Abstract
Objective
The National Institute for Occupational Safety and Health (NIOSH) Revised Lifting Equation (RNLE) was adapted to derive recommended weight limits (RWLs) for pregnant workers and to develop corresponding guidelines for clinicians.
Background
In the past three decades there has been a large increase in the number of women employed outside the home and remaining in the workforce during pregnancy. Practical authoritative guidelines based on accumulated evidence are needed to inform allowable work activity levels for healthy pregnant workers.
Method
Empirically based lifting criteria established by NIOSH to reduce the risk of overexertion injuries in the general U.S. working population were evaluated for application to pregnant workers. Our evaluation included an extensive review of the literature linking occupational lifting to maternal and fetal health. Decision logic and supporting literature are presented, along with computational details.
Results
Provisional RWLs for pregnant workers were derived from the RNLE, along with guidelines for clinicians. The guidelines advise against pregnant workers lifting below midshin and overhead.
Conclusion
Based on our review of the available evidence, we present lifting thresholds that most pregnant workers with uncomplicated pregnancies should be able to perform without increased risk of adverse maternal and fetal health consequences. Except for restrictions involving lifting from the floor and overhead, the provisional guidelines presented are compatible with NIOSH lifting recommendations adopted in the early 1990s for the general working population.
Application
Implementation of these provisional guidelines could protect millions of female workers in the work-place from fetal and maternal lifting-related health problems.
Keywords: manual lifting, occupational hazard, pregnancy, recommendations
BACKGROUND
Repetitive manual lifting of objects and materials is a major concern in numerous work sectors that employ large numbers of reproductive age women, including health care, retail, manufacturing, and the armed services. Historically, occupational low-back pain (LBP) is one of the leading health complaints for workers engaged in manual lifting, and LBP is responsible for numerous lost workdays and high costs to industry (Marras, 2008). There is a special concern, however, about potential maternal and fetal health effects associated with excessive manual lifting for women during pregnancy. In 1993, the National Institute for Occupational Safety and Health (NIOSH) published the Revised NIOSH Lifting Equation (RNLE), an assessment tool for estimating recommended weight limits (RWLs) for two-handed manual lifting (Waters, Putz-Anderson, & Garg, 1994; Waters, Putz-Anderson, Garg, & Fine, 1993). The a task-specific RWL that accounts for six specific variables considered important in determining how much weight is safe to manually lift for nearly all workers. Task conditions that affect the magnitude of the maximum RWL for manual lifting include the horizontal distance of the load from the spine, the vertical height of the hands from the floor, the frequency and duration of lifting exposure, the asymmetric nature of a lift, and the quality of object coupling. The RNLE, an assessment tool designed to reduce risk of overexertion injuries in the general U.S. working population, has been widely adopted internationally as a basis for recommending maximum weight limits for the past two decades (Colombini, Occhipinti, Alvarez-Casado, & Waters, 2012). This paper describes application of the RNLE in deriving maximum RWLs for healthy workers with uncomplicated pregnancies and in the development of provisional clinical guidelines. We describe how to apply these guidelines in a clinical setting in a companion paper by MacDonald et al. (2013).
EXISTING WEIGHT LIMITS FOR OCCUPATIONAL LIFTING DURING PREGNANCY
For the past 29 years, clinical management of pregnant workers for physical job activities has relied on the American Medical Association’s (AMA) Council on Scientific Affairs published guidance on the effects of pregnancy on work performance (AMA, 1984). Evidence suggests that these guidelines continue to inform physician practice and workplace policy (Pompeii, Evenson, & Delclos, 2011; U.S. Navy and Marine Corps Public Health Center, 2010). The AMA guidelines define permissible weight limits “that healthy employees with normal uncomplicated pregnancies should be able to perform . . . without undue difficulty or risk to the pregnancy.” These weight limits are shown in Table 1 and are summarized as follows:
TABLE 1.
American Medical Association (AMA) Weight Limits for Occupational Lifting During Pregnancy
| Intermittent Liftinga
|
Repetitivea
|
|||
|---|---|---|---|---|
| Week of Gestation | Metric | U.S. Customary | Metric | U.S. Customary |
| 20 | >23 kg | >51 lbs | ||
| 24 | 11–23 kg | 24–51 lbs | ||
| 30 | >23 kg | >51 lbs | ||
| 40 | <14 kg | <31 lbs | <11 kg | <24 lbs |
Source. AMA (1984).
The terms intermittent and repetitive were not defined in the AMA guidance. Also, the AMA guidelines do not differentiate weight limits with regard to duration of exposure.
Lifting more than 23 kg (51 lbs) is permitted repetitively for the first half of pregnancy (up to Week 20) and intermittently through Week 30.
Between Weeks 20 and 24, repetitive lifting up to 23 kg (51 lbs) is permitted. A weight limit of 11 kg (24 lbs) is specified after Week 24.
After Week 30, intermittent lifting up to 11 kg (24 lbs) is permitted.
The AMA guidelines do not account for a number of task conditions currently considered important in determining RWLs for manual lifting. These task conditions include the horizontal reach distance, vertical height of the lift, asymmetry (rotation of the spine), duration of lifting, and the nature of the hand-to-object coupling. Comparison of the maximum weight limits in the AMA guideline to those derived from the RNLE for ideal lifting conditions (i.e., short duration lifts close to and in front of the body at about waist height) indicates that the AMA recommended values are substantially higher than those derived from the NIOSH RNLE. The difference in RWL is more pronounced when considering the nonideal lifting conditions that exist in many workplaces and the increased horizontal reach distance imposed by increased abdominal girth in the later stages of pregnancy. In response to concern that pregnant workers may not be sufficiently protected from risk of overexertion injuries and other health hazards, we conducted an extensive literature review and propose recommended clinical guidelines derived from the RNLE, taking into account anatomic changes in pregnancy that have a direct impact on horizontal reach distances and empirical evidence linking occupational lifting to maternal and fetal health.
BIOMECHANICAL CONSIDERATIONS FOR MANUAL LIFTING DURING PREGNANCY
From a biomechanical perspective, some of the more important changes that occur during pregnancy include (a) changes in anthropometric characteristics (increase in overall mass of the body and in particular the upper body, changes in the location of the center of mass, increased abdominal girth, and changes in spinal curvature during pregnancy), (b) increased joint laxity and potential spinal instability, and (c) changes in balance control.
A pregnancy-related musculoskeletal risk model by Paul, van Dijk, and Frings-Dresen (1994) calls attention to increased load on the musculoskeletal system due to increased abdominal mass and change in the center of mass. Independent of external loading conditions, as the weight of the upper body increases, the magnitude of compression and shear force created at the spinal joints during a forward bending motion also increases, thereby increasing risk of damage to the spinal discs. Also, as a pregnancy progresses, the location of the center of mass (COM) of the upper body moves upward and away from the L5/S1 joint (Whitcome, Shapiro, & Lieberman, 2007). This change in COM results in an increase in the length of the moment arm through which the mass of the upper body acts during forward flexion, such as when lifting from below midthigh. This increased moment arm coupled with increased mass of the upper body in the later stages of pregnancy would further increase spinal loading. These loading considerations are especially important when lifting loads from below the waist, when the entire weight of the upper body must be lifted in addition to the weight of the external load.
Another important consideration for spinal loading involves the location of the external load in front of the body. The minimum horizontal distance for the hands in front of the spine during manual lifting is 25 cm (10 in.), as defined by the RNLE (Waters et al., 1993; Waters et al., 1994). This distance assumes that lifts can be performed freely in front of the body without interference from the abdomen. Anthropometric data from pregnant U.S. women showed that increases in abdominal depth range on average from 4.2 cm (1.7 in.) at 20 weeks to 12.0 cm (4.7 in.) at 37 to 38 weeks (Perkins & Blackwell, 1998). Correspondingly, as abdominal girth increases during pregnancy, the minimum horizontal distance of the hands from the spine increases from 25 cm (10 in.), the RNLE-defined minimum, to 30 cm (12 in.) at 20 weeks gestation, and 38 cm (15 in.) at 37 to 38 weeks of gestation, proportionally increasing spinal loading.
Curvature of the lower spine is a critical factor in stabilizing whole body posture by positioning the upper body’s COM over the hips, and evidence suggests that curvature of the spine varies with pregnancy as part of a complex set of adaptive responses (Whitcome et al., 2007). Gross postural adaption is evident in several prospective study findings involving standing tasks in advanced pregnancy, compared with early pregnancy and nonpregnant controls (Paul & Frings-Dresen, 1991, 1994; Poole, 1998); and advanced pregnancy is associated with increased anteroposterior postural sway (Oliveira, Vieira, Macedo, Simpson, & Nadal, 2009). These increased demands for maintenance of postural control likely increases risk of muscular fatigue, and may account for why pregnant women report difficulty performing work overhead, bending forward, and picking up objects from the floor (Cheng et al., 2006; Nicholls & Grieve, 1992). Difficulty in maintaining postural stability in later stages of pregnancy is attributed to increased risk of slips and falls, increasing risk of acute injury (Dunning, LeMasters, & Bhattacharya, 2010; Fries & Hellebrandt, 1943).
In addition, pregnancy is known to induce ligamentous laxity, a condition involving increased mobility of the joints to aid delivery (Calguneri, Bird, & Wright, 1982; Schauberger et al., 1996). A model by Paul et al. hypothesizes that pregnancy-related musculoskeletal problems arise, at least in part, from reduced load-bearing capacity associated with laxity (Paul et al., 1994). Laxity presents early in pregnancy and persists beyond 6 weeks postpartum (Schauberger et al., 1996). The associated reduction in ligament rigidity is believed to weaken joint stability, which would place greater demand on stabilizing muscles (Granata & Marras, 2000). Many researchers have identified laxity as a contributing factor in pregnancy-related pelvic girdle pain (Damen et al., 2001; Larsen et al., 2013; Mens, Pool-Goudzwaard, & Stam, 2009), LBP (Colliton, 1999), and knee pain (Blecher & Richmond, 1998; Charlton, Coslett-Charlton, & Ciccotti, 2001; Dumas & Reid, 1997; Marnach et al., 2003; Schauberger et al., 1996; van Lunen, Roberts, Branch, & Dowling, 2003).
NIOSH RWL
The RNLE is an ergonomic job analysis method for systematically evaluating the physical demands of manual handling tasks and computing an RWL (Waters et al., 1993; Waters et al., 1994). The RWL is the weight of the load that nearly all healthy workers could perform over a substantial period of time (e.g., up to 8 hr) without an increased risk of developing lifting-related LBP. By “healthy workers,” NIOSH means workers who are free of adverse health conditions that would increase their risk of musculoskeletal injury. According to the authors of the RNLE, the RWL provides weight limits acceptable to 90% of healthy females (Waters et al., 1993, p. 761, Table 5).
TABLE 5.
Provisional Recommended Weight Limit (RWL) Values (pounds) for the Clinical Guidelines
| Infrequent Lifting | Repetitive Short Duration | Repetitive Long Duration | |||||||
|---|---|---|---|---|---|---|---|---|---|
|
|
|||||||||
| Vertical Zone | Closea | Medium | Extended | Closea | Medium | Extended | Closea | Medium | Extended |
| Shoulder | 30 | 21 | 17 | 25 | 18 | 14 | 15 | 10 | 9 |
| Waist | 36 | 26 | 20 | 30 | 22 | 17 | 18 | 13 | 10 |
| Knee | 32 | 23 | 18 | 27 | 20 | 16 | 16 | 11 | 9 |
RWL values in the “close” lifting zone are not applicable at 20 weeks gestation or more.
The RNLE starts with a recommended weight (or load constant) that is considered safe for an “ideal” lift and then reduces that weight as task conditions become less favorable. The RWL is computed from a multiplicative model (see the following equation) that provides a weighting (multiplier) for each of six measured task variables. The measured task variables include the (a) horizontal distance of the load from the worker (H); (b) vertical height of the lift (V); (c) vertical displacement during the lift (D); (d) angle of asymmetry, in degrees (A); (e) frequency (F) and duration of lifting; and (f) quality of the hand-to-object coupling (C). These task measurements serve as inputs for deriving “multipliers” that are coefficients or weighting factors having a maximum value of 1, which reduce the maximum recommended load weight (51 lbs) when task conditions deviate from ideal. Multipliers can be computed using prescribed algorithms or determined from look-up tables in the RNLE Applications Manual (Waters et al., 1994), which is accessible from the NIOSH website at http://www.cdc.gov/niosh/docs/94-110/. The RNLE RWL equation is defined as follows:
Where:
| Metric | U.S. Customary | |
|---|---|---|
| LC = Load Constant = | 23 kg | 51 lb |
| HM = Horizontal Multiplier = | (25/H) | (10/H) |
| VM = Vertical Multiplier = | 1−(.003|V−75|) | 1−(.0075 |V−30|) |
| DM = Distance Multiplier = | .82 + (4.5/D) | .82 + (1.8/D) |
| AM = Asymmetric Multiplier = | 1−(.0032A) | 1−(.0032A) |
| FM = Frequency Multiplier = | From FM tablea | From FM tablea |
| CM = Coupling Multiplier = | From CM tablea | From CM tablea |
The FM and CM tables are listed as Tables 5 and 7, respectively, in the NIOSH Applications Manual for the Revised NIOSH Lifting Equation (Waters et al., 1994).
PROVISIONAL RNLE-BASED RWLS FOR MANUAL LIFTING DURING PREGNANCY
Motivated by the need for practical, evidence-based weight limits to aid clinical decision making for manual lifting during pregnancy, the RNLE was applied to define provisional RWLs for a range of lifting requirements, supplemented by considerations of scientific evidence linking occupational lifting and maternal and fetal health. To help ensure that the provisional guidelines would be practical and feasible to be implemented in a clinical setting, the following simplifying assumptions were made: Task parameters assumed to be “ideal” were the travel distance of the load, symmetry of the load, and good hand coupling of the object. Correspondingly, the proposed clinical guidelines assume that the vertical travel distance of the object being lifted is small, the lift can be performed without significant twisting of the spine (i.e., no more than 15° asymmetry), and the object being lifted has handles or handhold cutouts of optimal design. The multipliers for distance (D), asymmetry (A), and coupling (C) were accordingly assigned a value of 1. All remaining RNLE task parameters were considered in a multistep process that entailed defining the work space or “lifting zones,” defining task frequency and duration patterns, and then applying anatomical and other evidence-based considerations associated with lifting while pregnant.
Nine “lifting zones” were defined to signify the workspace in front of the body where lifting tasks are to be performed. The lifting zones were specified by dividing the horizontal (H) distance in front of the body into three nearly equal categories (12 < H ≤ 15 in.; 15 < H ≤ 20 in.; and 20 < H ≤ 25 in.) and vertical height into three categories according to anatomical reference points (shoulder, knuckle, and tibia). The minimum horizontal value was 10 in. for body clearance. Using the maximum horizontal distance for each of the three forward reach categories (i.e., 15, 20, and 25 in.), horizontal multipliers (HMs) were computed in accordance with the standard algorithm for the computation of HMs shown earlier; the resulting HM coefficient values are shown in Table 2. Vertical height values for shoulder, knuckle, and tibia locations were derived from reports of average U.S. female anthropometry and defined to be 132 cm (52 in.), 71 cm (28 in.), and 43 cm (17 in.), respectively (Chengalur, Rodgers, & Bernard, 2004); these vertical heights were used to compute the corresponding vertical multiplier (VM) according to the standard algorithm (Table 3).
TABLE 2.
Horizontal Multiplier (HM) Values for Three Horizontal Reach Distances
| Horizontal Reach | Close, 12–15 Inches | Medium, 15–20 Inches | Extended, 20–25 Inches |
|---|---|---|---|
| HM value | 0.7 | 0.5 | 0.4 |
TABLE 3.
Vertical Multiplier (VM) Values for Three Vertical Height Categories
| Anatomical Landmarks | Vertical Height (inches) | VM |
|---|---|---|
| Shoulder | 52 | 0.83 |
| Knuckle | 28 | 1.00 |
| Tibia | 17 | 0.90 |
To help ensure that the provisional clinical guidelines are applicable across a wide range of jobs, we defined the following three frequency and duration patterns: infrequent lifting, repetitive short duration lifting, and repetitive long duration lifting. The infrequent lifting pattern was defined as occurring less than 0.2 lifts per minute, which is equivalent to one lift every 5 min. The repetitive short duration lifting pattern was defined as a lifting frequency greater than 1 every 5 min but less than 3 per minute and having a continuous duration less than 1 hr. The repetitive long duration lifting pattern was defined as a lifting frequency greater than 1 every 5 min but less than 3 per minute and a continuous duration greater than 1 hr but not more than 8 hr. Short duration lifting can encompass multiple hours of lifting per day; however, each continuous lifting period should be less than 1 hr and be followed by a minimum of 1 hr of nonlifting activity before the next continuous lifting period is initiated. If short duration lifting activities are not followed by at least 1 hr of non-lifting activity, or if lifting occurs an hour or more per day, repetitive long duration lifting should be selected. The frequency multipliers that correspond to these patterns were derived from look-up tables in the RNLE Applications Manual (Waters et al., 1994) and are reported in Table 4.
TABLE 4.
Frequency Multiplier (FM) Values for Three Frequency-Duration Patterns
| Infrequent | Repetitive Short Duration | Repetitive Long Duration | |
|---|---|---|---|
| Frequency value | 1.0 | 0.85 | 0.50 |
The RWL for the provisional clinical guidelines was then computed as the load constant (51 lbs) multiplied by the HM, VM, and FM coefficients (Table 5). These RWL values reflect the maximum recommended weight for the associated task conditions. For each frequency-duration pattern, lifting in the area defined as “close” to the body and “waist” height yields the highest RWL, whereas an “extended” lift above shoulder height yields the lowest RWL. Task conditions assumed to be “ideal” (i.e., vertical displacement distance, asymmetric angle, and quality of hand-to-object coupling) would have multiplier values of 1, thus having no influence on the RWL values. In a workplace setting, where task parameters can be directly measured, we propose applying the full RNLE and computing RWLs to ensure that all task variables are fully considered. Of importance, because abdominal extension in the second half of pregnancy increases the horizontal load distance, RWLs derived in the first half of pregnancy likely would not be sufficiently protective. For this reason, we propose reanalysis of pregnant workers’ lifting tasks at least once in the second half of pregnancy.
PREGNANCY CONSIDERATIONS
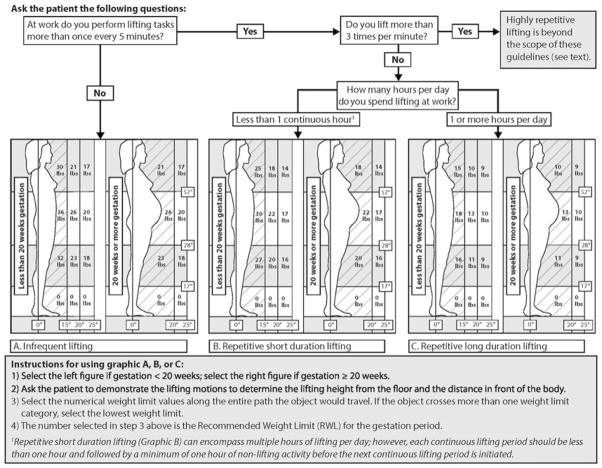
After computing RWLs for the “lifting zone” and frequency and duration task parameters described earlier, we applied anatomical and other evidence-based considerations associated with lifting while pregnant. The task parameter most directly influenced during the second half of pregnancy is the minimum horizontal lifting distance. Anthropometric data on pregnant civilian and uniformed service women collected for the U.S. Air Force were used to estimate the minimum horizontal distance by gestation period (Figure 1; Perkins & Blackwell, 1998). At 20 weeks gestation, abdominal depth increases approximately 5 cm or about 2 in.; as pregnancy advanced to near full term (37–38 weeks), abdominal depth increases almost 14 cm or 5.5 in. Accordingly, objects lifted in the later stages of pregnancy will be located farther from the spine, resulting in a larger horizontal moment arm, thereby increasing spinal loading. Since increased abdominal depth in the second half of pregnancy effectively prevents lifting within the “close” or most proximal lifting zone defined earlier, RWLs applied in the second half of pregnancy are based on the “medium” and “extended” reach zones only.
Figure 1.
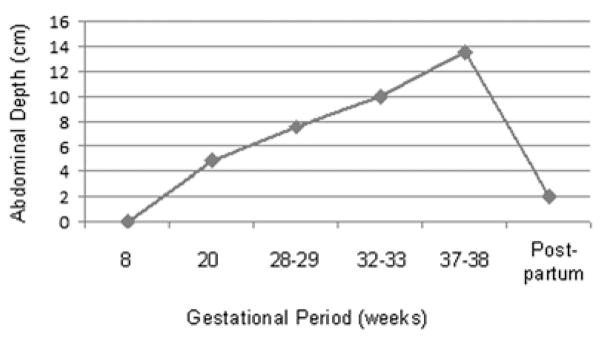
Abdominal depth (cm) in the horizontal plane as a function of gestation period.
Source. Perkins and Blackwell (1998).
Other evidence-based considerations associated with lifting while pregnant include maternal and fetal health concerns associated with lifting that occurs at the postural extremes, such as lifting from the floor or lifting overhead. Accordingly, our clinical guidelines propose no lifting/ lowering from the floor with hands below mid-shin or lifting/lowering with the hands overhead. Mechanical compression, altered venous tone, and poor venous return from the lower extremities may be exacerbated by constrained postural demands (e.g., prolonged standing, stooping), inducing conditions of fetal hypoxia (Spinillo et al., 1996; Sternfeld, 1997) and LBP (Noon & Hoch, 2012). Frequent or prolonged torso flexion is a significant risk factor for back injury (Punnett, Fine, Keyserling, Herrin, & Chaffin, 1991; Vandergrift, Gold, Hanlon, & Punnett, 2012), causing the American Conference of Governmental Industrial Hygienists (ACGIH) to set a Lifting Threshold Limit Value of zero for most lifting from the floor (ACGIH, 2012). Survey results show that a significant majority of pregnant women report difficulty performing work overhead, bending forward, and picking up objects from the floor in the later stages of pregnancy (Cheng et al., 2009; Nicholls & Grieve, 1992). In addition, Bonzini et al. (2009) and Florack, Zielhuis, Pellegrino, and Rolland (1993) each reported nearly a threefold increased risk of preterm labor and spontaneous abortion, respectively, for women whose job required bending at the waist more than 1 hr per day. We further propose no overhead lifting due to increased risk of postural instability shown to occur in conjunction with changes in the COM with increased gestation (Dunning et al., 2010; Fries & Hellebrandt, 1943) and increased antero-posterior postural sway (Oliveira et al., 2009).
A graphically based version of the provisional clinical guidelines that incorporates the tabulated RWL results with the aforementioned pregnancy considerations is shown in Figure 2. The three frequency-duration lifting patterns comprise Graphics A (infrequent lifting), B (repetitive short duration lifting), and C (repetitive long duration lifting). For each of the three graphics, provisional RWLs from Table 5 for the close, medium, and extended reach lift are shown for the image associated with the first half of pregnancy (less than 20 weeks gestation). In the second half of pregnancy, the “close” lifting zone is essentially obstructed, leaving RWLs for the “medium” and extended reach lift zones. Provisional RWL values of zero, indicating a lifting restriction, are shown for lifting/lowering below midshin. Although not shown, RWL values of zero also apply to lifting overhead. Details on how to apply these guidelines in a clinical setting are available in a companion paper (MacDonald et al., 2013).
Figure 2.
Recommended weight limits in early and late pregnancy for three lift frequency patterns.
RNLE TASK CONDITION RESTRICTIONS
Lifting task condition restrictions of the original RNLE would apply to these provisional clinical guidelines. The restrictions, summarized in Table 6, are work conditions in which application of the RNLE could underestimate the magnitude of physical stress associated with a particular lift (e.g., one-handed lifting, lifting more than 8 hr per day, lifting unstable loads). This list is supplemented by additional lifting condition restrictions associated with application of the clinical guidelines, shown in parentheses in the table. These include lifting/lowering below midshin and lifting overhead, very high frequency lifting (i.e., occurring more than 3 times per minute), lift travel distance greater than 10 in., spinal rotation of 15° or more, and poor hand coupling.
TABLE 6.
Work Conditions Not Covered by the NIOSH RNLE (and the Provisional Clinical Guidelines)
|
When lifting frequency exceeds 3 lifts per minute or when the simplifying assumptions applied in generating the RWLs for the clinical guidelines are violated, we recommend that a job analysis be performed to ensure that RWLs applied at the worksite reflect a complete consideration of all risk elements of a lifting task. When higher risk task conditions are present, we suggest that medical providers use clinical judgment to decide the best course of action for their patient. These actions typically range from work restrictions that prohibit lifting for the duration of pregnancy, choosing the lift condition in Figure 2 that most closely approximates the lifting conditions of the patient and reducing the RWL by an amount judged to mitigate the increased risk, or recommending to the patient’s employer that a formal job analysis be conducted by an occupational health professional to determine maximum weight limits based on actual lifting conditions.
DISCUSSION
Empirically based lifting criteria established by NIOSH to reduce the risk of overexertion injuries in the general U.S. working population were evaluated for application to pregnant workers. Our evaluation included an extensive review of the literature linking occupational lifting to maternal and fetal health (MacDonald et al., 2013). Decision logic and supporting literature were presented, along with resulting evidence-based provisional clinical guidelines. The RWLs within the provisional guidelines are considerably lower and therefore more protective than AMA guidelines published 29 years ago. Based on our review of the available evidence, the provisional clinical guidelines present lifting thresholds that most pregnant workers with uncomplicated pregnancies should be able to perform without increased risk of adverse maternal and fetal health consequences. Except for restrictions involving lifting from the floor and overhead, the guidelines are compatible with NIOSH lifting recommendations adopted in the early 1990s for the general U.S. workforce.
The proposed guidelines address a need for practical evidence-based criteria to aid decision making and clinical management of patients with uncomplicated pregnancies and may help ensure that pregnant workers are properly advised and afforded ample protections in accordance with accumulated scientific evidence. This need is underscored in the United States where federal regulations for occupational lifting are lacking and limited opportunities for paid antenatal leave are available (Laughlin, 2011; White, 2006). The guidelines should be useful to clinicians in advising their patients about weight threshold restrictions for occupational lifting tasks; they are also expected to be useful to ergonomic practitioners in the evaluation and redesign of lifting tasks. We anticipate that the adoption of these provisional guidelines by obstetric and occupational health medical providers would narrow the variability shown to exist in decisions about employment restrictions related to lifting among pregnant workers (Frazier, Ho, & Molgaard, 2001; Pompeii et al., 2011).
We applied simplifying assumptions to increase the practical application of the guidelines in a clinical setting (e.g., assuming short vertical travel distances, no rotation of the spine, and optimal coupling). Limitations of the original RNLE (e.g., one-handed lifting, lifting more than 8 hr per day) apply to the provisional clinical guidelines as well. These limitations notwithstanding, the guidelines account for horizontal and vertical lifting distances and lifting frequency and duration—task conditions that are among the most important determinants of overexertion injury associated with lifting (Waters et al., 1993). Increased abdominal depth in the later stages of pregnancy prevents lifting in the most biomechanically advantageous posture—thus RWLs in the “close” lifting zone are excluded after 20 weeks gestation. Other pregnancy-specific considerations warranted adoption of the ACGIH Threshold Limit Value of zero for lifting from the floor (ACGIH, 2012) to avoid risks to maternal (Nicholls & Grieve, 1992; Punnett et al., 1991; Vandergrift et al., 2012) and fetal health (Bonzini et al., 2009; Florack et al., 1993). The guidelines also restrict overhead lifting due to increased risk of acute trauma associated with postural instability (Dunning et al., 2010; Fries & Hellebrandt, 1943; Oliveira et al., 2009).
When lifting frequency exceeds 3 lifts per minute or when simplifying assumptions are violated, we recommend that a job analysis be performed to help ensure that RWLs applied at the worksite reflect a complete consideration of all risk elements of a lifting task. When higher risk task conditions exist (e.g., high frequency lifting) or when there are extenuating medical conditions, we suggest that obstetric providers use clinical judgment to decide the appropriate course of action for their patient as it relates to task restrictions. Some women may have medical conditions that make it unsafe to manually lift objects of any weight during pregnancy; these medical conditions may be specific to pregnancy (such as preeclampsia or cervical incompetence) or unrelated, such as a prior history of back injury. It is beyond our capability to identify those individuals, and it remains for the clinical medical practitioner to either restrict lifting or determine a lifting weight threshold for individuals with underlying medical conditions.
It is important to acknowledge limitations of the epidemiologic evidence that we reviewed in conjunction with the development of the provisional clinical guidelines. These limitations often include inadequate sample size, significant potential for selection bias, inadequate attention to exposure contrast, and poor specification and measurement of exposure (Bonzini, Coggon, & Palmer, 2007; Royal College of Physicians, 2009). Moreover, significant selection biases in epidemiologic studies of heavy lifting have been reported for investigations involving nonpregnant workers (Waters et al., 1999), and such biases are likely to be more pronounced among pregnant workers because antenatal leave is more common among those employed in heavy physical work (Saurel-Cubizolles & Kaminski, 1987).
In our effort to combine knowledge of the physical and physiological effects of pregnancy with empirical data on the association between occupational lifting and maternal–fetal health, we identified some notable research gaps. No empirical data exist to our knowledge on the effects of pregnancy-induced ligament laxity on muscular cocontraction and joint loading or to the potential effects on intraabdominal pressure. Due to the paucity of data on these topics, we did not directly account for the effect of laxity, intraabdominal pressure, or increased abdominal mass in the RWL computations; we expect, however, that design criteria of the original RNLE, which protects 90% of the female population from overexertion injury, combined with empirically based guidance to restrict lifting from the floor and overhead by pregnant workers, would attenuate potential increased risks due to these factors. As new scientific data become available on these and other topics relevant to lifting during pregnancy, the RWLs in the clinical guidelines should be evaluated and revised accordingly.
We present the first provisional clinical guidelines to address occupational lifting during pregnancy in the United States in nearly three decades—during which there was a large increase in the number of women employed outside the home and remaining in the workforce during pregnancy (Laughlin, 2011). The resulting RWLs are considerably lower, and therefore more protective, than AMA guidelines published 29 years ago and still used to inform physician practice and workplace policy (Pompeii et al., 2011; U.S. Navy and Marine Corps Public Health Center, 2010). Further research is needed to inform appropriate RWLs for highly repetitive lifting during pregnancy and for lifting during the post-partum period. Although testing these guidelines is beyond the scope of this paper, we encourage clinical researchers and professional organizations such as the American College of Obstetricians and Gynecologists and the American College of Occupational and Environmental Medicine to evaluate the application of these guidelines, to participate in and encourage more research on physical job demands and maternal–fetal health, and to suggest revisions to these guidelines as new research findings become available. We look forward to their input.
KEY POINTS.
The NIOSH Revised Lifting Equation was adapted for application to pregnant workers.
Provisional recommended weight limits are presented, specifying weight threshold that most pregnant workers with uncomplicated pregnancies should be able to perform without increased risk of adverse maternal and fetal health consequences.
Guidelines specifying the weight limits and associated task conditions should be useful to ergo-nomic practitioners in the evaluation and redesign of lifting tasks, as well as to clinicians advising patients’ about physical activity restrictions associated with lifting at work.
Acknowledgments
We thank Kathy Connick for conducting literature searches, generating EndNote libraries, and addressing our document retrieval needs; Greg Hartle for developing illustrations for this paper; Peter Napolitano, Megan Ryan, and Peter Nielsen for their contributions in the development of the clinical guidelines; and William Marras, John Wu, and John Meyer for valuable input on an earlier draft. This work was funded by the Centers for Disease Control, National Institute for Occupational Safety and Health, Cincinnati, Ohio. The findings and conclusions in this report are those of the author(s) and do not necessarily represent the views of the National Institute for Occupational Safety and Health nor are they the official policy of the U.S. Army Public Health Command, the Department of the Army, or the Department of Defense.
Biographies
Thomas R. Waters, now retired, was a senior research safety engineer at the National Institute for Occupational Safety and Health in Cincinnati, Ohio, at the time this article was developed. He earned his PhD in biomechanical engineering from the University of Cincinnati in 1987.
Leslie A. MacDonald is a scientist officer with the National Institute for Occupational Safety and Health. She earned her ScD in ergonomics from the University of Massachusetts Lowell Department of Work Environment in 2000.
Stephen D. Hudock is a research safety engineer in the Organizational Science and Human Factors Branch, Division of Applied Research and Technology, National Institute for Occupational Safety and Health. He earned his PhD in interdisciplinary engineering (occupational ergonomics) from Texas A&M University in 1998.
Donald E. Goddard is an ergonomist with the U.S. Army Public Health Command Current. He earned his master of science degree in occupational hygiene and occupational safety from West Virginia University in 1995.
Footnotes
Author(s) Note: The author(s) of this article are U.S. government employees and created the article within the scope of their employment. As a work of the U.S. federal government, the content of the article is in the public domain.
Contributor Information
Thomas R. Waters, National Institute for Occupational Safety and Health, Cincinnati, Ohio, USA
Leslie A. MacDonald, National Institute for Occupational Safety and Health, Cincinnati, Ohio, USA
Stephen D. Hudock, National Institute for Occupational Safety and Health, Cincinnati, Ohio, USA
Donald E. Goddard, USAPHC/Army Institute of Public Health, Occupational Health Sciences Portfolio, Aberdeen Proving Ground, Maryland, USA
References
- American Conference of Governmental Industrial Hygienists. TLVs and BEIs: Based on the documentation of the threshold limit values for chemical substances and physical agents and biological exposure indices. Cincinnati, OH: Author; 2012. Lifting; pp. 177–180. [Google Scholar]
- American Medical Association. Effects of pregnancy on work performance. Journal of the American Medical Association. 1984;251:1995–1997. [Google Scholar]
- Blecher A, Richmond J. Transient laxity of an anterior cruciate ligament-reconstructed knee related to pregnancy. Arthroscopy. 1998;14:77–79. doi: 10.1016/s0749-8063(98)70125-2. [DOI] [PubMed] [Google Scholar]
- Bonzini M, Coggon D, Godfrey K, Inskip H, Crozier S, Palmer K. Occupational physical activities, working hours and outcome of pregnancy: Findings from the Southampton Women’s Survey. Occupational and Environmental Medicine. 2009;66:685–690. doi: 10.1136/oem.2008.043935. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bonzini M, Coggon D, Palmer K. Risk of prematurity, low birthweight and pre-eclampsia in relation to working hours and physical activities: A systematic review. Occupational and Environmental Medicine. 2007;64:228–243. doi: 10.1136/oem.2006.026872. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Calguneri M, Bird H, Wright V. Changes in joint laxity occurring during pregnancy. Annals of the Rheumatic Diseases. 1982;41:126–128. doi: 10.1136/ard.41.2.126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Charlton W, Coslett-Charlton L, Ciccotti M. Correlation of estradiol in pregnancy and anterior cruciate ligament laxity. Clinical Orthopaedics and Related Research. 2001;387:165–170. doi: 10.1097/00003086-200106000-00022. [DOI] [PubMed] [Google Scholar]
- Cheng P, Dumas G, Smith J, Leger A, Plamondon A, McGrath M, Tranmer J. Analysis of self-reported problematic tasks for pregnant women. Ergonomics. 2006;49:282–292. doi: 10.1080/00140130500434929. [DOI] [PubMed] [Google Scholar]
- Cheng PL, Pantel M, Smith JT, Dumas GA, Leger AB, Plamondon A, Tranmer JE. Back pain of working pregnant women: Identification of associated occupational factors. Applied Ergonomics. 2009;40:419–423. doi: 10.1016/j.apergo.2008.11.002. [DOI] [PubMed] [Google Scholar]
- Chengalur SN, Rodgers SH, Bernard TE. Kodak’s ergonomic design for people at work. 2. Hoboken, NJ: John Wiley; 2004. [Google Scholar]
- Colliton J. Managing back pain during pregnancy. Medscape General Medicine. 1999;1(2):1–6. [Google Scholar]
- Colombini D, Occhipinti E, Alvarez-Casado E, Waters T. Manual lifting: A guide to the study of simple and complex tasks. Boca Raton, FL: CRC Press; 2012. [Google Scholar]
- Damen L, Buyruk H, Güler-Uysal F, Lotgering F, Snijders C, Stam H. Pelvic pain during pregnancy is associated with asymmetric laxity of the sacroiliac joints. Acta Obstetricia et Gynecologica Scandinavica. 2001;80:1019–1024. doi: 10.1034/j.1600-0412.2001.801109.x. [DOI] [PubMed] [Google Scholar]
- Dumas G, Reid J. Laxity of knee cruciate ligaments during pregnancy. Journal of Orthopaedic & Sports Physical Therapy. 1997;26:2–6. doi: 10.2519/jospt.1997.26.1.2. [DOI] [PubMed] [Google Scholar]
- Dunning K, LeMasters G, Bhattacharya A. A major public health issue: The high incidence of falls during pregnancy. Maternal and Child Health Journal. 2010;14:720–725. doi: 10.1007/s10995-009-0511-0. [DOI] [PubMed] [Google Scholar]
- Florack E, Zielhuis G, Pellegrino J, Rolland R. Occupational physical activity and the occurrence of spontaneous abortion. International Journal of Epidemiology. 1993;22:878–884. doi: 10.1093/ije/22.5.878. [DOI] [PubMed] [Google Scholar]
- Frazier L, Ho H, Molgaard C. Variability in physician management of employment during pregnancy. Women & Health. 2001;34(4):51–63. doi: 10.1300/J013v34n04_04. [DOI] [PubMed] [Google Scholar]
- Fries E, Hellebrandt F. The influence of pregnancy on the location of the center of gravity, postural stability, and body alignment. Journal of Obstetrics & Gynaecology. 1943;46:374–380. [Google Scholar]
- Granata KP, Marras WS. Cost-benefit of muscle cocontraction in protecting against spinal instability. Spine. 2000;25:1398–1404. doi: 10.1097/00007632-200006010-00012. [DOI] [PubMed] [Google Scholar]
- Larsen PS, Strandberg-Larsen K, Juhl M, Svendsen SW, Bonde JP, Nybo Andersen AM. Occupational lifting and pelvic pain during pregnancy: A study within the Danish National Birth Cohort. Scandinavian Journal of Work, Environment and Health. 2013;39:88–95. doi: 10.5271/sjweh.3304. [DOI] [PubMed] [Google Scholar]
- Laughlin L. Maternity leave and employment patterns: 2006–2008. Washington, DC: Current Population Report; 2011. [Google Scholar]
- MacDonald LA, Waters T, Napolitano P, Goddard D, Ryan M, Neilsen P, Hudock S. Clinical guidelines for occupational lifting in pregnancy: Evidence summary and provisional recommendations. American Journal of Obstetrics & Gynecology. 2013;209:80–88. doi: 10.1016/j.ajog.2013.02.047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marnach M, Ramin K, Ramsey P, Song SW, Stensland J, An KN. Characterization of the relationship between joint laxity and maternal hormones in pregnancy. Obstetrics & Gynecology. 2003;101:331–335. doi: 10.1016/s0029-7844(02)02447-x. [DOI] [PubMed] [Google Scholar]
- Marras W. The working back: A systems view. Hoboken, NJ: John Wiley; 2008. [Google Scholar]
- Mens J, Pool-Goudzwaard A, Stam H. Mobility of the pelvic joints in pregnancy-related lumbopelvic pain: A systematic review. Obstetrical & Gynecological Survey. 2009;64:200–208. doi: 10.1097/OGX.0b013e3181950f1b. [DOI] [PubMed] [Google Scholar]
- Nicholls J, Grieve D. Performance of physical tasks in pregnancy. Ergonomics. 1992;35:301–311. doi: 10.1080/00140139208967815. [DOI] [PubMed] [Google Scholar]
- Noon ML, Hoch AZ. Challenges of the pregnant athlete and low back pain. Current Sports Medicine Reports. 2012;11:43–48. doi: 10.1249/JSR.0b013e31824330b6. [DOI] [PubMed] [Google Scholar]
- Oliveira L, Vieira T, Macedo A, Simpson D, Nadal J. Postural sway changes during pregnancy: A descriptive study using stabilometry. European Journal of Obstetrics and Gynecology and Reproductive Biology. 2009;147:25–28. doi: 10.1016/j.ejogrb.2009.06.027. [DOI] [PubMed] [Google Scholar]
- Paul J, Frings-Dresen M. Changes in working posture and perceived effort due to pregnancy. In: Queinnec Y, Daniellou F, editors. Designing for everyone: Proceedings of the 11th Congress of the International Ergonomics Association. Vol. 2. Paris, France: Taylor & Francis; 1991. pp. 1562–1564. [Google Scholar]
- Paul J, Frings-Dresen M. Standing working posture compared in pregnant and nonpregnant conditions. Ergonomics. 1994;37:1563–1575. doi: 10.1080/00140139408964934. [DOI] [PubMed] [Google Scholar]
- Paul J, van Dijk F, Frings-Dresen M. Work load and musculoskeletal complaints during pregnancy. Scandinavian Journal of Work, Environment and Health. 1994;20:153–159. doi: 10.5271/sjweh.1414. [DOI] [PubMed] [Google Scholar]
- Perkins T, Blackwell S. Accommodation and occupational safety for pregnant military personnel: Final report (ADA364792) Dayton, OH: U.S. Air Force Research Laboratory, DTIC Online Information for the Defense Community; 1998. Retrieved from http://www.dtic.mil/dtic/ [Google Scholar]
- Pompeii LA, Evenson KR, Delclos GL. Obstetricians’ practices and recommendations for occupational activity during pregnancy. Journal of Reproductive Medicine. 2011;56(1–2):17–24. [PubMed] [Google Scholar]
- Poole J. Body mechanics during daily tasks to reduce back pain in women who are pregnant. Work. 1998;10:157–165. doi: 10.3233/WOR-1998-10207. [DOI] [PubMed] [Google Scholar]
- Punnett L, Fine LJ, Keyserling WM, Herrin GD, Chaffin DB. Back disorders and non-neutral trunk postures of automobile assembly workers. Scandinavian Journal of Work, Environment and Health. 1991;17:337–346. doi: 10.5271/sjweh.1700. [DOI] [PubMed] [Google Scholar]
- Royal College of Physicians of London. Physical and shift work in pregnancy: Occupational aspects of management—A national guideline. London, UK: Author; 2009. Retrieved from http://www.rcplondon.ac.uk/ [Google Scholar]
- Saurel-Cubizolles M, Kaminski M. Pregnant women’s working conditions and their changes during pregnancy—A national study in France. British Journal of Industrial Medicine. 1987;44:236–243. doi: 10.1136/oem.44.4.236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schauberger C, Rooney B, Goldsmith L, Shenton D, Silva P, Schaper A. Peripheral joint laxity increases in pregnancy but does not correlate with serum relaxin levels. American Journal of Obstetrics & Gynecology. 1996;174:667–671. doi: 10.1016/s0002-9378(96)70447-7. [DOI] [PubMed] [Google Scholar]
- Spinillo A, Capuzzo E, Baltaro F, Piazzi G, Nicola S, Iasci A. The effect of work activity in pregnancy on the risk of fetal growth retardation. Acta Obstetricia et Gynecologica Scandinavica. 1996;75:531–536. doi: 10.3109/00016349609054666. [DOI] [PubMed] [Google Scholar]
- Sternfeld B. Physical activity and pregnancy outcome: Review and recommendations. Sports Medicine. 1997;23:33–47. doi: 10.2165/00007256-199723010-00004. [DOI] [PubMed] [Google Scholar]
- U.S. Navy and Marine Corps Public Health Center. US Navy and Marine Corps Public Health Center technical manual NMCPHC-TM-OEM 6260.01C. Reproductive and developmental hazards: Guide for occupational health professionals. 2010 Retrieved from http://www.nmcphc.med.navy.mil/downloads/occmed/Repro2010d2.pdf.
- van Lunen B, Roberts J, Branch J, Dowling E. Association of menstrual-cycle hormone changes with anterior cruciate ligament laxity measurements. Journal of Athletic Training. 2003;38:298–303. [PMC free article] [PubMed] [Google Scholar]
- Vandergrift JL, Gold JE, Hanlon A, Punnett L. Physical and psychosocial ergonomic risk factors for low back pain in automobile manufacturing workers. Occupational and Environmental Medicine. 2012;69:29–34. doi: 10.1136/oem.2010.061770. [DOI] [PubMed] [Google Scholar]
- Waters TR, Baron SL, Piacitelli LA, Anderson VP, Skov T, Haring-Sweeney M, Wall DK, Fine LJ. Evaluation of the Revised NIOSH Lifting Equation—A cross-sectional epidemiologic study. Spine. 1999;24:386–394. doi: 10.1097/00007632-199902150-00019. [DOI] [PubMed] [Google Scholar]
- Waters T, Putz-Anderson V, Garg A. Applications manual for the Revised NIOSH Lifting Equation. Cincinnati, OH: U.S. Department of Health and Human Services, National Institute for Occupational Safety and Health; 1994. Retrieved from http://www.cdc.gov/niosh/docs/94-110/ [Google Scholar]
- Waters T, Putz-Anderson V, Garg A, Fine L. Revised NIOSH equation for the design and evaluation of manual lifting tasks. Ergonomics. 1993;36:749–776. doi: 10.1080/00140139308967940. [DOI] [PubMed] [Google Scholar]
- Whitcome KK, Shapiro LJ, Lieberman DE. Fetal load and the evolution of lumbar lordosis in bipedal hominins. Nature. 2007;450(7172):1075–1078. doi: 10.1038/nature06342. [DOI] [PubMed] [Google Scholar]
- White LA. Institutions, constitutions, actor strategies, and ideas: Explaining variation in paid parental leave policies in Canada and the United States. International Journal of Constitutional Law. 2006;4:319–346. [Google Scholar]