Abstract
Objectives
To determine how frequently physicians identify and address overweight/obesity in hospitalized children and to compare physician documentation across training level (medical student, intern, resident, attending).
Study design
We conducted a retrospective chart review. Using an administrative database, Centers for Disease Control and Prevention body mass index calculator, and random sampling technique, we identified a study population of 300 children aged 2–18 years with overweight/obesity hospitalized on the general medical service of a tertiary care pediatric hospital. We reviewed admission, progress, and discharge notes to determine how frequently physicians and physician trainees identified (documented in history, physical exam, or assessment) and addressed (documented in hospital or discharge plan) overweight/obesity.
Results
Physicians and physician trainees identified overweight/obesity in 8.3% (n = 25) and addressed it in 4% (n = 12) of 300 hospitalized children with overweight/obesity. Interns were most likely to document overweight/obesity in history (8.3% of the 266 patients they followed). Attendings were most likely to document overweight/obesity in physical examination (8.3%), assessment (4%), and plan (4%) of the 300 patients they followed. Medical students were least likely to document overweight/obesity including it in the assessment (0.4%) and plan (0.4%) of the 244 hospitalized children with overweight/obesity they followed.
Conclusions
Physicians and physician trainees rarely identify or address overweight/obesity in hospitalized children. This represents a missed opportunity for both patient care and physician trainee education.
Identification of overweight/obesity by physicians is associated with healthy weight counseling, treatment of comorbid conditions, and healthier patient and family lifestyle choices.1–4 The American Academy of Pediatrics and other organizations have recommended body mass index (BMI) calculations and universal overweight/obesity screening during preventive visits for patients over 2 years of age.5,6 There are no similar recommendations for overweight/obesity in the inpatient setting.
An acute hospital admission presents an important opportunity to identify and address overweight/obesity. Prior studies show that parents of hospitalized children wish to be told if their child is found to have overweight/obesity.7,8 Parents also believe that action should be taken with the majority identifying the inpatient physician as the person who should address weight concerns.7
Despite this, limited information exists about inpatient physician identification and management of pediatric overweight/obesity.8,9 Previous studies have reported that BMI calculations are seldom performed during hospitalization8–11 and that overweight/obesity is rarely included among discharge diagnoses.9–12
The primary goal of the study was to determine how frequently physicians identify and address overweight/obesity in hospitalized children. The secondary goal was comparison of physician documentation across training level (medical student, intern, senior resident, and attending). Our primary hypothesis was that physicians rarely identify or address overweight/obesity in hospitalized children. Our secondary hypothesis was that attendings identify and address overweight/obesity with greater frequency than trainees.
Methods
We conducted the study at Primary Children’s Hospital (PCH), a 289-bed freestanding pediatric hospital affiliated with the University of Utah, School of Medicine. With more than 12 000 admissions annually, PCH serves as the primary pediatric hospital for Salt Lake County and a tertiary referral center for Utah, Wyoming, Montana, Idaho, and Nevada. The patient population at PCH is similar to other large academic pediatric hospitals in terms of volume, socioeconomic status, and subspecialties. PCH is the inpatient pediatric training site for University of Utah medical students and residents from several programs. The University of Utah institutional review board and the Intermountain Healthcare privacy board approved the study.
We examined the medical records of children 2–18 years of age with overweight/obesity admitted to the PCH general medical service between January 1 and December 31, 2010. Per hospital protocol, nursing staff documented height and weight in the electronic health record (EHR) for all patients. The BMI and BMI percentile for age/sex were then automatically calculated and available in the EHR. Our primary goal was to determine the percentage of hospitalized children with overweight/obesity for whom physicians identified and addressed overweight/obesity. Our secondary outcome was comparison of overweight/obesity documentation by physician training levels.
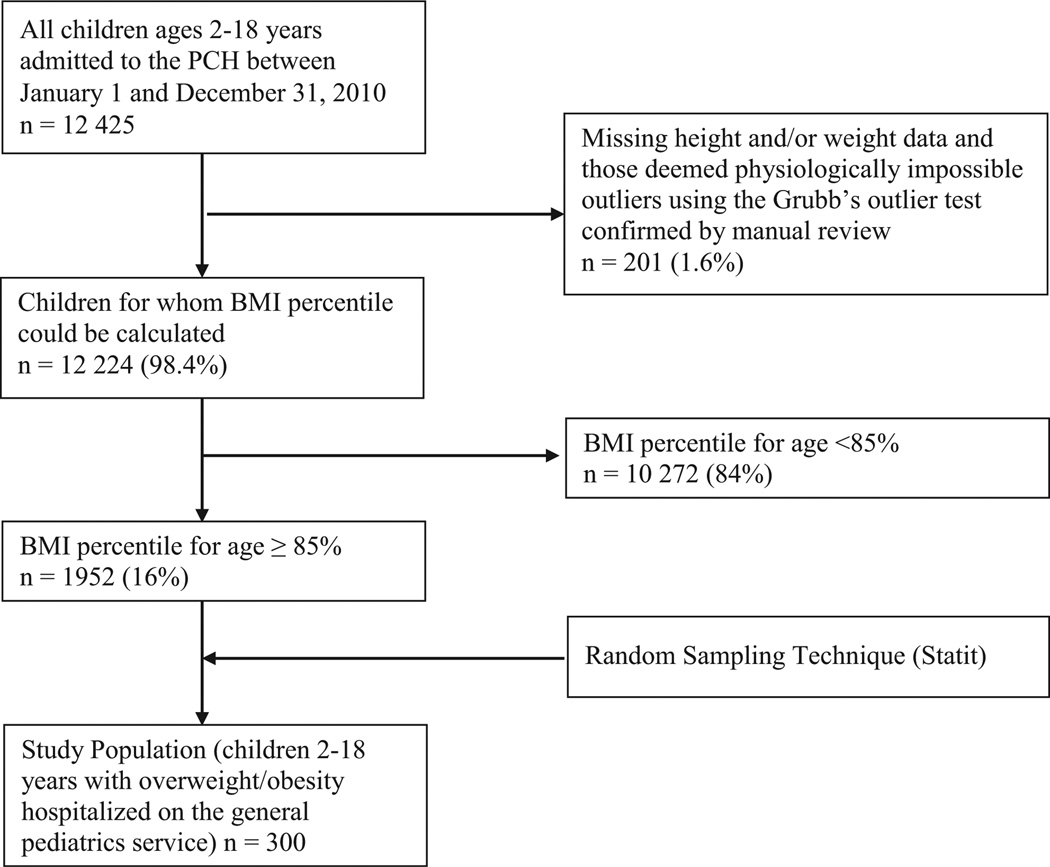
We extracted patient age, sex, weight, height, race, primary hospital service, length of stay, and discharge diagnoses from the Intermountain Healthcare Enterprise Data Warehouse: an integrated, searchable administrative database that stores over 8 million patient encounters and includes clinical, laboratory, and radiologic data from all inpatient and outpatient Intermountain Healthcare facilities.13 We restricted the search to patients admitted to the PCH general medical service and excluded records with missing weight and/or height (n = 56) and those deemed physiologically impossible outliers by Grubbs outlier test followed by individual inspection of each outlier to confirm they should be excluded based on age, weight, and height (n = 145)14 (Figure 1; available at www.jpeds.com). Next, we calculated BMI z-score and corresponding percentile for age and sex using the Centers for Disease Control and Prevention BMI calculator15 and selected patients with BMI at or above the 85th percentile (based on BMI z-score ≥1.4395) to include only those with overweight or obesity. We then used a random number sampling technique in Statit (Corvallis, Oregon) to select our study population of 300 children with overweight/obesity hospitalized on the general pediatric service.
Figure 1.
Patient selection.
We reviewed admission, progress, and discharge notes written by medical students, interns, senior residents, and attendings. We assessed documentation of overweight/obesity in: (1) history (diet, physical activity, screen time, family history of overweight/obesity); (2) physical examination (BMI, BMI percentile for age/sex, physical examination findings); (3) assessment; and (4) plan (inpatient nutrition consultation, diet counseling by physician team, laboratory studies discussed or ordered, activity counseling by physician team, referral to primary care physician, referral to weight management program).We extracted the training level of each note’s author (student, intern, resident, attending) and examined total documentation for a given patient by combining items noted by any member of the physician team (medical student, intern, resident, or attending) at any point during the hospitalization (admission, progress, or discharge notes). In cases where supervising physicians edited and co-signed trainee notes, we used the EHR history function to track information entered by each provider.
Statistical Analyses
We used descriptive statistics to characterize the study population and overall physician documentation frequency. We performed Holm-Šídák multiple comparisons test as a follow-up to 1-way ANOVA to compare documentation across physician level of training.16 Statistical significance was set at P < .05. Analyses were conducted with GraphPad Prism (GraphPad Software, Inc, San Diego, California).
Results
Sixteen percent of children 2–18 years of age hospitalized on the PCH general pediatric service had overweight or obesity. Median age of patients in our study was 9 years (IQR: 9). Fifty-three percent (n = 159) were male, 43% (n = 130) had overweight, and 57% (n = 170) had obesity. Of the patients with obesity, 3.7% (n = 11) met criteria for extreme obesity with BMI ≥99th percentile for age/sex.6 Seventy-one percent (n = 214) were Caucasian and 19% (n = 56) Hispanic (Table I; available at www.jpeds.com). The demographic characteristics of our study population of 300 randomly selected hospitalized patients with overweight/obesity were similar to known hospital demographics based on internal PCH data. We reviewed 1560 admission, progress, and discharge notes written for 300 hospitalized patients with overweight/obesity. All patients had documented attending notes. Eighty-one percent (n = 244) had medical student, 83% (n = 250) intern, and 89% (n = 267) resident notes within the EHR allowing for duplicate notes per patient.
Table I.
Patient characteristics
| Variables | |
|---|---|
| Median age (y) | 9 (IQR: 9) |
| Female | 47% (n = 141) |
| With overweight (BMI: 85%–94%) | 43% (n = 130) |
| With obesity (BMI ≥95%) | 57% (n = 170) |
| With extreme obesity (BMI ≥99% for age/sex) | 3.7% (n = 11) |
| Race | |
| Caucasian | 71% (n = 214) |
| Hispanic | 19% (n = 56) |
| Unknown | 5% (n = 14) |
| African American | 3% (n = 10) |
| Native American | 1% (n = 3) |
| Other | 1% (n = 3) |
| Median-length of stay (d) | 2 (IQR: 3) |
| Common discharge diagnoses | |
| Asthma | 15% (n = 45) |
| Pneumonia | 15% (n = 45) |
| Bronchiolitis | 4.7% (n = 14) |
| Cellulitis | 4.3% (n = 13) |
| Influenza or other flu-like illness | 4.3% (n = 13) |
| Dehydration | 2.7% (n = 8) |
| Poisoning | 2% (n = 6) |
| Attending service | |
| Hospitalist | 71% (n = 213) |
| Community | 29% (n = 87) |
Twenty-five (8.3%) of 300 hospitalized children with overweight/obesity had documentation of overweight/obesity (history, physical examination, or assessment) written by any member of the physician team (medical student, intern, senior, or attending) at some point during the hospitalization (admission, progress note, or discharge). None of the patients had overweight/obesity included among their discharge diagnoses. Physicians and physician trainees documented overweight/obesity most commonly in physical examination 8.3% (n = 25) and diet history 8% (n = 24) (Table II). The most likely time to document overweight/obesity in history and physical examination was on admission while the most common time to include overweight/obesity in the assessment was during subsequent hospital day progress notes.
Table II.
Frequency of physicians and physician trainee overweight/obesity documentation in hospitalized children with overweight/obesity*
| Overweight and obese patients (n = 300) |
||
|---|---|---|
| % | n | |
| Overall identification | 8.3 | 25 |
| History | 8 | 24 |
| Diet | 8 | 24 |
| Physical activity | 1.7 | 5 |
| Screen time | 0.7 | 2 |
| Family history | 0.7 | 2 |
| Physical examination | 8.3 | 25 |
| BMI | 5.3 | 16 |
| BMI percentile for age/sex | 2.7 | 8 |
| Physical examination findings | 8.3 | 25 |
| Assessment | 4.3 | 13 |
| Overall management | 4 | 12 |
| Hospital plan | 4 | 12 |
| Inpatient nutrition consultation | 2.7 | 8 |
| Diet counseling by physician team | 2 | 6 |
| Laboratory evaluation (discussed or ordered) | 1.7 | 5 |
| Activity counseling by physician team | 0.7 | 2 |
| Discharge plan | 0.7 | 2 |
| Referral to weight management program | 0.7 | 2 |
| Referral to primary care physician | 0.7 | 2 |
Items documented by any physician or physician trainee (medical student, intern, senior, or attending) involved in the care of the patient at any point during his/her hospitalization (admission, progress note, or discharge).
Twelve (4%) of 300 hospitalized children with overweight/obesity had documentation of a plan (hospital or discharge) to address overweight/obesity written by any member of the physician team (medical student, intern, senior, or attending) at some point during the hospitalization (admission, progress note, or discharge). Most common ways of addressing overweight/obesity were inpatient nutrition consultation (2.7%, n = 8) and dietary counseling by the physician team (2%, n = 8) (Table II). The most common time to document plans to address overweight/obesity was in subsequent hospital day progress notes. Only patients with overweight/obesity documented in the assessment had a care plan to address overweight/obesity.
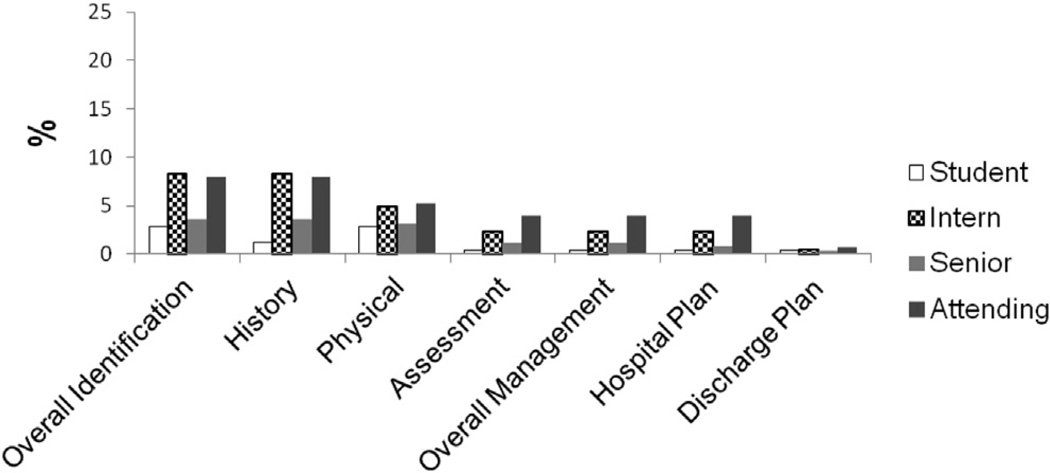
Figure 2 shows differences in the documentation associated with level of training. Interns and attendings were most likely to document overweight/obesity in history (8.3% of the 266 patients interns followed; 8.3% of the 300 patients for attendings) and physical (7.9% and 8.3%, respectively). Attendings were most likely to document overweight/obesity in assessment (4%). Frequency of including overweight/obesity in the hospital or discharge plan was very low and did not differ by physician training level. Medical students were least likely to document overweight/obesity including it in the assessment and plan of only 1 (0.4%) of the 244 hospitalized children with overweight/obesity they followed.
Figure 2.
Percentage of hospitalized children with overweight/obesity in whom physicians and physician trainees documented overweight/obesity. Items documented by specific physician and physician trainee providers (medical student, intern, resident, attending) involved in the care of the patient at any point during his/her hospitalization (admission, progress note, or discharge). Total overweight/obesity identification, history, and physical exam were documented more frequently by attendings and interns (P < .05). Assessment was documented more frequently by attendings (P < .05). Overweight/obesity management, hospital plan, and discharge plan documentation did not differ by physician training level.
Discussion
Previous studies of hospitalized children with overweight/obesity had small sample sizes8 and performed EHR queries for the terms “overweight” or “obesity” within physician notes without specifying whether these were included as part of the examination, assessment, or plan and which physician provider was performing the documentation.9 Our findings can be used to improve patient care because they identify specific areas of documentation that need improvement.
The 16% prevalence of overweight/obesity among hospitalized children is slightly lower than the 20.4% prevalence of pediatric overweight/obesity in Utah17 and is potentially secondary to conditions resulting in acute and/or chronic weight loss among hospitalized children. Physician documentation of overweight/obesity risk factors in the history for only 8% of hospitalized patients with overweight/obesity was lower than rates previously reported for outpatient well visits.1–3 Similar to outpatient visits, the most common overweight/obesity risk factor documented by physicians was diet. The default general physical examination phrase “well developed, well nourished” was used almost universally. Although BMI percentile for age/sex was available within the EHR for all patients, abnormal results were not “flagged;” a mechanism for automatically “flagging” abnormal growth values, having BMI percentile auto-populate directly into inpatient admission, progress, and discharge notes, as well as a drop-down menu with options from cachectic to obese to describe general physical examination may offer mechanisms to increase both awareness and appropriate documentation.
Overall, we found the low proportion of physician documentation of overweight/obesity differed slightly from previous studies. Physicians and physician trainees in our study documented overweight/obesity on physical examination (8.3%) and assessment (4.3%) of patients with overweight/obesity compared with 0% found in an Australian study8 and 13.2% in an American study.9 This difference likely reflects lower numbers of patients with overweight/obesity (12/102) in the Australian study8 and inclusion of only patients 8–18 years, who are more likely to be identified than children less than 5 years of age,18 in the American study.9 Whether physicians noted overweight/obesity as part of physical examination or assessment in the prior study was not specified.9
Physicians and physician trainees addressed overweight/obesity in hospital or discharge plans for 12 (4%) of the 300 hospitalized children with overweight/obesity. Likely barriers cited by outpatient pediatricians19 such as perceived lack of patient and family interest, sense of treatment futility, and lack of clinician time apply to the hospital setting. Barriers unique to the inpatient setting might include lack of guidelines specific for the hospital setting, lack of continuity with patients and families, perception that the responsibility lies with the child’s primary care provider, lack of knowledge regarding outpatient resources especially for families living further away from a tertiary care hospital, the perception that acute illness hospitalization is not the right time to address chronic health concerns, and mistaken7,8 belief that patients and families do not wish to address overweight/obesity during an acute illness hospitalization. Some physicians may not be aware that overweight/obesity are reimbursable diseases in Utah. In the inpatient setting overweight/obesity would be secondary conditions that would increase complexity and coding level when appropriately documented. Furthermore, time spent providing overweight/obesity counseling or resources would also count toward time spent on direct patient care and coordination of care.
Frequency of addressing overweight/obesity during the hospitalization (4%) and specifically percentage of patients for whom a nutrition consult was performed (2.7%) were lower in our study compared with rates reported by both O’Connor (4.8%)10 and Sleeper (24%).11 This is likely, at least in part, a reflection of hospital protocol.
At PCH a nutrition consult occurred only if ordered by a physician whereas it was automatic for all children with weights ≥95th percentile in the Sleeper study.11 The mechanism for nutrition referral was not specified by O’Connor.10
Lack of overweight/obesity recognition and management among inpatient physicians of all training levels is not only against the wishes of families of hospitalized children7,8 but also concerning in terms of physician trainee education. Education about obesity treatment for pediatric residents has been shown to improve patient outcomes in the outpatient setting.20 We are not aware of a similar study in the inpatient setting.
Limitations of this study were that data were collected at a single academic center and relied on physician documentation. It is possible that some physicians actually addressed overweight/obesity without documenting it in the medical record and that some documented plans for interventions that they did not carry out. In addition, sequential documentation with note attestations has the potential of overestimating the performance of supervisory physicians who “received credit” for information in notes they edited and attested.
Reversal of the rising prevalence of obesity requires a multifaceted approach with community partnerships and interventions directed at health care settings (including development of guidelines for inpatient treatment), schools, and communities.21 Future studies should focus on developing practice guidelines for identifying and addressing overweight/obesity in hospitalized children.
Acknowledgments
N.M. supported by National Heart, Lung, and Blood Institute (HL092069).
The authors are grateful for critical reviews provided by Paul Young, Debra Zand, Donna Halloran (supported by National Heart, Lung, and Blood Institute [HD061484-01]), and Sarah Halbern.
Glossary
- BMI
Body mass index
- EHR
Electronic health record
- PCH
Primary Children’s Hospital
Footnotes
The authors declare no conflicts of interest.
References
- 1.Barlow SE, Bobra SR, Elliott MB, Brownson RC, Haire-Joshu D. Recognition of childhood overweight during health supervision visits: does BMI help pediatricians? Obesity (Silver Spring) 2007;15:225–232. doi: 10.1038/oby.2007.535. [DOI] [PubMed] [Google Scholar]
- 2.Patel AI, Madsen KA, Maselli JH, Cabana MD, Stafford RS, Hersh AL. Underdiagnosis of pediatric obesity during outpatient preventive care visits. Acad Pediatr. 2010;10:405–409. doi: 10.1016/j.acap.2010.09.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Dilley KJ, Martin LA, Sullivan C, Seshadri R, Binns HJ. Identification of overweight status is associated with higher rates of screening for comorbidities of overweight in pediatric primary care practice. Pediatrics. 2007;119:e148–e155. doi: 10.1542/peds.2005-2867. [DOI] [PubMed] [Google Scholar]
- 4.Perrin EM, Jacobson Vann JC, Benjamin JT, Skinner AC, Wegner S, Ammerman AS. Use of a pediatrician toolkit to address parental perception of children’s weight status, nutrition, and activity behaviors. Acad Pediatr. 2010;10:274–281. doi: 10.1016/j.acap.2010.03.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Krebs NF, Jacobson MS. Prevention of pediatric overweight and obesity. Pediatrics. 2003;112:424–430. doi: 10.1542/peds.112.2.424. [DOI] [PubMed] [Google Scholar]
- 6.Barlow SE. Expert committee recommendations regarding the prevention, assessment, and treatment of child and adolescent overweight and obesity: summary report. Pediatrics. 2007;120(Suppl 4):S164–S192. doi: 10.1542/peds.2007-2329C. [DOI] [PubMed] [Google Scholar]
- 7.Bradford K, Kihlstrom M, Pointer I, Cockrell Skinner A, Slivka P, Perrin E. Parental attitudes toward obesity and overweight screening and communication for hospitalized children. Hosp Pediatr. 2012;2:126–132. doi: 10.1542/hpeds.2011-0036. [DOI] [PubMed] [Google Scholar]
- 8.McLean K, Wake M, McCallum Z. Overweight in medical paediatric inpatients: detection and parent expectations. J Paediatr Child Health. 2007;43:256–261. doi: 10.1111/j.1440-1754.2007.01056.x. [DOI] [PubMed] [Google Scholar]
- 9.Azhdam DB, Reyhan I, Grant-Guimaraes J, Feinstein R. Prevalence and documentation of overweight and obesity in hospitalized children and adolescents. Hosp Pediatr. 2014;4:377–381. doi: 10.1542/hpeds.2014-0040. [DOI] [PubMed] [Google Scholar]
- 10.O’Connor J, Youde LS, Allen JR, Hanson RM, Baur LA. Outcomes of a nutrition audit in a tertiary paediatric hospital: implications for service improvement. J Paediatr Child Health. 2004;40:295–298. doi: 10.1111/j.1440-1754.2004.00367.x. [DOI] [PubMed] [Google Scholar]
- 11.Sleeper EJ, Ariza AJ, Binns HJ. Do hospitalized pediatric patients have weight and blood pressure concerns identified? J Pediatr. 2009;154:213–217. doi: 10.1016/j.jpeds.2008.08.009. [DOI] [PubMed] [Google Scholar]
- 12.Woo JG, Zeller MH, Wilson K, Inge T. Obesity identified by discharge ICD-9 codes underestimates the true prevalence of obesity in hospitalized children. J Pediatr. 2009;154:327–331. doi: 10.1016/j.jpeds.2008.09.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Evans RS, Lloyd JF, Pierce LA. Clinical use of an enterprise data warehouse. AMIA Annu Symp Proc. 2012;2012:189–198. [PMC free article] [PubMed] [Google Scholar]
- 14.Grubbs F. Procedures for detecting outlying observations in samples. Technometrics. 1969;11:1–21. [Google Scholar]
- 15.Centers for Disease Control and Prevention BMI Calculator. [Accessed January 1, 2011]; http://nccd.cdc.gov/dnpabmi/Calculator.aspx.
- 16.Glantz SA. Primer of biostatistics. New York: McGraw-Hill, Medical Publicatin Division; 2002. [Google Scholar]
- 17.Overweight and Obesity. [Accessed August 22, 2014]; http://www.cdc.gov/obesity/stateprograms/fundedstates/pdf/utah-state-profile.pdf.
- 18.O’Brien SH, Holubkov R, Reis EC. Identification, evaluation, and management of obesity in an academic primary care center. Pediatrics. 2004;114:e154–e159. doi: 10.1542/peds.114.2.e154. [DOI] [PubMed] [Google Scholar]
- 19.Story MT, Neumark-Stzainer DR, Sherwood NE, Holt K, Sofka D, Trowbridge FL, et al. Management of child and adolescent obesity: attitudes, barriers, skills, and training needs among health care professionals. Pediatrics. 2002;110(1 Pt 2):210–214. [PubMed] [Google Scholar]
- 20.Stahl CE, Necheles JW, Mayefsky JH, Wright LK, Rankin KM. 5-4-3-2-1 go! Coordinating pediatric resident education and community health promotion to address the obesity epidemic in children and youth. Clin Pediatr (Phila) 2011;50:215–224. doi: 10.1177/0009922810385106. [DOI] [PubMed] [Google Scholar]
- 21.de la Torre A, Sadeghi B, Green RD, Kaiser LL, Flores YG, Jackson CF, et al. Ninos Sanos, Familia Sana: Mexican immigrant study protocol for a multifaceted CBPR intervention to combat childhood obesity in two rural California towns. BMC Public Health. 2013;13:1033. doi: 10.1186/1471-2458-13-1033. [DOI] [PMC free article] [PubMed] [Google Scholar]