Abstract
Objectives:
To conduct a feasibility study to compare concentric and eccentric rotator cuff strengthening exercises for rotator cuff tendinopathy.
Methods:
A total of 11 patients with rotator cuff tendinopathy who were on the waiting list for arthroscopic subacromial decompression surgery were randomised to perform eccentric rotator cuff strengthening exercises, concentric strengthening exercises or no exercises. Patients were evaluated in terms of levels of pain and function using the Oxford Shoulder Score and a Visual Analogue Scale initially, at 4 weeks and at 8 weeks.
Results:
The study design was found to be acceptable to patients and achieved a high level of 86% compliance. The drop-out rate was 0%. Two patients performing eccentric strengthening exercises improved sufficiently to cancel their planned surgery.
Conclusion:
Further research in this area is recommended. The study design was feasible and power calculations have been conducted to aid future research planning.
Keywords: Rotator cuff, tendinopathy, exercise, eccentric, concentric
Introduction
Shoulder pain is common with as many as one in three people experiencing it at some point during their lives.1 Of the many different pathologies that can affect the shoulder, rotator cuff tendinopathy is the most common and is often described using many different terms such as subacromial impingement syndrome, bursitis, tendonitis or tendinosis.1–4
The pathology that affects the rotator cuff is known to be mainly of a degenerative nature although the exact cause of this remains to be fully explained. Many factors seem to be involved such as age and occupation, extrinsic structural changes that may cause mechanical impingement and intrinsic factors such as lack of sufficient blood supply.4,5 This pathology is similar to that affecting other tendons in the body such as the Achilles and patella tendons.6 Evidence suggests that specific eccentric exercise may be useful in treating chronic degenerative tendinopathy,7–9 but to date, there is limited high quality research investigating the rotator cuff specifically.
There are many different conservative treatments that have been suggested and tried in the treatment of rotator cuff tendinopathy. These include simple rest and activity modification, non-steroidal anti-inflammatory drugs, corticosteroid injections and numerous physiotherapy interventions such as exercise, acupuncture and electrotherapy. Systematic reviews of the evidence for such treatments have been performed10 and specific guidelines have been formulated by the British Chartered Society of Physiotherapy.11 In terms of exercise-based treatment, these guidelines recommend a generalised programme of 14 separate exercises to work on flexibility, proprioception and strength of not just the rotator cuff muscles but also the deltoid and scapular stabilisers. This is based on an amalgamation of previous evidence. Each paper that is referenced investigates programmes of multiple exercises. It is unclear, therefore, which of the exercises is most beneficial. Since the 2004 guidelines, further studies12–15 have investigated the use of general programmes of shoulder stretching and strengthening again with significant improvements being demonstrated.
Following a publication by Alfredson et al.,16 the use of specific eccentric strengthening exercises has been popular among physiotherapists for the treatment of degenerative tendinopathy. This study investigated this approach for treating chronic Achilles tendinosis, and there have been numerous subsequent studies that have tried to investigate this approach further for the Achilles and other tendons prone to similar degenerative pathology. At a microscopic level, the proximal hamstrings’ tendon, the common wrist flexors and extensors, the patella tendon, the rotator cuff, biceps brachii and tibialis posterior tendon have all been shown to suffer from such pathology.6,8,9,17,18 The vast majority of these studies investigated eccentric exercises for lower limb tendinopathy; however, some have looked at the common wrist flexors and extensors. Systematic reviews8,9,13 of the evidence for eccentric exercises for degenerative tendinopathy all conclude that it is an effective treatment. It is also important to consider that no adverse effects have been reported from the use of eccentric exercises.19 To date, only three published studies20–22 have investigated specific eccentric exercises for treatment of the rotator cuff. The two Swedish studies20,21 investigated small numbers of patients (10 and 9 patients, respectively), but both found significant improvements in both pain and function. The Belgian study22 included 61 patients to compare a general exercise programme performed with or without additional eccentric exercise. Patients in both groups improved but there were no significant differences in pain or function between the groups. The eccentric group though gained 15% better strength.
Overall, there is a suggestion that eccentric exercises may be beneficial in the treatment of rotator cuff tendinopathy but further research is needed. No direct comparison has yet been made between eccentric and concentric exercises for this pathology.
Specifically, the objectives of the current feasibility study were
To test the feasibility, practicality and acceptability of the study design and protocol;
To evaluate the integrity of the study protocol (e.g. recruitment and retention rates, outcome measurement) to inform a fully powered randomised controlled trials (RCT);
To investigate the acceptability of the intervention and refine prior to a full RCT;
To inform a sample size calculation for a RCT.
Method
The aim was to design a feasible method of comparing the effectiveness of eccentric and concentric exercises for patients with rotator cuff tendinopathy. Subjects were recruited while on the waiting list for arthroscopic subacromial decompression surgery at Derby Hospitals National Health Service (NHS) Foundation Trust. All patients had been assessed by an experienced Orthopaedic Consultant. At the point where patients were offered surgical intervention (i.e. agreed to their name being added to the waiting list), they were given information regarding the study by the lead researcher (M.B.) and invited to participate while waiting for surgery. The trial recruitment period was 6 months and during that time, 14 suitable patients were identified, of which 11 agreed to participate.
Inclusion criteria
Patients who were on the waiting list for a shoulder arthroscopic subacromial decompression surgical procedure.
Sufficient investigations that include clinical assessment findings, x-ray and either diagnostic ultrasound or Magnetic Resonance Imaging to establish the diagnosis of rotator cuff tendinopathy. Short-term favourable response to subacromial corticosteroid injection was also considered diagnostic.
Failed conservative treatment previously such as a corticosteroid injection and/or a course of physiotherapy treatment.
Exclusion criteria
Patients with a history of shoulder fracture or dislocation, previous shoulder surgery, cervical radiculopathy, full thickness rotator cuff tear, glenohumeral joint degeneration, inflammatory arthropathy, significant acromio-clavicular joint arthrosis or large rotator cuff calcifications.
Patients with insufficient ability to understand the English language and hence have full understanding of what was being asked of them. Funding was not available for interpreter services.
Patients with cognitive impairment who may not understand what was required of them.
All participants provided written informed consent having had a minimum of 24 h to consider the implications of the trial. Patients took the patient information home and returned the completed consent form and patient details form via a free post envelope if they wished to go ahead. All personal information was stored securely as per NHS protocol.
On receipt of a completed consent form, patients were randomised blindly by an independent colleague into one of three groups using a ticket out of a hat approach (three tickets – one for each group). Group 1 acted as control and received no treatment. Group 2 was taught a specific concentric rotator cuff strengthening exercise. Group 3 was taught a specific eccentric rotator cuff strengthening exercise. Patients being placed on the waiting list for surgery do not usually have any additional treatment while waiting for surgery; therefore, the control group allocation of no treatment was regarded as standard practice and did not alter the normal patient treatment pathway.
Patients were allocated a unique participation number once it was known to which group they had been assigned. All data collected during the study were labelled by this code rather than the patient’s personal details for reasons of data security and management of personal information.
After randomisation, patients were telephoned and informed whether they had been allocated to an exercise group or no treatment. Patients allocated to one of the exercise groups were invited to attend the Physiotherapy Clinic at a mutually convenient time. They were taught concentric exercises or eccentric exercises dependent on their group allocation. Each participant was given written instruction with diagrams as an aide-memoire. They were also given an instructional film demonstrating the exercises in real time produced by the lead researcher (M.B.) in DVD format that they could use to ensure correct performance of the exercises. The instructions on both the exercise sheets and DVDs were written in such a way as to avoid the use of the words ‘eccentric’ and ‘concentric’ in an attempt to blind patients to which group they had been allocated.
Patients were asked to complete an exercise diary each day to record the number of times that they performed their exercises and number of repetitions performed each session. This information was used to assess compliance.
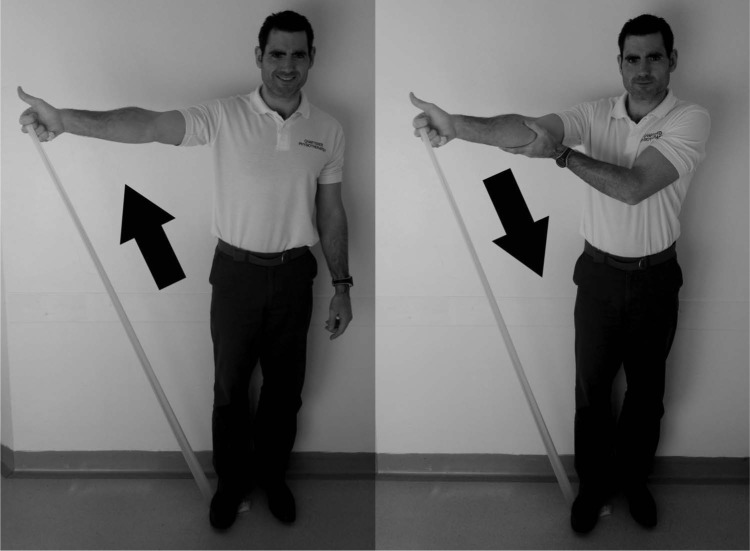
Both the concentric and eccentric exercises were performed with the arm in the same position focussing on strengthening the supraspinatus as this is the most commonly affected part of the rotator cuff in terms of degenerative tendinopathy. Based on the paper by Burke et al.,2 the exercise was performed into ‘full can’ abduction in the plane of the scapula, that is, abduction 30° in front of the coronal plane with the thumb pointing skyward. This position is thought to optimally load the supraspinatus without causing significant mechanical impingement against the acromial arch. Both intervention groups were asked to perform this exercise against the resistance of a yellow grade elastic exercise band provided by the research team. The concentric group was asked to lift the arm slowly over 3 s from 0° to 90° and to lower it back quickly (1 s) with the weight of the limb taken by the other arm (Figure 1). The eccentric group was asked to assist the arm using the other hand to take its weight up to 90° and lower it back slowly to 0° (Figure 2). Patients were asked to perform three sets of 15 repetitions twice a day over the trial period of 8 weeks. Patients were advised to expect some pain when performing the exercise and this was acceptable as long as the patient did not regard it as severe and that it did not persist for longer than 1 hour after completing the exercises.
Figure 1.
A demonstration of the concentric exercise technique.
Figure 2.
A demonstration of the eccentric exercise technique.
Patients were invited to telephone the lead researcher (M.B.) if they experienced any problems although none actually did. Patients in exercise groups had a review appointment with the lead researcher (M.B.) in the Physiotherapy Clinic 4 weeks after commencing the trial. It was felt that reviewing patients in the clinic more frequently than once every 4 weeks might have a negative effect on compliance if they had to arrange appointments around work or had to travel a long distance. At the 4-week appointment, the amount of resistance used for the exercise groups was increased as a treatment progression provided there had been no deterioration in symptoms. This was done by giving the patient the next grade of resistance of elastic exercise band (coloured red).
The outcome measures used were the Oxford Shoulder Score (OSS; 12–60 version, with 12 indicating no pain and normal function) and pain measured on a 100-mm Visual Analogue Scale (VAS; 0 indicating no pain). These were assessed initially, after 4 weeks and after 8 weeks. For the exercise groups, this was done in person at the initial and 4-week appointments but all other assessments were posted out to the patients for completion and were returned in a stamped self-addressed envelope. The research team were not blinded to the outcome scores in the exercise groups as this information was used to assess whether exercises could be progressed to higher resistance at 4 weeks. Compliance was measured using the patients’ exercise diary.
Results
The baseline age demographic of patients in each group was similar with mean ages of 55, 53 and 52 years in the respective control, concentric and eccentric groups. There were six men and five women, but unfortunately, due to chance, they were not evenly distributed with the control group 75% male, concentric group 100% male and eccentric group 100% female.
The outcomes are shown in Table 1. Two patients (CON002 and ECE001) did not complete the 8-week trial period due to being offered surgery earlier than expected as a result of other patients cancelling their operations. In both cases, the data recorded up to the 4-week period were included in the results and statistical analysis. No patients withdrew from the trial due to adverse reaction or their own volition.
Table 1.
Raw result data.
| Patient code | Oxford Shoulder Score |
VAS |
|||||
|---|---|---|---|---|---|---|---|
| Start | 4 weeks | 8 weeks | Start | 4 weeks | 8 weeks | ||
| CON001 | 28 | 29 | 27 | 49 | 43 | 34 | |
| CON002 | 26 | 25 | X | 77 | 87 | X | Surgery at week 6 |
| CON003 | 25 | 28 | 28 | 35 | 44 | 46 | |
| CON004 | 34 | 34 | 34 | 78 | 79 | 74 | |
| CCE001 | 23 | 27 | 30 | 51 | 72 | 76 | |
| CCE002 | 29 | 23 | 23 | 34 | 34 | 35 | |
| CCE003 | 20 | 22 | 20 | 42 | 66 | 44 | |
| ECE001 | 33 | 32 | X | 66 | 48 | X | Surgery at week 7 |
| ECE002 | 27 | 23 | 21 | 36 | 49 | 22 | Cancelled surgery |
| ECE003 | 34 | 24 | 38 | 68 | 25 | 85 | Cancelled surgery |
| ECE004 | 42 | 45 | 34 | 42 | 60 | 19 | |
| ANOVA (p value) | 0.083 | 0.428 | 0.443 | 0.443 | 0.465 | 0.890 | |
VAS: Visual Analogue Scale; CON: control group; CCE: concentric exercise group; ECE: eccentric exercise group; X: not recorded; ANOVA: analysis of variance.
Descriptive and inferential statistical analysis of the data was performed using IBM SPSS Statistics (v16.0) and was verified by a medical statistician. An unrelated one-way analysis of variance (ANOVA) was performed (5% confidence interval) assuming the data to be parametric. No statistical differences were observed between the groups in either the OSS or the VAS outcome measures at the start, at 4 or 8 weeks.
Following completion of the trial, nine patients underwent their planned surgery. Two patients allocated to the eccentric exercise group subsequently cancelled their operations due to improvements in symptoms as a result of the trial.
Compliance of patients was measured using the self-reported exercise diary. Compliance was expressed as a percentage where 100% was the completion of 3 × 15 repetitions of the exercise every day for 8 weeks, that is, 5040 repetitions in total. Five of the patients in the exercise groups returned their diaries. The mean compliance of those patients that completed the exercise diary was 86%.
Discussion
During the 6 months, only 14 suitable patients meeting the inclusion criteria were identified with a recruitment rate of 79%. When planning the study, the surgical waiting list for the previous 6 months was reviewed and 36 potential patients were identified. Unfortunately, due to natural fluctuations in caseload, this was not the case during the trial and fewer numbers were recruited than expected. This highlights the difficulty of predicting recruitment rates for research as historical data may not reflect current trends.
The usual patient pathway locally involves referral from a General Practitioner for physiotherapy treatment and then referral to an Orthopaedic Consultant for surgical opinion if insufficient improvements have been made. The reason for selecting patients while on the waiting list for surgery was to be able to justify the use of a control group of patients who had no treatment at all as per the normal pathway. Potentially more patients could have been selected earlier in the pathway but a different control method would have to have been used for ethical reasons.
The outcome measures used were found to have been appropriate. As expected, the VAS and OSS scores for the control group did not fluctuate significantly over the 8-week period. As the data were available, statistical analysis of the results was performed but did not show any statistically significant differences between the control and concentric exercise or eccentric exercise groups. With such low participant numbers, this was never likely but there was a trend towards improvement in the eccentric exercise group. Following the trial, two patients in the eccentric exercise group decided to cancel their planned surgery. One patient (ECE002) did this at 8 weeks and the other (ECE003) decided to continue the exercises for longer and cancelled at 12 weeks. The results appear distorted because ECE003 described a dramatic improvement at 4 weeks, so she returned to more vigorous daily and sporting activities. This aggravated her symptoms again, so at 8 weeks, the outcome scores appear much worse. By continuing the exercises for beyond the 8 weeks, she then improved again and cancelled surgery. If a longer follow-up period had been used, the results may, therefore, have shown a more obvious trend and may have been more significant. From both a patient and a cost–benefit perspective, the most important outcome measure was that surgery was not required in two cases. These findings echo those of Jonsson et al.21 who found that patients who had already tried other forms of conservative treatment could still benefit from specific eccentric strengthening exercise and avoid undergoing surgery.
All patients participating in the study had previously had a course of physiotherapy treatment involving the prescription of shoulder exercises. The fact that two patients should respond so well to further exercise treatment stands out. It is uncertain whether this relates to the exercise itself, the frequency and repetitions of the exercise or the high level of compliance achieved during the trial.
The research method design yielded high levels of compliance from those patients that did participate suggesting the acceptability of the intervention to patients. There was a 0% drop-out rate. However, the lack of numbers of patients recruited was the main limitation of the study. If future trials in this area of research are to be conducted, then efforts should be made to include more appropriate patients either by an extended study timescale or by selection from a wider geographical area, that is, a multi-centre study. As an aim of the study was to inform a sample size calculation for an adequately powered study, power calculations using the result data suggested that 86 patients in each of the three groups would be required to achieve significance before allowing for drop-out (90% power, 5% significance level and using half the standard deviation of change in OSS). This would suggest that a 12-centre study over 1 year would be required to achieve these numbers, although it is acknowledged that some centres are more prolific than ours in terms of numbers of arthroscopic subacromial decompression surgeries. An alternative would be to recruit patients earlier in the pathway to compare eccentric and concentric exercises, but a control group receiving no treatment would be difficult to justify ethically as this is not standard practice.
There is a lack of large-scale studies investigating specific shoulder exercises in the treatment of rotator cuff tendinopathy. Of those that do exist, the majority use a wide array of exercises over different timescales with no consistency in terms of the specific types of exercises and repetitions. Recent studies20–22 have added weight to support the use of eccentric strengthening exercises but overall patient participant numbers are low. To date no published studies have compared eccentric and concentric strengthening exercises of the shoulder. With such small numbers in this study no definitive conclusions can be drawn but feasibility of the research method was established.
Conclusion
Although the results of this small study did not show statistically significant differences in outcome measures, two patients in the eccentric exercise group did improve sufficiently so that they cancelled their planned arthroscopic shoulder surgery. The small sample size included in the study means that no definitive conclusions can be drawn from these results but there is an implication that eccentric exercise may be of benefit.
A further adequately powered trial would allow comparison between no treatment, concentric strengthening and eccentric strengthening. Certainly further research is required in this area of physiotherapy for this pathology.
Practical implications
Evidence to support eccentric exercise for rotator cuff tendinopathy
An appropriate design for a large-scale study
Power calculation for planning further investigation
Acknowledgments
The authors would like to thank Consultant Orthopaedic Surgeons Messrs David Clark, Tim Cresswell, Marius Espag and Amol Tambe for including their patients in this study; Apostolos Fakis for statistical support; Sarah Stewart for modelling for the exercise DVD; and Ben Smith for modelling for the photographs.
Footnotes
Declaration of conflicting interests: There were no conflicts of interest.
Ethical approval: Ethical approval was granted by the Trent Research and Ethics Committee. Reference number: 10/H0405/20.
Funding: The University of Nottingham sponsored and insured the study as part of a higher degree. The small cost of consumables was funded by the lead author (M.B.). No external funding was used.
Research and development approval: R&D approval was granted by Derby Hospitals NHS Foundation Trust. Reference number: DHRD/2010/015.
References
- 1. Lewis JS. Rotator cuff tendinopathy. Br J Sports Med 2009; 43: 236–241. [DOI] [PubMed] [Google Scholar]
- 2. Burke WS, Vangsness CT, Powers CM. Strengthening the supraspinatus: a clinical and biomechanical review. Clin Orthop Relat Res 2002; 402: 292–298. [PubMed] [Google Scholar]
- 3. Lewis JS. Rotator cuff tendinopathy/subacromial impingement syndrome: is it time for a new method of assessment? Br J Sports Med 2009; 43: 259–264. [DOI] [PubMed] [Google Scholar]
- 4. Mehta S, Gimbel JA, Soslowsky LJ. Etiologic and pathogenetic factors for rotator cuff tendinopathy. Clin Sports Med 2003; 22: 791–812. [DOI] [PubMed] [Google Scholar]
- 5. Uhthoff HK, Sano H. Pathology of failure of the rotator cuff tendon. Orthop Clin North Am 1997; 28(1): 31–41. [DOI] [PubMed] [Google Scholar]
- 6. Kraushaar BS, Nirschl RP. Current concepts review – tendinosis of the elbow (tennis elbow). Clinical features and findings of histological, immunohistochemical and electron microscopy studies. J Bone Joint Surg 1999; 81: 259–278. [PubMed] [Google Scholar]
- 7. Andres BM, Murrell GA. Treatment of tendinopathy: what works, what does not, and what is on the horizon. Clin Orthop Relat Res 2008; 466(7): 1539–1554. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Wasielewski NJ, Kotsko KM. Does eccentric exercise reduce pain and improve strength in physically active adults with symptomatic lower extremity tendinosis? A systematic review. J Athl Train 2007; 42(3): 409–421. [PMC free article] [PubMed] [Google Scholar]
- 9. Woodley BL, Newsham-West RJ, Baxter GD. Chronic tendinopathy: effectiveness of eccentric exercise. Br J Sports Med 2007; 41: 188–199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Grant HJ, Arthur A, Pichora DR. Evaluation of interventions for rotator cuff pathology: a systematic review. J Hand Ther 2004; 17: 274–299. [DOI] [PubMed] [Google Scholar]
- 11. Hanchard N, Cummins J, Jeffries C. Evidence-based clinical guidelines for the diagnosis, assessment and physiotherapy management of shoulder impingement syndrome. London: Chartered Society of Physiotherapy, 2004. [Google Scholar]
- 12. Bennell K, Wee E, Coburn S, et al. Efficacy of standardised manual therapy and home exercise programme for chronic rotator cuff disease: randomised placebo controlled trial. BMJ. Epub ahead of print 8 June 2010. DOI: 10.1136/bmj.c2756. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Camargo PR, Haik MN, Ludewig PM, et al. Effects of strengthening and stretching exercises applied during working hours on pain and physical impairment in workers with subacromial impingement syndrome. Physiother Theory Pract 2009; 25(7): 463–475. [DOI] [PubMed] [Google Scholar]
- 14. Lombardi R, Jr, Magri AG, Fleury AM, et al. Progressive resistance training in patients with shoulder impingement syndrome: a randomized controlled trial. Arthritis Rheum 2008; 59(5): 615–622. [DOI] [PubMed] [Google Scholar]
- 15. Roy J-S, Moffet H, Herbert LJ, et al. Effect of motor control and strengthening exercises on shoulder function in persons with impingement syndrome: a single-subject study design. Man Ther 2009; 14: 180–188. [DOI] [PubMed] [Google Scholar]
- 16. Alfredson H, Pietilä T, Jonsson P, et al. Heavy-load eccentric calf muscle training for the treatment of chronic Achilles tendinosis. Am J Sports Med 1998; 26(3): 360–366. [DOI] [PubMed] [Google Scholar]
- 17. Rees JD, Wilson AM, Wolman RL. Current concepts in the management of tendon disorders. Rheumatology (Oxford) 2006; 45: 508–521. [DOI] [PubMed] [Google Scholar]
- 18. Rees JD, Wolman RL, Wilson AM. Eccentric exercises; why do they work, what are the problems and how can we improve them? Br J Sports Med 2009; 43: 242–246. [DOI] [PubMed] [Google Scholar]
- 19. Maffulli N, Longo UG, Denaro V. Novel approaches for the management of tendinopathy. J Bone Joint Surg 2010; 92: 2604–2613. [DOI] [PubMed] [Google Scholar]
- 20. Bernhardsson S, Klintberg IH, Wendt GK. Evaluation of an exercise concept focusing on eccentric strength training of the rotator cuff for patients with subacromial impingement syndrome. Clin Rehabil 2011; 25(1): 69–78. [DOI] [PubMed] [Google Scholar]
- 21. Jonsson P, Wahlstrom P, Ohberg L, et al. Eccentric training in chronic painful impingement syndrome of the shoulder: results of a pilot study. Knee Surg Sports Traumatol Arthrosc 2006; 14(1): 76–81. [DOI] [PubMed] [Google Scholar]
- 22. Maenhout A, Mahieu N, De Muynck M, et al. Does adding heavy load eccentric training to rehabilitation of patients with unilateral subacromial impingement result in better outcome? A randomized, clinical trial. Knee Surg Sports Traumatol Arthrosc. Epub ahead of print 12 May 2012. DOI: 10.1007/s00167-012-2012-8. [DOI] [PubMed] [Google Scholar]