Abstract
Objective
To document a case series of 8 young First Nations patients diagnosed with acute rheumatic fever (ARF), a preventable disease that resulted in the death of 2 patients, in northwestern Ontario in the context of late diagnosis, overcrowded housing, and inadequate public health response.
Design
Retrospective case series over an 18-month period.
Setting
Remote First Nations communities in northwestern Ontario.
Participants
Eight patients with ARF.
Main outcome measures
Incidence, mortality, residual rheumatic heart disease, time to diagnosis, barriers to diagnosis and treatment, housing situation of patients, patient demographic characteristics (age, sex), and investigation results.
Results
The incidence of ARF in this population was 21.3 per 100 000, which is 75 times greater than the overall Canadian estimated incidence. The average patient age was 9.4 years. Most cases developed joint findings, and 5 of the surviving patients had rheumatic heart disease when they received echocardiography. The average time to diagnosis was 88 days. Two 4-year-old children died from ARF. Most patients lived in inadequate and crowded housing.
Conclusion
This rare disease still exists in remote First Nations communities. These communities demonstrate an incidence equal to that in aboriginal communities in Australia and New Zealand, which have among the highest international incidence of ARF. Primordial prevention, including improved on-reserve housing, is urgently needed. Case detection and ongoing surveillance for primary and secondary prophylaxis requires a well resourced regional strategy.
Résumé
Objectif
Documenter une série de cas dans laquelle 8 jeunes patients des Premières Nations ont souffert de rhumatisme articulaire aigu (RAA), une maladie évitable qui a entraîné la mort de 2 patients dans le Nord-Ouest de l’Ontario, dans un contexte de diagnostic tardif, de logis surpeuplés et d’une réponse inadéquate de la santé publique.
Type d’étude
Étude rétrospective d’une série de cas sur une période de 18 mois.
Contexte
Des communautés éloignées des Premières Nations dans le Nord-Ouest de l’Ontario.
Participants
Huit patients ayant présenté un RAA.
Principaux paramètres à l’étude
Incidence, mortalité, maladie rhumatismale cardiaque résiduelle, délai dans le diagnostic, obstacles au diagnostic et au traitement, état du logis des patients, caractéristiques démographiques des patients (âge, sexe) et résultats de l’investigation.
Résultats
L’incidence du RAA dans cette population était de 21,3 par 100 000, soit 75 fois l’incidence estimée pour l’ensemble du Canada. Les patients avaient en moyenne, 9,4 ans. La plupart des cas ont développé des signes articulaires; chez 5 des survivants, l’échographie a révélé une maladie rhumatismale cardiaque. Il a fallu en moyenne 88 jours pour poser le diagnostic. Deux enfants de 4 ans sont morts du RAA. La plupart des patients vivaient dans des logements inadéquats et surpeuplés.
Conclusion
Cette maladie rare existe encore dans certaines communautés éloignées des Premières Nations. Dans ces communautés, l’incidence est égale à celle de communautés aborigènes de l’Australie et de la Nouvelle-Zélande où l’incidence du RAA est parmi les plus élevées au monde. Il y a un urgent besoin de prévention primordiale, incluant une amélioration des logements dans les réserves. La détection des cas et une surveillance constante pour assurer les prophylaxies primaire et secondaire exigeront des mesures régionales dotées d’excellentes ressources.
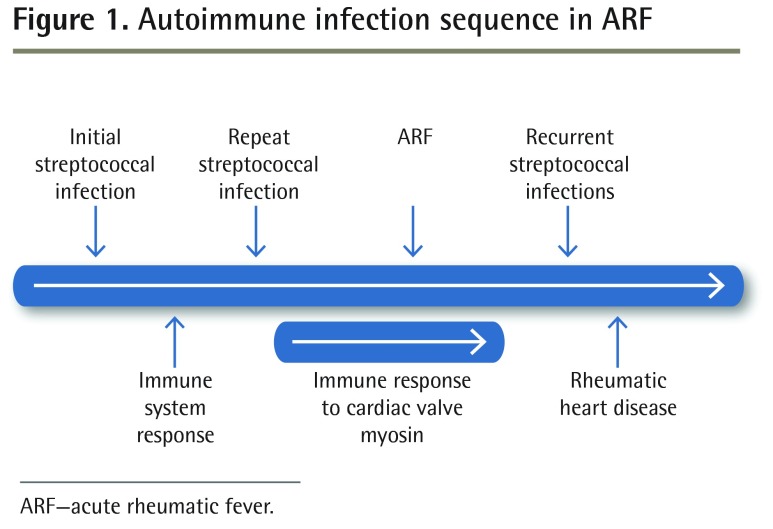
Acute rheumatic fever (ARF) is the immunologic sequela to untreated group A streptococcal (GAS) infection; it primarily affects children and has lifelong consequences1,2 (Figure 1). As the leading cause of acquired heart disease globally, incidence of rheumatic fever is often an indicator of the health status of a population.3 It is clearly linked to socioeconomic determinants, such as poverty and overcrowded housing, and it highlights the health inequities facing indigenous communities in high-income countries such as Canada, Australia, and New Zealand.4–8
Figure 1.
Autoimmune infection sequence in ARF
ARF—acute rheumatic fever.
While thought to be a disease of the past in Canada, ARF continues to present at an alarming rate in northwestern Ontario.9 In 2009, local physicians published a case series of 5 cases over 36 months at the Sioux Lookout Meno Ya Win Health Centre in Ontario.9 This review further documents a series of 8 cases of ARF over an 18-month period among First Nations youth and young adults from the Sioux Lookout region.
METHODS
Cases were identified by the authors and communicated to them by colleagues. Chart reviews were completed for cases diagnosed between September 1, 2013, and March 1, 2015, including information from hospital electronic records, physician primary care electronic medical records, and nursing notes from the community nursing stations. When examined, 5 years of hospital admission and discharge diagnostic code records provided no new cases and rarely referenced the 8 known cases, as the recorded diagnosis for most cases was typically one of the presenting Jones criteria and not the eventual diagnosis of ARF. The diagnosis was typically arrived at in an outpatient setting after test results were completed.
Community and specialist consultant physicians for the cases were contacted as needed to clarify case presentation and management details. General housing information was obtained from publicly available Statistics Canada data sets. Case-specific housing details were collected by community representatives. Consistency with the First Nations OCAP (ownership, control, access, possession) principles was assessed and ethics approval was granted by the Sioux Lookout Meno Ya Win Health Centre Research Review and Ethics Committee.
In January 2015, an ad hoc Acute Rheumatic Heart Disease Working Group was established to examine these new cases. Representatives from Health Canada, Sioux Lookout First Nations Health Authority, Sioux Lookout Meno Ya Win Health Centre, the University of Ottawa Department of Infectious Diseases, and the Anishinaabe Bimaadiziwin Research Program were included. This working group ensured case detection was accurate and that treatment, investigation, secondary prophylaxis, and documentation were undertaken in these known cases.
RESULTS
In a catchment area of 25 000 primarily First Nations patients in 31 remote communities, 8 cases of ARF were identified in the 18-month period from September 1, 2013, to March 1, 2015 (Table 1).10 One case was diagnosed and another was confirmed postmortem, with ARF listed as the cause of death. The remaining cases were confirmed using the Jones criteria. Patients ranged in age from 3 to 20 years (mean 9.4) and originated from 5 different communities. One patient had a previous history of rheumatic fever.
Table 1.
Patient characteristics
| CHARACTERISTIC | PATIENT 1 | PATIENT 2 | PATIENT 3 | PATIENT 4 | PATIENT 5 | PATIENT 6 | PATIENT 7 | PATIENT 8 |
|---|---|---|---|---|---|---|---|---|
| Age, y | 4 | 4 | 20 | 3 | 12 | 8 | 15 | 9 |
| Sex | Male | Female | Female | Female | Female | Female | Female | Male |
| Sore throat | No | Yes | Yes | NA | Yes | Yes | No | No |
| Time from presentation to diagnosis, d | NA* | 240 | 4 | 43 | 43 | 70 | 140 | 77 |
| Outcome | Deceased | Deceased | CHF, RHD | CHF, RHD | Chorea | CHF, RHD | RHD | RHD |
CHF—congestive heart failure, NA—not available, RHD—rheumatic heart disease.
Diagnosis was made post mortem.
Patients initially presented with cardiac signs and symptoms (n = 3), arthritis (n = 2), and chorea (n = 1), and 5 of the 8 patients developed transient arthritis during the course of their illness. The average time to diagnosis for the 6 surviving patients was 88 days (range 4 to 240). Four patients had preceding pharyngitis and received treatment for positive findings of GAS infection. Three patients were originally misdiagnosed with conditions including juvenile rheumatoid arthritis and septic arthritis.
Identified risk factors included inadequate or crowded housing in many of the cases involved. One patient had a wound swab positive for GAS before ARF, and 1 patient had spent time in the local women’s crisis shelter with family around the time of infection. All patients had access to nursing station health care 24 hours a day, 7 days a week. Several of the communities involved had in-community physicians, while others had monthly, week-long doctor visits.
Death attributable to rheumatic fever occurred in 2 cases. Rheumatic heart disease (RHD) was diagnosed in 5 of the surviving patients, with documentation of moderate to severe valvular dysfunction. Initiating secondary prophylaxis with penicillin was delayed in several cases. The reasons for delay included the patient not being registered under the Indian Act and as such not having coverage with the Non-Insured Health Benefits program, as well as limited community follow-up following discharge from tertiary hospitals.
All patients had up-to-date immunizations. The annual incidence rate for ARF was calculated to be 21.3 per 100 000.
DISCUSSION
Minimal data on ARF in Canada exist, and it is largely considered to be a disease of the past. A prospective review by the Canadian Paediatric Surveillance Program between 2004 and 2007 found an incidence of 2.9 cases per million population per year for those aged 0 to 19.11 In comparison, the incidence for the Sioux Lookout region in this case series was nearly 75 times higher, with 21.3 cases per 100 000 population. This incidence is likely an underestimate. Rheumatic fever is not a reportable illness in Ontario, and no other formal surveillance systems exist. In addition, physicians are unfamiliar with the diagnosis and are likely to miss cases.
Globally, ARF remains prevalent in low-income countries and marginalized indigenous communities in high-income countries.12 The incidence of ARF among First Nations children and youth in the Sioux Lookout region is consistent with indigenous populations in Northern Australia and New Zealand—both of which demonstrate among the highest reported rates in the world.13,14 In 2010, the incidence of ARF was reported to be 26 per 100 000 in the Northern Territories of Australia.13 Similar rates of 24 per 100 000 are found among Maori children aged 5 to 14 in New Zealand.14,15
Unlike Canada, both Australia and New Zealand have committed to addressing the health inequity of ARF in indigenous children. Both countries have national and state-level rheumatic fever strategies that incorporate surveillance, prevention, and ongoing facilitation of secondary prophylaxis. In addition, there is explicit recognition of the contribution of crowded housing conditions and socioeconomic deprivation.16 In contrast, a coordinated response to the ARF crisis in northwestern Ontario is impeded by the lack of accountability toward First Nations child health, rooted in jurisdictional complexities across all levels of government for public health service delivery on reserves.
Surveillance and prevention
There is an immediate need for the establishment of a surveillance system for timely detection and diagnosis of cases of ARF and for monitoring trends in the Sioux Lookout region. While rheumatic fever is not a notifiable disease in Canada or Ontario, it is reportable in many US states, as well as in Australia and New Zealand. Given the potentially increasing and undocumented incidence of this preventable disease in northwestern Ontario, as well as the profound consequences in terms of age of onset and the severity and complexity of the lifelong consequences, we advocate for Ontario to add ARF to the list of reportable diseases. Additionally, other regional surveillance mechanisms such as active case finding or the establishment of a regional registry should be pursued. This requires dedicated resources and commitment from both federal and provincial public health authorities to establish an effective regional program.
Effective ARF control programs integrate features of primordial, primary, and secondary prevention. Rheumatic fever is inextricably linked to the social determinants of health, and primordial prevention addresses the underlying behavioural, social, and environmental conditions that contribute to the acquisition and spread of GAS infections. The overall decrease in ARF in high-income countries has long been attributed to improved determinants such as housing, nutrition, and access to primary care.17 A 2010 New Zealand–sponsored systematic review of 34 international studies concluded that there is an association between crowded and poor-quality housing and rates of ARF.4,18
Remote First Nations populations in Ontario continue to face a housing crisis that undoubtedly puts them at risk of poor health outcomes including rheumatic fever (Table 2).19–23 The Ontario results of the First Nations Regional Health Survey in 2008 to 2010 described living conditions for some First Nations people on reserve.20 Overall, 93.5% of adult respondents indicated that they lived in households in need of general or major repair.20 Relative to the general Canadian population, Statistics Canada census data from 2006 reported that First Nations people on reserve had the highest rate of over-crowding and were 4 times more likely to live in homes in need of major repairs.21 Housing improvement strategies are key components of primordial prevention programs in New Zealand.4 A similar approach is needed to address ARF in the Sioux Lookout region.
Table 2.
Canadian on-reserve housing
Primary prevention attempts to prevent the development of ARF by ensuring appropriate antibiotic treatment of GAS infections.24 Approaches involve early identification and treatment of GAS pharyngitis through school- and community-based programs, improved access to primary care, and education of health care providers.14 This incorporates both community-level and targeted education campaigns. Following the recognition of an increased number of ARF cases in Sioux Lookout, educational sessions have been coordinated by local care providers targeting physicians and community health nurses. However, primary care on reserve suffers from a lack of continuity in front-line providers, which has led to inconsistent approaches to GAS pharyngitis. Ongoing educational and treatment protocols that recognize this as a high-risk region for ARF are needed. Investigation pathways in Australia and New Zealand propose treatment with penicillin while lengthy investigations are undertaken, and investigations with negative results in suspected cases are routinely repeated in 2 to 4 weeks’ time to ensure thorough case detection. As both pharyngitis and carditis might be silent, a high index of suspicion and common treatment and follow-up pathway are needed.25–27
Secondary prevention targets progression or worsening of known ARF disease. Chemoprophylaxis with monthly administration of benzathine penicillin G has been shown to be both clinically effective and cost-effective.14,28 An ARF recurrence rate of 10% exists in the 5-year period following the initial episode.27 In areas with high disease frequency, such as New Zealand, secondary prophylaxis is recommended for 10 years, compared with the 5-year Canadian recommendation. Without recurrences the carditis might improve in subsequent years but it will worsen with repeat incidences of ARF.25 In our study, the ARF working group discovered that registration under the federal Indian Act was not up to date for several participants. This meant they could not get prescriptions filled under their treaty rights by the First Nations and Inuit Health Branch benefits program. We learned that there was an 18-month backlog in processing such applications already filed. We further learned that registration for health insurance benefits both provincially and federally presented substantial administrative and cultural hurdles for First Nations children and their families. This creates more potential barriers to appropriately funded transportation, treatment, and follow-up for this life-threatening disease. While the ARF working group has been able to expedite this process for current ARF patients, urgent transition to a system where registration can easily be initiated at the hospital at birth is needed. Leaving a vulnerable population of First Nations children uninsured is unacceptable. The recent Auditor General of Canada’s 2015 report recognized how critical such registration is, as it enables funded medical transportation: “First Nations individuals who are denied access to medical transportation benefits may not be able to receive health services that are only available outside of their community.”29
Diagnosis of ARF is difficult if it is not routinely included in the differential diagnosis of children presenting with inflamed joints in a region with a high incidence of ARF. In our series, 1 case was diagnosed and another case was confirmed post mortem. Overall, there was an average delay in diagnosis from first presentation of 88 days. Physicians should be mindful of this diagnosis when assessing migratory polyarthritis or new, undocumented cardiac murmurs in aboriginal children or other groups at risk.
With this case series and the establishment of a temporary working group, the provision of secondary prophylaxis has been more vigilant, and all 6 surviving cases are receiving prophylaxis. While effective advocacy by local physicians reestablished penicillin on the list of drug benefits covered by the Non-Insured Health Benefits program without a special access request, a coordinated patient care follow-up mechanism has yet to be established.
Registries for ARF and RHD in Australia and New Zealand have been shown to improve appropriate case follow-up and facilitation of secondary prophylaxis.14,25 The Sioux Lookout First Nations Health Authority currently administers a successful tuberculosis program, which performs case detection and ongoing management of tuberculosis. A similar regional service for ARF would be beneficial, as ARF and its sequela, RHD, are lifelong issues, often requiring anticoagulation, cardiology follow-up, and timely surgical intervention as required. It is important to rethink our approach to pharyngitis in our region in order to ensure timely management of streptococcal pharyngitis.
Limitations
As this disease is not reportable, case detection was by word of mouth. Other cases might have gone unrecognized and our estimate might underreport actual disease incidence.
Conclusion
The documentation of 8 cases of rheumatic fever within an 18-month time frame in remote First Nations communities in northwestern Ontario is very concerning. It represents a clear indication of the ongoing contribution of social determinants of health and persistent health inequities that exist in this region. Deficient and overcrowded housing is not a benign social condition. While the ad hoc Acute Rheumatic Heart Disease Working Group has been effective, the high rate of ARF requires an organized ongoing strategy and permanent oversight by both the public health and primary care systems. An accountability to First Nations children’s health is clearly needed. We advocate for immediate action on the establishment of a surveillance system and a coordinated approach to primordial, primary, and secondary prevention.
Our case series serves to demonstrate, as detailed by the Auditor General of Canada, that “Health Canada has not adequately managed its support of access to health services for remote First Nations.”29 This community-based research also highlights areas identified by the recent Truth and Reconciliation Commission in which we must “close the gaps in health outcomes between Aboriginal and non-Aboriginal communities.”30 Action is urgently needed.
EDITOR’S KEY POINTS
Acute rheumatic fever (ARF) is generally thought to be a disease of the past in high-income countries like Canada, yet it continues to present at an alarming rate in northwestern Ontario. The incidence is approximately 75 times that in the general Canadian population.
This retrospective case series detected 8 cases of ARF in an 18-month period in the Sioux Lookout region of Ontario. Two of the patients died, and 5 of the surviving patients developed rheumatic heart disease, with documentation of moderate to severe valvular dysfunction. Diagnosis was generally delayed, as was secondary prophylaxis in several of the cases.
The authors identify an urgent need for a robust regional ARF strategy incorporating primordial prevention, addressing the social determinants of health, particularly inadequate and crowded housing; primary prevention, improving early diagnosis and treatment of group A streptococcal infection; and secondary prevention, removing barriers to accessing secondary prophylaxis.
POINTS DE REPÈRE DU RÉDACTEUR
On croit généralement que le rhumatisme articulaire aigu (RAA) est une entité du passé dans les pays industrialisés comme le Canada et pourtant, il continue d’être présent à un taux alarmant dans le Nord-Ouest de l’Ontario où son incidence est environ 75 fois celle de la population canadienne générale.
Cette étude rétrospective a trouvé 8 cas de RAA sur une période de 18 mois dans la région de Sioux Lookout en Ontario. Deux des patients sont décédés et cinq des survivants ont développé une maladie cardiaque rhumatismale avec des troubles valvulaires de modérés à sévères. Le diagnostic était généralement tardif et dans plusieurs cas, la prophylaxie secondaire retardait également.
Les auteurs estiment qu’il est urgent de mettre en place une stratégie régionale intensive concernant le RAA, qui porterait d’abord surla prévention vitale qui tiendrait compte des déterminants sociaux de la santé, notamment les logis surpeuplés et inadéquats; sur la prévention primaire, permettant un diagnostic et un traitement précoces des infections au streptocoque du groupe A; et sur la prévention secondaire, en éliminant les facteurs qui empêchent d’avoir accès à la prophylaxie secondaire.
Footnotes
This article has been peer reviewed.
Cet article fait l’objet d’une révision par des pairs.
Contributors
All authors contributed to the concept and design of the study; data gathering, analysis, and interpretation; and preparing the manuscript for submission.
Competing interests
None declared
References
- 1.Seckeler MD, Hoke TR. The worldwide epidemiology of acute rheumatic fever and rheumatic heart disease. Clin Epidemiol. 2011;3:67–84. doi: 10.2147/CLEP.S12977. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Guilherme L, Kalil J. Rheumatic fever and rheumatic heart disease: cellular mechanisms leading to autoimmune reactivity and disease. J Clin Immunol. 2010;30(1):17–23. doi: 10.1007/s10875-009-9332-6. Epub 2009 Oct 3. [DOI] [PubMed] [Google Scholar]
- 3.World Heart Federation [website] Rheumatic heart disease. Geneva, Switz: World Heart Federation; Available from: www.world-heart-federation.org/press/fact-sheets/rheumatic-heart-disease. Accessed 2015 Apr 7. [Google Scholar]
- 4.New Zealand Guidelines Group . RapidE: rheumatic fever: a systematic review of the literature on health literacy, overcrowding and rheumatic fever. Wellington, NZ: New Zealand Guidelines Group; 2011. Available from: www.health.govt.nz/system/files/documents/publications/rf20systematic20review20w20nz20case20studies20included.pdf. Accessed 2015 Apr 7. [Google Scholar]
- 5.Jaine R, Baker M, Venugopal K. Acute rheumatic fever associated with household crowding in a developed country. Pediatr Infect Dis J. 2011;30(4):315–9. doi: 10.1097/INF.0b013e3181fbd85b. [DOI] [PubMed] [Google Scholar]
- 6.Kerdemelidis M, Lennon DR, Arroll B, Peat B, Jarman J. The primary prevention of rheumatic fever. J Paediatr Child Health. 2010;46(9):534–48. doi: 10.1111/j.1440-1754.2010.01854.x. [DOI] [PubMed] [Google Scholar]
- 7.Kurahara DK, Grandinetti A, Galario J, Reddy DV, Tokuda A, Langan S, et al. Ethnic differences for developing rheumatic fever in a low-income group living in Hawaii. Ethn Dis. 2006;16(2):357–61. [PMC free article] [PubMed] [Google Scholar]
- 8.Steer AC, Carapetis JR, Nolan TM, Shann F. Systematic review of rheumatic heart disease prevalence in children in developing countries: the role of environmental factors. J Paediatr Child Health. 2002;38(3):229–34. doi: 10.1046/j.1440-1754.2002.00772.x. [DOI] [PubMed] [Google Scholar]
- 9.Madden S, Kelly L. Update on acute rheumatic fever. It still exists in remote communities. Can Fam Physician. 2009;55:475–8. [PMC free article] [PubMed] [Google Scholar]
- 10.Walker R, Cromarty H, Kelly L, St Pierre-Hansen N. Achieving cultural safety in aboriginal health services: implementation of a cross-cultural safety model in a hospital setting. Divers Health Care. 2009;6(1):11–22. [Google Scholar]
- 11.Canadian Paediatric Surveillance Program. 2007 Results. Ottawa, ON: Canadian Paediatric Society, Public Health Agency of Canada; Available from: www.cpsp.cps.ca/uploads/publications/Results-2007.pdf. Accessed 2015 Apr 7. [Google Scholar]
- 12.Steer AC, Carapetis JR, Nolan TM, Shann F. Systematic review of rheumatic heart disease prevalence in children in developing countries: the role of environmental factors. J Paediatr Child Health. 2002;38(3):229–34. doi: 10.1046/j.1440-1754.2002.00772.x. [DOI] [PubMed] [Google Scholar]
- 13.Australian Institute of Health and Welfare . Rheumatic heart disease and acute rheumatic fever in Australia: 1996–2012. Cardiovascular disease series. Canberra, Aust: Australian Institute of Health and Welfare; 2013. Cat. no. CVD 60. [Google Scholar]
- 14.Webb R, Wilson N. Rheumatic fever in New Zealand. J Paediatr Child Health. 2013;49(3):179–84. doi: 10.1111/j.1440-1754.2011.02218.x. Epub 2011 Nov 3. [DOI] [PubMed] [Google Scholar]
- 15.Parnaby MG, Carapetis JR. Rheumatic fever in indigenous Australian children. J Paediatr Child Health. 2010;46(9):527–33. doi: 10.1111/j.1440-1754.2010.01841.x. [DOI] [PubMed] [Google Scholar]
- 16.ARF/RHD Writing Group . The Australian guideline for prevention, diagnosis and management of acute rheumatic fever and rheumatic heart disease. 2nd ed. Perth, Aust: National Heart Foundation of Australia, Cardiac Society of Australia and New Zealand; 2012. Available from: www.rhdaustralia.org.au/sites/default/files/guideline_0.pdf. Accessed 2015 Apr 2. [Google Scholar]
- 17.Von Schirndning Y. Health in sustainable development planning: the role of indicators. Geneva, Switz: World Health Organization; 2002. Available from: www.who.int/mediacentre/events/IndicatorsChapter3.pdf?ua=1. Accessed 2015 Aug 28. [Google Scholar]
- 18.Steer A, Colquhoun S, Noonan S, Kado J, Viale S, Carapetis J. Control of rheumatic heart disease in the Pacific region. Pac Health Dialog. 2006;13(2):49–55. [PubMed] [Google Scholar]
- 19.Proceedings of the Standing Senate Committee on Aboriginal Peoples. Issue 1, 2nd session, 41st Parliament. 2013 Nov 26. Ottawa, ON: Parliament of Canada; 2013. Available from: http://publications.gc.ca/collections/collection_2014/sen/yc28/YC28-412-1.pdf. Accessed 2015 Aug 31. [Google Scholar]
- 20.First Nations Information Governance Centre . First Nations Regional Health Survey (RHS) phase 2 (2008/10) Ontario region final report. Ontario region report on the adult, youth and children living in First Nations communities. Toronto, ON: Chiefs of Ontario; 2012. Available from: http://health.chiefs-of-ontario.org/sites/default/files/files/First%20Nations%20Regional%20Health%20Survey%20%28RHS%29%20Phase%202%20%2808-10%29%20Ontario%20Region%20Final%20Report%2012nov01v8.pdf. Accessed 2015 Apr 1. [Google Scholar]
- 21.Statistics Canada . 2006 Census: aboriginal peoples in Canada in 2006: Inuit, Métis and First Nations, 2006 census: First Nations people. Ottawa, ON: Statistics Canada; 2006. Available from: www12.statcan.ca/census-recensement/2006/as-sa/97-558/p18-eng.cfm. Accessed 2015 Aug 28. [Google Scholar]
- 22.Assembly of First Nations . Structural transformation & critical investments in First Nations on the path to shared prosperity. Pre-budget submission, 2011. A submission to the House of Commons Standing Committee on Finance. Ottawa, ON: Assembly of First Nations; 2011. Available from: www.afn.ca/uploads/files/2011-pre-budget-submission.pdf. Accessed 2015 Aug 28. [Google Scholar]
- 23.Proceedings of the Standing Senate Committee on Aboriginal Peoples, Issue 3, 2nd session, 41st Parliament. 2014 Jan 29. Ottawa, ON: Parliament of Canada; 2014. Available from: http://publications.gc.ca/collections/collection_2014/sen/yc28/YC28-412-3.pdf. Accessed 2015 Aug 31. [Google Scholar]
- 24.Gerber MA, Baltimore RS, Eaton CB, Gewitz M, Rowley AH, Shulman ST, et al. Prevention of rheumatic fever and diagnosis and treatment of acute streptococcal pharyngitis: a scientific statement from the American Heart Association Rheumatic Fever, Endocarditis, and Kawasaki Disease Committee of the Council on Cardiovascular Disease in the Young, the Interdisciplinary Council on Functional Genomics and Translational Biology, and the Interdisciplinary Council on Quality of Care and Outcomes Research: endorsed by the American Academy of Pediatrics. Circulation. 2009;119(11):1541–51. doi: 10.1161/CIRCULATIONAHA.109.191959. [DOI] [PubMed] [Google Scholar]
- 25.Veasy LG, Tani LY, Daly JA, Korgenski K, Milner L, Bale J, et al. Temporal association of mucoid strains of Streptococcus pyogenes with a continuing high incidence of rheumatic fever in Utah. Pediatrics. 2004;113(3 Pt 1):e168–72. doi: 10.1542/peds.113.3.e168. [DOI] [PubMed] [Google Scholar]
- 26.Stollerman GH. Rheumatic fever in the 21st century. Clin Infect Dis. 2001;33(6):806–14. doi: 10.1086/322665. Epub 2001 Aug 13. [DOI] [PubMed] [Google Scholar]
- 27.Williamson L, Bowness P, Mowat A, Ostman-Smith I. Lesson of the week: difficulties in diagnosing acute rheumatic fever—arthritis may be short lived and carditis silent. BMJ. 2000;320(7231):362–5. doi: 10.1136/bmj.320.7231.362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Rémond MG, Hodder SY, Nelson MC, Martin J, Nelson C, Atkinson D, et al. Variability in disease burden and management of rheumatic fever and rheumatic heart disease in two regions of tropical Australia. Intern Med J. 2013;43(4):386–93. doi: 10.1111/j.1445-5994.2012.02838.x. [DOI] [PubMed] [Google Scholar]
- 29.Auditor General of Canada . Report 4—access to healthcare services for remote First Nations communities. Ottawa, ON: Auditor General of Canada; 2015. Available from: www.oag-bvg.gc.ca/internet/English/att__e_40382.html. Accessed 2015 Apr 21. [Google Scholar]
- 30.Honouring the truth, reconciling for the future. Summary of the final report of the Truth and Reconciliation Commission of Canada. Winnipeg, MB: Truth and Reconciliation Commission; 2015. Available from: www.trc.ca/websites/trcinstitution/File/2015/Honouring_the_Truth_Reconciling_for_the_Future_July_23_2015.pdf. Accessed 2015 Jun 2. [Google Scholar]