Abstract
Background
A routine 2-dose varicella vaccination program was adopted in 2007 in the United States to help further decrease varicella disease and prevent varicella outbreaks. We describe trends and characteristics of varicella outbreaks reported to CDC during 2005–2012 from 9 states.
Methods
Data on varicella outbreaks collected by 9 state health departments were submitted to CDC using the CDC outbreak reporting worksheet. Information was collected on dates of the outbreak, outbreak setting, and number of cases by outbreak; aggregate data was provided on the numbers of outbreak-related cases by age group, vaccination status, and laboratory confirmation.
Results
Nine hundred and twenty-nine outbreaks were reported from the 6 states which provided data for each year during 2005–2012. Based on data from these 6 states, the number of outbreaks declined by 78%, decreasing from 147 in 2005 to 33 outbreaks in 2012 (p=0.0001). There were a total of 1,015 varicella outbreaks involving 13,595 cases reported by the 9 states from 2005–2012. The size and duration of outbreaks declined significantly over time (p<0.001). The median size of outbreaks was 12, 9, and 7 cases and median duration of outbreaks was 38, 35, and 26 days during 2005–2006, 2007–2009, and 2010–2012 respectively. Majority of outbreaks (95%) were reported from schools, declining from 97% in 2005–2006 to 89% in 2010–2012. Sixty-five percent of outbreak-related cases occurred among 5–9 year olds, with the proportion declining from 76% in 2005–2006 to 45% during 2010–2012.
Conclusions
The routine 2-dose varicella vaccination program appears to have significantly reduced the number, size, and duration of varicella outbreaks in the U.S.
Keywords: varicella, chickenpox, outbreaks, surveillance, varicella vaccination
Introduction
In 2007, the Advisory Committee on Immunization Practices (ACIP) adopted a recommendation for a routine 2-dose varicella vaccination program in the United States1. Prior to that, the U.S. had a routine 1-dose varicella vaccination program implemented beginning in 1996. Although the 1-dose program significantly reduced varicella disease burden, especially for severe disease resulting in hospitalizations and deaths, outbreaks continued to be reported, even among elementary school-aged populations with high 1-dose coverage1–4. These outbreaks were burdensome and challenging for state health departments to control and investigate. Therefore, one of the rationales for implementation of the routine 2-dose varicella vaccination program was to help further decrease and prevent varicella outbreaks.
Varicella in vaccinated children, also known as breakthrough varicella, can occur in about 15–20% of 1-dose vaccinated children. Breakthrough varicella has been found to be milder than varicella in unvaccinated children5. However, these cases are still infectious. Studies have shown that 2 doses of varicella vaccine provide more protection than 1-dose6, 7 with a vaccine-effectiveness of approximately 94–98%6, 8, 9. Since implementation of the routine 2-dose varicella vaccination program, additional declines in varicella incidence and outbreaks have been documented in a limited number of states, communities, and health systems.10–13
We describe the trends and characteristics of varicella outbreaks reported by state health departments to CDC during 2005–2012, the period in which the 2-dose varicella vaccination program was implemented in the United States.
Materials and Methods
We reviewed state outbreak surveillance practices and state-based school entry requirements for varicella vaccination among participating states. Data on varicella outbreaks collected by state health departments were submitted to CDC using the CDC outbreak reporting worksheet http://www.cdc.gov/chickenpox/outbreaks/downloads/appx-a-vor-wksht.pdf. Six states (California, Maryland, Minnesota, Texas, Vermont, and West Virginia) provided data on varicella outbreaks annually to CDC during the entire period 2005–2012. Data from these states were used to describe trends in varicella outbreaks. Data from three additional states (Colorado, Michigan, and Mississippi), which were not available for every year of the study period were included in the analysis of outbreak characteristics.
Varicella outbreaks were defined differently by state and changed across time for some states. Varicella outbreaks were defined as the occurrence of ≥2–5 cases that are epidemiology-linked (Table 1). For this analysis, we defined a varicella outbreak as ≥3 cases. States provided information on dates of the outbreak (rash onset dates of the first and the last reported varicella case), outbreak setting, and number of cases by outbreak. Aggregate data were provided on the numbers of cases by outbreak by age group (<1, 1–4, 5–9, 10–14, 15–19, and ≥20 years), vaccination status (unvaccinated, 1 or 2-doses, unknown), and laboratory confirmation. A laboratory-confirmed outbreak was defined as an outbreak that had ≥1 case with a positive varicella-zoster virus (VZV) laboratory test. Calendar years were grouped as 2005–2006, 2007–2009, and 2010–2012 to reflect the period before the 2-dose program was implemented, early implementation of the 2-dose program, and later implementation of the 2-dose program.
Table 1.
Summary of varicella outbreak surveillance and varicella immunization school-entry requirements by state
| State | Type of varicella outbreak surveillance | Definition of varicella outbreak | Years of outbreak surveillance data | Varicella immunization requirements for Kindergarten entry | |
|---|---|---|---|---|---|
| Year 1-dose requirement implemented | Year 2-dose requirement implemented | ||||
| California | passive surveillance | ≥ 5 cases | 2005–2012 | 2001 | |
| Colorado | passive surveillance | ≥ 5 cases | 2007–2012 | 2000 | 2007 |
| Maryland | passive surveillance | ≥ 3 cases | 2005–2012 | 2001 | 2014 |
| Michigan | passive surveillance | ≥ 5 cases | 2006–2012 | 2002 | 2010 |
| Minnesota | passive surveillance 2005–2012 and active surveillance in a subset of school sentinel sites 2009–2012 | ≥ 5 cases | 2005–2012 | 2004 | 2009 |
| Mississippi | passive surveillance | ≥ 2 cases, dependent on setting | 2007–2011 | 2002 | 2009 |
| Texas | passive surveillance | ≥ 2 to 5 cases, dependent on setting | 2005–2012 | 2000 | 2009 |
| Vermont | passive surveillance | ≥ 5 cases | 2005–2012 | 2008 | |
| West Virginia | passive surveillance 2005–2009 and active surveillance 2010–2012 | ≥ 5 cases (during 2010–2011, revised definition to ≥ 3 cases) | 2005–2012 | 2008 | |
We used Poisson regression to look at trends during 2005–2012 in the number of outbreaks, size of the outbreak, duration of outbreak, and proportion of laboratory-confirmed outbreaks. We used the Cochrane Armitage trend test to look for trends during the study period in the age distribution of cases, setting, size, and cases by vaccination status and their vaccine doses. We excluded 2 outbreaks which were missing information on outbreak dates from the entire analysis. Two-sided P-values < 0.05 were considered statistically significant. Data were analyzed using SAS 9.3 (SAS Institute Inc., Cary, NC).
Varicella outbreak surveillance practices evolved during the period in which these data were collected (Table 1). Two of the states, Minnesota and West Virginia, participated in CDC-funded projects to strengthen school-based varicella outbreak surveillance during 2009–2012. Beginning in 2009, Minnesota expanded school-based surveillance by adding active outbreak surveillance in 80 schools to their existing passive surveillance in sentinel schools. West Virginia, which began collecting information on varicella outbreaks from schools in 2005, implemented active surveillance in all schools statewide in 2010. The remaining states used passive outbreak surveillance during the study period.
State-based school entry requirements for varicella vaccination also evolved during 2005–2012 (Table 1). Seven states implemented a 1-dose varicella vaccination requirement for Kindergarten entry prior to 2005. Two-dose varicella vaccination requirements for school entry were implemented in 8 of the states during the study period beginning in 2007 (Table 1).
Results
Nine hundred and twenty-nine outbreaks were reported from the 6 states which provided data for each year during this study period: 417 (45%) from California, 53 (6%) from Maryland, 252 (27%) from Minnesota, 117 (13%) from Texas, 24 (3%) from Vermont and 66 (7%) from West Virginia. One outbreak reported from Texas with 2 cases was excluded from the analysis. The number of outbreaks declined by 78%, decreasing from 147 in 2005 to 33 outbreaks in 2012 (p=0.0001) (Figure 1). For California and Maryland, the average annual number of outbreaks during 2005–2012 decreased over time, from 97 to 12 in California and from 14 to 2 in Maryland. In Minnesota, 1 of 2 states which participated in the CDC-funded varicella outbreak surveillance project, the average annual number of outbreaks decreased from 54 outbreaks before the 2009–2010 school-year to 12 outbreaks in the 2010–2011 school-year even as active surveillance was implemented in 80 schools. In West Virginia, the other state which participated in the varicella outbreak surveillance project, there was an increase in the average annual number of outbreaks reported coincident with implementation of active surveillance with a peak of 21 outbreaks in 2010 compared to 2 in 2009 followed by a decline to 4 in 2012. In Texas, the average annual number of outbreaks increased from 12 in 2005–2006 to 23 in 2007–2009, and then decreased to 8 in 2010–2012. In Vermont, the average annual number of outbreaks was relatively stable across the 3 time periods, with an average of 2–4 outbreaks reported per year.
Figure 1. Number of Varicella Outbreaks by Year, Data from 6 States, 2005–2012 (N=929 Outbreaks)a.
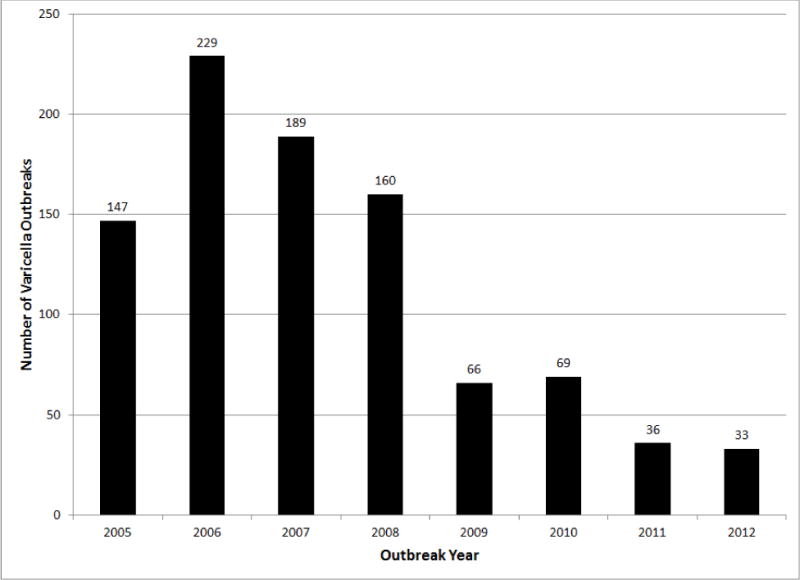
aData from Minnesota in 2005 was only available starting in September 2005.
There were a total of 1,015 varicella outbreaks involving 13,595 cases reported by the 9 states during 2005–2012, including the 929 outbreaks reported by the 6 states described above. The size and duration of outbreaks declined significantly over time (p<0.001). The median size of outbreaks was 12, 9, and 7 cases and the median duration of outbreaks was 38, 35, and 26 days during 2005–2006, 2007–2009, and 2010–2012 respectively. Among states with reporting of outbreaks with <5 cases, the proportion of outbreaks with <5 cases increased to 14.6% (25 outbreaks) in 2010–2012 from 1.6% (6 outbreaks) in 2005–2006 (Table 2). There were 2 large outbreaks with ≥51 cases reported in 2010–2012. One outbreak has been previously described14, involved 2 elementary schools and 60 vaccinated cases with 48% 1-dose cases and 52% 2-dose cases. The other large outbreak occurred in a K-8th grade school and involved 55 cases; information on vaccination status was available for 13% of cases, all of whom were vaccinated with 1-dose. The proportion of outbreaks that were laboratory confirmed increased to 16.4% in 2010–2012 from 0.3% in 2005–2006 (p<0.001).
Table 2.
Reported Varicella Outbreaks during 2005–2012, Data from 9 States: Selected Variables
| Variable | 2005–2006 | 2007–2009 | 2010–2012 | p-value for trend test | |||
|---|---|---|---|---|---|---|---|
|
| |||||||
| Varicella Outbreak Data (N=1,015 outbreaks) | |||||||
| Total # Outbreaks | 387 | 457 | 171 | ||||
| # | % | # | % | # | % | ||
| Settinga | |||||||
| Daycare | 7 | 1.9 | 8 | 1.9 | 7 | 4.1 | 0.0084b |
| School | 367 | 97.1 | 410 | 95.1 | 151 | 88.8 | 0.0014b |
| Otherd | 4 | 1.1 | 13 | 3.0 | 12 | 7.1 | <0.0001b |
| Totale | 378 | 97.7 | 431 | 94.3 | 170 | 99.4 | |
| Outbreak Size | |||||||
| <5 cases | 6 | 1.6 | 16 | 3.5 | 25 | 14.6 | <0.0001b |
| 5–9 cases | 142 | 36.7 | 223 | 48.8 | 87 | 50.9 | 0.0005b |
| 10–20 cases | 159 | 41.1 | 147 | 32.2 | 42 | 24.6 | 0.0001b |
| 21–50 cases | 73 | 18.9 | 63 | 13.8 | 15 | 8.8 | 0.0006b |
| ≥51 cases | 7 | 1.8 | 8 | 1.8 | 2 | 1.2 | 0.9713b |
| Totale | 387 | 100.0 | 457 | 100.0 | 171 | 100.0 | |
|
| |||||||
| Varicella Case Data (N=13,595 Cases) | |||||||
| Total # Cases | 5,812 | 6,020 | 1,763 | ||||
| # | % | # | % | # | % | ||
|
| |||||||
| Age (% among cases with non-missing data) (N=8,059 Cases) | |||||||
| <1 year | 5 | 0.2 | 26 | 0.8 | 16 | 0.9 | 0.0001c |
| 1–4 years | 93 | 3.2 | 126 | 3.7 | 115 | 6.7 | <0.0001b |
| 5–9 years | 2,187 | 75.5 | 2,276 | 66.0 | 774 | 45.2 | <0.0001b |
| 10–14 years | 589 | 20.3 | 961 | 27.9 | 669 | 39.1 | <0.0001b |
| 15–19 years | 16 | 0.6 | 41 | 1.2 | 63 | 3.7 | <0.0001b |
| ≥20 years | 7 | 0.2 | 20 | 0.6 | 75 | 4.4 | <0.0001b |
| Totale | 2,897 | 49.8 | 3,450 | 57.3 | 1,712 | 97.1 | |
| Vaccination Status (% among cases with non-missing data) (N=7,454 Cases) | |||||||
| Unvaccinatedf | 513 | 21.9 | 766 | 20.6 | 469 | 33.8 | <0.0001b |
| Vaccinatedf | 1,825 | 78.1 | 2,961 | 79.4 | 920 | 66.2 | <0.0001b |
| Totale | 2,338 | 40.2 | 3,727 | 61.9 | 1,389 | 78.8 | |
| Number Vaccine Doses (% among vaccinated cases) (N=3,850 Cases) | |||||||
| 1-dose | 1,077 | 59.0 | 1,838 | 62.1 | 613 | 66.6 | 0.3588b |
| 2-dose | 1 | 0.1 | 97 | 3.3 | 224 | 24.3 | <0.0001b |
| Totalg | 1,078 | 59.1 | 1,935 | 65.3 | 837 | 91.0 | |
Information on outbreak setting missing for 36 outbreaks.
Cochrane Armitage Trend test used.
Exact Cochrane Armitage Trend test used.
Other settings include community, correctional facilities, healthcare facilities, and universities.
Percentages calculated out of total number of reported outbreaks or cases by study period.
We excluded those with prior varicella disease if information was available on prior disease history.
Percentages calculated out of total reported number of vaccinated cases by study period.
Information on outbreak setting was available for 96% of outbreaks. The majority of outbreaks were reported from schools, although the proportion of outbreaks occurring in schools was slightly lower in 2010–2012 compared to 2005–2006 (89% versus 97%). There were 928 school-associated outbreaks involving 12,334 varicella cases. The median duration of these outbreaks was 34 days (range, 0–206 days) and median size was 10 cases (range, 3–131 cases). The number of outbreaks reported from schools declined from 138 in 2005 to 39 in 2012 (p=0.0001). Overall, 76% (4,938/6,522) of varicella cases with information on vaccination status were vaccinated. Among these 4,938 vaccinated cases, 57% were 1-dose vaccinees and 6% were 2-dose vaccinees. There were 31 (3%) school-associated outbreaks with laboratory confirmation.
Completeness of information on age of outbreak-related cases increased from 50% (2,897/5,812) in 2005–2006 to 97% (1,712/1,763) in 2010–2012. Although the majority of outbreak-related cases occurred among 5–9 year olds, the proportion of cases in this age group declined from 76% of outbreak-related cases during 2005–2006, to 45% during 2010–2012 (Table 1). There was a corresponding increase in the proportion of cases reported among children <5 and ≥10 years of age.
Completeness of vaccination information on cases increased over time. Information on vaccination status was available for 40% of cases (2,338/5812) in 2005–2006 increasing to 79% (1,389/1,763) in 2010–2012. Information on number of vaccine doses received was available for 59% (1,078/1,825) of vaccinated cases in 2005–2006 and rose to 91% (837/920) in 2010–2012. We analyzed a subset of data in 2010–2012 with information on the vaccination status for the majority of the cases. There were 121 outbreaks in 2010–2012 for which vaccination status was available for ≥75% of cases. Among these 121 outbreaks, 68 (56%) outbreaks involved ≤30% unvaccinated cases, 37 (31%) involved 31–89% unvaccinated cases, and 16 (13%) involved ≥90% unvaccinated cases. Among the 16 outbreaks involving ≥90% unvaccinated cases, 11 occurred in schools, 2 in daycares, and 3 in other settings. The median size of these outbreaks was 6 cases (range, 3–28 cases), and the median duration was 22 days (range, 3–105 days). The median proportion of unvaccinated cases was 100% (range, 94%–100%).
Discussion
The number of varicella outbreaks in the 6 states with data for all years of the study period (California, Maryland, Minnesota, Texas, Vermont, and West Virginia) decreased by nearly 80% during the first 6 years since implementation of a recommendation for a routine 2-dose varicella vaccination program. We also observed declines in the size and duration of outbreaks. These data corroborate what has been previously reported from an active surveillance site and one state shortly after implementation of the 2-dose program. In an active surveillance site in California, varicella outbreaks declined 75% in 2007–2010 compared with 2003–200611. In a report from Connecticut, the number and size of school outbreaks decreased from 42 in 2005–2006 to 2 outbreaks in 2008–2009, with the average outbreak size decreasing from 14 to 5 varicella cases12. The declines in varicella outbreaks, as well as declines in varicella incidence11, 12, have occurred as 2-dose varicella vaccination coverage has rapidly increased. Two-dose coverage among 7 year-old children increased from <10% in 2006 to >80% in 201215 and reached 94% among Kindergartners in the 2012–2013 school year16; 2-dose varicella vaccine coverage among adolescents approached 75% in 201217. The number of states with a 2-dose varicella vaccination school entry requirement for Kindergarten increased from 4 (8%) states in 2007 to 36 (71%) in 201215. Although these decreases in varicella outbreaks were noted before many of these states implemented 2-dose varicella vaccine requirements for school entry, requirements are important for maintaining high vaccine coverage, which is critical for preventing or curtailing outbreaks.
During the study period, the proportion of cases among children aged < 5 and ≥10 years increased and may be related to lower 2-dose varicella vaccination coverage in these age groups since the routine 2nd dose is recommended for children aged 4–6 years and the majority of school requirements are targeted for Kindergarten school-entry. We did see a slight increase in the proportion of outbreaks occurring among daycares and in settings other than schools during the study period, including adult facilities such as correctional and healthcare facilities, although the proportion of outbreaks occurring in these settings remained small compared to outbreaks reported in schools. There is likely under-reporting of varicella outbreaks in these other settings because the primary reporting source for outbreak surveillance is schools. In settings at increased risk of VZV transmission and varicella outbreaks, strategies for preventing outbreaks may include surveillance, assessment and documentation of evidence of immunity to VZV1 in exposed persons, and vaccination of susceptible persons with 2-doses of varicella vaccine.
We found that the majority of varicella outbreaks continued to occur in elementary and middle schools and among vaccinated children 5–14 years of age. However, we also saw an increase in the proportion of outbreak-related cases in unvaccinated children. Of the 121 reported outbreaks during 2010–2012 with complete information on vaccination status of cases, 16 predominantly involved unvaccinated individuals. Although varicella vaccine exemption rates are low nationally (1.8%)16, clusters of vaccine exemptors exist. Some of the outbreaks with high proportions of unvaccinated cases occurred in schools or communities where vaccine hesitancy is common, but others were reported from schools with high vaccine coverage that may have been driven by multiple cases within a small number of families who were vaccine exemptors. Rates of non-medical vaccine exemption are rising, particularly in states that allow for philosophical exemptions18, 19. These growing pockets of susceptible individuals fuel disease transmission and lead to outbreaks with possibly longer sustained transmission that may result in severe consequences20.
Although varicella outbreaks have declined during the 2-dose varicella vaccine era, they continue to pose a challenge to manage and control14, 21. Outbreaks continue to occur mainly among vaccinated persons, in whom disease can be modified, mild, and difficult to diagnose clinically. It is not clear if there are differences in clinical severity between varicella cases who previously received 1-dose of varicella vaccine compared to those who received 2-doses, although studies of medically attended varicella have reported no significant differences11, 14, 21. It is also unknown whether the contagiousness differs between 1-dose versus 2-dose vaccinated cases, although it seems plausible that the number of lesions would play a role. Nevertheless, because 2-dose vaccinated cases are a potential source of infection, health departments need to continue monitoring varicella cases reported among 1 and 2-dose vaccine recipients and ensure that control measures are implemented as soon as possible to prevent further disease transmission. Better laboratory diagnostics for confirming breakthrough varicella cases are also needed.
There were several limitations to this analysis. The analysis was based on aggregate data and we did not have case-based data on the outbreak-related cases. We were unable to look at individual characteristics of the cases, and thus unable to describe the age distribution or disease severity by vaccination status. Although data on age and vaccination status were missing for a significant proportion of the cases (40% for age and 45% for vaccination status), completeness for these variables significantly improved over time, from 50% to 97% for age and 40% to 79% for vaccination status. Information on lesion severity was collected, but was not reported in this manuscript since information was missing for 90% of cases. Completeness of reporting for outbreak-related variables may continue to improve as the number of outbreaks decline over time and an increased number of states conduct case-based varicella surveillance. Much progress has been made in expanding national varicella surveillance in the United States with varicella now reportable in 44 out of 51 jurisdictions (50 states and DC) as of 201222.
In conclusion, the routine 2-dose varicella vaccination program appears to have significantly reduced the number, size, and duration of varicella outbreaks in the U.S. Ongoing surveillance is important to continue monitoring the impact of the varicella vaccination program and the epidemiology of varicella outbreaks to better target control and prevention strategies. CDC encourages state health departments to report annual varicella outbreak data to CDC using this form: http://www.cdc.gov/chickenpox/outbreaks/downloads/appx-a-vor-wksht.pdf. With additional increases in 2-dose varicella vaccination coverage and implementation of 2-dose school entry requirements, varicella incidence and outbreaks in the U.S. should continue to decrease.
Supplementary Material
Acknowledgments
We would like to thank state and local health departments for their invaluable work in conducting outbreak surveillance. We would also like to thank Craig Hales for his technical assistance in analyzing the data.
Source of Funding: TW was funded in part by the Federal 317 Immunization Grant Program. VB was funded in part by an Epidemiology and Laboratory Capacity (ELC) grant from CDC. CT and MDR were funded in part by American Recovery and Reinvestment Act (ARRA) funding. For the remaining others, no sources of funding were declared.
Footnotes
Disclaimer: The findings and conclusions in this report are those of the authors and do not necessarily represent the official position of the Centers for Disease Control and Prevention, US Department of Health and Human Services.
Conflicts of Interest: There were no conflicts of interest declared.
References
- 1.Marin M, Guris D, Chaves SS, Schmid S, Seward JF. Prevention of varicella: recommendations of the Advisory Committee on Immunization Practices (ACIP) MMWR Recomm Rep. 2007;56:1–40. [PubMed] [Google Scholar]
- 2.Lopez AS, Zhang J, Brown C, Bialek S. Varicella-related hospitalizations in the United States, 2000–2006: the 1-dose varicella vaccination era. Pediatrics. 2011;127:238–245. doi: 10.1542/peds.2010-0962. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Marin M, Meissner HC, Seward JF. Varicella prevention in the United States: a review of successes and challenges. Pediatrics. 2008;122:e744–751. doi: 10.1542/peds.2008-0567. [DOI] [PubMed] [Google Scholar]
- 4.Marin M, Zhang JX, Seward JF. Near elimination of varicella deaths in the US after implementation of the vaccination program. Pediatrics. 2011;128:214–220. doi: 10.1542/peds.2010-3385. [DOI] [PubMed] [Google Scholar]
- 5.Chaves SS, Zhang J, Civen R, Watson BM, Carbajal T, Perella D, et al. Varicella disease among vaccinated persons: clinical and epidemiological characteristics, 1997–2005. J Infect Dis. 2008;197(Suppl 2):S127–131. doi: 10.1086/522150. [DOI] [PubMed] [Google Scholar]
- 6.Shapiro ED, Vazquez M, Esposito D, Holabird N, Steinberg SP, Dziura J, et al. Effectiveness of 2 doses of varicella vaccine in children. J Infect Dis. 2011;203:312–315. doi: 10.1093/infdis/jiq052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kuter B, Matthews H, Shinefield H, Black S, Dennehy P, Watson B, et al. Ten year follow-up of healthy children who received one or two injections of varicella vaccine. Pediatr Infect Dis J. 2004;23:132–137. doi: 10.1097/01.inf.0000109287.97518.67. [DOI] [PubMed] [Google Scholar]
- 8.Thomas SL, Minassian C, Ganesan V, Langan SM, Smeeth L. Chickenpox and risk of stroke: a self-controlled case series analysis. Clin Infect Dis. 2014;58:61–68. doi: 10.1093/cid/cit659. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.World Health Organization. Varicella and herpes zoster vaccines: WHO position paper. 2014 Jun; Available at: http://www.who.int/entity/wer/2014/wer8925.pdf?ua=1. Accessed February 4, 2015.
- 10.Baxter R, Tran TN, Ray P, Lewis E, Fireman B, Black S, et al. Impact of vaccination on the epidemiology of varicella: 1995–2009. Pediatrics. 2014;134:24–30. doi: 10.1542/peds.2013-4251. [DOI] [PubMed] [Google Scholar]
- 11.Bialek SR, Perella D, Zhang J, Mascola L, Viner K, Jackson C, et al. Impact of a routine two-dose varicella vaccination program on varicella epidemiology. Pediatrics. 2013;132:e1134–1140. doi: 10.1542/peds.2013-0863. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kattan JA, Sosa LE, Bohnwagner HD, Hadler JL. Impact of 2-dose vaccination on varicella epidemiology: Connecticut–2005–2008. J Infect Dis. 2011;203:509–512. doi: 10.1093/infdis/jiq081. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Singleton RJ, Holman RC, Person MK, Steiner CA, Redd JT, Hennessy TW, et al. Impact of varicella vaccination on varicella-related hospitalizations among American Indian/Alaska Native people. Pediatr Infect Dis J. 2014;33:276–279. doi: 10.1097/INF.0000000000000100. [DOI] [PubMed] [Google Scholar]
- 14.Mahamud A, Wiseman R, Grytdal S, Basham C, Asghar J, Dang T, et al. Challenges in confirming a varicella outbreak in the two-dose vaccine era. Vaccine. 2012;30:6935–6939. doi: 10.1016/j.vaccine.2012.07.076. [DOI] [PubMed] [Google Scholar]
- 15.Lopez AS, Cardemil C, Pabst LJ, Cullen KA, Leung J, Bialek SR. Two-Dose Varicella Vaccination Coverage Among Children Aged 7 years – Six Sentinel Sites, United States, 2006–2012. MMWR Morb Mortal Wkly Rep. 2014;63:174–177. [PMC free article] [PubMed] [Google Scholar]
- 16.Vaccination coverage among children in kindergarten – United States, 2012–13 school year. MMWR Morb Mortal Wkly Rep. 2013;62:607–612. [PMC free article] [PubMed] [Google Scholar]
- 17.National and state vaccination coverage among adolescents aged 13–17 years–United States, 2012. MMWR Morb Mortal Wkly Rep. 2013;62:685–693. [PMC free article] [PubMed] [Google Scholar]
- 18.Constable C, Blank NR, Caplan AL. Rising rates of vaccine exemptions: Problems with current policy and more promising remedies. Vaccine. 2014;32:1793–1797. doi: 10.1016/j.vaccine.2014.01.085. [DOI] [PubMed] [Google Scholar]
- 19.Omer SB, Richards JL, Ward M, Bednarczyk RA. Vaccination policies and rates of exemption from immunization, 2005–2011. N Engl J Med. 2012;367:1170–1171. doi: 10.1056/NEJMc1209037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Varicella death of an unvaccinated, previously healthy adolescent–Ohio, 2009. MMWR Morb Mortal Wkly Rep. 2013;62:261–263. [PMC free article] [PubMed] [Google Scholar]
- 21.Gould PL, Leung J, Scott C, Schmid DS, Deng H, Lopez A, et al. An outbreak of varicella in elementary school children with two-dose varicella vaccine recipients–Arkansas, 2006. Pediatr Infect Dis J. 2009;28:678–681. doi: 10.1097/INF.0b013e31819c1041. [DOI] [PubMed] [Google Scholar]
- 22.Lopez AS, Lichtenstein M, Schmid SD, Bialek S. Assessment of varicella surveillance and outbreak control practices – United States, 2012. MMWR Morb Mortal Wkly Rep. 2014;63:785–788. [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


