Abstract
Objectives
Hypertension is the leading modifiable cause of mortality worldwide. Unlike many conditions where limited evidence exists for management of older individuals, multiple large, robust trials have provided a solid evidence-base regarding the management of hypertension in older adults. Understanding the impact of age on how the prevalence of hypertension and the role of pharmacotherapy in managing hypertension among older persons is a critical element is the provision of optimal health care for older populations. The aim of this study was to explore how the prevalence of hypertension changes with age, the evidence regarding pharmacological management in older adults and to identify known barriers to the optimal management of hypertension in older patients.
Methods
A review of English language studies published prior to 2013 in Medline, Embase and Google scholar was conducted. Key search terms included hypertension, pharmacotherapy, and aged.
Results
The prevalence of hypertension was shown to increase with age, however there is good evidence for the use of a number of pharmacological agents to control blood pressure in older populations. System, physician and patient related barriers to optimal blood pressure control were identified.
Conclusions
Despite good evidence for pharmacological management of hypertension among olderpopulations, under treatment of hypertension is an issue. Concerns regarding adverse effects appearcentral to under treatment of hypertension among older populations.
Keywords: Hypertension, Older adults, Prevalence, Pharmacotherapy, Drug utilization
Introduction
Population aging has considerable implications for health care systems internationally, especially from the perspective of pharmaceutical practice and policy. “Older adults” are commonly defined in the medical literature as individuals aged 65 years or over [1]. Internationally, the proportion of the population defined as older adults is increasing, primarily as a result of the increase in life expectancy [2]. By 2050 it is anticipated that older population will account for 21 % of the total population in most developed countries [3], while in some countries, such as Japan, older adults already represent one-fifth of the total population [4, 5]. A similar increase applies to the very old adults (age ≥80 years), one of the fastest growing segments of older adults population and one that is expected to triple by 2050 [6].
Hypertension is the leading modifiable cause of mortality worldwide [7]. Unlike many conditions where limited evidence exists for management of those aged over 65 years due to the exclusion of older populations from clinical trials [8, 9], the findings of multiple large, robust trials have provided a solid evidence-base regarding the management of hypertension in older adults [7]. Adverse outcomes associated with poor blood pressure (BP) control in older persons have been well documented. A Cochrane review of 12 clinical trials showed that the management of hypertension in people aged 60 years and over was associated with a reduction in mortality (Relative Risk (RR)) = 0.9, 95 % confidence interval ((CI) 0.84–0.97) [10]. The same review reported pharmacological management of hypertension in older adults was associated with significant reductions in both cardiovascular (RR = 0.77, 95 % CI 0.68–0.86) and cerebrovascular mortality (RR = 0.66, 95 % CI 0.53–0.82) [10].
Given the expected increase in the older adult population and the wealth of evidence regarding the management of hypertension in older persons, understanding how the prevalence of hypertension changes with age as well as how physicians currently manage older patients with increased BP is important. Furthermore, insight into current barriers to the provision of optimal management is essential if clinicians are to meet the health needs of the growing older populations. The aim of this study was to provide an overview of the prevalence of hypertension and its pharmacological management in older adults. A secondary aim was to explore known barriers to the optimal management of hypertension in older patients.
Methods
Narrative review methodology as described by Green et al. [11] was used to conduct a non-systematic narrative review of the literature regarding pharmacotherapy for the management of hypertension in older populations.
Data sources and study selection
An electronic search of the electronic databases EMBASE, MEDLINE for studies published prior to 2013 regarding the use of pharmacotherapy for the pharmacological management of hypertension among older populations was conducted. In addition, Google scholar was searched to identify any non-indexed relevant publications. Search terms used included: hypertension, pharmacotherapy, and aged. Additional search terms used included: drug therapy, elderly, older patients, and geriatric. Search terms were mapped to MESH headings in Medline and EMTREE headings in Embase. Studies which focused specifically on pharmacological management of hypertension in older persons were included in the review. Exclusion criteria were non-English language studies, studies in non-human populations as well as studies that did not specifically focus on populations aged 65 years and older or on pharmacological management of hypertension.
Data synthesis
A narrative synthesis of the prevalence of hypertension in older populations, the evidence regarding the use of different pharmacological agents and identification of barrier to optimal pharmacological management of hypertension among older persons was conducted.
Review
Prevalence of hypertension in older populations
Data from the Framingham study in 1978 and 2002 [12–14] and the 2005 US National Health and Nutrition Survey (NHANES) [15] have shown clear increases in the prevalence of hypertension with age (Fig. 1). The original Framingham study followed 5209 respondents from 1948 until 2005, exploring the development of cardiovascular disease and identification of associated risk factors over time [2, 3]. The NHANES surveys are annual cross sectional surveys which combine interview and physical examination, to assess health status across representative samples of the American population.[15] The NHANES data demonstrated that increases in the prevalence of hypertension prevalence begin in adulthood, with the prevalence doubling between the ages of 20–40 years, and then with a further 100 % increase occurring between 40 and 60 years. The Framingham study showed that this pattern continues as people age, with the prevalence of hypertension increasing from 27.3 % in those aged ≥ 60 years to 74.0 % in those aged over 80 years.
Fig. 1.
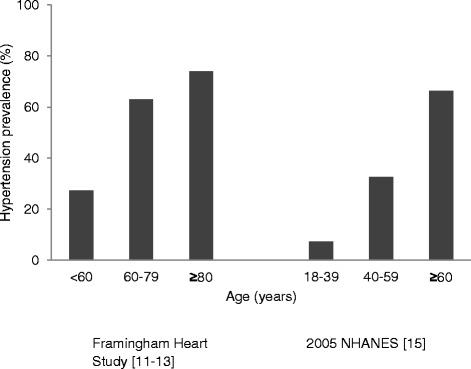
Increasing prevalence of hypertension with age
Gender differences in the prevalence of hypertension have been noted in both younger and older populations. A number of studies have shown found that although women have a lower prevalence of hypertension than men at a younger ages, this pattern changes after the age of 60 years when the pattern reverses with the prevalence in women exceeding that in men.[13, 16–21],
Differences have been reported in terms of aging with respect to increases in systolic blood pressure (SBP) compared with diastolic blood pressure (DBP). Both systolic and diastolic pressure have been reported to increase with age. [15] This increase continues until the ninth decade however it is believed that DBP may plateau or even decrease around the age of 60 years. [15] These differences may account for the increase in isolated systolic hypertension that is associated with aging. Isolated systolic hypertension refers to elevated SBP with a normal DBP. [22] .
Pathophysiological changes including increased peripheral vascular resistance due to arterial stiffening, which occur with age, are believed to be one factor associated with the increase in hypertension associated with aging. [15, 23]. This increase in arterial stiffness with ageing is believed to alter the normal hemodynamic pattern of blood pressure (BP) causing an increased pulse wave velocity, an index of arterial stiffness, and widening pulse pressure therefore accounting for the observed age–related decline in DBP and increase in SBP. [17, 23–25]. Other factors such as the changes in renin and aldosterone levels, decreases in renal salt excretion, age-related declines in renal function and associated changes in the autonomic nervous system and endothelial function are also considered contributory factors.[16, 26–28]. Life style related factors might also contribute to the development of hypertension. Factors such as stress, excessive alcohol intake, sedentary life style, high sodium intake and obesity are risk factors for hypertension [16, 29–31]. Moreover a synergistic effect on the risk of hypertension has been observed when multiple factors exist synchronously [16, 29–31].
Pharmacological management of hypertension in the elderly
While life-style interventions are generally the first-line strategy for the management of all persons with hypertension, the majority of hypertensive patients will require pharmacological intervention to adequately control their blood pressure. [32]. A number of large well-conducted clinical trials exploring pharmacological management of hypertension in the elderly have been conducted and there is good evidence for the use of a variety of different antihypertensive agents in the management of hypertension in the elderly. [10]
Thiazide and thiazide –like diuretics
Thiazides diuretics are one of the oldest drug classes used in the treatment of hypertension. [33] Evidence of effectiveness in lowering BP and preventing the cardio and cerebrovascular adverse outcomes associated with hypertension in the elderly has been supported by several clinical trials, including the Hypertension in the very elderly (HyVET) [34], the Swedish Trial in Old Patients with Hypertension (STOP)[35, 36] and the Antihypertensive and Lipid-Lowering Treatment to prevent Heart Attack Trial (ALLHAT) [37] studies While not all these studies focused specifically on the elderly, the mean participant age was over 65 years for all, and their recommendations were especially relevant for the younger elderly population.
Use of thiazide and thiazide like diuretics for the management of hypertension in older persons has declined over the past decade. [19, 20, 38–40]. There are a number of possible explanations for this change in the pattern of thiazide prescribing including increased use of other diuretics, particularly in elderly with complicated hypertension [41, 42], the advent of other antihypertensive medications such as Calcium Channel Blockers (CCBs) or agents acting on the Renin Angiotensin System (RAS), as well as greater caution by prescribers due to increased risk of adverse drug reactions in elderly [43, 44]. Yet, despite this general decline in thiazide use among older persons with hypertension, their use remains high [15, 45, 46], and they are the most commonly used agents in combination therapy in the management of hypertension. [19, 20, 38, 39, 45, 47].
Agents acting on the Renin-Angiotensin System (RAS)
There are three main three antihypertensive classes that act on RAS. These are the angiotensin receptor blockers (ARBs), the Angiotensin concerting enzyme inhibitors (ACEI) and the direct renin inhibitors. The use of both ARBs [15, 38, 45] and ACEIs [15, 19, 20, 38, 40, 45, 47–49] in the elderly is generally high, and has increased over years surpassing other antihypertensive classes such as CCBs. The increase in use of these agents has been supported by clinical trials such as the Second Australian National Blood Pressure (ANBP2) [50] which demonstrated that ACEI were superior to thiazide diuretics in terms of cardiovascular outcomes, however there was no difference between the regimens in terms of all cause mortality. In addition to increased use as monotherapy, ACEI and ARB use in combination with other antihypertensive medications has also increased over recent years [19, 20, 38, 39, 45, 47]. In contrast to the common use of ACEIs and ARBs, use of aliskiren, a direct renin inhibitor that has been approved for use since 2007 in elderly hypertension patients is minimal[15, 47]. The slow uptake of aliskiren for use among the elderly may be hindered by its limited efficacy and relatively poor safety profile.[51, 52]
Calcium channel blockers (CCBs)
Since the introduction of CCBs, the prescribing pattern of this antihypertensive medication class in the elderly has increased both as monotherapy and combination therapy. [15, 20, 39, 48, 49] Despite publication of the Systolic Hypertension in the Europe Trial (SYST-EUR) in 1997 which showed that treating 1000 patients for 5 years with a CCB regimen prevents 29 strokes or 53 MIs [53], a decline in the use of CCBs has generally been noticed in elderly and very elderly patients since the mid 1990s has been observed. [19, 38, 45] This decline in use may be secondary to proposed safety concerns including increased risk of cancer, myocardial infarction and gastrointestinal heamorrhage with long term use [54–56].
Beta blockers (BBs)
Beta blockers were among the most commonly prescribed agents since their introduction as an option for the treatment of hypertension [40, 47, 48]. However, use in the elderly has decreased [19, 20, 38, 39, 43]. following publication of a meta-analyses raising questions about their efficacy and highlighting safety concerns with an increased risk of stroke reported with BB use as monotherapy [57]. The current low rate of use was highlighted in a recently published observational study. [45]
Alpha blockers
While several studies have shown a slight increase in the use of alpha blockers in the management of hypertension in the elderly and very elderly patients [15, 40], overall their use has declined [20, 45, 47, 48]. This decline in use may be due to the poor adverse effect profile of the alpha blockers in the elderly as well as to a lack of evidence in preventing cardiovascular related complications when compared with other antihypertensive agents.
Barriers to the optimal management of hypertension in the elderly
Despite the wealth of evidence regarding the benefits of managing hypertension in older and very old populations, a substantial proportion of older persons have suboptimal blood pressure control. [58]. A number of barriers to optimal blood pressure control in the elderly have been identified and these barriers can generally be considered as system-, physician- or patient-related barriers.
System–related barriers affecting blood pressure control in the elderly include the variability in treatment recommendations for this population. [59, 60]. While a number of clinical trials have been conducted in the elderly, the extent to which this evidence has been incorporated into treatment guidelines and translated into practice remains unknown.
Physician-related barriers include differences in physician attitudes towards the risks and benefits of managing hypertension in older persons as well as differences in interpretation of the evidence. [61–64]. Inconsistency between treatment guidelines regarding management of hypertension in the elderly may make it difficult for clinicians to incorporate the evidence-based recommendations in their daily clinical practice. [61, 62, 65]. The lack of consistency in guidelines may also influence prescribing decisions in the treatment of complex patients, such as those with multiple co-morbidities. [61, 63, 66, 67]
Patient awareness of their condition may also influence medication use and BP control. Patients with a higher awareness of the need for regular blood pressure monitoring are more likely to have controlled blood pressure, [63, 66–70] while those with poorer adherence to prescribed medication are less likely to have controlled BP. [18, 71–74]
Adverse drug reactions may influence both the clinician’s decision to prescribe a medication[75, 76], as well as the patient’s decision to continue using a medication [66], and more work is needed to better understand the role adverse drug reactions play in the use of antihypertensive medications in the elderly.
Unlike a systeamtic review where the aim is to capture all revelant literature, as a non-systematic narrative review, the aim of this study was to provide an wide overview of the prevalence of hypertension and its pharmacological management in older adults. To cover a wide range of published literature, searches were conducted in both Medline and Embase electronic databases. In addition, a general search of Google scholar was also conducted to capture relevant published work not indexed in either Medline or Embase. However inclusion of other databases may have widened the range of literature included in the analysis and is one limitation of this work.
Conclusion
The prevalence of hypertension increases significantly with age. While approximately 30 % of the adult population aged less than 65 years has hypertension, by the age of 80 over 70 % of the population has or is being treated for elevated blood pressure. The estimated direct and indirect economic impacts and medical expenditure of hypertension is high and, given predicted increases in the elderly population, likely to increase. Despite the availability of effective antihypertensive medications and good evidence for blood pressure reduction in older populations, current management, management appears suboptimal. Barriers to optimal blood pressure control in older populations are often multifactorial highlighting the clinical complexity of this patient population. System, prescriber and patient related barriers to the management of hypertension exist and is interplay between these such as the lack of clinical guidance regarding management of hypertension in complex older patients with multiple comorbidities contribute to suboptimal blood pressure control in older populations.
Abbreviations
- RR
Relative risk
- CI
Confidence interval
- SBP
Systolic blood Pressure
- DBP
Diastolic blood pressure
- BP
Blood pressure
- RAS
Renin angiotensin system
- ARB
Angiotensin receptor blocker
- ACEI
Angiotensin concerting enzyme inhibitor
- CCB
Calcium channel blocker
- BB
Beta blocker
Footnotes
Competing interests
The authors declare they have no competing interests.
Authors’ contributions
MK, IS, BS and LR proposed and designed the experiments. MK and BW performed the experiments, MK and LR analyzed the bioinformatics data and LR prepared phylogenetic trees. MK, IS, BS, and LR wrote the paper. All authors approved the final manuscript.
Contributor Information
Tariq M Alhawassi, Email: tarriq@KSU.EDU.SA.
Ines Krass, Email: ines.krass@sydney.edu.au.
Lisa G Pont, Email: lisa.pont@mq.edu.au.
References
- 1.Aronow WS, Fleg JL, Pepine CJ, Artinian NT, Bakris G, Brown AS, et al. ACCF/AHA 2011 Expert Consensus Document on Hypertension in the ElderlyA Report of the American College of Cardiology Foundation Task Force on Clinical Expert Consensus Documents Developed in Collaboration With the American Academy of Neurology, American Geriatrics Society, American Society for Preventive Cardiology, American Society of Hypertension, American Society of Nephrology, Association of Black Cardiologists, and European Society of Hypertension. J Am Coll Cardiol. 2011;57:2037–2114. doi: 10.1016/j.jacc.2011.01.008. [DOI] [PubMed] [Google Scholar]
- 2.Oeppen J, Vaupel JW. Broken limits to life expectancy. Science. 2002;296:1029–1031. doi: 10.1126/science.1069675. [DOI] [PubMed] [Google Scholar]
- 3.United Nations Department of Economic and Social Affairs Population Division. World Population Aging: 1950-2050. New York: United Nations; 2001.
- 4.He W, Sengupta M, Velkoff VA, DeBarros KA. U.S. Census Bureau, Current Population Reports, P23-209, 65+ in the United States: 2005. Washington DC: U.S. Government Printing Office; 2005.
- 5.Ogawa N, Matsukura R. Ageing in Japan: the health and wealth of older persons. In United Nations expert group meeting on social and economic implications of changing population age structures. 2007;199–220.
- 6.United Nations, Department of Economic and Social Affairs, Population Division. World Population Ageing 2013. New York: United Nations, 2013.
- 7.Pimenta E, Oparil S. Management of hypertension in the elderly. Nat Rev Cardiol. 2012;9:286–296. doi: 10.1038/nrcardio.2012.27. [DOI] [PubMed] [Google Scholar]
- 8.White SM. Including the very elderly in clinical trials. Anaesthesia. 2010;65:778–780. doi: 10.1111/j.1365-2044.2010.06456.x. [DOI] [PubMed] [Google Scholar]
- 9.Devlin G. Women and elderly: subgroups under-represented in clinical trials. Curr Opin Cardiol. 2010;25:335–339. doi: 10.1097/HCO.0b013e328338bcab. [DOI] [PubMed] [Google Scholar]
- 10.Musini VM, Tejani AM, Bassett K, Wright JM. Pharmacotherapy for hypertension in the elderly. Cochrane Database Syst Rev. 2009;7(4). CD000028. [DOI] [PubMed]
- 11.Green BN, Johnson CD, Adams A. Writing narrative literature reviews for peer-reviewed journals: secrets of the trade. J Chiropr Med. 2006;5(3):101–117. doi: 10.1016/S0899-3467(07)60142-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kannel WB, Gordan T. Evaluation of cardiovascular risk in the elderly. The Framingham study. Bull N Y Acad Med. 1978;54(6):573–91. [PMC free article] [PubMed] [Google Scholar]
- 13.Franklin SS, Gustin W, Wong ND, Larson MG, Weber MA, Kannel WB, et al. Hemodynamic patterns of age-related changes in blood pressure The Framingham Heart Study. Circulation. 1997;96:308–315. doi: 10.1161/01.CIR.96.1.308. [DOI] [PubMed] [Google Scholar]
- 14.Vasan RS, Beiser A, Seshadri S, Larson MG, Kannel WB, D’Agostino RB, et al. Residual lifetime risk for developing hypertension in middle-aged women and men: The Framingham Heart Study. JAMA. 2002;287(8):1003–10. doi: 10.1001/jama.287.8.1003. [DOI] [PubMed] [Google Scholar]
- 15.Bromfield SG, Bowling CB, Tanner RM, Peralta CA, Odden MC, Oparil S, et al. Trends in hypertension prevalence, awareness, treatment, and control among US adults 80 years and Older, 1988–2010. J Clin Hypertens. 2014;16(4):270–76. doi: 10.1111/jch.12281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Halter JB, Ouslander JG, Tinetti ME, Studenski S, High KP, Asthana S. Hazzard's Geriatric Medicine and Gerontology, 6th Edition. USA: McGraw-Hill; 2009.
- 17.Mann SJ. Systolic hypertension in the elderly: pathophysiology and management. Arch Intern Med. 1992;152:1977–1984. doi: 10.1001/archinte.1992.00400220015004. [DOI] [PubMed] [Google Scholar]
- 18.Lu F-H, Tang S-J, Wu J-S, Yang Y-C, Chang C-J. Hypertension in elderly persons its prevalence and associated cardiovascular risk factors in Tainan city, southern Taiwan. J Gerontol A Biol Sci Med Sci. 2000;55:M463–M468. doi: 10.1093/gerona/55.8.M463. [DOI] [PubMed] [Google Scholar]
- 19.Primatesta P, Poulter NR. Hypertension management and control among English adults aged 65 years and older in 2000 and 2001. J Hypertens. 2004;22:1093–1098. doi: 10.1097/00004872-200406000-00008. [DOI] [PubMed] [Google Scholar]
- 20.Trenkwalder P, Ruland D, Stender M, Gebhard J, Trenkwalder C, Lydtin H, et al. Prevalence, awareness, treatment and control of hypertension in a population over the age of 65 years: results from the Starnberg Study on Epidemiology of Parkinsonism and Hypertension in the Elderly (STEPHY) J Hypertens. 1994;12:709. doi: 10.1097/00004872-199406000-00012. [DOI] [PubMed] [Google Scholar]
- 21.Gambassi G, Lapane K, Sgadari A, Landi F, Carbonin P, Hume A, et al. Prevalence, clinical correlates, and treatment of hypertension in elderly nursing home residents. Arch Intern Med. 1998;158:2377–2385. doi: 10.1001/archinte.158.21.2377. [DOI] [PubMed] [Google Scholar]
- 22.Franklin SS, Jacobs MJ, Wong ND, Gilbert J, Lapuerta P. Predominance of isolated systolic hypertension among middle-aged and elderly US hypertensives analysis based on National Health and Nutrition Examination Survey (NHANES) III. Hypertension. 2001;37:869–874. doi: 10.1161/01.HYP.37.3.869. [DOI] [PubMed] [Google Scholar]
- 23.Mitchell GF, Parise H, Benjamin EJ, Larson MG, Keyes MJ, Vita JA, et al. Changes in arterial stiffness and wave reflection with advancing age in healthy men and women the Framingham Heart Study. Hypertension. 2004;43:1239–1245. doi: 10.1161/01.HYP.0000128420.01881.aa. [DOI] [PubMed] [Google Scholar]
- 24.Pinto E. Blood pressure and ageing. Postgrad Med J. 2007;83:109–114. doi: 10.1136/pgmj.2006.048371. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Mackey RH, Sutton-Tyrrell K, Vaitkevicius PV, Sakkinen PA, Lyles MF, Spurgeon HA, et al. Correlates of aortic stiffness in elderly individuals: a subgroup of the Cardiovascular Health Study. Am J Hypertens. 2002;15:16–23. doi: 10.1016/S0895-7061(01)02228-2. [DOI] [PubMed] [Google Scholar]
- 26.Weinberger MH. Salt sensitivity of blood pressure in humans. Hypertension. 1996;27:481–490. doi: 10.1161/01.HYP.27.3.481. [DOI] [PubMed] [Google Scholar]
- 27.Fliser D, Ritz E. Relationship between hypertension and renal function and its therapeutic implications in the elderly. Gerontology. 1998;44:123–131. doi: 10.1159/000021995. [DOI] [PubMed] [Google Scholar]
- 28.Wallace SM, McEniery CM, Mäki-Petäjä KM, Booth AD, Cockcroft JR, Wilkinson IB. Isolated systolic hypertension is characterized by increased aortic stiffness and endothelial dysfunction. Hypertension. 2007;50:228–233. doi: 10.1161/HYPERTENSIONAHA.107.089391. [DOI] [PubMed] [Google Scholar]
- 29.Carretero OA, Oparil S. Essential hypertension part I: definition and etiology. Circulation. 2000;101:329–335. doi: 10.1161/01.CIR.101.3.329. [DOI] [PubMed] [Google Scholar]
- 30.MacMahon SW, Blacket RB, Macdonald GJ, Hall W. Obesity, Alcohol Consumption and Blood Pressure in Australian Men and Women The National Heart Foundation of Australia Risk Factor Prevalence Study. J Hypertens. 1984;2:85–91. doi: 10.1097/00004872-198402000-00015. [DOI] [PubMed] [Google Scholar]
- 31.Barreto SM, Passos VMA, Firmo JOA, Guerra HL, Vidigal PG, Lima-Costa MFF. Hypertension and clustering of cardiovascular risk factors in a community in Southeast Brazil: the Bambuí Health and Ageing Study. Arq Bras Cardiol. 2001;77:576–581. doi: 10.1590/S0066-782X2001001200008. [DOI] [PubMed] [Google Scholar]
- 32.Mancia G, Fagard R, Narkiewicz K, Redon J, Zanchetti A, Böhm M, et al. ESH/ESC Guidelines for the management of arterial hypertension The Task Force for the management of arterial hypertension of the European Society of Hypertension (ESH) and of the European Society of Cardiology (ESC) Eur Heart J. 2013;2013(34):2159–2219. doi: 10.1093/eurheartj/eht151. [DOI] [PubMed] [Google Scholar]
- 33.Huebschmann AD, Bublitz C, Anderson RJ. Are hypertensive elderly patients treated differently? Clin Interv Aging. 2006;1:289. doi: 10.2147/ciia.2006.1.3.289. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Beckett NS, Peters R, Fletcher AE, Staessen JA, Liu L, Dumitrascu D, et al. Treatment of hypertension in patients 80 years of age or older. N. Engl. J. Med. 2008;358:1887–1898. doi: 10.1056/NEJMoa0801369. [DOI] [PubMed] [Google Scholar]
- 35.Dahlöf B, Hansson L, Lindholm L, Schersten B, Ekbom T, Wester P. Morbidity and mortality in the Swedish trial in old patients with hypertension (STOP-Hypertension) The Lancet. 1991;338:1281–1285. doi: 10.1016/0140-6736(91)92589-T. [DOI] [PubMed] [Google Scholar]
- 36.Hansson L, Lindholm LH, Ekbom T, Dahlöf B, Lanke J, Scherstén B, et al. Randomised trial of old and new antihypertensive drugs in elderly patients: cardiovascular mortality and morbidity the Swedish Trial in Old Patients with Hypertension-2 study. The Lancet. 1999;354:1751–1756. doi: 10.1016/S0140-6736(99)10327-1. [DOI] [PubMed] [Google Scholar]
- 37.Davis B, Cutler JA, Gordon D. Major outcomes in high risk hypertensive patients randomized to angiotensin-converting enzyme inhibitor or calcium channel blocker vs diuretic: The Antihypertensive and Lipid Lowering treatment to prevent Heart Attack Trial (ALLHAT) Jama. 2002;288:2981–2997. doi: 10.1001/jama.288.22.2820-JLT1211-1-4. [DOI] [PubMed] [Google Scholar]
- 38.Triantafyllou A, Douma S, Petidis K, Doumas M, Panagopoulou E, Pyrpasopoulou A, et al. Prevalence, awareness, treatment and control of hypertension in an elderly population in Greece. Rural Remote Health. 2010;10(1225). [PubMed]
- 39.Prencipe M, Casini A, Santini M, Ferretti C, Scaldaferri N, Culasso F. Prevalence, awareness, treatment and control of hypertension in the elderly: results from a population survey. J Hum Hypertens. 2000;14:825–830. doi: 10.1038/sj.jhh.1001117. [DOI] [PubMed] [Google Scholar]
- 40.Psaty BM, Manolio TA, Smith NL, Heckbert SR, Gottdiener JS, Burke GL, et al. Time trends in high blood pressure control and the use of antihypertensive medications in older adults: the Cardiovascular Health Study. Arch Intern Med. 2002;162:2325–2332. doi: 10.1001/archinte.162.20.2325. [DOI] [PubMed] [Google Scholar]
- 41.Van Kraaij D, Jansen R, Gribnau F, Hoefnagels W. Loop diuretics in patients aged 75 years or older: general practitioners’ assessment of indications and possibilities for withdrawal. Eur J Clin Pharmacol. 1998;54:323–327. doi: 10.1007/s002280050467. [DOI] [PubMed] [Google Scholar]
- 42.Van Kraaij DJ, Jansen RW, De Gier JJ, Gribnau FW, Hoefnagels WH. Prescription patterns of diuretics in Dutch community‐dwelling elderly patients. Br J Clin Pharmacol. 1998;46:403–407. doi: 10.1046/j.1365-2125.1998.00793.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Onder G, Gambassi G, Landi F, Pedone C, Cesari M, Carbonin P, et al. Trends in antihypertensive drugs in the elderly: the decline of thiazides. J Hum Hypertens. 2001;15:291–297. doi: 10.1038/sj.jhh.1001176. [DOI] [PubMed] [Google Scholar]
- 44.Moser M. Why are physicians not prescribing diuretics more frequently in the management of hypertension? Jama. 1998;279:1813–1816. doi: 10.1001/jama.279.22.1813. [DOI] [PubMed] [Google Scholar]
- 45.Rodriguez-Roca GC, Llisterri JL, Prieto-Diaz MA, Alonso-Moreno FJ, Escobar-Cervantes C, Pallares-Carratala V, et al. Blood pressure control and management of very elderly patients with hypertension in primary care settings in Spain. Hypertens Res. 2013;37:166–171. doi: 10.1038/hr.2013.130. [DOI] [PubMed] [Google Scholar]
- 46.Tu K, Campbell NR, Chen Z, McAlister FA. Thiazide diuretics for hypertension: prescribing practices and predictors of use in 194,761 elderly patients with hypertension. Am J Geriatr Pharmacother. 2006;4:161–167. doi: 10.1016/j.amjopharm.2006.06.004. [DOI] [PubMed] [Google Scholar]
- 47.Svetkey LP, George LK, Tyroler HA, Timmons PZ, Burchett BM, Blazer DG. Effects of gender and ethnic group on blood pressure control in the elderly. Am J Hypertens. 1996;9:529–535. doi: 10.1016/0895-7061(96)00026-X. [DOI] [PubMed] [Google Scholar]
- 48.Barker WH, Mullooly JP, Linton KL. Trends in hypertension prevalence, treatment, and control in a well-defined older population. Hypertension. 1998;31:552–559. doi: 10.1161/01.HYP.31.1.552. [DOI] [PubMed] [Google Scholar]
- 49.Prince MJ, Ebrahim S, Acosta D, Ferri CP, Guerra M, Huang Y, et al. Hypertension prevalence, awareness, treatment and control among older people in Latin America, India and China: a 10/66 cross-sectional population-based survey. J Hypertens. 2012;30:177–187. doi: 10.1097/HJH.0b013e32834d9eda. [DOI] [PubMed] [Google Scholar]
- 50.Wing LM, Reid CM, Ryan P, Beilin LJ, Brown MA, Jennings GL, et al. A comparison of outcomes with angiotensin-converting–enzyme inhibitors and diuretics for hypertension in the elderly. N. Engl. J. Med. 2003;348:583–592. doi: 10.1056/NEJMoa021716. [DOI] [PubMed] [Google Scholar]
- 51.Parving H-H, Brenner BM, McMurray JJ, de Zeeuw D, Haffner SM, Solomon SD, et al. Cardiorenal end points in a trial of aliskiren for type 2 diabetes. N. Engl. J. Med. 2012;367:2204–2213. doi: 10.1056/NEJMoa1208799. [DOI] [PubMed] [Google Scholar]
- 52.Gheorghiade M, Böhm M, Greene SJ, Fonarow GC, Lewis EF, Zannad F, et al. Effect of aliskiren on postdischarge mortality and heart failure readmissions among patients hospitalized for heart failure: the ASTRONAUT randomized trial. Jama. 2013;309:1125–1135. doi: 10.1001/jama.2013.1954. [DOI] [PubMed] [Google Scholar]
- 53.Staessen JA, Fagard R, Thijs L, Celis H, Arabidze GG, Birkenhager WH, et al. Randomised double-blind comparison of placebo and active treatment for older patients with isolated systolic hypertension. The Systolic Hypertension in Europe (Syst-Eur) Trial Investigators. The Lancet. 1997;350:757–764. doi: 10.1016/S0140-6736(97)05381-6. [DOI] [PubMed] [Google Scholar]
- 54.Pahor M, Guralnik JM, Ferrucci L, Corti M-C, Salive ME, Cerhan JR, et al. Calcium-channel blockade and incidence of cancer in aged populations. The Lancet. 1996;348:493–497. doi: 10.1016/S0140-6736(96)04277-8. [DOI] [PubMed] [Google Scholar]
- 55.Pahor M, Carbonin P, Guralnik J, Havlik R, Furberg C. Risk of gastrointestinal haemorrhage with calcium antagonists in hypertensive persons over 67 years old. The Lancet. 1996;347:1061–1065. doi: 10.1016/S0140-6736(96)90276-7. [DOI] [PubMed] [Google Scholar]
- 56.Maclure M, Dormuth C, Naumann T, McCormack J, Rangno R, Whiteside C, et al. Influences of educational interventions and adverse news about calcium-channel blockers on first-line prescribing of antihypertensive drugs to elderly people in British Columbia. The Lancet. 1998;352:943–948. doi: 10.1016/S0140-6736(97)11390-3. [DOI] [PubMed] [Google Scholar]
- 57.Larochelle P, Tobe SW, Lacourcière Y. β-Blockers in Hypertension: Studies and Meta-analyses Over the Years. Can. J. Cardiol. 2014;30:S16–S22. doi: 10.1016/j.cjca.2014.02.012. [DOI] [PubMed] [Google Scholar]
- 58.Falaschetti E, Mindell J, Knott C, Poulter N. Hypertension management in England: a serial cross-sectional study from 2011. The Lancet. 1994;2014(383):1912–1919. doi: 10.1016/S0140-6736(14)60688-7. [DOI] [PubMed] [Google Scholar]
- 59.Schäfer H-H, De Villiers JN, Sudano I, Dischinger S, Theus G-R, Zilla P. Dieterle T. Swiss Med Wkly Epub: Recommendations for the treatment of hypertension in the elderly and very elderly–a scotoma within international guidelines; 2012. [DOI] [PubMed] [Google Scholar]
- 60.Psaty BM, Koepsell TD, Yanez ND, Smith NL, Manolio TA, Heckbert SR, et al. Temporal patterns of antihypertensive medication use among older adults, 1989 through 1992: an effect of the major clinical trials on clinical practice? Jama. 1995;273:1436–1438. doi: 10.1001/jama.1995.03520420052037. [DOI] [PubMed] [Google Scholar]
- 61.Alhawassi TM, Krass I, Pont LG. Hypertension in Older Persons: A Systematic Review of National and International Treatment Guidelines. J Clin Hypertens. 2015;17:486–492. doi:10.1111/jch.12536. [DOI] [PMC free article] [PubMed]
- 62.Cranney M, Barton S, Walley T. Addressing barriers to change: an RCT of practice-based education to improve the management of hypertension in the elderly. Br. J. Gen. Pract. 1999;49:522–526. [PMC free article] [PubMed] [Google Scholar]
- 63.Onder G, Gambassi G, Sgadari A, Williamson JD, Cesari M, Landi F, et al. Impact of hospitalization on blood pressure control in Italy: results from the Italian Group of Pharmacoepidemiology in the Elderly (GIFA) Pharmacotherapy: The Journal of human pharmacology and drug therapy. 2003;23:240–247. doi: 10.1592/phco.23.2.240.32087. [DOI] [PubMed] [Google Scholar]
- 64.Eastman P. Antihypertensive prescribing: A survey of general practice supervisors and registrars. Aust Fam Physician. 2008;37:969. [PubMed] [Google Scholar]
- 65.Fotherby M, Harper G, Potter J. General practitioners’ management of hypertension in elderly patients. BMJ [Br. Med. J.] 1992;305:750. doi: 10.1136/bmj.305.6856.750. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Wang PS, Avorn J, Brookhart MA, Mogun H, Schneeweiss S, Fischer MA, et al. Effects of noncardiovascular comorbidities on antihypertensive use in elderly hypertensives. Hypertension. 2005;46:273–279. doi: 10.1161/01.HYP.0000172753.96583.e1. [DOI] [PubMed] [Google Scholar]
- 67.Brindel P, Hanon O, Dartigues J-F, Ritchie K, Lacombe J-M, Ducimetière P, et al. Prevalence, awareness, treatment, and control of hypertension in the elderly: the Three City study. J Hypertens. 2006;24:51–58. doi: 10.1097/01.hjh.0000198028.84353.86. [DOI] [PubMed] [Google Scholar]
- 68.McDonald M, Hertz RP, Unger AN, Lustik MB. Prevalence, awareness, and management of hypertension, dyslipidemia, and diabetes among United States adults aged 65 and older. J Gerontol A Biol Sci Med Sci. 2009;64:256–263. doi: 10.1093/gerona/gln016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Al Ghatrif M, Kuo Y-F, Al Snih S, Raji MA, Ray LA, Markides KS. Trends in hypertension prevalence, awareness, treatment and control in older Mexican Americans, 1993–2005. Ann Epidemiol. 2011;21:15–25. doi: 10.1016/j.annepidem.2010.06.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.De Backer G, Myny K, De Henauw S, Doyen Z, Van Oyen H, Tafforeau J, et al. Prevalence, awareness, treatment and control of arterial hypertension in an elderly population in Belgium. J Hum Hypertens. 1998;12:701–706. doi: 10.1038/sj.jhh.1000695. [DOI] [PubMed] [Google Scholar]
- 71.Monane M, Bohn RL, Gurwitz JH, Glynn RJ, Levin R, Avorn J. The Effects of Initial Drug Choice and Comorbidity on Antihypertensive Therapy Compliance* Results From a Population-Based Study in the Elderly. Am J Hypertens. 1997;10:697–704. doi: 10.1016/S0895-7061(97)00056-3. [DOI] [PubMed] [Google Scholar]
- 72.Hsu Y-H, Mao C-L, Wey M. Antihypertensive Medication Adherence Among Chinese Americans. J Transcult Nurs. 2010;21(4):297–305. doi: 10.1177/1043659609360707. [DOI] [PubMed] [Google Scholar]
- 73.Turner BJ, Hollenbeak C, Weiner MG, Ten Have T, Roberts C. Barriers to adherence and hypertension control in a racially diverse representative sample of elderly primary care patients. Pharmacoepidemiology and Drug Safety. 2009;18:672–681. doi: 10.1002/pds.1766. [DOI] [PubMed] [Google Scholar]
- 74.Krousel-Wood MA, Muntner P, Islam T, Morisky DE, Webber LS. Barriers to and determinants of medication adherence in hypertension management: perspective of the cohort study of medication adherence among older adults. Med. Clin. North Am. 2009;93:753–769. doi: 10.1016/j.mcna.2009.02.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Butt T, Branch R, Beesley L, Martin U. Managing hypertension in the very elderly: effect of adverse drug reactions (ADRs) on achieving targets. J Hum Hypertens. 2010;24:514–518. doi: 10.1038/jhh.2009.116. [DOI] [PubMed] [Google Scholar]
- 76.Sato I, Akazawa M. Polypharmacy and adverse drug reactions in Japanese elderly taking antihypertensives: a retrospective database study. Drug, Healthcare and Patient Safety. 2013;5:143. doi: 10.2147/DHPS.S45347. [DOI] [PMC free article] [PubMed] [Google Scholar]


