Abstract
Background
Chronic rhinosinusitis (CRS) is a common condition encountered in primary care medicine and is estimated to affect 12.5% of the United States population. This study aims to compare methods of assessing health utility in CRS
Methods
A cross-sectional sample of CRS patients (n=137) were interviewed using direct health utility assessment measures: the visual analog scale (VAS), time trade-off (TTO), and standard gamble (SG). General quality of life (QOL) scores were obtained via the 36-item Short Form Health Survey (SF-36) and converted to SF-6D health utility values using a Bayesian algorithm. Disease specific quality of life was measured with the SNOT-22. A selected subgroup of patients (n=51) not initiating surgery or new treatment for CRS were re-interviewed within three weeks.
Results
The mean (±SD) health utilities were VAS 0.69(±0.19), TTO 0.80(±0.27), SG 0.93(±0.11), SF-6D 0.72(±0.12) and differed significantly (p<0.001). Only VAS scores differed based on disease state classification or the presence of nasal polyposis. Correlations between methods of determining health utility were weak, but significant. VAS, TTO and SF-6D scores were significantly associated with SNOT-22 (p<0.001 for all), however SG and SNOT-22 were poorly correlated (Spearman correlation=-0.33). The test-retest reliability of TTO (Spearman correlation=0.71) and SG (0.73) was strong.
Conclusions
CRS patients show significant impairment in quality of life, with health utility values similar to those of patients with AIDS or intermittent claudication using similar methods. The method of ascertainment significantly affects measured health utility, but the degree of impairment warrants improved recognition and appropriate treatment of the condition.
Keywords: chronic rhinosinusitis, quality of life, utility values, time trade-off, standard gamble, visual analog scale, SF-6D
Introduction
Chronic rhinosinusitis (CRS) is among the most common conditions encountered in medicine and is estimated to affect 12.5% of the United States population and account for approximately 7% of ambulatory care visits which result in an antibiotic prescription.1–3 Since CRS primarily impairs quality-of-life rather than survival, it is crucial to accurately measure health utility in order to establish economic evaluations of management algorithms.4,5
At present, CRS is diagnosed based on the presence of the cardinal symptoms of nasal obstruction/congestion, facial pain/pressure, anterior/posterior discharge and/or olfactory loss for a duration greater than twelve weeks. These symptoms must be corroborated by objective signs of inflammation on radiographic or endoscopic evaluation.3 While the duration and severity of CRS symptoms are the motivating factors for patients to seek medical and surgical therapy,6 the burden of these impairments does not correlate well with the degree of objective findings.6–9 CRS additionally has been sub-classified into two types based on the presence of nasal polyps. Studies suggest that there are differences in the inflammatory milleu and symptomatic presentation of patients with nasal polyps but limited studies have examined if there are differences in quality of life between these subtypes.10
Health utilities are preference weights that measure a patient's value of a particular health state. This differs from disease specific quality-of-life instruments, such as the Sinonasal Outcome Test-22(SNOT-22), which quantify a health state in terms of symptoms and functioning without ascribing a global preference value.11 Utility values are a critical component of economic evaluations of medical interventions, including cost-effectiveness research, and serve as the weights for quality-adjusted life years. Health utilities are defined on a scale from 0 to 1, with 0 representing death and 1 perfect health. Direct methods of determining health utilities ask patients to make judgments regarding the value of particular health states in comparison with one another, for example using a Time Trade Off(TTO) or Standard Gamble(SG) approach. Indirect methods of determining utilities use generic preference instruments(EQ-5D, SF-6D) or disease specific instruments to assign scores to components of health and then convert these scores using an algorithm to a health utility level.12 Since direct and indirect measures of health utility have been applied to a variety of diseases, they can also provide a metric by which the impairment of one disease or health state can be compared with another using similar methodology.
While disease specific tools, such as SNOT-22, are frequently used to assess CRS disease burden, only limited studies have applied general quality-of-life instruments such as the Short-Form 36(SF-36) and EQ-5D to CRS populations. There are no prior studies, to our knowledge, that have assessed direct measures of health utility in CRS. Furthermore, there is a fundamental assumption in the CRS definition that it is a chronic disease akin to diabetes or chronic renal failure without recognition that CRS is likely a chronic episodic disease that has fluctuating health utility depending on the timing of assessment.13 Obtaining health utilities using multiple instruments is critical to mature the field of outcomes research in CRS.14 Our objectives were to 1) obtain estimates of direct and indirect measures of health utility in patients with CRS, 2) evaluate the stability of health utility when applied to a chronic episodic disease conceptual model,13 3) assess the stability of health utility values in patients with stable disease, and 4) compare health utility measures with disease-specific measures such as the SNOT-22 instrument.
Methods
Subjects
The study population consisted of patients 18-89 years old with CRS seen in an outpatient Otolaryngology clinic of a tertiary medical center from July 2013 to March 2014. All patients had a new or existing diagnosis of CRS, defined using the AAO-HNS task force criteria: at least two cardinal symptoms of obstruction, drainage, smell loss, or facial pain/pressure for a duration of 3 months or longer; and objective evidence of sinus inflammation via nasal endoscopy and/or computed tomography. Patients were excluded if they had a diagnosis of recurrent acute sinusitis, were pregnant, or were unable (for cognitive or language reasons) to participate in the health utility interviews. The Northwestern IRB reviewed and approved this protocol.
All patients enrolled were asked to complete three components: 1) an electronic survey assessing demographic information, past medical/allergic history, and SNOT-22 questions, 2) an in-person health utility interview, and 3) a paper version of the generic SF-36. Disease severity was defined using the EPOS 2012 Scale (Mild=VAS 0-3, Moderate=VAS 3-7, and Severe=VAS 7-10).15 A subset of patients with CRS, Recalcitrant CRS, or Remitted CRS (See Table 1 for definitions) were asked for permission to be contacted for a follow-up phone interview three weeks after the initial interview. These patients were those for whom symptoms were stable and were not being initiated on new medical or surgical therapy. The SG and TTO questions were repeated, while the VAS and SF-36 were unable to be repeated over the phone. The electronic survey was completed either during the office visit on an iPad(Apple Inc, Cupertino, CA) or at their convenience via an emailed link. All in-person and phone interviews were conducted based on a transcript by one of two trained study coordinators.
Table 1.
Chronic Rhinosinusitis Disease State Classification
| CRS Disease State | Definition |
|---|---|
| Chronic rhinosinusitis (CRS) | • At least two cardinal symptoms (obstruction, drainage, smell loss, facial pain/pressure) • Minimum of 3 months duration • Objective evidence of sinus inflammation via endoscopy and/or CT imaging |
| CRS exacerbation | Met definition for CRS in past AND: • Preceded by defined duration of mild/moderate symptoms for 1+ month • At least a single cardinal symptom worsening within the past 7 days |
| Recalcitrant CRS | Met definition for CRS in the past AND: • Two or more sinus surgeries; OR • Oral corticosteroid treatment more than twice per year for CRS indication; OR • Antibiotics more than three per year for CRS indication; OR • Polyps recurred after sinus surgery |
| Remitted CRS | Met definition for CRS in the past AND: • No moderate or severe symptoms that persisted for at least 3 months in prior year; AND • No antibiotics, oral corticosteroids, or surgery for CRS in past year |
During the patient's clinic exam, presence of nasal polyps was noted on endoscopy. Participants were classified by their treating Otolaryngologist into one of four CRS disease state classifications that are proposed for the conceptualization of CRS as a chronic episodic disease.13 The treating Otolaryngologists were blinded to the health utility and QOL study data other than the VAS.
Health Utility Assessment
Visual Analog Scale(VAS)
Participants were asked to make a mark where they felt their current CRS health state was on a 10 cm line with anchors at 0 labeled “worst imaginable health” and at 10 labeled “perfect health” and the measured distance divided by 10.14,16
Time Trade-Off(TTO)
The TTO method asks patients to compare their life with CRS to a life of full health.4,17 Patients were asked to choose between living 20 years with their current CRS symptoms or 10 years in perfect sinus health, then the number of years was adjusted until the patient found the choices equivalent and the ratio was determined.
Standard Gamble(SG)
For the SG method, patients were asked to choose between living with their current CRS symptoms for 20 years or taking a gamble which consisted of drawing a single marble out of a bag of 100 marbles.18,19 A white marble would lead to immediate cure of their sinus symptoms, while a black marble would cause instant death. The ratio of marbles in the bag was initially set at 99 white and 1 black marble, and the number of black marbles was increased until patients valued the gamble as equal to living with their current symptoms for the next 20 years. The final ratio of marbles bag was used as the health utility value.
36-Item Short Form Health Survey (SF-36)
Participants were asked to complete the SF-36 questionnaire(QualityMetric Inc, Lincoln, RI), which has been widely used as a generic quality-of-life measurement.11,20–23 The SF-36 covers 8 domains of quality-of-life, values in each area were converted to SF-6D values and subsequently into a single health utility value using the Sheffield Bayesian Excel Program(The University of Sheffield, Sheffield, UK).24–26
Sino-Nasal Outcome Test(SNOT-22)
The SNOT-22 is a disease specific quality-of-life measure that assesses the presence and severity of current symptoms and provides a total number representing disease burden.27,28 Its 22 items are graded from 0(“no problem”) to 5(“Problem as bad as it can be”). While not designed to measure health utility, the SNOT-22 is used in clinical practice to quantify the full burden of disease experienced by an individual patient.6 We additionally defined a SNOT Nasal score that included only the 7 questions(1/3/ 5/6/10/21/22) to determine the extent to which nasal symptoms correlated with health utility.
Statistical Methods
Mean health utilities were determined for each test for all disease-state classifications and for patients with and without nasal polyps. The distribution of health utilities was found to be non-normal for all four tests(Shapiro-Wilk VAS p<0.001,TTO p<0.001, SG p<0.001, SF-6D P=0.007) while SNOT-22 scores were normally distributed(p=0.07). Therefore, nonparametric analysis techniques were used.
Mean health utilities were compared across groups using the Kruskal-Wallis test or the Mann-Whitney U test and overall using a Friedman ANOVA. A Bonferroni correction was used due to multiple health utility assessments compared(p= 0.05/4 = 0.0125). Kruskal-Wallis and Friedman post-hoc multiple comparison analysis was performed using the Dunn Procedure.29 In order to assess the relationship among the health utility assessments and between health utility assessments and SNOT-22 and SNOT Nasal, Spearman correlation coefficients were calculated. We also carried out multivariate regression analysis in order to explain the variation in health utilities as a function of demographics (age, gender, and race), co-morbidities(asthma, allergic rhinitis), nasal polyposis, disease state, SNOT-22 and SNOT Nasal. Independent variables were removed from the model if their p-value was > 0.05 and if they did not substantially affect other parameter estimates. Separate regressions were carried out for different quality-of-life instruments. A stepwise multivariate regression was also performed to analyze the association of individual SNOT-22 questions with health utility. Test and retest correlations were calculated with Spearman correlations. All analysis was performed with SAS version 9.4(Statistical Analysis System Institute, Cary, NC). All statistical tests were carried out at the 0.05 significance level and adjusted for multiple comparisons when appropriate.
Results
Study population
Of the 149 patients consented and enrolled, 137(92%) patients completed all four health utility assessments(Table 2). There were no differences in CRS disease classification, age, gender, race, co-morbidities or nasal polyposis between patients who completed the health utility assessments and those who did not. 104(70%) patients completed all health utility assessments and the SNOT-22 questionnaire. Patients who did not complete the SNOT-22 questionnaire were on average slightly younger(49.6 +-14.5 years versus 44.5+-13.6, p=0.048) but did not differ in any other characteristics. 51 patients(41% of patients with stable CRS symptoms) completed the follow-up TTO and SG assessments, and patients who did not complete the follow-up assessments did not differ in any dimension.
Table 2.
Characteristics of the Study Population
| Overall | CRS | Exacerbation | Recalcitrant | Remitted | p-value | ||
|---|---|---|---|---|---|---|---|
| N=137 | N=60 | N=22 | N=45 | N=10 | |||
| Age (Y, Std Dev) | 48.1 +- 14.6 | 45.9 +- 14.9 | 46.4 +- 13.3 | 48.8+- 14.7 | 61.4 +- 7.7 | 0.016 | |
| Gender(N, %) | Female | 71 (51.8) | 27 (45.0) | 16 (72.7) | 24 (53.3) | 4 (40.0) | 0.13 |
| Male | 66 (48.2) | 33 (55.0) | 6 (27.3) | 21 (47.7) | 6 (60.0) | ||
| Race (N, %) (missing=2) | White | 117 (86.7) | 49 (83.1) | 19 (90.5) | 41 (91.1) | 8 (80.0) | 0.85 |
| Black | 11 (8.2) | 5 (8.5) | 2 (9.5) | 2 (4.4) | 2 (20.0) | ||
| Hispanic | 3 (2.2) | 2 (3.4) | 0 (0) | 1 (2.2) | 0 (0) | ||
| Asian | 2 (1.5) | 2 (3.4) | 0 (0) | 0 (0) | 0 (0) | ||
| Other | 2 (1.5) | 1 (1.7) | 0 (0) | 1 (2.2) | 0 (0) | ||
| Asthma (N, %) | 66 (48.2) | 27 (45.) | 11 (50.0) | 24 (53.3) | 4 (40.0) | 0.80 | |
| Allergic Rhinitis (N, %) | 82 (59.9) | 35 (58.3) | 12 (54.6) | 29 (64.4) | 6 (60.0) | 0.87 | |
| Nasal Polyps (N, %) | 61 (44.5) | 17 (28.3) | 6 (27.3) | 31 (68.9) | 7 (70.0) | <0.001 | |
| History of Sinus Surgery (N, %) | 96 (70.1) | 26 (43.3) | 18 (81.8) | 43 (95.6) | 9 (90.0) | <0.001 | |
| SNOT-22 Score N=104 (Mean, Std Dev) | 35.1 (19.5) | 36.9 (17.0) | 43.4 (19.1) | 34.2 (21.1) | 14.6 (13.9) | 0.003 |
Health utility measures
The mean health utilities based on the VAS, TTO, SG and SF-6D are shown in Table 3 by disease state classification, by presence of nasal polyposis and prior history of sinus surgery. Overall, the mean health utility differed significantly among the four methods of assessments (eFigure 1). The TTO and SG values differed significantly (p<0.05) from the other health utility assessments while the VAS and SF-6D values did not differ significantly. VAS differed significantly between disease state classification groups and between patients with and without polyps, but not between patients with and without a history of ESS. TTO, SG or SF-6D scores were not significantly different (Table 3, Figure 1 and eFigure 2).
Table 3.
Mean Health Utility Overall and by Disease State Classification and Nasal Polyposis
| Disease State Classifications Mean (Std Dev) | Polyp Classification Mean (Std Dev) | ESS Classification Mean (Std Deviation) | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Overall Mean (Std Dev) N=137 | Mean CRS, Exacerbation, and Recalcitrant Groups Combined (Std Dev) N=127 | CRS N=60 | Exacerbation N=22 | Recalcitrant N=45 | Remitted N=10 | Kruskal-Wallis* | No Polyps N=76 | Nasal Polyps N=61 | Mann-Whitney* | No History ESS N=41 | Prior ESS N=96 | Mann-Whitney | |
| VAS | 0.69 (0.19) | 0.68 (0.19) | 0.70 (0.18) | 0.61 (0.18) | 0.68 (0.21) | 0.87 (0.13) | 0.004 | 0.65 (0.19) | 0.74 (0.19) | 0.005 | 0.66 (0.21) | 0.70 (0.19) | 0.30 |
| TTO | 0.80(0.27) | 0.78 (0.28) | 0.76 (0.30) | 0.78 (0.25) | 0.81 (0.27) | 0.98 (0.05) | 0.055 | 0.77 (0.28) | 0.82 (0.26) | 0.24 | 0.70 (0.31) | 0.83 (0.25) | 0.014 |
| SG | 0.93 (0.11) | 0.93 (0.11) | 0.93 (0.11) | 0.92 (0.13) | 0.94 (0.10) | 1.00 (0.00) | 0.042 | 0.93 (0.13) | 0.95 (0.07) | 0.77 | 0.90 (0.15) | 0.96 (0.08) | 0.018 |
| SF-6D | 0.72 (0.12) | 0.71 (0.13) | 0.74 (0.14) | 0.68 (0.10) | 0.71 (0.13) | 0.76 (0.11) | 0.37 | 0.70 (0.12) | 0.73 (0.13) | 0.15 | 0.70 (0.12) | 0.72 (0.13) | 0.21 |
| Friedman p-value | <0.001 | <0.001 | <0.001 | <0.001 | <0.001 | <0.001 | <0.001 | <0.001 | <0.001 | <0.001 | |||
p-value (significance level = 0.0125)
Figure 1. Comparison of Mean Health Utility Assessment Values by Disease State Classification.
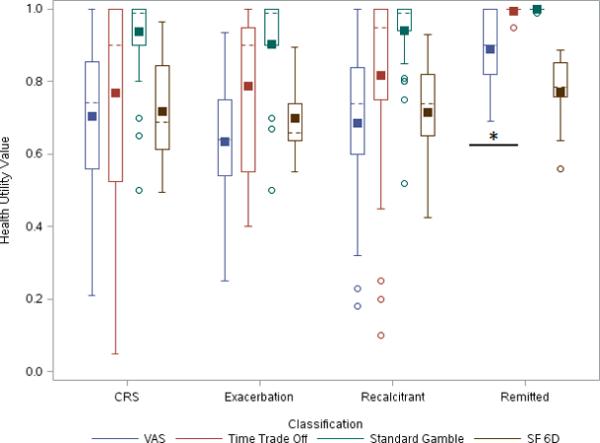
Dash line- median; Filled Square- mean; Open Circle- outliers; Asterix - p-value= 0.004 (patients with Remitted CRS had a significantly higher VAS score compared to patients in other disease states)
Test-retest reliability of health utility in stable disease
Both TTO and SG health utility assessment initial and retest values 3 weeks later in patients with stable CRS symptoms were stable and highly correlated(eTable 1).
Correlation of SNOT-22 with measures of health utility
Since a higher score on the SNOT-22 indicates a higher burden of illness, we would expect the correlations between SNOT-22 and health utility assessments to be negative and the correlations are in the expected direction for all four assessments(Table 4). Overall the different measures of health utility were weak, but significantly, correlated. Modest correlations were found between both VAS and SF-36 and SNOT-22 Total scores. SNOT Nasal had weaker correlations with all four health utility assessments compared to SNOT-22 Total.
Table 4.
Correlations among Methods of Determining Health Utility and between Health Utility Assessments and SNOT-22
| VAS | TTO | SG | SF 36 | SNOT 22 | |
|---|---|---|---|---|---|
| VAS | 1.000 | ||||
| TTO | 0.361 | 1.000 | |||
| <0.001 | |||||
| SG | 0.273 | 0.448 | 1.000 | ||
| 0.001 | <0.001 | ||||
| SF-6D | 0.397 | 0.353 | 0.206 | 1.000 | |
| <0.001 | <0.001 | 0.016 | |||
| SNOT 22 | −0.475 | −0.388 | −0.330 | −0.648 | 1.000 |
| <0.001 | <0.001 | <0.001 | <0.001 | ||
| SNOT Nasal | −0.331 | −0.291 | −0.227 | −0.328 | 0.787 |
| <0.001 | 0.003 | 0.020 | <0.001 | <0.001 |
Regression analysis of factors associated with health utility
The regression analysis(eTable 2) confirmed the results of the correlation analysis. SNOT-22 Total score was associated with VAS, TTO and SF-6D but not SG health utility assessment when adjusted for gender, race, asthma, allergic rhinitis, and history of sinus surgery. As SNOT-22 Total score increased by one point, health utility assessment decreased for these three tests by 0.0039-0.0051. The explanatory power was highest for the regressions explaining the SF-6D model. A separate set of regression analyses were performed with SNOT Nasal, and the score was significantly associated with VAS, TTO and SF-6D but not SG values. Similar to the correlation results, the explanatory power of SNOT Nasal was lower than that of SNOT-22 for all health utility assessments.
When individual SNOT-22 questions were regressed against the health utility values, no question was individually significantly associated with TTO or VAS score. Question 19, reduced concentration, was associated with SG values, and questions 15, lack of a good night's sleep, and 17, fatigue, were associated with SF-6D values.
Discussion
This study compared measures of health utility in a cohort of CRS patients diagnosed using consensus guidelines. We further evaluated the effect of timing of assessment using a chronic episodic disease model. We found estimates of health utility among CRS patients at baseline, during exacerbations, and among recalcitrant CRS to be relatively stable. VAS scores were significantly higher for patients with remitted CRS compared to the other disease states. Findings were similar, but not significant, for TTO and SG. VAS scores were also significantly higher for patients with nasal polyps compared to those without nasal polyps, but not for symptomatic patients with or without a history of ESS. TTO, SG, and SF-6D scores were not significantly different for CRS patients with or without nasal polyps or history of ESS. VAS, TTO and SF-6D scores were significantly associated with SNOT-22, but SG was not.
Consistent with our findings, previous studies of chronic and acute health states found a strong tendency for VAS to yield the lowest estimates of health utility, TTO the middle while SG yields the highest.12,30 The VAS approach has the least grounding in economic theory because it does not involve an element of choice or decision making under uncertainty.12 However, it is often used as a “warm up” to TTO or SG exercises, or as part of the EQ-5D, in order to allow patients to become familiar with rating health states.12 Our VAS estimates are similar to those reported by Remenschneider et al. as part of their study on EQ-5D among patients undergoing surgery for CRS, where they found a baseline VAS of 73.9 +- 16.2 compared to 69.1+- 19.5 in our study and 84.3 +- 23.8 in the general U.S. population.14 Similar to Zheng et al., we found that VAS utility was higher in patients with nasal polyps compared to those without.9
We are aware of no prior studies that have applied direct measures of health utility to populations of CRS patients. The TTO method is based on value theory while the SG is based on expected utility theory. The TTO assumes the choice is made under conditions of certainty, while the SG is dependent on the risk behavior of the individual. TTO utility estimates will be lower than SG values among risk averse patients especially in non life-threatening illness.12 This phenomenon is demonstrated in our data, as TTO estimates were consistently lower than SG estimates for patients with the same CRS disease state. In general, health economists support the use of choice-based methods(SG or TTO) over the VAS, however these approaches are relatively time-consuming and some patients have difficulties understanding the concept of probabilities.12 Even with trained study coordinators, two patients interviewed were unable to complete the SG exercise because of difficulty understanding the methodology. Of note, the SG was not significantly associated with SNOT-22 in the multivariate analysis suggesting factors besides disease-specific burden may drive variability. Both direct measures also exhibited significant ceiling effect, with many risk averse patients selecting high utility values.31 Additionally, the TTO values have the highest standard deviation across CRS health states and exhibit the largest differences between median and mean estimates, suggesting significant variability and skewing in TTO-obtained utility estimates.12
Generic instruments, such as the EQ-5D, HUI-Mark III and SF-6D, address some of the practical difficulties of conducting direct assessments and have been used to measure CRS health utility.11,12,14,32All can be completed in minutes and do not require modification for specific diseases.12 However, generic questionnaires may not cover aspects of health affected by CRS or reflect utility changes arising spontaneously or as a result of interventions.33 These instruments also differ in their descriptive attributes and valuation objectives- the EQ-5D has been valued using TTO while the SF-6D is derived from the SF-36 and utilizes SG valuation.12,24
The Bayesian algorithms for conversion of generic instruments to health utility were developed using data on patients with general medical conditions in the U.K. and the domains measured may not be relevant for CRS or reflect U.S. population preferences.34 Our SF-6D utility estimate of 0.72(95% CI 0.69-0.74), is slightly higher than that of Soler et al. who found a value of 0.65(CI 0.63-0.66) in their study of SF-6D values in patients undergoing endoscopic sinus surgery.11 However, their estimate was based on patients who had failed medical therapy and were planned for initial or revision ESS. Both estimates are lower than our SG utility estimate of 0.93 even though the SF-6D conversion was based on SG valuation. The SF-6D might further be unresponsive to change in disease states as SF-6D showed the least improvement between symptomatic and remitted states and utility estimates obtained when minimally symptomatic did not approach 1.0. Prior studies using SF-6D scores have found an improvement from 0.67 at baseline to 0.75 in the short term (average 1.5 years) and 0.80 in the long term (average 5.2 years) after ESS.11,22 Our findings indicate that a greater difference in utility scores based on disease state may have been found using the TTO or SG valuation techniques. The lack of responsiveness in generic questionnaires has previously led to the development of disease specific questionnaires such as SNOT-22, however at this time there is no conversion of a CRS disease specific questionnaire to a health utility value.11
Interestingly, while the SNOT-22 total scores had weak but highly significant correlations with the utility measures, few individual SNOT-22 items were associated with utility estimates. Only “reduced concentration” was associated with SG values and “lack of a good night's sleep” and “fatigue” were associated with SF-6D values, but no individual symptoms were significantly associated with either TTO or VAS values. Previously, Remenschneider et al. found that symptoms of fatigue, reduced productivity and reduced concentration were most closely correlated with pre-operative VAS and ear pain, dizziness and irritability were associated with change in VAS post-operatively using stepwise regression.14 These findings provide insight into the types of CRS symptoms which affect patients’ view of their overall health, but suggest that cardinal disease symptoms may not be significant drivers of a patient's perception of utility. Moreover, while a conversion factor between a CRS-specific QOL instrument (such as SNOT-22 score) and a utility score would be useful, the low correlation of SNOT-22 with VAS, TTO, and SG makes a viable conversion algorithm unlikely.
Our study suggests that the TTO, VAS and SF-6D population estimates are fairly consistent, but there were large random errors within estimates obtained via each method. Individuals also had large differences in their health utility levels depending on what techniques were used. This leads to poor correlation even though the methods measure fundamentally similar ideas.4 This is especially true for the SG and TTO method, where difficult and hypothetical choice situations are presented to the patients resulting in significant ceiling effects when risk averse patients select high utility values.4 These direct measures require significant time to administer and trained interviewers. The advantages of quality-of-life instruments, such as SF-6D and EQ-5D, are that they are easy to administer and understand, which leads to lower random errors and higher reliability but may have the consequence of lower responsiveness to disease-specific changes.4 This may result in a significant underestimation of cost-effectiveness of CRS treatment in studies that have relied on this methodology.11,34 A limitation of this study is the relatively small sample size of 137 patients. Patients may not be representative of all patients with CRS as our sample was drawn from a tertiary medical center and also may underrepresent minority patients. The response rates of patients enrolled are similar to previous studies of quality-of-life in CRS.11,14
Finally, the health utility estimates obtained in this study can be compared with estimates for other chronic diseases and with the general U.S. population. U.S. population norms have previously been estimated on cross sectional surveys as VAS 0.661-0.872 and SF-6D 0.700-0.872 depending on age and gender(VAS 0.884 and SF-6D 0.885 in patients with no chronic health problems),11,32,35–38 and TTO 0.936 and SG 0.946 on a survey of primary care patients.39 A 1999 cross sectional survey of Canadians used the HUI-Mark III to measure utility scores for a range of chronic diseases, including self-reported sinusitis which was present in 5% of the population with a score of 0.84.32 The study did not differentiate between acute versus chronic sinusitis nor was CRS defined using guideline criteria.32 CRS patients in our study show significant impairment in quality-of-life with health utility values similar to the published values for asthma(VAS 0.68, TTO 0.89, SG 0.91), AIDS patients(VAS 0.69, TTO 0.81, SG 0.80) or patients with arteriosclerosis obliterans and intermittent claudication(VAS 0.74, TTO 0.76, SG 0.86).4,30 However, patients were enrolled from a tertiary level clinic and there may be selection bias for more severe disease compared to a cohort of patients with CRS sampled from a primary care office. Our TTO utility estimates would suggest that moving from symptomatic CRS to a remitted disease state (0.76 vs. 0.98, difference of 0.22) would result in 4.4 QALYs assuming 20 remaining years of persistent disease (20 years × 0.22 utility change). At a cost per QALY ratio of $50,000, an interventions that accurately diagnose CRS patients and direct them toward therapies that reliably achieve this change in disease state may be cost-effective even up to the price of $220,000 (4.4 QALYs × $50,000 per QALY).40 Further research is necessary to determine the natural history of CRS and evaluate the effectiveness of treatments in achieving CRS remission in order to fully evaluate the cost-effectiveness of interventions for CRS.
Conclusion
CRS patients show significant impairment in quality-of-life, with health utility values similar to patients with AIDS or intermittent claudication using similar methods. The method of ascertainment significantly affects measured health utility, with VAS and SF-6D health utility estimates being lower and SG estimates higher. Only VAS scores differed based on disease state classification or the presence of nasal polyposis. VAS, TTO and SF-6D scores were significantly associated with SNOT-22, however SG and SNOT-22 were poorly correlated. The test-retest reliability of TTO and SG estimates in patients with stable CRS was strong.
Supplementary Material
Acknowledgements
Drs Ference and Tan had full access to all of the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis. The authors have no potential conflicts of interest. This work was supported by NIH grant K23DC012067 (B.K.T) and the Triological Society/ American College of Surgeons (B.K.T), Chronic Rhinosinusitis Integrative Studies Program (CRISP) P01 AI106683 (B.K.T and R.C.K). The funders had no role in the design and conduct of the study; collection, management, analysis and interpretation of the data; or the preparation, review or approval of the manuscript. This study was approved by the Northwestern University Institutional Review Board.
Footnotes
Conflicts of Interest/ Financial Disclosures: None
Meeting: Some of this data was presented as a poster presentation at the 117th Triological Society Annual Meeting, Las Vegas, NV May 17, 2014
Works Cited
- 1.Hamilos DL. Chronic rhinosinusitis: epidemiology and medical management. J Allergy Clin Immunol. 2011;128(4):693–707. doi: 10.1016/j.jaci.2011.08.004. quiz 708-9. doi:10.1016/j.jaci.2011.08.004. [DOI] [PubMed] [Google Scholar]
- 2.Smith SS, Kern RC, Chandra RK, Tan BK, Evans CT. Variations in antibiotic prescribing of acute rhinosinusitis in United States ambulatory settings. Otolaryngol Head Neck Surg. 2013;148(5):852–9. doi: 10.1177/0194599813479768. doi:10.1177/0194599813479768. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Fokkens WJ, Lund VJ, Mullol J, et al. European Position Paper on Rhinosinusitis and Nasal Polyps 2012. [October 28, 2014];Rhinol Suppl. 2012 (23):3. preceding table of contents, 1-298. Available at: http://www.ncbi.nlm.nih.gov/pubmed/22764607. [PubMed]
- 4.Blumenschein K, Johannesson M. Relationship between quality of life instruments, health state utilities, and willingness to pay in patients with asthma. Ann Allergy Asthma Immunol. 1998;80(2):189–94. doi: 10.1016/S1081-1206(10)62954-7. doi:10.1016/S1081-1206(10)62954-7. [DOI] [PubMed] [Google Scholar]
- 5.Linder JA, Atlas SJ. Health-related quality of life in patients with sinusitis. [June 25, 2014];Curr Allergy Asthma Rep. 2004 4(6):490–5. doi: 10.1007/s11882-004-0017-1. Available at: http://www.ncbi.nlm.nih.gov/pubmed/15462717. [DOI] [PubMed] [Google Scholar]
- 6.Soler ZM, Smith TL. Quality of life outcomes after functional endoscopic sinus surgery. Otolaryngol Clin North Am. 2010;43(3):605–12. x. doi: 10.1016/j.otc.2010.03.001. doi:10.1016/j.otc.2010.03.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Stewart MG, Smith TL. Objective versus subjective outcomes assessment in rhinology. [June 26, 2014];Am J Rhinol. 19(5):529–35. Available at: http://www.ncbi.nlm.nih.gov/pubmed/16270610. [PubMed] [Google Scholar]
- 8.Bhattacharyya N. A comparison of symptom scores and radiographic staging systems in chronic rhinosinusitis. [July 10, 2014];Am J Rhinol. 19(2):175–9. Available at: http://www.ncbi.nlm.nih.gov/pubmed/15921217. [PubMed] [Google Scholar]
- 9.Zheng Y, Zhao Y, Lv D, et al. Correlation between computed tomography staging and quality of life instruments in patients with chronic rhinosinusitis. Am J Rhinol Allergy. 24(1):e41–5. doi: 10.2500/ajra.2010.24.3430. doi:10.2500/ajra.2010.24.3430. [DOI] [PubMed] [Google Scholar]
- 10.Dietz de Loos DAE, Hopkins C, Fokkens WJ. Symptoms in chronic rhinosinusitis with and without nasal polyps. Laryngoscope. 2013;123(1):57–63. doi: 10.1002/lary.23671. doi:10.1002/lary.23671. [DOI] [PubMed] [Google Scholar]
- 11.Soler ZM, Wittenberg E, Schlosser RJ, Mace JC, Smith TL. Health state utility values in patients undergoing endoscopic sinus surgery. Laryngoscope. 2011;121(12):2672–8. doi: 10.1002/lary.21847. doi:10.1002/lary.21847. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Tolley K. [June 26, 2014];What Are Health Utilities? 2009:1–8. Available at: http://www.medicine.ox.ac.uk/bandolier/painres/download/whatis/Health-util.pdf. [Google Scholar]
- 13.Tan BK, Kern RC, Schleimer RP, Schwartz BS. Chronic rhinosinusitis: the unrecognized epidemic. Am J Respir Crit Care Med. 2013;188(11):1275–7. doi: 10.1164/rccm.201308-1500ED. doi:10.1164/rccm.201308-1500ED. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Remenschneider AK, D'Amico L, Gray ST, Holbrook EH, Gliklich RE, Metson R. The EQ-5D: A new tool for studying clinical outcomes in chronic rhinosinusitis. Laryngoscope. 2014 doi: 10.1002/lary.24715. doi:10.1002/lary.24715. [DOI] [PubMed] [Google Scholar]
- 15.Fokkens WJ, Lund VJ, Mullol J, et al. EPOS 2012: European position paper on rhinosinusitis and nasal polyps 2012. A summary for otorhinolaryngologists. Rhinology. 2012;50(1):1–12. doi: 10.4193/Rhino12.000. doi:10.4193/Rhino50E2. [DOI] [PubMed] [Google Scholar]
- 16.Soler ZM, Mace J, Smith TL. Symptom-based presentation of chronic rhinosinusitis and symptom-specific outcomes after endoscopic sinus surgery. Am J Rhinol. 22(3):297–301. doi: 10.2500/ajr.2008.22.3172. doi:10.2500/ajr.2008.22.3172. [DOI] [PubMed] [Google Scholar]
- 17.Torrance GW, Thomas WH, Sackett DL. A utility maximization model for evaluation of health care programs. [June 25, 2014];Health Serv Res. 1972 7(2):118–33. Available at: http://www.pubmedcentral.nih.gov/articlerender.fcgi?artid=1067402&tool=pmcentrez&rendertype=abstract. [PMC free article] [PubMed] [Google Scholar]
- 18.Sox H, Blatt M, Higgins M, Marton K. Medical Decision Making. 1st edition The American College of Physicians; 2006. p. 406. [Google Scholar]
- 19.Garza AG, Wyrwich KW. Health utility measures and the standard gamble. [June 25, 2014];Acad Emerg Med. 2003 10(4):360–3. doi: 10.1197/aemj.10.4.360. Available at: http://www.ncbi.nlm.nih.gov/pubmed/12670850. [DOI] [PubMed] [Google Scholar]
- 20.Wang P-C, Tai C-J, Lin M-S, Chu C-C, Liang S-C. Quality of life in Taiwanese adults with chronic rhino-sinusitis. [June 25, 2014];Qual Life Res. 2003 12(4):443–8. doi: 10.1023/a:1023494025748. Available at: http://www.ncbi.nlm.nih.gov/pubmed/12797716. [DOI] [PubMed] [Google Scholar]
- 21.Baumann I, Blumenstock G. Impact of gender on general health-related quality of life in patients with chronic sinusitis. [June 25, 2014];Am J Rhinol. 19(3):282–7. Available at: http://www.ncbi.nlm.nih.gov/pubmed/16011135. [PubMed] [Google Scholar]
- 22.Rudmik L, Mace J, Soler ZM, Smith TL. Long-term utility outcomes in patients undergoing endoscopic sinus surgery. Laryngoscope. 2014;124(1):19–23. doi: 10.1002/lary.24135. doi:10.1002/lary.24135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Gliklich RE, Metson R. The health impact of chronic sinusitis in patients seeking otolaryngologic care. [May 31, 2014];Otolaryngol Head Neck Surg. 1995 113(1):104–9. doi: 10.1016/S0194-59989570152-4. Available at: http://www.ncbi.nlm.nih.gov/pubmed/7603703. [DOI] [PubMed] [Google Scholar]
- 24.Brazier J, Usherwood T, Harper R, Thomas K. Deriving a preference-based single index from the UK SF-36 Health Survey. [June 24, 2014];J Clin Epidemiol. 1998 51(11):1115–28. doi: 10.1016/s0895-4356(98)00103-6. Available at: http://www.ncbi.nlm.nih.gov/pubmed/9817129. [DOI] [PubMed] [Google Scholar]
- 25.Kharroubi SA, Brazier JE, Roberts J, O'Hagan A. Modelling SF-6D health state preference data using a nonparametric Bayesian method. J Health Econ. 2007;26(3):597–612. doi: 10.1016/j.jhealeco.2006.09.002. doi:10.1016/j.jhealeco.2006.09.002. [DOI] [PubMed] [Google Scholar]
- 26. [June 26, 2014];Bayesian programme - SF-6D - Measuring & Valuing Health - HEDS - Sections - ScHARR - The University of Sheffield. Available at: https://www.sheffield.ac.uk/scharr/sections/heds/mvh/sf-6d/bayesian.
- 27.Hopkins C, Gillett S, Slack R, Lund VJ, Browne JP. Psychometric validity of the 22-item Sinonasal Outcome Test. Clin Otolaryngol. 2009;34(5):447–54. doi: 10.1111/j.1749-4486.2009.01995.x. doi:10.1111/j.1749-4486.2009.01995.x. [DOI] [PubMed] [Google Scholar]
- 28.Piccirillo JF, Merritt MG, Richards ML. Psychometric and clinimetric validity of the 20-Item Sino-Nasal Outcome Test (SNOT-20). [June 25, 2014];Otolaryngol Head Neck Surg. 2002 126(1):41–7. doi: 10.1067/mhn.2002.121022. Available at: http://www.ncbi.nlm.nih.gov/pubmed/11821764. [DOI] [PubMed] [Google Scholar]
- 29.Elliott AC, Hynan LS. A SAS(®) macro implementation of a multiple comparison post hoc test for a Kruskal-Wallis analysis. Comput Methods Programs Biomed. 2011;102(1):75–80. doi: 10.1016/j.cmpb.2010.11.002. doi:10.1016/j.cmpb.2010.11.002. [DOI] [PubMed] [Google Scholar]
- 30.Morimoto T, Fukui T. Utilities measured by rating scale, time trade-off, and standard gamble: review and reference for health care professionals. [June 26, 2014];J Epidemiol. 2002 12(2):160–78. doi: 10.2188/jea.12.160. Available at: http://www.ncbi.nlm.nih.gov/pubmed/12033527. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Guyatt GH, Feeny DH, Patrick DL. Measuring health-related quality of life. [June 12, 2014];Ann Intern Med. 1993 118(8):622–9. doi: 10.7326/0003-4819-118-8-199304150-00009. Available at: http://www.ncbi.nlm.nih.gov/pubmed/8452328. [DOI] [PubMed] [Google Scholar]
- 32.Mittmann N, Trakas K, Risebrough N, Liu BA. Utility scores for chronic conditions in a community-dwelling population. [September 13, 2014];Pharmacoeconomics. 1999 15(4):369–76. doi: 10.2165/00019053-199915040-00004. Available at: http://www.ncbi.nlm.nih.gov/pubmed/10537955. [DOI] [PubMed] [Google Scholar]
- 33.Juniper EF, Thompson AK, Roberts JN. Can the standard gamble and rating scale be used to measure quality of life in rhinoconjunctivitis? Comparison with the RQLQ and SF-36. [June 25, 2014];Allergy. 2002 57(3):201–6. doi: 10.1034/j.1398-9995.2002.1o3306.x. Available at: http://www.ncbi.nlm.nih.gov/pubmed/11906333. [DOI] [PubMed] [Google Scholar]
- 34.Rudmik L, Soler ZM, Mace JC, Schlosser RJ, Smith TL. Economic evaluation of endoscopic sinus surgery versus continued medical therapy for refractory chronic rhinosinusitis. Laryngoscope. 2015;125(1):25–32. doi: 10.1002/lary.24916. doi:10.1002/lary.24916. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Luo N, Johnson JA, Shaw JW, Feeny D, Coons SJ. Self-reported health status of the general adult U.S. population as assessed by the EQ-5D and Health Utilities Index. [September 7, 2014];Med Care. 2005 43(11):1078–86. doi: 10.1097/01.mlr.0000182493.57090.c1. Available at: http://www.ncbi.nlm.nih.gov/pubmed/16224300. [DOI] [PubMed] [Google Scholar]
- 36.Hanmer J, Lawrence WF, Anderson JP, Kaplan RM, Fryback DG. Report of nationally representative values for the noninstitutionalized US adult population for 7 health-related quality-of-life scores. Med Decis Making. 26(4):391–400. doi: 10.1177/0272989X06290497. doi:10.1177/0272989X06290497. [DOI] [PubMed] [Google Scholar]
- 37.Fryback DG, Dunham NC, Palta M, et al. US norms for six generic health-related quality-of-life indexes from the National Health Measurement study. Med Care. 2007;45(12):1162–70. doi: 10.1097/MLR.0b013e31814848f1. doi:10.1097/MLR.0b013e31814848f1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Bharmal M, Thomas J. Comparing the EQ-5D and the SF-6D descriptive systems to assess their ceiling effects in the US general population. Value Health. 9(4):262–71. doi: 10.1111/j.1524-4733.2006.00108.x. doi:10.1111/j.1524-4733.2006.00108.x. [DOI] [PubMed] [Google Scholar]
- 39.Wells KB, Sherbourne CD. Functioning and utility for current health of patients with depression or chronic medical conditions in managed, primary care practices. [September 7, 2014];Arch Gen Psychiatry. 1999 56(10):897–904. doi: 10.1001/archpsyc.56.10.897. Available at: http://www.ncbi.nlm.nih.gov/pubmed/10530631. [DOI] [PubMed] [Google Scholar]
- 40.Neumann PJ, Cohen JT, Weinstein MC. Updating Cost-Effectiveness — The Curious Resilience of the $50,000-per-QALY Threshold. N Engl J Med. 2014;371(9):796–797. doi: 10.1056/NEJMp1405158. doi:10.1056/NEJMp1405158. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


