Abstract
Background
Dysphagia is associated with aspiration, pneumonia and malnutrition, but remains challenging to identify at the bedside. A variety of exam protocols and maneuvers are commonly used, but the efficacy of these maneuvers is highly variable.
Methods
We conducted a comprehensive search of seven databases, including MEDLINE, EMBASE and Scopus, from each database’s earliest inception through June 5th, 2013. Studies reporting diagnostic performance of a bedside examination maneuver compared to a reference gold standard (videofluoroscopic swallow study [VFSS] or flexible endoscopic evaluation of swallowing with sensory testing [FEEST]) were included for analysis. From each study, data were abstracted based on the type of diagnostic method and reference standard study population and inclusion/exclusion characteristics, design and prediction of aspiration.
Results
The search strategy identified 38 articles meeting inclusion criteria. Overall, most bedside examinations lacked sufficient sensitivity to be used for screening purposes across all patient populations examined. Individual studies found dysphonia assessments, abnormal pharyngeal sensation assessments, dual axis accelerometry, and one description of water swallow testing to be sensitive tools, but none were reported as consistently sensitive. A preponderance of identified studies was in post-stroke adults, limiting the generalizability of results.
Conclusions
No bedside screening protocol has been shown to provide adequate predictive value for presence of aspiration. Several individual exam maneuvers demonstrated reasonable sensitivity, but reproducibility and consistency of these protocols was not established. More research is needed to design an optimal protocol for dysphagia detection.
Keywords: Bedside swallow, videofluoroscopy, dysphagia, aspiration, systematic review
Introduction
Dysphagia is a serious medical condition that can lead to aspiration pneumonia, malnutrition, and dehydration.1 Dysphagia is the result of a variety of medical etiologies, including stroke, traumatic brain injury, progressive neurologic conditions, head and neck cancers, and general deconditioning. Prevalence estimates for dysphagia vary depending upon the etiology and patient age, but estimates as high as 38% for lifetime prevalence have been reported in those over age 65.2
In order to avoid adverse health outcomes, early detection of dysphagia is essential. In hospitalied patients, early detection has been associated with reduced risk of pneumonia, decreased length of hospital stay, and improved cost-effectiveness resulting from a reduction in hospital days due to fewer cases of aspiration pneumonia.3–5 Stroke guidelines in the U.S. recommend screening for dysphagia for all patients admitted with stroke.6 Consequently, the majority of screening procedures have been designed for and tested in this population.7–10
The videofluoroscopic swallow study (VFSS) is a commonly accepted “reference standard” instrumental evaluation technique for dysphagia as it provides the most comprehensive information regarding anatomic and physiologic function for swallowing diagnosis and treatment. Flexible endoscopic evaluation of swallowing (FEES) is also available as are several less commonly used techniques (scintigraphy, manometry, and ultrasound). Due to availability, patient compliance, and expertise needed, it is not possible to perform instrumental examination on every patient with suspected dysphagia. Therefore, a number of minimally invasive bedside screening procedures for dysphagia have been developed.
The value of any diagnostic screening test centers on performance characteristics which, under ideal circumstances, include a positive result for all those who have dysphagia (sensitivity) and negative result for all those who do not have dysphagia (specificity). Such an ideal screening procedure would reduce unnecessary referrals and testing, thus resulting in cost savings, more effective utilization of speech-language pathology consultation services, and less unnecessary radiation exposure. In addition, an effective screen would detect all those at risk for aspiration pneumonia in need of intervention. However, most available bedside screening tools are lacking in some or all of these desirable attributes.11, 12 We undertook a systematic review and meta-analysis of bedside procedures to screen for dysphagia.
METHODS
Data Sources and Searches
We conducted a comprehensive search of seven databases, including MEDLINE, EMBASE and Scopus, from each database’s earliest inception through June 9th, 2014 for English-language articles and abstracts. The search strategy was designed and conducted by an experienced librarian with input from one researcher (JO). Controlled vocabulary supplemented with keywords was used to search for comparative studies of bedside screening tests for predicting dysphagia. The full strategy can be found in Appendix 1.
All abstracts were screened, and potentially relevant articles were identified for full text review. Those references were manually inspected to identify all relevant studies.
Study Selection
A study was eligible for inclusion if it tested a diagnostic swallow study of any variety against an acceptable reference standard (videofluoroscopic swallow study [VFSS] or flexible endoscopic evaluation of swallowing with sensory testing [FEEST]).
Data Extraction and Quality Assessment
The primary outcome of the study was aspiration, as predicted by a bedside exam compared to gold standard visualization of aspirated material entering below the vocal cords. From each study, data were abstracted based on the type of diagnostic method and reference standard study population and inclusion/exclusion characteristics, design and prediction of aspiration. Prediction of aspiration was compared against the reference standard to yield “true positives” (TP), “true negatives” (TN), “false positives” (FP) and “false negatives” (FN). Additional potential confounding variables were abstracted using a standard form based on the preferred reporting items for systematic reviews and meta-analysis (PRISMA);13 the full abstraction template can be found in Appendix 2.
Data Synthesis and Analysis
Sensitivity and specificity for each test that identified the presence of dysphagia was calculated for each study. These were used to generate positive and negative likelihood ratios (LRs), which were plotted on a likelihood matrix, a graphic depiction of the logarithm of the +LR on the ordinate versus the logarithm of the −LR on the abscissa, dividing the graphic into quadrants such that the right upper quadrant is tests that can be used for confirmation, right lower quadrant neither confirmation nor exclusion, left lower quadrant exclusion only, and left upper quadrant an ideal test with both exclusionary and confirmatory properties.14 A good screening test would thus be on the left half of the graphic as one that can effectively “rule out” dysphagia, and the ideal test with both good sensitivity and specificity would be found in the left upper quadrant. Graphics were constructed using the Stata MIDAS package.15
RESULTS
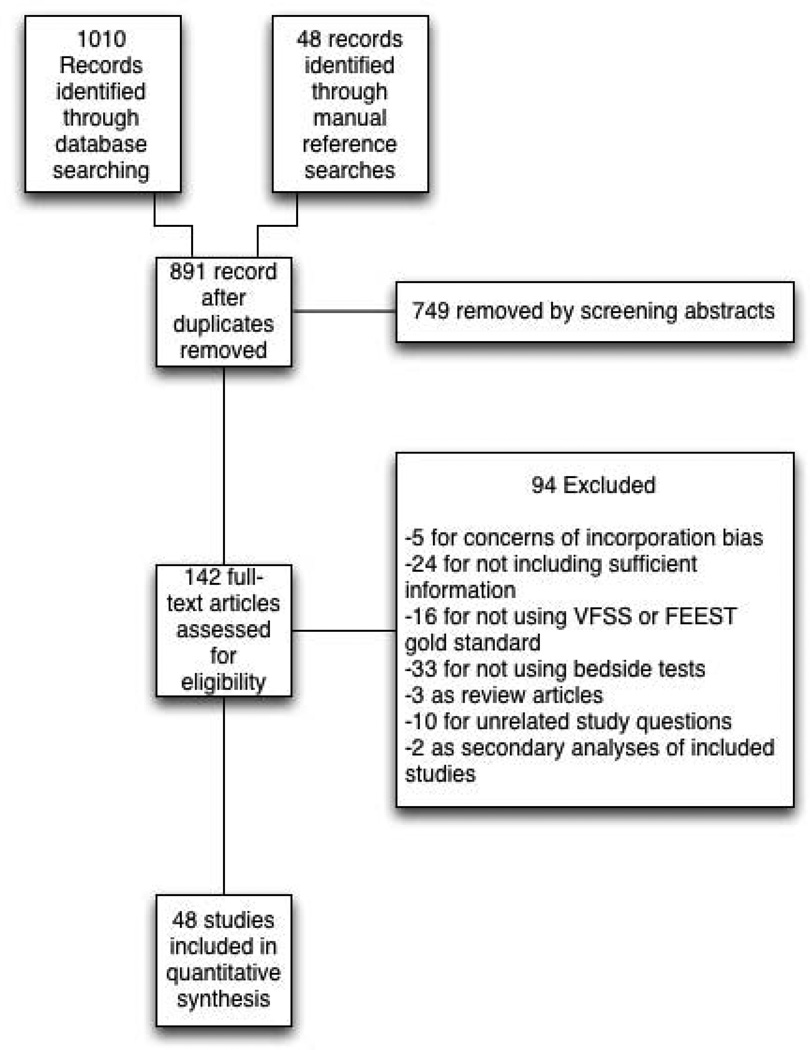
We identified 891 distinct articles. Of these, 749 were excluded based on abstract review. After reviewing the remaining 142 full text articles, 48 articles were determined to meet inclusion criteria, which included 10,437 observations across 7,414 patients (Figure 1). We initially intended to conduct meta-analysis on each type, but heterogeneity in design and statistical heterogeneity in aggregate measures precluded pooling of results.
Figure 1. PRISMA flow diagram.
Characteristics of Included Studies
Of the 48 included studies, the majority (n=42) were prospective observational studies,7, 14, 16–54 while two were randomized trials,55, 56 two studies were double blind observational,9, 16 one was a case-control design,57 and one was a retrospective case series.58 The majority of studies were exclusively inpatient7, 14, 17–19, 21, 22, 24–26, 31–33, 35, 36, 38, 39, 41, 43–47, 49, 51–53, 56, 57, 59 with five in mixed in and outpatient populations,20, 27, 40, 55, 60 two in outpatient populations,23, 42 and the remainder not reporting the setting from which they drew their study populations.
The indications for swallow evaluations fit broadly into four categories; stroke,7, 14, 21, 22, 24–26, 31, 33–35, 38, 39, 41–44, 46, 49, 53, 56, 58, 59 other neurologic disorders,17, 18, 23, 28, 40, 48 all causes,16, 20, 27, 29, 30, 36, 37, 45, 47, 50, 52–55, 60 and post-surgical.19, 32, 34 Most used VFSS as a reference standard,7, 14, 16–19, 21–23, 25–30, 34, 36–48, 51–56, 58–60 with eight using FEEST,20, 24, 31–33, 35, 50, 57 and one accepting either VSE or FEEST.49
Studies were placed into one or more of the following four categories; subjective bedside examination,18, 19, 31, 34, 39, 49, 56 questionnaire-based tools,17, 23, 47, 54 protocolized multi-item evaluations,20–22, 25, 30, 33, 34, 37, 40, 45, 46, 53, 54, 59, 60 and single-item exam maneuvers, symptoms or signs.7, 14, 16, 24, 26–32, 34–38, 40–44, 48–52, 56, 58, 60, 61 The characteristics of all studies are detailed in Table 1.
Table 1.
Characteristics of included studies.
| Study | Location | Design | Mean Age (SD) |
Reason(s) for dysphagia | Index Test | Description | Reference Standard |
Sample size (No of patients) |
Sample Size (No of observations) |
|---|---|---|---|---|---|---|---|---|---|
| Splaingard et al., 198845 |
Milwaukee, Wisconsin, USA |
Prospective Observational Study |
NR | Multiple | Clinical Bedside Swallow Exam |
Combination of scored comprehensive physical exam, history and observed swallow |
VFSS | 107 | 107 |
| DePippo et al., 199244 |
White Plains, NY, USA |
Prospective Observational Study |
71 (10) |
Stroke | WST | Observation of swallow |
VFSS | 44 | |
| Horner et al., 199257 |
Durham, North Carolina, USA |
Retrospective Case Series |
64** | Stroke | Clinical bedside swallow evaluation |
VFSS | 38 | 114 | |
| Kidd et al., 199343 |
Belfast, UK | Prospective Observational Study |
72 (10) |
Stroke | Bedside 50 mL swallow evaluation |
Patient swallows 50 mL of water in 5 mL aliquots, with therapist assessing for choking, coughing or change in vocal quality after each swallow |
VFSS | 60 | 240 |
| Collins et al., 199742 |
Southampton, UK |
Prospective Observational Study |
65** | Stroke | Desaturation | Desaturation of at least 2% during videofluroscopic study |
VFSS | 54 | 54 |
| Daniels et al., 199741 |
New Orleans, Louisiana, USA |
Prospective Observational Study |
66 (11) |
Stroke | Clinical Bedside examination |
6 individual bedside assessments (dysphonia, dysphagia, cough before/after swallow, gag reflex and voice change) examined as predictors for aspiration risk |
VFSS | 59 | 354 |
| Mari et al., 199740 |
Ancona, Italy | Prospective Observational Study |
60 (16) |
Mixed neurologic diseases | Combined history and exam |
Assessed symptoms of dysphagia, cough, and 3-oz water swallow |
VFSS | 93 | 372 |
| Daniels et al., 19987 |
New Orleans, Louisiana, USA |
Prospective Observational Study |
66 (11) |
Stroke | Clinical bedside swallow evaluation |
Describes sensitivity and specificity of several component physical exam maneuvers comprising the bedside exam |
VFSS | 55 | 330 |
| Smithard et al., 199839 |
Ashford, UK | Prospective Observational Study |
79** | Stroke | Clinical bedside swallow evaluation |
Not described | VFSS | 83 | 249 |
| Addington et al., 199938 |
Kansas City, Missouri, USA |
Prospective Observational Study |
80** | Stroke | NR | Reflex Cough | VFSS | 40 | 40 |
| Logemann et al., 199937 |
Evanston, Illinois, USA |
Prospective Observational Study |
65* | Multiple | Northwestern Dysphagia Check Sheet |
28 item screening procedure including history, observed swallos and physical exam |
VFSS | 200 | 1400 |
| Smith et al., 200055 |
Manchester, UK |
Double blind observational |
69* | Stroke | Clinical bedside swallow evaluation, pulse oximetry evaluation |
After eating/drinking, patient is evaluated for signs of aspiration including coughing, choking or "wet voice." Procedure is repeated with several consistencies. Also evaluated if patient desaturates by at least 2% during evaluation. |
VFSS | 53 | 53 |
| Warms et al., 200036 |
Melbourne, Australia |
Prospective Observational Study |
67* | Multiple | Wet voice | Voice was recorded and analyzed with Sony DAT during videofluoroscopy |
VFSS | 23 | 708 |
| Lim et al., 200135 |
Singapore, Singapore |
Prospective Observational Study |
NR | Stroke | Water Swallow Test, desaturation during swallow |
50 mL swallow done in 5 mL aliquots with assesment of phonation/choking afterwards, desaturation >2% during swallow |
FEEST | 50 | 100 |
| McCullough et al., 200134 |
Nashville, Tennessee, USA |
Prospective Observational Study |
60 (10) |
Stroke | Clinical bedside swallow evalulation |
15-item physical exam with observed swallow |
VFSS | 2040 | 60 |
| Rosen et al., 200134 |
Newark, New Jersey, USA |
Prospective Observational Study |
60* | Head and Neck cancer | Wet voice | Observation of swallow |
VFSS | 26 | 26 |
| Leder et al., 200233 |
New Haven, Connecticut, USA |
Prospective Observational Study |
70** | Stroke | Clinical exam | Checklist evaluation of cough and voice change after swallow, volitional cough, dysphonia, dysarthria, and abnormal gag |
FEEST | 49 | 49 |
| Belafsky et al., 200332 |
San Francisco, California, USA |
Prospective Observational Study |
65 (11) |
Post-Tracheostomy patients |
Modified Evans Blue Dye Test (MEBDT) |
Three boluses of dye-impregnated ice are given to patient. Tracheal secretions are suctioned, and evaluated for the presence of dye. |
FEES | 30 | 30 |
| Chong et al., 200331 |
Jalan Tan Tock Seng, Singapore |
Prospective Observational Study |
75 (7) | Stroke | Water Swallow Test, desaturation during, Clinical exam |
Subjective exam, drinking 50 mL of water in 10 mL aliquots, and evaluating for desaturation >2% during FEES |
FEEST | 50 | 150 |
| Tohara et al., 200330 |
Tokyo, Japan |
Prospective Observational Study |
63 (17) |
Multiple | Food/water swallow tests, and a combination of the two |
Protocolized observation of sequential food and water swallows with scored outcomes |
VFSS | 63 | 63 |
| Rosenbek et al., 200414 |
Gainesville, Florida, USA |
Prospective Observational Study |
68** | Stroke | Clinical bedside swallow evaluation |
Describes 5 parameters of voice quality and 15 physical examination maneuvers used |
VFSS | 60 | 1200 |
| Ryu et al., 200429 |
Seoul, South Korea |
Prospective Observational Study |
64 (14) |
Multiple | Voice analysis parameters |
Analysis of the "a" vowel sound with Visi-Pitch II 3300 |
VFSS | 93 | 372 |
| Shaw et al., 200428 |
Sheffield, UK | Prospective Observational Study |
71* | Neurologic disease | Bronchial auscultation |
Auscultation over the right main bronchus during trial feeding to listen for sounds of aspiration |
VFSS | 105 | 105 |
| Wu et al., 200427 |
Taipei, Taiwan |
Prospective Observational Study |
72 (11) |
Multiple | 100- ml swallow test |
Patient lifts a glass of 100 mL of water and drinks as quickly as possible, and is assessed for signs of choking, coughing or wet voice, and is timed for speed of drinking. |
VFSS | 54 | 54 |
| Nishiwaki et al., 200526 |
Shizuoaka, Japan |
Prospective Observational Study |
70** | Stroke | Clinical bedside swallow evaluation |
Describes sensitivity and specificity of several component physical exam maneuvers comprising the bedside exam |
VFSS | 31 | 248 |
| Wang et al., 200554 |
Taipei, Taiwan |
Prospective double-blind study |
41** | Multiple | Desaturation | Desaturation of at least 2% during videofluoroscopic study |
VFSS | 60 | 60 |
| Ramsey et al., 200625 |
Kent, UK | Prospective Observational Study |
71 (10) |
Stroke | BSA | Assessment of lip seal, tongue movement, voice quality, cough, and observed 5 mL swallow |
VFSS | 54 | 54 |
| Trapl et al., 200724 |
Krems, Austria |
Prospective Observational Study |
76 (2) | Stroke | Gugging Swallow Screen |
Progressive observed swallow trials with saliva, then w mL liquid, then dry bread |
FEEST | 49 | 49 |
| Suiter and Leder, 200850 |
Several centers across the USA |
Prospective Observational Study |
68.3 | Multiple | 3 oz water swallow test |
Observation of swallow |
FEEST | 3000 | 3000 |
| Wagasugi et al., 200851 |
Tokyo, Japan |
Prospective Observational Study |
NR | Multiple | Cough test | Acoustic analysis of cough |
VFSS | 204 | 204 |
| Baylow et al. 200946 |
New York, New York, USA |
Prospective Observational Study |
NR | Stroke | Northwestern Dysphagia Check Sheet |
28 item screening procedure including history, observed swallos and physical exam |
VFSS | 15 | 30 |
| Cox et al., 200923 |
Leiden, The Netherlands |
Prospective Observational Study |
68 (8) | Inclusion body myositis | Dysphagia questionnaire |
Questionnaire assessing symptoms of dysphagia |
VFSS | 57 | 57 |
| Kagaya et al., 201052 |
Tokyo, Japan |
Prospective Observational Study |
NR | Multiple | Simple Swallow Provocation Test |
Injection of 1–2 mL water through nasal tube directed at the suprapharnyx |
VFSS | 46 | 46 |
| Martino et al., 200958 |
Toronto, Canada |
Randomized trial | 69 (14) |
Stroke | Toronto Bedside Swallow Screening Test (TOR-BSST) |
4 item physical assessment including Kidd water swallow test, pharyngeal sensation, tongue movement and dysphonia (before and after water swallow) |
VFSS | 59 | 59 |
| Santamato et al., 200956 |
Bari, Italy | Case Control | NR | Multiple | Acoustic analysis- post swallow apnea |
Acoustic analysis of cough |
VFSS | 15 | 15 |
| Smith Hammond et al., 200949 |
Durham, North Carolina, USA |
Prospective observational study |
67.7 (1.2) |
Multiple | Cough expiratory phase peak flow |
Acoustic analysis of cough |
VFSS or FEES |
96 | 288 |
| Leigh et al., 201022 |
Seoul, South Korea |
Prospective Observational Study |
NR | Stroke | Clinical bedside swallow evaluation |
Not described | VFSS | 167 | 167 |
| Pitts et al., 201048 |
Gainesville, Florida, USA |
Prospective Observational Study |
NR | Parkinson | Cough compression phase duration |
Acoustic analysis of cough |
VFSS | 58 | 232 |
| Cohen et al., 201147 |
Tel Aviv, Israel |
Prospective observational Study |
NR | Multiple | Swallow Disturbance Questionnaire |
15 item questionnaire |
FEES | 100 | 100 |
| Edmiaston et al., 201121 |
St. Louis, Missouri, USA |
Prospective Observational Study |
63** | Stroke | SWALLOW-3D Acute Stroke Dysphagia Screen |
5 item screen including mental status, asymmetry or weakness of face, tongue or palate, and subjective signs of aspiration when drinking 3oz water |
VFSS | 225 | 225 |
| Mandysova et al., 201120 |
Pardubice, Czech Republic |
Prospective Observational Study |
69 (13) |
Multiple | Brief Bedside Dysphagia Screening Test (BBDS Test) |
8- item physician exam including ability to clench teeth, symmetry/strength of tongue, facial and shoulder muscles, dysarthria, and choking, coughing or dripping of food after taking thick liquid |
FEES | 87 | 87 |
| Steele et al., 201159 |
Toronto, Canada |
Double blind observational |
67* | Stroke | 4-item bedside exam |
Tongue lateralization, cough, throat clear and voice quality |
VFSS | 400 | 40 |
| Yamamoto et al., 201117 |
Kodaira, Japan |
Prospective Observational Study |
67 (9) | Parkinson’s Disease | Swallowing Disturbance Questionnaire |
15 item questionnaire |
VFSS | 61 | 61 |
| Bhama et al., 2012 19 |
Pittsburgh, Pennsylvania , USA |
Prospective Observational Study |
57 (14) |
Post-lung transplant | Clinical bedside swallow evaluation |
Not described | VFSS | 128 | 128 |
| Shem et al., 201218 |
San Jose, California, USA |
Prospective Observational Study |
42 (17) |
Spinal cord injuries resulting in tetraplegia |
Clinical bedside swallow evaluation |
After eating/drinking, patient is evaluated for signs of aspiration including coughing, choking or "wet voice." Procedure is repeated with several consistencies. |
VFSS | 26 | 26 |
| Steele et al., 201316 |
Toronto, Canada |
Prospective Observational Study |
67 (14) |
Multiple | Dual-axis Accelerometry |
Computed accelerometry of swallow |
VFSS | 37 | 37 |
| Edmiaston et al., 201453 |
St. Louis, Missouri, USA |
Prospective Observational Study |
63 (15) |
Stroke | Barnes Jewish Stroke Dysphagia Screen |
5 item screen including mental status, asymmetry or weakness of face, tongue or palate, and subjective signs of aspiration when drinking 3 oz water |
VFSS | 225 | 225 |
| Rofes et al, 201454 |
Barcelona, Spain |
Prospective Observational Study |
74 (12) |
Mixed | EAT-10 questionnaire and variable viscosity swallow test |
Symptom based questionnaire (EAT- 10) and repeated observations and measurements of swallow with different thickness liquids |
VFS | 134 | 134 |
NR=Not reported,
=median provided instead of mean,
=SD not available.
Subjective Clinical Exam
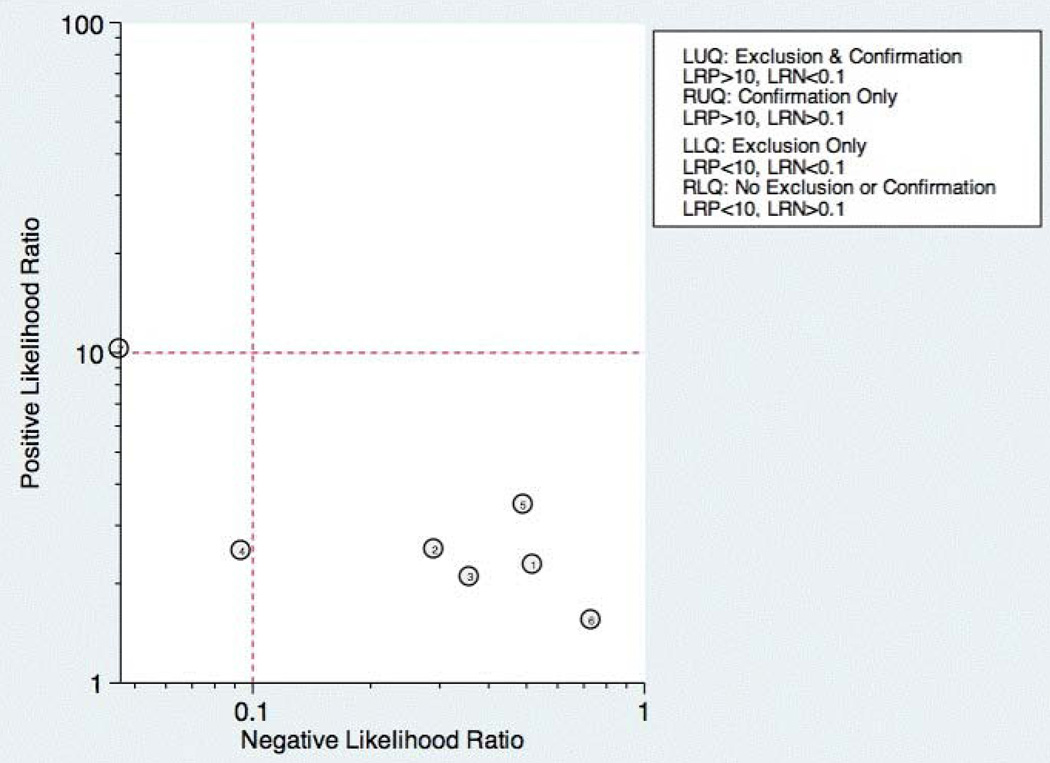
Seven studies reported the sensitivity and specificity of subjective assessments of nurses and speech-language pathologists in observing swallowing and predicting aspiration.18, 19, 31, 34, 39, 49, 56 The overall distribution of studies is summarized in the likelihood matrix in Figure 2. Two studies, Chong et al.31 and Shem et al.,18 were on the left side of the matrix, indicating a sensitive “rule out” test. However, both were small studies, and only Chong et al reported reasonable sensitivity with incorporation bias from knowledge of a desaturation study outcome. Overall, subjective exams did not appear reliable in ruling out dysphagia.
Figure 2. Likelihood Matrix for curve for subjective clinical exam.
Each point corresponds to a study as follows: 1=Smithard et al., 1998;, 2=Smith et al., 2000; 3=McCullough et al., 2001; 4=Chong et al., 2003; 5= Smith-Hammond et al., 2009, 6=Bhama et al., 2012, 7= Shem et al., 2012
Questionnaire Based Tools
Only four studies used questionnaire based tools filled out by the patient, asking about subjective assessment of dysphagia symptoms and frequency.17, 23, 47, 54 Yamamoto et al. reported results of using the swallow dysphagia questionnaire in patients with Parkinson’s disease.17 Rofes et al. looked at the EAT-10 questionnaire among all referred patients and a small population of healthy volunteers.54 Each was administered the questionnaire before undergoing a VF study. Overall, sensitivity and specificity were 77.8% and 84.6% respectively. Cox et al. studied a different questionnaire in a group of patients with inclusion body myositis, finding 70% sensitivity and 44% specificity.23 Cohen et al., 2011 examined the swallow dysphagia questionnaire across several different causes of dysphagia, finding at optimum, this test is 78% specific and 73% sensitive.47 Rofes et al. had an 86% sensitivity and 68% specificity for the EAT-10 tool.54
Multi-Item Exam Protocols
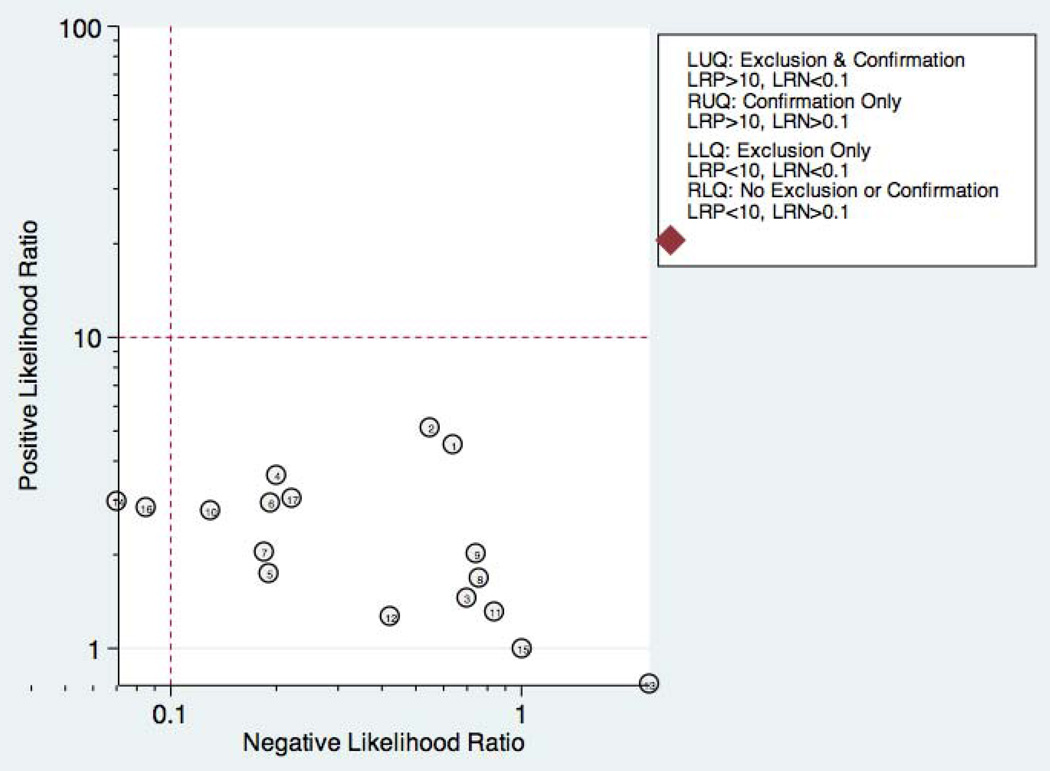
Sixteen studies reported multi-step protocols for determining a patient’s risk for aspiration.20–22, 25, 30, 33, 34, 37, 40, 45, 46, 53, 54, 56, 59, 60 Each involved a combination of physical exam maneuvers and history elements, detailed in Table 1. This is shown in the likelihood matrix in Figure 3. Only two of these studies were in the left lower quadrant, Edmiaston et al. 201121 and 2014.53 Both studies were restricted to stroke populations, but found reasonable sensitivity and specificity in identifying dysphagia.
Figure 3. Likelihood Matrix of Multi-Item Protocols.
1=Splaingard et al., 1988; 2= Mari et al., 1997, 3=Logemann et al., 1999; 4=Smith et al., 2000; 5= McCullough et al., 2001, 6=Leder et al., 2002; 7=Tohara et al., 2003; 8=Ramsey et al., 2006; 9=Baylow et al., 2009, 10=Martino et al., 2009; 11=Leigh et al., 2010, 12=Mandysova et al., 2011, 13=Steele et al, 2011 (SLP assessment); 14=Edmiaston et al., 2011; 15=Steele et al (RN assessment), 16=Edmiaston et al, 2014 17=Rofes et al, 2014
Individual Exam Maneuvers
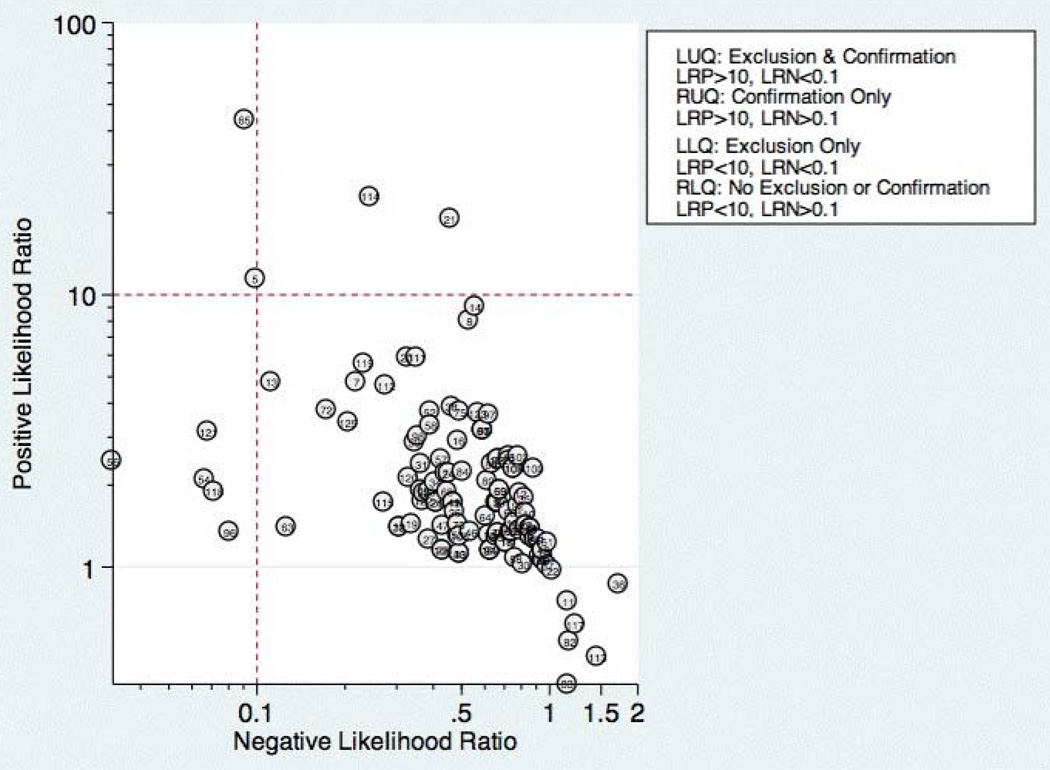
Thirty studies reported the diagnostic performance of individual exam maneuvers and signs.7, 14, 16, 24, 26–32, 34–38, 40–44, 48–52, 55, 56, 58, 60 Each is depicted in Figure 4 as a likelihood matrix demonstrating the +LR and −LR for individual maneuvers as seen in the figure, most fall into the right lower quadrant, where they are not diagnostically useful tests. Studies in the left lower quadrant demonstrating the ability to exclude aspiration desirable in a screening test were dysphonia in McCullough et al., 2001,34 dual-axis accelerometry in Steele et al., 2013,16 and the water swallow test in DePippo et al., 1992,44 and Suiter and Leder, 2008.50
Figure 4. Likelihood matrix of individual exam maneuvers.
Studies in the LLQ demonstrating the ability to exclude aspiration were 56= Kidd et al., 1993 (abnormal pharyngeal sensation) 96=McCullogh et al., 2001 (dysphonia), 54=Steele et al., 2013 (dual axis accelerometry), 121=DePippo et al., 1992 (water swallow test) and 118=Suiter and Leder et al., 2008 (water swallow test). Key to other tests can be located in the appendix
McCullough et al. found dysphonia to be the most discriminatory sign or symptom assessed, with an AUC of 0.818. Dysphonia was judged by a sustained “a,” and had 100% sensitivity, but only 27% specificity. “Wet voice” within the same study was slightly less informative, with AUC of 0.77 (sensitivity 50% and specificity 84%).34
Kidd et al. verified the diagnosis of stroke, and then assessed several neurologic parameters, including speech, muscle strength and sensation. Pharyngeal sensation was assessed by touching each side of the pharyngeal wall and asking patients if they felt sensation differed from each side. Patient report of abnormal sensation during this maneuver was 80% sensitive and 86% specific as a predictor of aspiration on VFSS.43
Steele et al. described the technique of dual axis accelerometry, where an accelerometer was placed at the midline of the neck over the cricoid cartilage during VFSS. The movement of the cricoid cartilage was captured for analysis in a computer algorithm to identify abnormal pharyngeal swallow behavior. Sensitivity was 100%, and specificity was 54%. Although the study was small (n=40), this novel method demonstrated good discrimination.60
DePippo et al. evaluated a 3 oz water swallow in stroke patients. This protocol called for patients to drink the bolus of water without interruption, and be observed for 1 minute after for cough or wet-hoarse voice. Presence of either sign was considered abnormal. Overall, sensitivity was 94% and specificity 30% looking for the presence of either sign.44 Suiter et al., 2008 used a similar protocol with sensitivity of 97% and specificity of 49%.50
Discussion
Our results show that most bedside swallow examinations lack the sensitivity to be used as a screening test for dysphagia across all patient populations examined. This is unfortunate as the ability to determine which patients require formal SLP consultation or imaging as part of their diagnostic evaluation early in the hospital stay would lead to improved allocation of resources, cost reductions, and earlier implementation of effective therapy approaches. Furthermore, although radiation doses received during VFSS are not high when compared with other radiologic exams like CT scans,62 increasing awareness about the long-term malignancy risks associated with medical imaging makes it desirable to reduce any test involving ionizing radiation.
There were several categories of screening procedures identified during this review process. Those classified as subjective bedside exams and protocolized multi-item evaluations were found to have high heterogeneity in their sensitivity and specificity, though a few exam protocols did have a reasonable sensitivity and specificity.21, 31, 53 The following individual exam maneuvers were found to demonstrate high sensitivity and an ability to exclude aspiration: a test for dysphonia through production of a sustained “a34” and use of dual-axis accelerometry16. Two other tests, the 3-oz water swallow test44 and testing of abnormal pharyngeal sensation43, were each found effective in a single study, with conflicting results from other studies.
Our results extend the findings from previous systematic reviews on this subject, most of which focused only on stroke patients.5, 12, 63, 64 Martino and colleagues5 in 2000 conducted a review focused on screening for adults post-stroke. From thirteen identified articles, it was concluded that evidence to support inclusion or exclusion of screening was poor. Daniels et al. 2012 conducted a systematic review of swallowing screening tools specific to patients with acute or chronic stroke.12 Based on sixteen articles, the authors concluded that a combination of swallowing and non-swallowing features may be necessary for development of a valid screening tool. The generalizability of these reviews is limited given that all were conducted in patients post-stroke and, therefore, results and recommendations may not be generalizable to other patients.
Wilkinson et al.64 conducted a recent systematic review that focused on screening techniques for inpatients 65 years or older which excluded patients with stroke or Parkinson’s disease. The purpose of this review was to examine sensitivity and specificity of bedside screening tests as well as ability to accurately predict pneumonia. The authors concluded that existing evidence is not sufficient to recommend the use of bedside tests in a general older population.64
Specific screening tools identified by Martino and colleagues5 to have good predictive value in detecting aspiration as a diagnostic marker of dysphagia were an abnormal test of pharyngeal sensation43 and the 50-ml water swallow test. Daniels et al. identified a water swallow test as an important component of a screen.7 These results were consistent with those of this review in that the abnormal test of pharyngeal sensation43 was identified for high levels of sensitivity. However, the 3-oz water swallow test,44, 50 rather than the 50-ml water swallow test43 was identified in this review as the version of the water swallow test with the best predictive value in ruling out aspiration. Results of our review identified two additional individual items, dual axis accelerometry16 and dysphonia,34 that may be important to include in a comprehensive screening tool. In the absence of better tools, the 3 oz swallow test, properly executed, seems to be the best currently available tool validated in more than one study.
Several studies in this review included an assessment of oral tongue movement that is not described thoroughly and varies between studies. Tongue movement as an individual item on a screening protocol was not found to yield high sensitivity or specificity. However, tongue movement or range of motion is only one aspect of oral tongue function; pressures produced by the tongue reflecting strength also may be important and warrant evaluation. Multiple studies have shown patients with dysphagia resulting from a variety of etiologies to produce lower than normal maximum isometric lingual pressures,65–70 or pressures produced when the tongue is pushed as hard as possible against the hard palate. Tongue strengthening protocols that results in higher maximum isometric lingual pressures have been shown to carry over to positive changes in swallow function.71–75 Inclusion of tongue pressure measurement in a comprehensive screening tool may help to improve predictive capabilities.
We believe our results have implications for practicing clinicians, and serve as a call to action for development of an easy to perform, accurate tool for dysphagia screening. Future prospective studies should focus on practical tools that can be deployed at the bedside, and correlate the results with not only “gold standard” VFSS and FEES, but with clinical outcomes, such as pneumonia and aspiration events leading to prolonged length of stay.
There were several limitations to this review. High levels of heterogeneity were reported in the screening tests present in the literature, precluding meaningful meta-analysis. In addition, the majority of studies included were in post-stroke adults, which limits the generalizability of results.
In conclusion, no screening protocol has been shown to provide adequate predictive value for presence of aspiration. Several individual exam maneuvers demonstrate high sensitivity; however, the most effective combination of screening protocol components is unknown. There is a need for future research focused on the development of a comprehensive screening tool that can be applied across patient populations for accurate detection of dysphagia as well as prediction of other adverse health outcomes, including pneumonia.
Supplementary Material
ACKNOWLEDGEMENTS
The authors would like to thank Drs. Byun-Mo Oh and Catrionia Steele for providing additional information in response to requests for unpublished information.
Source of funding: Nasia Safdar is supported by an NIH R03 GEMSSTAR award and a MERIT award from the Department of Veterans Affairs.
Footnotes
Conflicts of interest: None of the authors have any conflicts of interest to disclose
This manuscript is not under consideration elsewhere, nor have its contents been presented at any meetings
REFERENCES
- 1.Clave P, Rofes L, Carrion S, et al. Pathophysiology, relevance and natural history of oropharyngeal dysphagia among older people. Nestle Nutrition Institute workshop series. 2012;72:57–66. doi: 10.1159/000339986. [DOI] [PubMed] [Google Scholar]
- 2.Roy N, Stemple J, Merrill RM, Thomas L. Dysphagia in the elderly: preliminary evidence of prevalence, risk factors, and socioemotional effects. The Annals of otology, rhinology, and laryngology. 2007 Nov;116(11):858–865. doi: 10.1177/000348940711601112. [DOI] [PubMed] [Google Scholar]
- 3.Perry L, Hamilton S, Williams J. Formal dysphagia screening protocols prevent pneumonia. Stroke; a journal of cerebral circulation. 2006 Mar;37(3):765. doi: 10.1161/01.str.0000204140.01459.dc. [DOI] [PubMed] [Google Scholar]
- 4.Odderson IR, Keaton JC, McKenna BS. Swallow management in patients on an acute stroke pathway: quality is cost effective. Archives of physical medicine and rehabilitation. 1995 Dec;76(12):1130–1133. doi: 10.1016/s0003-9993(95)80121-9. [DOI] [PubMed] [Google Scholar]
- 5.Martino R, Pron G, Diamant N. Screening for oropharyngeal dysphagia in stroke: insufficient evidence for guidelines. Dysphagia. 2000 Winter;15(1):19–30. doi: 10.1007/s004559910006. [DOI] [PubMed] [Google Scholar]
- 6.Jauch EC, Saver JL, Adams HP, Jr, et al. Guidelines for the early management of patients with acute ischemic stroke: a guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke; a journal of cerebral circulation. 2013 Mar;44(3):870–947. doi: 10.1161/STR.0b013e318284056a. [DOI] [PubMed] [Google Scholar]
- 7.Daniels SK, Brailey K, Priestly DH, Herrington LR, Weisberg LA, Foundas AL. Aspiration in patients with acute stroke. Archives of physical medicine and rehabilitation. 1998 Jan;79(1):14–19. doi: 10.1016/s0003-9993(98)90200-3. [DOI] [PubMed] [Google Scholar]
- 8.Smithard DG, O'Neill PA, Park C, et al. Can bedside assessment reliably exclude aspiration following acute stroke? Age and ageing. 1998 Mar;27(2):99–106. doi: 10.1093/ageing/27.2.99. [DOI] [PubMed] [Google Scholar]
- 9.Smith HA, Lee SH, O'Neill PA, Connolly MJ. The combination of bedside swallowing assessment and oxygen saturation monitoring of swallowing in acute stroke: a safe and humane screening tool. Age and ageing. 2000 Nov;29(6):495–499. doi: 10.1093/ageing/29.6.495. [DOI] [PubMed] [Google Scholar]
- 10.Edmiaston J, Connor LT, Loehr L, Nassief A. Validation of a dysphagia screening tool in acute stroke patients. American journal of critical care : an official publication, American Association of Critical-Care Nurses. 2010 Jul;19(4):357–364. doi: 10.4037/ajcc2009961. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Perry L, Love CP. Screening for dysphagia and aspiration in acute stroke: a systematic review. Dysphagia. 2001 Winter;16(1):7–18. doi: 10.1007/pl00021290. [DOI] [PubMed] [Google Scholar]
- 12.Daniels SK, Anderson JA, Willson PC. Valid items for screening dysphagia risk in patients with stroke: a systematic review. Stroke; a journal of cerebral circulation. 2012 Mar;43(3):892–897. doi: 10.1161/STROKEAHA.111.640946. [DOI] [PubMed] [Google Scholar]
- 13.Moher D, Liberati A, Tetzlaff J, Altman DG, Grp P. Preferred Reporting Items for Systematic Reviews and Meta-Analyses: The PRISMA Statement. Ann Intern Med. 2009 Aug 18;151(4) doi: 10.7326/0003-4819-151-4-200908180-00135. 264-W264. [DOI] [PubMed] [Google Scholar]
- 14.Rosenbek JC, McCullough GH, Wertz RT. Is the information about a test important? Applying the methods of evidence-based medicine to the clinical examination of swallowing. Journal of communication disorders. 2004 Sep-Oct;37(5):437–450. doi: 10.1016/j.jcomdis.2004.04.007. [DOI] [PubMed] [Google Scholar]
- 15.Dwamena B. MIDAS: Stata module for meta-analytical integration of diagnostic test accuracy studies. Statistical Software Components. 2009 [Google Scholar]
- 16.Steele CM, Sejdic E, Chau T. Noninvasive detection of thin-liquid aspiration using dual-axis swallowing accelerometry. Dysphagia. 2013 Mar;28(1):105–112. doi: 10.1007/s00455-012-9418-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Yamamoto T, Ikeda K, Usui H, Miyamoto M, Murata M. Validation of the Japanese translation of the Swallowing Disturbance Questionnaire in Parkinson's disease patients. Qual Life Res. 2012 Sep;21(7):1299–1303. doi: 10.1007/s11136-011-0041-2. [DOI] [PubMed] [Google Scholar]
- 18.Shem KL, Castillo K, Wong SL, Chang J, Kao M-C, Kolakowsky-Hayner SA. Diagnostic accuracy of bedside swallow evaluation versus videofluoroscopy to assess dysphagia in individuals with tetraplegia. Pm R. 2012 Apr;4(4):283–289. doi: 10.1016/j.pmrj.2012.01.002. [DOI] [PubMed] [Google Scholar]
- 19.Bhama JK, Baumann BM, Byers S, et al. Aspiration after lung transplantation: Incidence, risk factors, and accuracy of the bedside swallow evaluation. Journal of Heart and Lung Transplantation; Conference: 32nd Annual Meeting and Scientific Sessions of the International Society for Heart and Lung Transplantation Prague Czech Republic. Conference Start: 20120418 Conference End: 20120421. Conference Publication: (var.pagings).; 2012. Apr, pp. S247–S248. [Google Scholar]
- 20.Mandysova P, Skvrnakova J, Ehler E, Cerny M. Development of the Brief Bedside Dysphagia Screening Test in the Czech Republic. Nurs Health Sci. 2011 Dec;13(4):388–395. doi: 10.1111/j.1442-2018.2011.00630.x. [DOI] [PubMed] [Google Scholar]
- 21.Edmiaston JM, Connor LT, Ford AL. SWALLOW-3D, a simple 2-minute bedside screening test, detects dysphagia in acute stroke patients with high sensitivity when validated against video-fluoroscopy. Stroke; a journal of cerebral circulation; Conference: 2011 International Stroke Conference Los Angeles, CA United States. Conference Start: 20110209 Conference End: 20110211. Conference Publication: (var.pagings); 2011. Mar 01, p. e352. [Google Scholar]
- 22.Leigh JH, Lim JY, Han MK, Bae HJ, Paik NJ. Bedside screening and subacute reassessment of post-stroke dysphagia: A prospective study. International Journal of Stroke; Conference: World Stroke Congress 2010 Seoul South Korea. Conference Start: 20101013 Conference End: 20101016. Conference Publication: (var.pagings); 2010. Oct, p. 200. [Google Scholar]
- 23.Cox FM, Verschuuren JJ, Verbist BM, Niks EH, Wintzen AR, Badrising UA. Detecting dysphagia in inclusion body myositis. J Neurol. 2009 Dec;256(12):2009–2013. doi: 10.1007/s00415-009-5229-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Trapl M, Enderle P, Nowotny M, et al. Dysphagia bedside screening for acute-stroke patients: the Gugging Swallowing Screen. Stroke; a journal of cerebral circulation. 2007 Nov;38(11):2948–2952. doi: 10.1161/STROKEAHA.107.483933. [DOI] [PubMed] [Google Scholar]
- 25.Ramsey DJC, Smithard DG, Kalra L. Can pulse oximetry or a bedside swallowing assessment be used to detect aspiration after stroke? Stroke; a journal of cerebral circulation. 2006 Dec;37(12):2984–2988. doi: 10.1161/01.STR.0000248758.32627.3b. [DOI] [PubMed] [Google Scholar]
- 26.Nishiwaki K, Tsuji T, Liu M, Hase K, Tanaka N, Fujiwara T. Identification of a simple screening tool for dysphagia in patients with stroke using factor analysis of multiple dysphagia variables. Journal of rehabilitation medicine : official journal of the UEMS European Board of Physical and Rehabilitation Medicine. 2005 Jul;37(4):247–251. doi: 10.1080/16501970510026999. [DOI] [PubMed] [Google Scholar]
- 27.Wu MC, Chang YC, Wang TG, Lin LC. Evaluating swallowing dysfunction using a 100-ml water swallowing test. Dysphagia. 2004 Winter;19(1):43–47. doi: 10.1007/s00455-003-0030-x. [DOI] [PubMed] [Google Scholar]
- 28.Shaw JL, Sharpe S, Dyson SE, et al. Bronchial auscultation: an effective adjunct to speech and language therapy bedside assessment when detecting dysphagia and aspiration? Dysphagia. 2004 Fall;19(4):211–218. doi: 10.1007/s00455-004-0008-3. [DOI] [PubMed] [Google Scholar]
- 29.Ryu JS, Park SR, Choi KH. Prediction of laryngeal aspiration using voice analysis. American Journal of Physical Medicine and Rehabilitation. 2004 Oct;83(10):753–757. doi: 10.1097/01.phm.0000140798.97706.a5. [DOI] [PubMed] [Google Scholar]
- 30.Tohara H, Saitoh E, Mays KA, Kuhlemeier K, Palmer JB. Three tests for predicting aspiration without videofluorography. Dysphagia. 2003 Spring;18(2):126–134. doi: 10.1007/s00455-002-0095-y. [DOI] [PubMed] [Google Scholar]
- 31.Chong MS, Lieu PK, Sitoh YY, Meng YY, Leow LP. Bedside clinical methods useful as screening test for aspiration in elderly patients with recent and previous strokes. Annals of the Academy of Medicine, Singapore. 2003 Nov;32(6):790–794. [PubMed] [Google Scholar]
- 32.Belafsky PC, Blumenfeld L, LePage A, Nahrstedt K. The accuracy of the modified Evan's blue dye test in predicting aspiration. Laryngoscope. 2003 Nov;113(11):1969–1972. doi: 10.1097/00005537-200311000-00021. [DOI] [PubMed] [Google Scholar]
- 33.Leder SB, Espinosa JF. Aspiration risk after acute stroke: comparison of clinical examination and fiberoptic endoscopic evaluation of swallowing. Dysphagia. 2002 Summer;17(3):214–218. doi: 10.1007/s00455-002-0054-7. [DOI] [PubMed] [Google Scholar]
- 34.McCullough GH, Wertz RT, Rosenbek JC. Sensitivity and specificity of clinical/bedside examination signs for detecting aspiration in adults subsequent to stroke. Journal of communication disorders. 2001 Jan-Apr;34(1–2):55–72. doi: 10.1016/s0021-9924(00)00041-1. [DOI] [PubMed] [Google Scholar]
- 35.Lim SH, Lieu PK, Phua SY, et al. Accuracy of bedside clinical methods compared with fiberoptic endoscopic examination of swallowing (FEES) in determining the risk of aspiration in acute stroke patients. Dysphagia. 2001 Winter;16(1):1–6. doi: 10.1007/s004550000038. [DOI] [PubMed] [Google Scholar]
- 36.Warms T, Richards J. ``Wet Voice'' as a Predictor of Penetration and Aspiration in Oropharyngeal Dysphagia. [2000/03/01];Dysphagia. 2000 15(2):84–88. doi: 10.1007/s004550010005. [DOI] [PubMed] [Google Scholar]
- 37.Logemann JA, Veis S, Colangelo L. A screening procedure for oropharyngeal dysphagia. Dysphagia. 1999 Winter;14(1):44–51. doi: 10.1007/PL00009583. [DOI] [PubMed] [Google Scholar]
- 38.Addington WR, Stephens RE, Gilliland K, Rodriguez M. Assessing the laryngeal cough reflex and the risk of developing pneumonia after stroke. Archives of physical medicine and rehabilitation. 1999 Feb;80(2):150–154. doi: 10.1016/s0003-9993(99)90112-0. [DOI] [PubMed] [Google Scholar]
- 39.Smithard DG, O'Neill PA, Park C, et al. Can bedside assessment reliably exclude aspiration following acute stroke? Age Ageing. 1998 Mar;27(2):99–106. doi: 10.1093/ageing/27.2.99. [DOI] [PubMed] [Google Scholar]
- 40.Mari F, Matei M, Ceravolo MG, Pisani A, Montesi A, Provinciali L. Predictive value of clinical indices in detecting aspiration in patients with neurological disorders. J Neurol Neurosurg Psychiatry. 1997 Oct;63(4):456–460. doi: 10.1136/jnnp.63.4.456. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Daniels SK, McAdam CP, Brailey K, Foundas AL. Clinical Assessment of Swallowing and Prediction of Dysphagia Severity. [November 1, 1997];Am J Speech Lang Pathol. 1997 6(4):17–24. [Google Scholar]
- 42.Collins MJ, Bakheit AM. Does pulse oximetry reliably detect aspiration in dysphagic stroke patients? Stroke; a journal of cerebral circulation. 1997 Sep;28(9):1773–1775. doi: 10.1161/01.str.28.9.1773. [DOI] [PubMed] [Google Scholar]
- 43.Kidd D, Lawson J, Nesbitt R, MacMahon J. Aspiration in acute stroke: a clinical study with videofluoroscopy. Q J Med. 1993 Dec;86(12):825–829. [PubMed] [Google Scholar]
- 44.DePippo KL, Holas MA, Reding MJ. Validation of the 3-oz water swallow test for aspiration following stroke. Arch Neurol. 1992 Dec;49(12):1259–1261. doi: 10.1001/archneur.1992.00530360057018. [DOI] [PubMed] [Google Scholar]
- 45.Splaingard ML, Hutchins B, Sulton LD, Chaudhuri G. Aspiration in rehabilitation patients: videofluoroscopy vs bedside clinical assessment. Archives of physical medicine and rehabilitation. 1988 Aug;69(8):637–640. [PubMed] [Google Scholar]
- 46.Baylow HE, Goldfarb R, Taveira CH, Steinberg RS. Accuracy of clinical judgment of the chin-down posture for dysphagia during the clinical/bedside assessment as corroborated by videofluoroscopy in adults with acute stroke. Dysphagia. 2009 Dec;24(4):423–433. doi: 10.1007/s00455-009-9220-5. [DOI] [PubMed] [Google Scholar]
- 47.Cohen JT, Manor Y. Swallowing disturbance questionnaire for detecting dysphagia. The Laryngoscope. 2011 Jul;121(7):1383–1387. doi: 10.1002/lary.21839. [DOI] [PubMed] [Google Scholar]
- 48.Pitts T, Troche M, Mann G, Rosenbek J, Okun MS, Sapienza C. Using voluntary cough to detect penetration and aspiration during oropharyngeal swallowing in patients with Parkinson disease. Chest. 2010 Dec;138(6):1426–1431. doi: 10.1378/chest.10-0342. [DOI] [PubMed] [Google Scholar]
- 49.Smith Hammond CA, Goldstein LB, Horner RD, et al. Predicting aspiration in patients with ischemic stroke: comparison of clinical signs and aerodynamic measures of voluntary cough. Chest. 2009 Mar;135(3):769–777. doi: 10.1378/chest.08-1122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Suiter DM, Leder SB. Clinical utility of the 3-ounce water swallow test. Dysphagia. 2008 Sep;23(3):244–250. doi: 10.1007/s00455-007-9127-y. [DOI] [PubMed] [Google Scholar]
- 51.Wakasugi Y, Tohara H, Hattori F, et al. Screening test for silent aspiration at the bedside. Dysphagia. 2008 Dec;23(4):364–370. doi: 10.1007/s00455-008-9150-7. [DOI] [PubMed] [Google Scholar]
- 52.Kagaya H, Okada S, Saitoh E, Baba M, Yokoyama M, Takahashi H. Simple swallowing provocation test has limited applicability as a screening tool for detecting aspiration, silent aspiration, or penetration. Dysphagia. 2010 Mar;25(1):6–10. doi: 10.1007/s00455-009-9222-3. [DOI] [PubMed] [Google Scholar]
- 53.Edmiaston J, Connor LT, Steger-May K, Ford AL. A simple bedside stroke dysphagia screen, validated against videofluoroscopy, detects dysphagia and aspiration with high sensitivity. Journal of Stroke and Cerebrovascular Diseases. 2014 Apr;23(4):712–716. doi: 10.1016/j.jstrokecerebrovasdis.2013.06.030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Rofes L, Arreola V, Mukherjee R, Clavé P. Sensitivity and specificity of the Eating Assessment Tool and the Volume-Viscosity Swallow Test for clinical evaluation of oropharyngeal dysphagia. Neurogastroenterology & Motility. 2014;26(9):1256–1265. doi: 10.1111/nmo.12382. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Wang T-G, Chang Y-C, Chen S-Y, Hsiao T-Y. Pulse oximetry does not reliably detect aspiration on videofluoroscopic swallowing study. Archives of Physical Medicine & Rehabilitation. 2005 Apr;86(4):730–734. doi: 10.1016/j.apmr.2004.10.021. [DOI] [PubMed] [Google Scholar]
- 56.Smith HA, Lee SH, O'Neill PA, Connolly MJ. The combination of bedside swallowing assessment and oxygen saturation monitoring of swallowing in acute stroke: a safe and humane screening tool. Age Ageing. 2000 Nov;29(6):495–499. doi: 10.1093/ageing/29.6.495. [DOI] [PubMed] [Google Scholar]
- 57.Santamato A, Panza F, Solfrizzi V, et al. Acoustic analysis of swallowing sounds: a new technique for assessing dysphagia. Journal of rehabilitation medicine. 2009 Jul;41(8):639–645. doi: 10.2340/16501977-0384. [DOI] [PubMed] [Google Scholar]
- 58.Horner J, Brazer SR, Massey EW. Aspiration in bilateral stroke patients: a validation study. Neurology. 1993 Feb;43(2):430–433. doi: 10.1212/wnl.43.2.430. [DOI] [PubMed] [Google Scholar]
- 59.Martino R, Silver F, Teasell R, et al. The Toronto Bedside Swallowing Screening Test (TOR-BSST): development and validation of a dysphagia screening tool for patients with stroke. Stroke; a journal of cerebral circulation. 2009 Feb;40(2):555–561. doi: 10.1161/STROKEAHA.107.510370. [DOI] [PubMed] [Google Scholar]
- 60.Steele CM, Molfenter SM, Bailey GL, et al. Exploration of the utility of a brief swallow screening protocol with comparison to concurrent videofluoroscopy. Canadian Journal of Speech-Language Pathology and Audiology. 2011;35(3):228–242. [Google Scholar]
- 61.Hinchey JA, Shephard T, Furie K, et al. Formal dysphagia screening protocols prevent pneumonia. Stroke; a journal of cerebral circulation. 2005 Sep;36(9):1972–1976. doi: 10.1161/01.STR.0000177529.86868.8d. [DOI] [PubMed] [Google Scholar]
- 62.Bonilha HS, Humphries K, Blair J, et al. Radiation exposure time during MBSS: influence of swallowing impairment severity, medical diagnosis, clinician experience, and standardized protocol use. Dysphagia. 2013 Mar;28(1):77–85. doi: 10.1007/s00455-012-9415-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Westergren A. Detection of eating difficulties after stroke: a systematic review. International nursing review. 2006 Jun;53(2):143–149. doi: 10.1111/j.1466-7657.2006.00460.x. [DOI] [PubMed] [Google Scholar]
- 64.Wilkinson AH, Burns SL, Witham MD. Aspiration in older patients without stroke: A systematic review of bedside diagnostic tests and predictors of pneumonia. European Geriatric Medicine. 2012;3(3):145–152. 6// [Google Scholar]
- 65.Robinovitch SN, Hershler C, Romilly DP. A tongue force measurement system for the assessment of oral-phase swallowing disorders. Archives of physical medicine and rehabilitation. 1991 Jan;72(1):38–42. [PubMed] [Google Scholar]
- 66.Solomon NP, Robin DA, Luschei ES. Strength, Endurance, and Stability of the Tongue and Hand in Parkinson Disease. Journal of Speech, Language, and Hearing Research. 2000;43(1):256–267. doi: 10.1044/jslhr.4301.256. [DOI] [PubMed] [Google Scholar]
- 67.Lazarus C, Logemann JA, Pauloski BR, et al. Effects of radiotherapy with or without chemotherapy on tongue strength and swallowing in patients with oral cancer. Head & neck. 2007 Jul;29(7):632–637. doi: 10.1002/hed.20577. [DOI] [PubMed] [Google Scholar]
- 68.Hori K, Ono T, Iwata H, Nokubi T, Kumakura I. Tongue pressure against hard palate during swallowing in post-stroke patients. Gerodontology. 2005 Dec;22(4):227–233. doi: 10.1111/j.1741-2358.2005.00089.x. [DOI] [PubMed] [Google Scholar]
- 69.Stierwalt JA, Youmans SR. Tongue measures in individuals with normal and impaired swallowing. Am J Speech Lang Pathol. 2007 May;16(2):148–156. doi: 10.1044/1058-0360(2007/019). [DOI] [PubMed] [Google Scholar]
- 70.Lazarus CL, Husaini H, Anand SM, et al. Tongue strength as a predictor of functional outcomes and quality of life after tongue cancer surgery. The Annals of otology, rhinology, and laryngology. 2013 Jun;122(6):386–397. doi: 10.1177/000348941312200608. [DOI] [PubMed] [Google Scholar]
- 71.Lazarus C, Logemann JA, Huang CF, Rademaker AW. Effects of two types of tongue strengthening exercises in young normals. Folia phoniatrica et logopaedica : official organ of the International Association of Logopedics and Phoniatrics. 2003 Jul-Aug;55(4):199–205. doi: 10.1159/000071019. [DOI] [PubMed] [Google Scholar]
- 72.Robbins J, Gangnon RE, Theis SM, Kays SA, Hewitt AL, Hind JA. The effects of lingual exercise on swallowing in older adults. Journal of the American Geriatrics Society. 2005 Sep;53(9):1483–1489. doi: 10.1111/j.1532-5415.2005.53467.x. [DOI] [PubMed] [Google Scholar]
- 73.Robbins J, Kays SA, Gangnon RE, et al. The effects of lingual exercise in stroke patients with dysphagia. Archives of physical medicine and rehabilitation. 2007 Feb;88(2):150–158. doi: 10.1016/j.apmr.2006.11.002. [DOI] [PubMed] [Google Scholar]
- 74.Carroll WR, Locher JL, Canon CL, Bohannon IA, McColloch NL, Magnuson JS. Pretreatment swallowing exercises improve swallow function after chemoradiation. Laryngoscope. 2008 Jan;118(1):39–43. doi: 10.1097/MLG.0b013e31815659b0. [DOI] [PubMed] [Google Scholar]
- 75.Clark HM, O'Brien K, Calleja A, Corrie SN. Effects of directional exercise on lingual strength. Journal of speech, language, and hearing research : JSLHR. 2009 Aug;52(4):1034–1047. doi: 10.1044/1092-4388(2009/08-0062). [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.