. The factors conferring the highest PAFs differed by sex: for men the highest proportions of cancer were attributable to tobacco smoke12(15.8%), solar radiation10 (7.1%) and alcohol consumption13(3.0%); while for women tobacco smoke12(10.1%), solar radiation10(5.0%) and overweight and obesity7(4.5%) were the leading causes.
Table 2.
Proportion (%) of incident cancer cases diagnosed in 2010 in Australia attributable to lifestyle and environmental factors
| % of cancer (0–85+ years) attributable to exposure, by cancer site |
|||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Cancer site | Oral cavity and pharynx (C00-C06; C09-C14)a | All Oesophagus (C15)a | Stomach (C16)a | Colorectum (C18-C20)a | Anus (C21)a | Liver (C22)a | Gall Bladder (C23)a | Pancreas (C25)a | Larynx (C32)a | Lung (C34)a | Melanoma (C43)a | Kaposi's Sarcoma (C46)a | Breast (C50)a | Vulva (C51)a | Vagina (C52)a | Uterine Cervix (C53)a | Endometrium (C54, C55)a | Ovary (C56)a | Penis (C60)a | Kidney & ureter (C64-C66)a | Bladder (C67)a | Hodgkin's lymphoma (C81)a | Non-Hodgkin's lymphoma (C82-C85, C96)a | Leukaemia (C91-C95)a | All cancersb |
| Males | |||||||||||||||||||||||||
| Tobacco smoke | 71.0 | 71.4 | 23.6 | 5.9 | - | 24.3 | - | 23.7 | 76.9 | 84.5 | - | - | - | - | - | - | - | - | - | 26.3 | 33.8 | - | - | 7.0 | 15.8 |
| Alcohol | 24.7 | 9.9 | - | 12.9 | - | 15.4 | - | - | 22.1 | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | 3.0 |
| UV radiation | - | - | - | - | - | - | - | - | - | - | 69.7 | - | - | - | - | - | - | - | - | - | - | - | - | - | 7.1 |
| Infections | 16.9 | - | 32.8 | - | 74.5 | 34.4 | - | - | - | - | - | 100.0 | - | - | - | - | - | - | 45.8 | - | - | 34.0 | 3.9 | - | 2.4 |
| Overweight and obesity | - | 18.0 | - | 11.7 | - | - | 15.8 | 9.1 | - | - | - | - | - | - | - | - | - | - | - | 17.6 | - | - | - | - | 2.5 |
| Insufficient physical activity | - | - | - | 4.2 | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | 0.5 |
| Diet – insufficient fibre | - | - | - | 18.6 | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | 2.3 |
| Diet – insufficient vegetables | 6.0 | 2.6 | 1.5 | - | - | - | - | - | 5.9 | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | 0.3 |
| Diet – insufficient fruit | 6.0 | 12.0 | 6.5 | - | - | - | - | - | 5.9 | 6.9 | - | - | - | - | - | - | - | - | - | - | - | - | - | - | 1.5 |
| Diet – red and processed meat | - | - | - | 21.7 | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | 2.7 |
| PAF combinedc | 83.9 | 74.2 | 52.7 | 55.8 | 74.5 | 58.0 | 15.8 | 30.6 | 84.1 | 86.0 | 69.7 | 100.0 | - | - | - | - | - | - | 45.8 | 39.3 | 33.8 | 34.0 | 3.9 | 7.0 | 32.9 |
| Females | |||||||||||||||||||||||||
| Tobacco smoke | 51.2 | 61.6 | 10.7 | 7.0 | - | 10.8 | - | 23.0 | 72.6 | 77.0 | - | - | - | - | - | 6.8 | - | 2.0 | - | 10.7 | 25.6 | - | - | 2.0 | 10.1 |
| Alcohol | 9.2 | 6.2 | - | 4.2 | - | 4.5 | - | - | 7.1 | - | - | - | 5.9 | - | - | - | - | - | - | - | - | - | - | - | 2.4 |
| UV radiation | - | - | - | - | - | - | - | - | - | - | 54.2 | - | - | - | - | - | - | - | - | - | - | - | - | - | 5.0 |
| Infections | 14.4 | - | 38.4 | - | 90.5 | 34.4 | - | - | - | - | - | 100.0 | - | 40.5 | 70.1 | 100.0 | - | - | - | - | - | 31.5 | 3.2 | - | 3.7 |
| Overweight and obesity | - | 7.7 | - | 5.5 | - | - | 13.3 | 6.1 | - | - | - | - | 6.8 | - | - | - | 26.4 | 3.6 | - | 14.4 | - | - | - | - | 4.5 |
| Insufficient physical activity | - | - | - | 5.4 | - | - | - | - | - | - | - | - | 6.8 | - | - | - | 6.0 | - | - | - | - | - | - | - | 2.9 |
| Diet – insufficient fibre | - | - | - | 16.2 | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | 2.1 |
| Diet – insufficient vegetables | 7.1 | 6.0 | 1.8 | - | - | - | - | - | 7.1 | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | 0.2 |
| Diet – insufficient fruit | 5.8 | 23.5 | 6.4 | - | - | - | - | - | 6.0 | 9.6 | - | - | - | - | - | - | - | - | - | - | - | - | - | - | 1.2 |
| Diet – red and processed meat | - | - | - | 12.5 | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | 1.6 |
| Hormones – MHT | - | - | - | - | - | - | - | - | - | - | - | - | 3.2 | - | - | - | 3.0 | 1.5 | - | - | - | - | - | - | 1.1 |
| Hormones – combined OCPs | - | - | - | - | - | - | - | - | - | - | - | - | 0.7 | - | - | 6.4 | - | - | - | - | - | - | - | - | 0.3 |
| Insufficient breast feeding | - | - | - | - | - | - | - | - | - | - | - | - | 1.7 | - | - | - | - | - | - | - | - | - | - | - | 0.5 |
| PAF combinedc | 66.8 | 76.1 | 49.4 | 41.6 | 90.5 | 44.1 | 13.3 | 27.8 | 77.8 | 79.3 | 54.2 | 100.0 | 22.8 | 40.5 | 70.1 | 100.0 | 32.9 | 6.9 | - | 23.6 | 25.6 | 31.5 | 3.2 | 2.0 | 30.7 |
| Persons | |||||||||||||||||||||||||
| Tobacco smoke | 65.3 | 60.0 | 19.2 | 6.4 | - | 20.7 | - | 23.4 | 76.4 | 81.6 | - | - | - | - | - | 6.8 | - | 2.0 | - | 20.4 | 31.8 | - | - | 4.9 | 13.4 |
| Alcohol | 20.3 | 8.8 | - | 9.0 | - | 12.5 | - | - | 20.1 | - | - | - | 5.9 | - | - | - | - | - | - | - | - | - | - | - | 2.8 |
| UV radiation | - | - | - | - | - | - | - | - | - | - | 63.3 | - | - | - | - | - | - | - | - | - | - | - | - | - | 6.2 |
| Infections | 16.2 | - | 34.7 | - | 84.0 | 34.4 | - | - | - | - | - | 100.0 | - | 40.5 | 70.1 | 100.0 | - | - | 45.8 | - | - | 32.9 | 3.6 | - | 2.9 |
| Overweight and obesity | - | 15.0 | - | 9.0 | - | - | 14.1 | 7.7 | - | - | - | - | 6.8 | - | - | - | 26.4 | 3.6 | - | 16.4 | - | - | - | - | 3.4 |
| Insufficient physical activity | - | - | - | 4.8 | - | - | - | - | - | - | - | - | 6.8 | - | - | - | 6.0 | - | - | - | - | - | - | - | 1.6 |
| Diet – insufficient fibre | - | - | - | 17.6 | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | 2.2 |
| Diet – insufficient vegetables | 6.3 | 3.6 | 1.6 | - | - | - | - | - | 6.1 | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | 0.3 |
| Diet – insufficient fruit | 6.0 | 15.4 | 6.5 | - | - | - | - | - | 5.9 | 9.6 | - | - | - | - | - | - | - | - | - | - | - | - | - | - | 1.3 |
| Diet – red and processed meat | - | - | - | 17.6 | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | 2.2 |
| Hormones – MHT | - | - | - | - | - | - | - | - | - | - | - | - | 3.2 | - | - | - | 3.0 | 1.5 | - | - | - | - | - | - | 0.5 |
| Hormones – combined OCPs | - | - | - | - | - | - | - | - | - | - | - | - | 0.7 | - | - | 6.4 | - | - | - | - | - | - | - | - | 0.1 |
| Insufficient breast feeding | - | - | - | - | - | - | - | - | - | - | - | - | 1.7 | - | - | - | - | - | - | - | - | - | - | - | 0.2 |
| PAF combinedc | 79.6 | 74.7 | 51.4 | 49.8 | 84.0 | 54.4 | 14.1 | 29.3 | 83.3 | 83.3 | 63.3 | 100.0 | 22.8 | 40.5 | 70.1 | 100.0 | 32.9 | 6.9 | 45.8 | 33.4 | 31.8 | 32.9 | 3.6 | 4.9 | 31.9 |
Abbreviations: PAF = Population attributable fraction; MHT = menopausal hormone therapy; OCPs = oral contraceptive pills
a: International Classification of Diseases (ICD-10) code
b: Excluding cases of basal cell carcinoma and squamous cell carcinoma of the skin;
Note: The proportions (%) presented here are for the entire Australian population (0–85+ years) to ensure comparability across all exposures. The PAFs in the table therefore may differ from the PAFs presented in the exposure-specific papers in this series.
Figure 1.
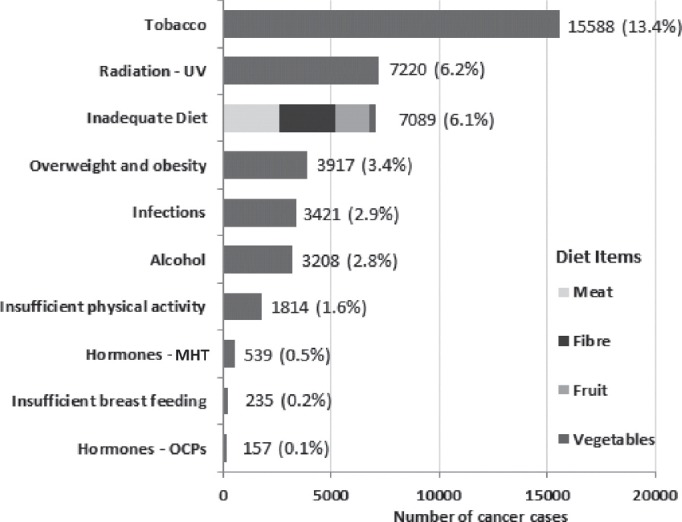
Number and percentage of cancer cases diagnosed in Australia in 2010 attributable to select lifestyle and environmental exposures. Abbreviations: MHT – menopausal hormone therapy; OCPs – combined oral contraceptive pills.
The cancer sites with the greatest fractions of potentially preventable cases were uterine cervix (100%) and Kaposi's sarcoma (100%), for which infectious agents (human papillomarvirus [HPV] and Kaposi's sarcoma herpes virus [KSHV], respectively) are considered necessary causal factors (Figure 2). Other sites with very high fractions of potentially preventable cancers were oral cavity and pharynx (80%), oesophagus (75%), anus (84%), larynx (83%) and lung (83%). In absolute terms, the sites with the greatest number of potentially preventable cancers were lung (8,569), colorectal (7,404), melanoma of the skin (7,220) and breast (3,233).
Figure 2.
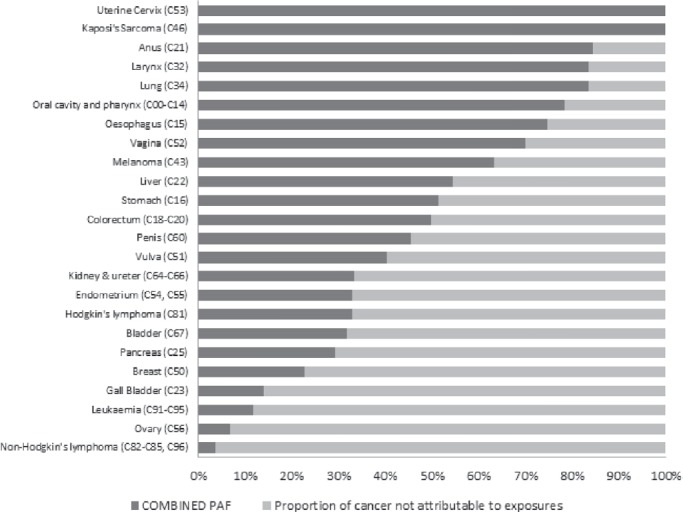
Combined PAF for cancers associated with one or more modifiable exposures.
The incidence and attributable fraction of the 10 most common cancers in Australian men and women are displayed in Figure 3. Prostate cancer is the most commonly occurring cancer in Australian men and has no accepted causes. The PAF estimate for all cancers is clearly affected by the lack of modifiable factors for this very common cancer. Of the subset of cancers with known, modifiable causes, we estimated that 43% of those arising in the Australian population in 2010 could be attributed to exposure to the 13 causal factors listed. For some exposures, PAFs were much higher for men than women. This was most noticeable for cancers attributable to alcohol (e.g. oral cavity and pharynx: men 25% vs. women 9%; colorectum: men 13% vs. women 4%; liver: men 15% vs. women 5%), red and processed meat intake (colorectal cancer: men 22% vs. women 13%), and tobacco (oral cavity and pharynx: men 71% vs. women 51%; stomach: men 24% vs. women 11%). As a result, a markedly higher proportion of those cancers were attributable to exposure to modifiable factors in men (52%) than women (35%), see Table 2.
Figure 3.
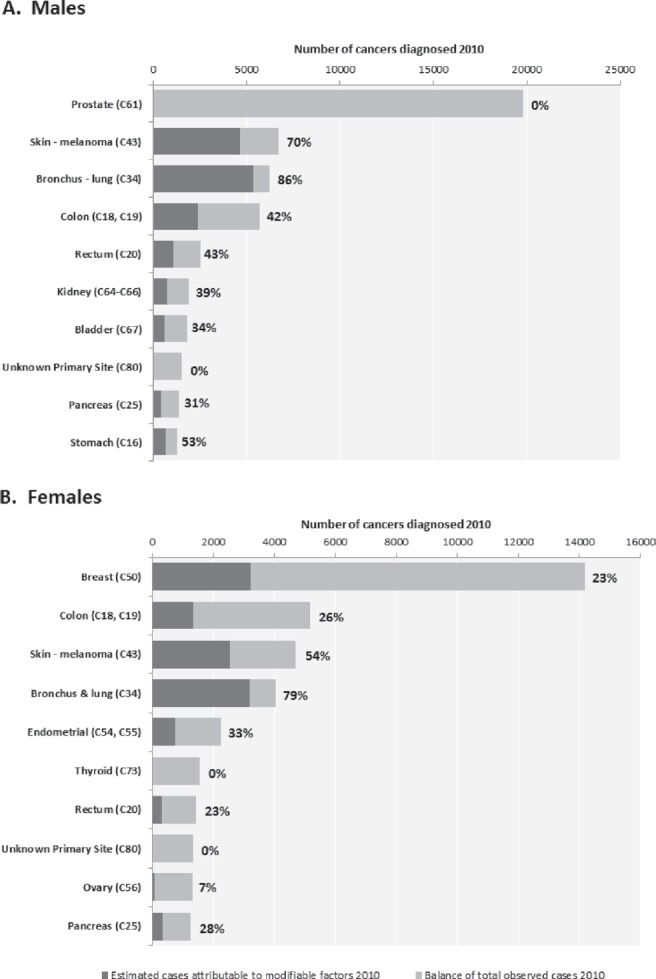
The ten cancer sites with highest incidence in Australia in 2010: total number of cases and fraction attributable to modifiable factors for A. Males and B. Females.
Knowledge about the causes of cancer continues to evolve. There is strengthening evidence that a number of the factors considered here also cause cancer at other sites, including overweight/obesity,7,15 (cancers of the thyroid, non-Hodgkin's lymphoma, multiple myeloma, melanoma and leukaemia), menopausal hormone therapy4 (cancers of the breast – oestrogen-only formulations – and ovary) and insufficient breast-feeding5 (ovarian cancer). Because no independent cancer agencies have declared these associations to be causal, we did not include them in our primary analyses. However, we did conduct supplementary analyses to investigate the potential magnitude of the additional cancer burden that might have accrued due to these exposures. In fact, including these ‘supplementary’ cancers made negligible difference to the total PAFs for men (from 32% to 33%) and women (from 31% to 32%).
The summaries reported above do not include estimates of the fraction of cancer attributable to occupational exposures. This is because there were no reliable data on past exposures to occupational carcinogens in Australia, although recent occupational exposures have been recorded with high quality.16 We considered using a ‘lifetime risk’ approach for occupational exposures, which estimates the proportion of future cancers that can be attributed to exposures received in a specific year. While similar in concept to the attributable risk approach used for all other exposures, the outputs from the two approaches cannot be combined. In future work, we plan to explore the burden of cancer in Australia attributable to occupation exposures.
Prevented fractions
Four factors (daily sunscreen use,10 daily aspirin use,14 menopausal hormone therapy [MHT]4 and combined oral contraceptives6) were deemed likely to prevent certain cancers; for these factors, we estimated the prevented fraction (PF) of cancer associated with exposure (Table 3). The PF estimates the proportion of the hypothetical ‘total load’ of cancer that was prevented due to prevailing levels of exposure to the factor in the population.17 About 28% of Australians reported using sunscreen daily in 2010, and we estimated that this level of use reduced the population incidence of SCC of the skin by about 9% (and possibly melanoma of the skin by about 14%).10 Similarly, the incidence of cancers of the colorectum and oesophagus were reduced by about 2% and 3%, respectively, due to prevailing levels of aspirin use in the population.14 Estimating the impact of exogenous hormones on cancer incidence presents some challenges, as certain formulations cause some cancers and prevent others. On balance, MHT caused more cancers than it prevented, whereas the oral contraceptive pill prevented more cancers than it caused. We estimated that exposure to the combined oral contraceptive pill prevented 1,032 endometrial (PF 31%) and 308 ovarian (PF 19%) cancers, but likely caused 105 breast (PAF 0.7%) and 52 cervical (PAF 6.4%) cancers.6 Similarly, oestrogen-only MHT was estimated to prevent 52 colorectal cancers, but post-menopausal MHT (combined and oestrogen-only) caused up to 670 cancers, mostly breast cancers.4
Table 3.
Prevented fraction (PF) and estimated number of cancers prevented in Australia in 2010 through use of aspirin, exogenous hormones and sunscreen
| Exposure | Colorectal (C18-C20)a | Oesophagus (C15)a | SCC of the Skinb | Endometrium (C54, C55)a | Ovarian (C56)a | |||||
|---|---|---|---|---|---|---|---|---|---|---|
| PF% | Cancers Prevented | PF% | Cancers Prevented | PF% | Cancers Prevented | PF% | Cancers Prevented | PF% | Cancers Prevented | |
| Males | ||||||||||
| Aspirin | 2.3 | 198 | 3.3 | 34 | – | – | – | – | – | – |
| Sunscreen | – | – | – | – | 7.5 | 6,793 | – | – | – | – |
| Females | ||||||||||
| Aspirin | 2.0 | 136 | 3.9 | 17 | - | - | – | – | – | – |
| Sunscreen | – | – | – | – | 12.1 | 7,399 | – | – | – | – |
| Hormones – MHTc | 0.8 | 52 | – | – | – | – | – | – | – | – |
| Hormones – combined OCPd | – | – | – | – | – | – | 31.4 | 1,032 | 19.1 | 308 |
a: International Classification of Diseases (ICD-10) Code
b: SCC of the skin = Squamous cell carcinoma of the skin
c: MHT = menopausal hormone therapy
d: OCP = combined oral contraceptive pill
Potential impact of changing the prevalence of exposures
The PAF for any causal factor represents the theoretical maximum proportion by which the incidence of cancer could have been reduced, assuming that everybody in the population had been exposed at the reference level. For many exposures, however, it is not feasible to expect population-wide changes to an optimum exposure level. We therefore measured the potential impact on cancer incidence in Australia in 2010 of changing the prevalence of some common factors to those levels recommended by Australian guidelines (for alcohol,18 red & processed meat19 and physical activity20) or to historic levels (for overweight/obesity) or otherwise achievable targets (for dietary fibre,8 breastfeeding5 and MHT4), see Table 4. Again, we used standard formulae to calculate the potential impact fraction (PIF) using either of two similar approaches, depending upon whether we modelled a shift in the prevalence distributions21 or a change in the risks of exposure.22 Briefly, for each cancer site, we calculated the number of cases that would have occurred in Australia in 2010 if the alternative scenario of exposure had prevailed. The PIF is then the proportional difference between the numbers of cancers actually observed and the numbers expected under the alternative (counterfactual) exposure scenarios. Our analyses suggest that substantial gains in cancer prevention could be achieved through relatively modest reductions in alcohol13 and meat intake,9 and an increase in fibre intake simply by eating fruit (2 servings/day) and vegetables (5 servings/day).8
Table 4.
The potential impact on cancer incidence of changing exposure to modifiable causal factors
| Modifiable factor | Alternative scenarios in population exposures | PIF (%) |
|---|---|---|
| Alcohol | 1. All who consume > 4 drinks/day reduce intake to ≤4 drinks/day 2. All who consume > 4 drinks/day reduce intake to ≤2 drinks/day | 2.2% 4.3% |
| Breast feeding | 1. Parous women who never breast feed increase to 1–3 months and those who breast feed for 1–6 months increase to >6–7 months 2. Parous women who breast feed for 1–6 months increase to >6–7 months (i.e. no change in prevalence of those who never breast feed) | 0.4% 0.3% |
| Diet – inadequate fibre | 1. Entire population increases fibre intake by eating the recommended daily serves of fruit and vegetables | 8.8% |
| Diet – red and processed meat | 1. All who consume >100g meat/day reduce intake to ≤100g meat/day 2 All who consume >65g meat/day reduce intake to ≤65g meat/day | 1.4% 5.4% |
| Menopausal hormone therapy | 1. Reduce MHT use by 25% across all age categories | 0.8% |
| Overweight/obesity | 1. Australian population reverts to BMI distribution of 1990 | 2.0% |
| Insufficient physical activity | 1. All who exercise below 30 MET-hours/week increase their exercise by 3 MET-hours/week (30 minutes per week) | 1.2% |
Comparisons with international studies
The approach used in this Australian study was virtually identical to that taken for the recent UK PAF Project,23 and was greatly enabled by the UK investigator (DMP) making his background materials, including worked spreadsheets, freely available. Overall, the proportions of cancers attributable to modifiable exposures were remarkably consistent, with tobacco contributing by far the highest cancer burden in both countries (Table 5). Nonetheless, there were some differences between the Australian and UK studies in the magnitude of specific PAF estimates. In part, this was due to the use of updated (and typically lower) risk estimates for dietary factors, based on new meta-analyses of prospective cohort studies that were not available at the time of the UK study. However, given the overall uniformity of approaches, most of the differences between the UK and Australian PAF estimates largely reflect differences in the underlying prevalence of exposures between the two populations. Thus, the proportions of cancers attributable to smoking and alcohol were notably higher in the UK than Australia, due to higher exposure prevalences of both factors in the UK population in recent decades. Not surprisingly, the proportion of all cancers (except BCC and SCC) in Australia attributable to sunlight was almost twice that of the UK. While some caution is warranted in comparing the PAFs for sunlight, since different reference populations were required for the calculations in each country, the relative proportions of cancer attributable to sunlight in the two populations appear consistent with the relative amounts of solar radiation to which they are exposed.
Table 5.
Comparison of PAF estimates for Australia and the United Kingdom
| Exposure | Aust PAF males (%) | Aust PAF females (%) | Aust PAF persons (%) | UK PAF males (%) | UK PAF females (%) | UK PAF persons (%) |
|---|---|---|---|---|---|---|
| Tobacco | 15.8 | 10.1 | 13.4 | 23.0 | 15.6 | 19.4 |
| Alcohol | 3.0 | 2.4 | 2.8 | 4.6 | 3.3 | 4.0 |
| Solar (UV) radiation | 7.1 | 5.0 | 6.2 | 3.5 | 3.6 | 3.5 |
| Infectious agents | 2.4 | 3.7 | 2.9 | 2.5 | 3.7 | 3.1 |
| Overweight and obesity | 2.5 | 4.5 | 3.4 | 4.1 | 6.9 | 5.5 |
| Insufficient physical activity | 0.5 | 2.9 | 1.6 | 0.4 | 1.7 | 1.0 |
| Diet – insufficient fibre | 2.3 | 2.1 | 2.2 | 1.4 | 1.7 | 1.5 |
| Diet – insufficient fruit | 1.5 | 1.2 | 1.3 | 6.1a | 3.4a | 4.7a |
| Diet – insufficient non-starchy vegetables | 0.3 | 0.2 | 0.3 | |||
| Diet – red and processed meat | 2.7 | 1.6 | 2.2 | 3.5 | 1.9 | 2.7 |
| Diet – salt | n/a | n/a | n/a | 0.9 | 0.2 | 0.5 |
| Hormones – MHT | – | 1.1 | 0.3 | – | 1.1b | 0.5b |
| Hormones – combined OCP | – | 0.3 | 0.1 | – | – | – |
| Breast feeding | – | 0.5 | 0.2 | – | 1.7 | 0.9 |
| Ionising radiation | n/a | n/a | n/a | 1.7 | 2.0 | 1.8 |
| Occupation | n/a | n/a | n/a | 4.9 | 2.4 | 3.7 |
| PAF Combinedc | 32.8 | 30.6 | 31.8 | 45.3 | 40.1 | 42.7 |
Abbreviations: PAF – population attributable fraction expressed as a percentage; Aust – Australia; UK – United Kingdom; UV – ultraviolet; MHT – menopausal hormone therapy; OCP – oral contraceptive pills; n/a – not applicable
a: UK analysis provided PAF estimate for fruit and vegetables combined
b: UK analysis provided PAF estimate for post-menopausal hormones only
c: PAF Combined = 1- (1-PAF1)*(1-PAF2)*(1-PAFn)
Estimates of the burden of cancer attributable to modifiable factors have also been conducted for other populations recently, including France24 and the US.25 Those investigations reported generally higher fractions attributable to each factor than we have reported here. Again, some of this is explained by different exposure prevalences, but the methods used in those studies differed substantially from the recent UK and Australian studies. In particular, those studies tended to stratify the population into a limited number of exposure categories, an approach that does not account for the gradations in risk associated with continuous distributions of exposure. As such, they tend to inflate the estimates of attributable fractions and, for this reason, are not directly comparable to the analyses reported by the UK and Australian studies.
Limitations
A number of issues have a bearing on the interpretation of the estimates reported here and in companion papers. First, in terms of the overall proportion of cancers attributable to modifiable factors, we note that our investigation was limited to only 13 factors for which there is international consensus regarding causality for cancer. Other factors known to cause cancer were not included in our final analyses, either because they cannot be modified in any practical sense (such as early menarche or nulliparity) or because prevalence data in the Australian population are so poorly collated as to be unusable (such as exposure to ionising radiation from medical sources). The latter is especially disturbing; since one might expect that a register of exposures to a known carcinogen would be mandated and audited for safety purposes.26
Second, as mentioned above, the estimates of attributable fractions are sensitive to the magnitude of effect sizes and prevalence. For our primary analyses, we used the most recent summary risk estimates from independent agencies when available; if not, we used estimates from recent, high-quality meta-analyses, preferably restricted to cohort studies. Prevalence data were sourced preferentially from national surveys, or else from population-based studies with large samples when national survey data were not available. A salutary finding from this exercise was the overall low quality of information regarding exposure to Group 1 carcinogens in the Australian population. For pharmacological factors in particular, nationally representative data describing past exposures across age and sex were not available, and so we constructed matrices of exposure using multiple data sources. Detailed data on population exposures to ionising radiation from medical sources are not collected, rendering analyses for these exposures incomplete. Similarly, data on exposures to infectious agents and dietary factors were incomplete or out of date. Given these constraints, we conducted sensitivity analyses for all factors incorporating a range of estimates of risk or exposure prevalence to assess the distribution within which a plausible estimate of attributable fraction might lie. We did not model interactions between causes owing to a scarcity of summary risk estimates and absence of suitably stratified prevalence data. As such, it is likely that estimates of the fraction of cancer attributable to certain factors will include a proportion that was caused only because of exposure to a co-factor. Thirdly, cancer risk assessments and causal associations are continually being reviewed. While we have anticipated some likely changes in assessments of causality for certain cancers (e.g. for obesity and thyroid cancer, non-Hodgkin's lymphoma, multiple myeloma and leukaemia), future assessments of cancer burden will need to consider newly classified associations. Notably, at the time of performing our analyses, obesity was not considered causally associated with prostate cancer; however, an update in November 201427 found that body fatness is “probably” a cause of advanced prostate cancer. We performed preliminary analyses to estimate the ramifications of the WCRF declaration and found that about 353 advanced prostate cancer cases (6% of all advanced prostate cancers; 1.8% of all prostate cancers) diagnosed in 2010 might be attributed to overweight and obesity in the Australian adult population.7 Clearly, newly declared associations of this type will require further investigation as new data are generated.
Finally, consideration was given to the likely latent period between exposure and cancer for each factor, as this determined the choice of time period for obtaining prevalence data. For most factors, the latent period is unknown but is assumed to be many years; thus we typically sought data for the prevalence of exposures about 10 years before cancer diagnosis, except for specific factors for which other patterns of exposure were considered relevant (e.g. exogenous hormones: MHT – current use; breast feeding – total duration; OCP – ever exposed).
Conclusions
Cancer imposes a heavy burden on Australians' health. In total, cancers are the leading cause of death and disability-adjusted life years (DALYs) in Australia and one of the most expensive disease categories in terms of health expenditure.28,29 Many cancers are known to be caused by factors that are prevalent in the environment and for which exposures can be modified.
Continued and better monitoring of exposure to causal factors is recommended to inform primary prevention efforts. While the National Health Surveys are an important tool for assessing the prevalence of health-related factors, they are necessarily limited in scope and cannot capture information on all causes of cancer. Moreover, there is no capacity presently to link the records from that survey to health outcomes data. Given the investment in collecting these prevalence data, serious consideration ought to be given to the enormous benefits that would be derived from linking them to health datasets in the future, particularly as techniques for preserving privacy are now well-established. It is greatly concerning, however, that nationally representative, person-based datasets are lacking for key factors known to cause cancer, especially medical exposure to ionising radiation and pharmacological factors. Establishing such repositories should be a national priority.
Conservatively, we estimate that about one-third of cancers arising in the Australian population are attributable to modifiable causes and could – in theory – be prevented if exposure to those factors were eliminated entirely. Of those cancers that have known causes, about half are potentially preventable in men, and more than one-third are preventable in women. Extreme interventions would be required to achieve such outcomes, however, and are unlikely ever to be realised. More modest targets can be identified by calculating potential impact fractions; our analyses suggest substantial gains by targeting smoking, diet, alcohol and sun exposure.
Acknowledgments
This work was supported by a grant from Cancer Council Australia. DCW, PMW, REN, NP, SJJ and AA were supported by Research Fellowships from the National Health and Medical Research Council of Australia (NHMRC). Associate investigators were supported by a NHMRC Program Grant (552429). The funding bodies had no role in the design and conduct of the study, the collection, management, analysis, and interpretation of the data, or the preparation, review, or approval of the manuscript.
PAF Project
Chief Investigators: David C. Whiteman, Penelope M. Webb, Adele C. Green, Rachel E. Neale, Lin Fritschi
Associate Investigators: Louise F. Wilson, Catherine M. Olsen, Christina M. Nagle, Nirmala Pandeya, Susan J. Jordan, Annika Antonsson, Bradley J. Kendall, Torukiri I. Ibiebele, Maria Celia B. Hughes, Kyoko Miura, Susan Peters, Renee N. Carey
Advisers: Christopher J. Bain, D. Max Parkin
References
- 1.Australian Institute of Health and Welfare. Cancer Data. Pivot Table [Internet] Canberra (AUST): AIHW; 2015. [cited 2014 Jun 23]. Available from: http://www.aihw.gov.au/cancer-data/ [Google Scholar]
- 2.Whiteman DC, Webb PM, Green AC, Neale RE, Fritschi L, Bain CJ, et al. Cancers in Australia in 2010 attributable to modifiable factors: introduction and overview. Aust NZ J Public Health. 2015;39:403–7. doi: 10.1111/1753-6405.12468. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Antonsson A, Wilson LF, Kendall BJ, Bain CJ, Whiteman DC, Neale RE. Cancers in Australia in 2010 attributable to infectious agents. Aust NZ J Public Health. 2015;39:446–51. doi: 10.1111/1753-6405.12445. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Jordan SJ, Wilson LF, Nagle CM, Green AC, Olsen CM, Bain CJ, et al. Cancers in Australia in 2010 attributable to and prevented by the use of menopausal hormone therapy. Aust NZ J Public Health. 2015;39:434–40. doi: 10.1111/1753-6405.12451. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Jordan SJ, Wilson LF, Nagle CM, Green ACCM, Bain CJ, et al. Cancers in Australia in 2010 attributable to total breastfeeding durations of 12 months or less by parous women. Aust NZ J Public Health. 2015;39:418–21. doi: 10.1111/1753-6405.12457. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Jordan SJ, Wilson LF, Nagle CM, Green AC, Olsen CM, Bain CJ, et al. Cancers in Australia in 2010 attributable to and prevented by the use of combined oral contraceptives. Aust NZ J Public Health. 2015;39:441–5. doi: 10.1111/1753-6405.12444. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kendall BJ, Wilson LF, Olsen CM, Webb PM, Neale RE, Bain CJ, et al. Cancers in Australia in 2010 attributable to overweight and obesity. Aust NZ J Public Health. 2015;39:452–7. doi: 10.1111/1753-6405.12458. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Nagle CM, Wilson LF, Hughes MB, Ibiebele TI, Miura K, Bain CJ, et al. Cancers in Australia in 2010 attributable to inadequate consumption of fruit, non-starchy vegetables and dietary fibre. Aust NZ J Public Health. 2015;39:422–8. doi: 10.1111/1753-6405.12449. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Nagle CM, Wilson LF, Hughes MB, Ibiebele TI, Miura K, Bain CJ, et al. Cancers in Australia in 2010 attributable to the consumption of red and processed meat. Aust NZ J Public Health. 2015;39:429–33. doi: 10.1111/1753-6405.12450. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Olsen CM, Wilson LF, Green AC, Bain CJ, Fritschi L, Neale RE, et al. Cancers in Australia attributable to exposure to solar ultraviolet radiation and prevented by regular sunscreen use. Aust NZ J Public Health. 2015;39:471–6. doi: 10.1111/1753-6405.12470. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Olsen CM, Wilson LF, Nagle CM, Kendall BJ, Bain CJ, Pandeya N, et al. Cancers in Australia in 2010 attributable to insufficient physical activity. Aust NZ J Public Health. 2015;39:458–63. doi: 10.1111/1753-6405.12469. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Pandeya N, Wilson LF, Bain CJ, Martin KL, Webb PM, Whiteman DC. Cancers in Australia in 2010 attributable to tobacco smoke. Aust NZ J Public Health. 2015;39:464–70. doi: 10.1111/1753-6405.12446. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Pandeya N, Wilson LF, Webb PM, Neale RE, Bain CJ, Whiteman DC. Cancers in Australia in 2010 attributable to the consumption of alcohol. Aust NZ J Public Health. 2015;39:408–13. doi: 10.1111/1753-6405.12456. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Wilson LF, Green AC, Kendall BJ, Jordan SJ, Nagle CM, Bain CJ, et al. Cancers prevented in Australia in 2010 through the consumption of aspirin. Aust NZ J Public Health. 2015;39:414–7. doi: 10.1111/1753-6405.12443. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Renehan AG, Tyson M, Egger M, Heller RF, Zwahlen M. Body-mass index and incidence of cancer: A systematic review and meta-analysis of prospective observational studies. Lancet. 2008;371(9612):569–78. doi: 10.1016/S0140-6736(08)60269-X. [DOI] [PubMed] [Google Scholar]
- 16.Carey RN, Driscoll TR, Peters S, Glass DC, Reid A, Benke G, et al. Estimated prevalence of exposure to occupational carcinogens in Australia (2011-2012) Occup Environ Med. 2014;71(1):55–62. doi: 10.1136/oemed-2013-101651. [DOI] [PubMed] [Google Scholar]
- 17.Porter M, Greenland S, Hernan M, dos Santos Silva I, Last JM, editors. A Dictionary of Epidemiology. 6th ed. New York (NY): Oxford University Press; 2014. [Google Scholar]
- 18.National Health and Medical Research Council. Australian Guidelines to Reduce Health Risks for Drinking Alcohol. Canberra (AUST): Commonwealth of Australia; 2009. [Google Scholar]
- 19.National Health and Medical Research Council. Australian Dietary Guidelines. Canberra (AUST): Commonwealth of Australia; 2013. [Google Scholar]
- 20.Department of Health. Australia's Physical Activity and Sedentary Behaviour Guidelines for Adults (18-64 Years) [Internet] Canberra (AUST): Commonwealth of Australia; 2014. [cited 2014 Feb 11]. Available from: http://www.health.gov.au/internet/main/publishing.nsf/content/health-pubhlth-strateg-phys-act-guidelines#apaadult. [Google Scholar]
- 21.Morgenstern H, Bursic ES. A method for using epidemiologic data to estimate the potential impact of an intervention on the health status of a target population. J Community Health. 1982;7(4):292–309. doi: 10.1007/BF01318961. [DOI] [PubMed] [Google Scholar]
- 22.Barendregt JJ, Veerman JL. Categorical versus continuous risk factors and the calculation of potential impact fractions. J Epidemiol Community Health. 2010;64(3):209–12. doi: 10.1136/jech.2009.090274. [DOI] [PubMed] [Google Scholar]
- 23.Parkin DM, Boyd L, Walker LC. The fraction of cancer attributable to lifestyle and environmental factors in the UK in 2010. Br J Cancer. 2011;105(Suppl 2):77–81. doi: 10.1038/bjc.2011.489. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.International Agency for Research on Cancer Working Group. Attributable Causes of Cancer in France in the Year 2000. Lyon (FRC): World Health Organization; 2007. [Google Scholar]
- 25.World Cancer Research Fund. Policy and Action for Cancer Prevention, Food, Nutrition and Physical Activity: A Global Perspective. Washington (DC): American Institute for Cancer Research; 2009. [Google Scholar]
- 26.Mathews JD, Forsythe AV, Brady Z, Butler MW, Goergen SK, Byrnes GB, et al. Cancer risk in 680,000 people exposed to computed tomography scans in childhood or adolescence: Data linkage study of 11 million Australians. BMJ. 2013;346:f2360. doi: 10.1136/bmj.f2360. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.World Cancer Research Fund International. Continuous Update Project Report: Diet, Nutrition, Physical Activity and Prostate Cancer. London (UK): WCRF International; 2014. [Google Scholar]
- 28.Institute for Health Metrics and Evaluation. GBD Compare. Australia, DALYs Both Sexes, All Ages, 2010 [Internet] Seattle (WA): Univesity of Washington; 2013. [cited 2015 Jul 17]. Available from: http://vizhub.healthdata.org/gbd-compare/ [Google Scholar]
- 29.Australian Institute of Health and Welfare. Cancer Series No.: 81. Canberra (AUST): AIHW; 2013. Health System Expenditure on Cancer and Other Neoplasms in Australia: 2008-09. [Google Scholar]


