Abstract
Background
Racial disparities in access to care and access to high quality care have been persistent over many decades. They have been documented in all areas of health care, including ambulatory care. Policy initiatives have been implemented to address disparities and close the gaps in care that minorities face. Less is known about the effectiveness of these polices.
Objectives
To evaluate whether disparities in quality of ambulatory care have abated during the 2000 decade by answering two questions: 1) Were there differences in ambulatory care sensitive hospital admissions rates by race? 2) Have these differences been declining over time?
Research design
Multivariable linear regressions with fixed county effects and robust standard errors of longitudinal panel data.
Subjects
4,032,322 discharges in 172 counties in 6 states during 2003–2009.
Measures
Prevention Quality Indicators (PQIs) developed by the Agency for Healthcare Research and Quality, by county and race calculated from the HCUP data set.
Results
In 2003 the overall PQI admission rates were higher for African-Americans (around 16.5/1000) than for Whites (around 15/1000). By 2009, the overall and the chronic PQI admission rates declined significantly (p< 0.01) for Whites. They either did not decline or increased for African-Americans. Acute PQI rates declined significantly for Whites and remained stable for African-Americans.
Conclusions
Policies addressing persisting racial disparities in quality of ambulatory care for African-Americans should focus on the chronic PQIs. Additionally, efforts should be made to improve data quality for race and ethnicity information on hospital discharge data to enable informed policy evaluation and planning.
Keywords: disparities, quality of care, ambulatory care sensitive conditions
INTRODUCTION
Racial disparities in health care are not a new phenomenon. They have been documented, discussed, and the subject of policies designed to ameliorate or eliminate them for decades.1 As far back as 1964, with the passage of Title VI of the 1964 Civil Rights Act, the U.S. Department of Health and Human Services (DHHS) was charged with enforcing federal statutes and regulations prohibiting discrimination in health care. Recent policy initiatives include the 1999 Congressional mandate to the Agency for Healthcare Research and Quality (AHRQ) to produce an annual “National Healthcare Disparities Report”.2 Healthy People 2010 and 2010 goals include reducing disparities.3 The final review of Healthy People 2010, however, reported that of the 169 disparities related objectives for which data were available, overall there was no change during the decade, as disparities decreased for 27 and increased for 25.4
In this study we examine disparities in quality of acute and chronic primary-care. We adopt the approach pioneered by Billings et al.,5 which relies on comparisons of hospital admission rates for conditions that could have been prevented had the patient received high quality primary care. These admissions, called ambulatory care sensitive (ACS), have been used extensively to assess quality of ambulatory care6,7 and disparities in care.8,9
Previous studies reported higher ACS admissions for African Americans compared with Whites,10–16 indicating that African Americans receive lower quality ambulatory care. While most studies were cross sectional, several examined trends over time. Davis et al.17 found that gaps in the hospitalization rates of African Americans compared to non-Hispanic Whites for certain chronic conditions widened between 1991 and 1998. Similarly, ACS hospitalizations between 1998 and 2006 in Tennessee for African Americans did not experience the same improvement in trends, especially for the chronic ACS admissions, as experienced by Whites.18 Moy et al.19 investigated ACS admissions trends during the more recent 2001–2009 period and concluded that disparities, measured by an overall composite, have persisted.
In this study we expand on the Moy et al. study in several ways. We study trends in ACS admissions controlling for several important additional factors likely to influence ACS admissions, including insurance and population health-status. We also investigate separately trends for acute and chronic ACS conditions, hypothesizing that they may exhibit different trends because they arise due to different processes of care (see discussion section).
METHODS
Data and sample
The study included 6 states: Arizona, California, Colorado, Florida, Iowa, and New York. These states were chosen because they include relatively large minority populations, are in different regions of the country, and have a mix of urban and rural areas with high and low incomes. While these 6 states do not offer a nationally representative population, they do provide a diverse population, capturing differences in culture, health care system characteristics, and practices styles,20 all of which may affect disparities, as discussed below.
We obtained hospital discharge data for these states from the State Inpatient Database (SID) for the period 2003–2009, the most recent data available at the time the analyses were performed. The SID was developed as part of the Healthcare Cost and Utilization Project (HCUP) by AHRQ.21 It contains data for all patients admitted to all acute care community hospitals. The information includes age, gender, race, diagnoses and procedures, county of residence, and admission and discharge dates.
To obtain population characteristics we merged the SID data with the population file accompanying the AHRQ PQI software. We also obtained median household income by county from the Census and Medicare and Medicaid enrollment by county from the Area Resource Files.
Two data exclusions were applied
Exclusions due to poor quality race data
Race information in the SID is not always accurate. We followed the methodology recommended by AHRQ. Hospitals with poor quality race data were excluded if: (1) more than 30% of discharges in the hospital recorded patient race as “other”; (2) more than 50% of discharges in the hospital were missing race; or (3) all discharges in the hospital were recorded as “white”, “other” or “missing”.22 In our data the number of excluded hospitals varied by state and year. It ranged from zero in some states to as many as 24 (30%) for Colorado in 2006.
Exclusion due to unstable admission rates
Some counties had very few African American admissions. This lowers the accuracy and stability of the rate estimates. We, therefore, excluded all counties with less than a minimum African American population. To evaluate the effect of this exclusion on our findings, we repeated and present analyses, setting the exclusions at different levels ranging from a low of 1,000 to a high of 10,000 African Americans. This resulted in samples with numbers of counties ranging from a high of 172 to a low of 65 respectively. 116 counties did not meet even the low threshold of 1000 African Americans and were excluded altogether.
Variables
The dependent variables were county ACS admission rates by race and by year. Preventable hospitalizations were measured using the Prevention Quality Indicators (PQIs) developed by AHRQ.23 Using the QI SAS Version 4.4 software and the SID, we calculated the PQI Overall Composite Rate (PQI90), and its two sub-components, the Chronic Composite Rate (PQI92) and the Acute Composite Rate (PQI91).
The PQIs are ACS admissions developed and validated by AHRQ to identify access to and quality of care for “ambulatory care sensitive conditions.” The overall PQI composite rate includes admissions of people 18 and older. They include 8 chronic conditions: diabetes with short-term complications, diabetes with long-term complications, uncontrolled diabetes without complications, diabetes with lower-extremity amputation, asthma, hypertension, congestive heart failure, angina without a cardiac procedure; and 3 acute conditions: dehydration, bacterial pneumonia, or urinary tract infection. Although chronic obstructive pulmonary disease (COPD) admissions are normally included in PQI90 and PQI92, because the definition of a COPD admission changed during the period we studied, we created overall and chronic composite rates that excluded COPD, as suggested by AHRQ. Because four of the eight chronic PQI measures relate to diabetes, we also performed sub-analyses for the diabetes PQIs and “other chronic” PQIs separately.
As our interest was in understanding time trends in ACS admission rates vis-a-vis race, we included in the analyses several variables that are likely to influence ACS admission rates and hence confound the estimated time trend. To account for demographic variations we included county-level population rates for 4 age categories (18–39, 40–64, 65–74 and 75+) and the population rates for females. To control for cross-sectional and longitudinal variations in population health status we included four county level race-specific admission rates for marker conditions. These are low variation admission rate conditions, which are not likely to be influenced by the quality of ambulatory care provided in the county and are more likely to reflect unexplained differences in the health status of the populations.7,24 These included: (1) Appendicitis with appendectomy (2) Acute myocardial infarction with a length of stay greater than 5 days or a disposition of death (3) Gastrointestinal obstruction (4) Fracture of hip/femur for ages 45 and older. These were calculated from the SID as well. We also included Medicare and Medicaid enrollment rates in the county and county median household income. Other potential variables that might influence the ACS admission rates, such as local practice styles, primary-care physician density 7, managed care penetration rates,6,7,25,26 and rurality27–29 were either not available longitudinally or are stable over time. Therefore, we also included county fixed effects to control for these and other time invariant factors.
Statistical Analysis
We estimated two models, one for Whites and one for African Americans, as follows:
where t denotes year and j denotes county. The unit of analysis was the county. The PQI composite rate in year t and county j was the dependent variable. We estimated longitudinal panel linear regression models with a time variable (t) to capture the trend, time varying demographic variables (age and female population rates), a vector X of other time-varying covariates (marker admission rates, median income, Medicare and Medicaid enrollment rates), fixed time-invariant county effects, and robust standard errors with clustering at the county level to control for heteroscedasticity. We used seemingly unrelated estimation to compare the coefficients for time across the two equations for the two races and tested for equality of the time coefficients across models using the Wald test.
RESULTS
Table 1 shows a comparison of the 172 counties in the analysis to the 116 that were excluded, and to all U.S. counties. Counties in the analysis are more diverse, larger in terms of population (mean of 477,246 compared with 36,541 in the excluded counties and 78,142 in the U.S.), have higher median household income ($47,671 compared with $43,365 and $40,658 respectively), and are less likely to be rural (12% compared with 50% and 44% respectively).
Table 1.
Comparison of analysis counties for the overall composite PQI to those excluded in 2006
| Analysis Counties N=172 | Excluded Counties N=116 | All counties in the U.S. N=3,147 | ||||
|---|---|---|---|---|---|---|
| Mean | SD | Mean1 | SD | Mean2 | SD | |
| Population3 | 477,246 | 936,518 | 36,541* | 31,880 | 78,142* | 277,911 |
| Percent of adults | ||||||
| Age 18–39 | 38 | 7 | 34* | 6 | 35* | 7 |
| Age 40–64 | 43 | 3 | 46* | 4 | 45* | 4 |
| Age 65–74 | 10 | 3 | 10 | 2 | 10* | 2 |
| Age 75 and older | 9 | 3 | 9 | 3 | 9* | 3 |
| Male | 50 | 3 | 50 | 3 | 49* | 3 |
| Female | 50 | 3 | 50 | 3 | 51* | 3 |
| Non-Hispanic white | 69 | 19 | 81* | 18 | 80* | 20 |
| African American | 9 | 8 | 1* | 1 | 9 | 14 |
| Hispanic | 16 | 15 | 13 | 15 | 7* | 12 |
| Asian and Pacific | 4 | 5 | 1* | 1 | 1* | 3 |
| Islander | ||||||
| Median Household Income in $4 | 47,671 | 12,003 | 43,365* | 9,929 | 40,658* | 10,508 |
| Poverty Percent All Ages | 14 | 5 | 13 | 6 | 15* | 6 |
| Percent of persons 25years and older with less than a high school diploma (2005–2009)5 | 16 | 7 | 14* | 6 | 18* | 8 |
| Percent of population eligible for Medicare6 | 16 | 5 | 17* | 4 | 17* | 4 |
| Percent of population eligible for Medicaid | 21 | 9 | 20 | 9 | 20 | 9 |
| N | % | N | % | N | % | |
| Rural7 | 20 | 12 | 58* | 50 | 1,382* | 44 |
*denotes a statistically significant difference (at the 0.05 level) between sample and excluded counties
*denotes a statistically significant difference (at the 0.05 level) between sample and U.S. cities
Source: Intercensal population estimates for 2006 accompanying the AHRQ PQI SAS 4.4 software; also the source for the age and gender comparisons.
Source: Small Area Income and Poverty Estimates for 2006. http://www.census.gov/did/www/saipe/data/statecounty/data/index.html Also the source for poverty percent all ages. (N=3,140 non-missing US counties)
Source: Area Resource File 2011–2012 Version http://arf.hrsa.gov/ (N=3,143 non-missing US counties)
Source: Area Resource File 2013–2014 Version. http://arf.hrsa.gov/ Also the source for percent of population eligible for Medicaid. (N=3,139 non-missing US counties)
Source: Non-metro areas as defined by the Office of Management and Budget issued in 2003. http://www.census.gov/population/metro/data/pastmetro.html
Table 2 provides descriptive statistics for the 4 samples we analyzed. The data are provided for 2006 – the midyear of our study. Whites and African Americans were split about evenly between males and females except for the largest sample which included the smallest counties, where Blacks tended to have more males, at 55.76%. The age distribution was similar across both samples and races, with about 80% of the population below the age of 65. Most surprising were the rates for the marker conditions, which while mostly stable across samples, varied substantially across the two races, with the rates for Whites being higher than the rates for African Americans, by as much as a factor of 5 for hip or femur fracture for ages 45+.
Table 2.
Descriptive Statistics for County Level Variables in 2006 by Race and Sample Size
| >= 1,000 population per White and Black |
>= 3,000 population per White and Black |
>= 5,000 population per White and Black |
>= 10,000 population per White and Black |
|||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| N = 172 | N = 115 | N = 95 | N = 65 | |||||||||
| Prevention Quality Indicator Composite Rates per 1000 people | ||||||||||||
| White | Black | White | Black | White | Black | White | Black | |||||
| Mean (SD) | Mean (SD) | Diff: W-B | Mean (SD) | Mean (SD) | Diff: W-B | Mean (SD) | Mean (SD) | Diff: W-B | Mean (SD) | Mean (SD) | Diff: W-B | |
| Overall (PQI90) | 14.80 (5.12) | 15.53 (6.39) | −0.73 | 14.96 (4.97) | 16.94 (5.73) | −1.98** | 14.76 (4.49) | 16.97 (5.03) | −2.21** | 14.40 (4.85) | 17.00(4.85) | −2.60** |
| Chronic (PQI92) | 6.95 (2.74) | 10.38(4.42) | −3.42*** | 7.14 (2.66) | 11.47 (3.88) | −4.33*** | 7.10 (2.48) | 11.53 (3.46) | −4.43*** | 6.99 (2.30) | 11.68 (3.40) | −4.69*** |
| Acute (PQI91) | 7.84 (2.60) | 5.15 (2.20) | 2.69*** | 7.82 (2.49) | 5.47 (2.06) | 2.35*** | 7.66 (2.17) | 5.44(1.81) | 2.22*** | 7.42 (2.00) | 5.33 (1.57) | 2.09*** |
| Population Characteristics measured as the percent of population over 18 years in the county | ||||||||||||
| White | Black | White | Black | White | Black | White | Black | |||||
| Mean (SD) | Mean (SD) | Diff: W-B | Mean (SD) | Mean (SD) | Diff: W-B | Mean (SD) | Mean (SD) | Diff: W-B | Mean (SD) | Mean (SD) | Diff: W-B | |
| Male | 49.38 (2.46) | 55.76 (11.98) | −6.38*** | 48.91 (1.98) | 51.37 (7.77) | −2.46** | 48.53 (1.49) | 50.00 (5.69) | −1.47* | 48.36 (1.10) | 48.08 (2.99) | 0.27 |
| Female | 50.62 (2.46) | 44.24 (11.98) | 6.38*** | 51.09 (1.98) | 48.63 (7.77) | 2.46** | 51.47 (1.49) | 50.00 (5.69) | 1.47* | 51.64 (1.10) | 51.92 (2.99) | −0.27 |
| 18–39 | 38.35 (6.69) | 38.79 (6.76) | −0.44 | 38.53 (7.06) | 38.71 (7.07) | −0.17 | 38.21 (7.12) | 38.30 (7.08) | −0.09 | 39.35 (6.22) | 39.34 (6.21) | 0.01 |
| 40–64 | 43.07 (3.33) | 43.00 (3.38) | 0.07 | 42.65 (3.19) | 42.61 (3.23) | 0.04 | 42.62 (2.87) | 42.60 (2.89) | 0.02 | 42.53 (2.62) | 42.52 (2.62) | 0.01 |
| 65–74 | 9.85 (3.20) | 9.74 (3.20) | 0.11 | 9.89 (3.45) | 9.84 (3.43) | 0.05 | 9.98 (3.68) | 9.95 (3.65) | 0.03 | 9.37 (2.77) | 9.37 (2.77) | 0.00 |
| 75 plus | 8.73 (2.90) | 8.47 (2.97) | 0.26 | 8.93 (3.15) | 8.84 (3.17) | 0.09 | 9.18 (3.34) | 9.14 (3.35) | 0.05 | 8.75 (2.89) | 8.76 (2.89) | −0.01 |
| Total Population | 191,987 (268,641) | 35,941 (87,148) | 156,046*** | 257,780 (306,508) | 52,854 (102,573) | 204,926*** | 299,199 (320,756) | 63,179 (110,183) | 236,020*** | 388,002 (352,016) | 88,979 (125,256) | 299,023*** |
| Marker Condition Rates per 1000 people | ||||||||||||
| White | Black | White | Black | White | Black | White | Black | |||||
| Mean (SD) | Mean (SD) | Diff: W-B | Mean (SD) | Mean (SD) | Diff: W-B | Mean (SD) | Mean (SD) | Diff: W-B | Mean (SD) | Mean (SD) | Diff: W-B | |
| Acute myocardial infarction with length of stay >5 days or disposition of death | 0.87 (0.42) | 0.50 (0.31) | 0.38*** | 0.94 (0.43) | 0.57 (0.29) | 0.38*** | 0.97 (0.43) | 0.59 (0.28) | 0.38*** | 1.00 (0.44) | 0.57 (0.23) | 0.43*** |
| Appendicitis with appendectomy | 0.94 (0.25) | 0.50 (0.22) | 0.44*** | 0.95 (0.25) | 0.50 (0.15) | 0.45*** | 0.96 (0.24) | 0.50 (0.15) | 0.46*** | 0.98 (0.22) | 0.51 (0.12) | 0.46*** |
| Gastro-intestinal obstruction | 1.44 (0.41) | 1.10 (0.40) | 0.34*** | 1.47 (0.40) | 1.13 (0.35) | 0.34*** | 1.47 (0.37) | 1.14 (0.31) | 0.33*** | 1.44 (0.36) | 1.13 (0.29) | 0.31*** |
| Hip/femur fracture (ages 45 plus) | 3.23 (1.05) | 0.60 (0.34) | 2.63*** | 3.40 (1.06) | 0.66 (0.30) | 2.73*** | 3.45 (0.99) | 0.67 (0.27) | 2.78*** | 3.54 (0.99) | 0.67 (0.26) | 2.88*** |
p<.05;
p<.01;
p<.001
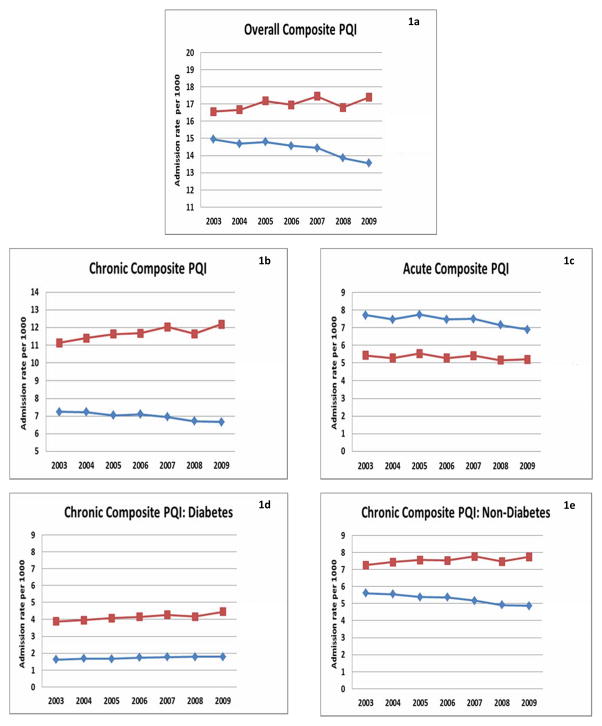
Figure 1 presents the unadjusted PQI rates over time for the sample with the most stable rates, with African American populations of at least 10,000. Figure 1a shows that the overall composite PQI rate has been declining for Whites, from about 15 admissions per 1000 population in 2003 to about 13.5 by 2009, a 10% improvement. During the same period, the rate has been increasing for African Americans from 16.6 per 1000 to 17.4, a 5% worsening. As a result, the gap, which in 2003 was about 1.6 admissions per 1000, has more than doubled to about 3.8 admissions per 1000 by 2009. Figures 1b and 1c indicate that this divergent trend can be attributed to both the chronic PQIs and the acute PQIs. Whites have experienced an improvement in the chronic PQIs while African Americans experienced a worsening. Thus by 2009 the gap in chronic PQIs was larger than it was in the 2003 by about 1.6 admissions per 1000. The acute PQIs were lower for African Americans throughout the period but showed only minimal improvement, compared with a larger improvement for Whites. Hence by 2009, Whites closed the gap, with African American having lower acute PQIs rates by about 1 admission per 1000.
Figure 1.
Unadjusted PQI Admission Rates 2003–2009
Figures 1d and 1e further divide the chronic PQIs into those that are diabetes related and those that are not: asthma, hypertension, congestive heart failure, and angina without a cardiac procedure. For the diabetes related PQIs the gap has increased only slightly, by 0.4 admissions per 1000 over the period. Most of the increase in the gap is due to the other chronic conditions, for which Whites have experienced an improvement and African Americans have experienced a slight worsening, with the gap increasing by 1.2 admissions per 1000 population.
Table 3 summarizes the results of the regression models for the 4 samples and the two races. These results, unlike the figures, are adjusted for characteristics of the local population and the health care system. As a reference point, the top line for each sample reports the PQI admission rate in 2003. The overall PQI rates ranged from 14.94 to 15.76 for Whites and from 15.34 to 17.03 for African Americans. While the rates for Whites were lower in all samples the differences reached significance (0.1 level or less) only for counties with 5000 African Americans or more. The rate of chronic PQIs admissions for Whites ranged from 7.24 to 7.64, and was also lower than the African Americans’ rate, which ranged from 10.11–11.28. This difference was highly significant (p<0.001) for all samples. The opposite was true for the acute PQIs. The rate for Whites, ranging from 7.71 to 8.13, exceeded the rate for African Americans, which ranged from 5.43 to 5.75. These differences were also highly significant (p<0.001) for all samples.
Table 3.
Coefficients for Time trend in Fixed-Effect Models Predicting the Prevention Quality Indicators Per 1000 People (2003–2009)
| Overall Composite Rate (PQI 90) | Chronic Composite Rate (PQI 92) | Acute Composite Rate (PQI 91) | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| White | Black | Diff: W-B | White | Black | Diff: W-B | White | Black | Diff: W-B | ||
| Counties with >=1,000 population per White and Black races # observations = 1204 # counties = 172 |
Baseline Rate (2003) Mean (SE) | 15.57 (6.05) | 15.34 (7.33) | 0.23 | 7.39 (3.28) | 10.11 (5.02) | −2.73**** | 8.18 (3.13) | 5.23 (2.83) | 2.95**** |
| Time Trend Mean (SE) | −0.351**** (0.093) | 0.046 (0.128) | −0.397*** | −0.175**** (0.052) | 0.092 (0.101) | −0.267*** | −0.177**** (0.053) | −0.046 (0.046) | −0.131** | |
| R2 | 0.933 | 0.857 | 0.925 | 0.826 | 0.899 | 0.763 | ||||
| Counties with >=3,000 population per White and Black races #observations = 805 # counties = 115 |
Baseline Rate (2003) Mean (SE) | 15.76 (5.58) | 17.03 (6.62) | −1.26 | 7.64 (3.09) | 11.28 (4.35) | −3.65**** | 8.13 (2.77) | 5.75 (2.62) | 2.38**** |
| Time Trend Mean (SE) | −0.320*** (0.105) | 0.028 (0.142) | −0.348** | −0.176*** (0.063) | 0.094 (0.107) | −0.270*** | −0.144*** (0.054) | −0.065 (0.051) | −0.079 | |
| R2 | 0.935 | 0.870 | 0.925 | 0.849 | 0.909 | 0.826 | ||||
| Counties with >=5,000 population per White and Black races # observations = 665 # counties = 95 |
Baseline Rate (2003) Mean (SE) | 15.46 (5.08) | 16.76 (5.61) | −1.30* | 7.49 (2.89) | 11.21 (3.77) | −3.72**** | 7.97 (2.46) | 5.56 (2.16) | 2.41**** |
| Time Trend Mean (SE) | −0.202** (0.079) | 0.221* (0.131) | −0.423*** | −0.095** (0.047) | 0.268*** (0.098) | −0.363**** | −0.107** (0.044) | −0.047 (0.046) | −0.060 | |
| R2 | 0.956 | 0.892 | 0.954 | 0.874 | 0.931 | 0.843 | ||||
| Counties with >=10,000 population per White and Black races # observations = 455 # counties = 65 |
Baseline Rate (2003) Mean (SE) | 14.94 (4.48) | 16.56 (4.90) | −1.62* | 7.24 (2.50) | 11.14 (3.26) | −3.90**** | 7.71 (2.17) | 5.43 (1.82) | 2.28**** |
| Time Trend Mean (SE) | −0.177* (0.097) | 0.351* (0.183) | −0.528** | −0.083* (0.048) | 0.375*** (0.133) | −0.458*** | −0.094 (0.061) | −0.024 (0.062) | −0.070 | |
| R2 | 0.961 | 0.920 | 0.964 | 0.917 | 0.936 | 0.866 | ||||
p<.10;
p<.05;
p<.01;
p<.001
The second line for each sample in Table 3 reports the trend (the coefficient of the time variable) from the regressions for Whites and for African Americans. It also reports the result of the Wald test comparing the two, testing the hypothesis that the trend for the two races is the same.
Table 3 does not report the other variables, but we note that in general several of the gender and age variables, several of the county fixed effects, and the marker condition variables were highly significant and in the expected direction. At least one of the Medicare and Medicaid county-level enrollment rates and median county income were statistically significant predictors of ACS admissions at the 0.1 level in 12 of the 24 models we estimated. The R2 for the equations ranged from 0.76 to 0.96.
The overall PQI for Whites exhibited a decreasing trend in all samples (P<0.1 or better). For African-Americans, the coefficient for time trend was positive in all samples, but only significant at the 0.1 level in the 2 smallest samples which exclude most rural counties. The difference between the trend for Whites and African Americans was statistically significant for all samples.
This result is attributable to the chronic PQI rates and not the acute PQI. The chronic PQI findings mimic the results for the overall PQIs, with a declining rate for Whites and a flat or increasing rate for African Americans, resulting in a highly significant difference in the trends over the period. On the other hand, the rates for acute PQIs seem to be declining for both groups, but are only significant for Whites, and the difference in time trend between the two races is significant only in the largest sample.
DISCUSSION
This study was designed to examine trends in PQI/ACS admission rates for Whites and African Americans during the 2000 decade, when addressing health care inequalities was high on the policy agenda. Our findings suggest that at least in the context of primary care and for the 6 states included in our study, this objective has not been achieved. While rates of PQI admissions have been declining for Whites, they have been stagnant or increasing for African Americans. Moy et al.19 have come to similar conclusions in a study of 36 states, suggesting that that this is a wide-spread phenomenon. Our study offers the added insights that these observed trends in disparities cannot be attributed to co-existing economic or insurance enrollment trends during the period, or to time-invariant community and health system characteristics, such as availability of primary care physicians and local practice styles.
What might explain these diverging trends? We note that most of the divergence between the trends for Whites and African Americans can be attributed to the chronic PQIs. While the descriptive statistics, presented in figures 1a–1e, suggest that African Americans have been losing grounds with respect to acute PQIs as well, the multivariable analysis, in which we controlled for local demographics, economics, and health system characteristics (Table 3) does not bear that conclusion: The differences in trends between Whites and African Americans were not statistically significant for the acute PQIs, except for the largest sample which includes the smallest and most rural counties.
The concentration of ACS admissions in chronic conditions has already been observed by Davis et al.17 during the 1990s. Its persistence over time suggests that the primary care system is less well attuned to dealing with the care needs of African Americans with chronic diseases compared to their acute care needs. The chronic PQIs are indicative of conditions that require constant monitoring and medication management, often involving a team of clinicians (e.g. primary care physicians and specialists, nutritionists) and continuity of care. The acute PQIs, on the other hand, measure discreet care episodes typically treated with a time limiting intervention such as one course of antibiotics. It seems likely that it is easier for both patients and their providers to address acute conditions, then to maintain the ongoing interaction required for chronic care. This suggests that more emphasis should be placed on improving care for minorities with chronic conditions, and on exploring barriers to ongoing chronic care, which may include not only financial burdens but also the time-cost involved in obtaining care.
In 2010, the U.S. health care system underwent a major reform with the enactment of the Patient Protection and Affordable Care Act (ACA).30 The act has two important features that might impact the care that vulnerable populations, including racial minorities, have access to. The first, and most obvious one, is the provision of access to insurance to all, either through private insurance regulated or subsidized in the Public Market Places, or through Medicaid expansion. Studies have shown that private insurance, specifically private managed-care, lowers ACS admissions.7 The impact of expanded Medicaid may not, however, be as predictable, as findings about quality and access to primary care are mixed,31 suggesting that addressing financial barriers is not sufficient to ensure high quality care.32 Indeed, Massachusetts, after its statewide health reform in 2006, did not experience an improvement in ACS admissions for racial and ethnic minorities compared to the pre-reform period.33 Thus, it is unclear whether the improvement in access to insurance coverage offered by the ACA, by itself, will impact primary care and ACS admissions.
Another feature of the ACA that may have more of an impact on ACS admissions is the major expansion of the Federally Qualified Health Centers (FQHCs) mandated under ACA.34 Recent studies found that FQHCs seem to have different practice styles for both Medicare35 and Medicaid36 beneficiaries, when compared to similar patients treated in physician offices. The FQHCs emphasize more primary care and less specialists and hospital care. While these studies did not examine ACS admissions specifically, they suggest that the emphasis on primary care might help prevent unnecessary hospitalizations. As the FQHCs expand and serve more patients in the coming years, their potential impact on hospital use and disparities should be assessed.
This study also raises two important data related issues. The first relates to the quality of the race information in the SID, and particularly the designation of Hispanics. We attempted to include in our analyses data for Hispanics as well. However, the rates calculated for Hispanics were substantially below the rates for both Whites and African Americans, suggesting that the Hispanic designation in the SID data is not sufficiently accurate to warrant their inclusion in the study. We, therefore, chose not to present data for Hispanics. This implies not only a limitation for this study but also for other studies relying on this important data resource and any policy initiatives that might be indicated by such studies.
The second data issue relates to the acute PQIs. The ACS admission rates in 2003, our baseline year, for the acute PQIs, which include dehydration, bacterial pneumonia, and urinary tract infection, were significantly lower for African Americans. This suggests that either the acute PQIs do not actually capture the quality of primary care, or that African Americans received better primary acute care. Separating these two possibilities is beyond the scope of this study. Further research is required to determine if the definition of the acute PQIs should be refined.
Addressing these data limitations is important. The DHHS plan, adopted in 2011,37 calls for continuous assessment of the impact of all of the Department’s policies and programs on racial and ethnic health disparities, and requires DHHS to promote integrated, evidence-based, best-practices to reduce disparities. Availability of reliable and valid data is a prerequisite to achieving these goals. Thus, AHRQ as the steward of these measures, with its state partners, should work to improve data quality.
Another possible limitation of this study might arise if there is a correlation between the quality of race data and quality of ambulatory care in a county. This may introduce a bias. We examined this issue by comparing the counties that would have to be excluded if we were to exclude all counties in which any hospital was excluded due to poor race data. We found that the sample was very similar to our largest sample of 172 counties. We, therefore, concluded that this limitation is not likely to introduce a bias.
In summary, this paper finds that during the 2000 decade, disparities in quality of ambulatory care in 6 states have not only not decreased, but have actually increased, and that the increase is primarily due to chronic care. Hence, policies addressing these disparities should focus primarily on primary care targeting chronic care. Furthermore, policies addressing data quality for race and ethnicity information on hospital discharge data should also be considered, to enable informed policy evaluation and planning.
Acknowledgments
Funding: NIH/NIMHD grant # R01 MD007662
Footnotes
Disclosure/Disclaimer: The views expressed in this article are those of the authors and do not necessarily reflect the official policies of the Department of Health and Human Services, the National Institutes of Health, nor the Agency of Healthcare Research and Quality, nor does mention of the department or agency imply endorsement by the U.S. government.
Contributor Information
Dana B. Mukamel, Department of Medicine, Health Policy Research Institute, University of California, Irvine, 100 Theory, Suite 110 Irvine, CA 92697-5800; Telephone: 949-824-8873, Fax: 949-824-3388.
Heather Ladd, Email: hladd@uci.edu, Health Policy Research Institute, University of California, Irvine, 100 Theory, Suite 110 Irvine, CA 92697-5800; Telephone: 949-824-8873, Fax: 949-824-3388.
Yue Li, Email: yue_li@urmc.rochester.edu, Department of Public Health Sciences, University of Rochester School of Medicine, 265 Crittenden Blvd., CU 420644, Rochester, New York 14642; Teleehone: (585) 275-3276, Fax: (585) 461-4532.
Helena Temkin-Greener, Email: Helena_Temkin-Greener@urmc.rochester.edu, Department of Public Health Sciences, University of Rochester School of Medicine, 265 Crittenden Blvd., CU 420644, Rochester, New York 14642; Telephone: 585-275-8713, Fax: (585) 461-4532.
Quyen Ngo-Metzger, Email: Quyen.Ngo-Metzger@ahrq.hhs.gov, Agency for Healthcare Research and Quality, 540 Gaither Road, Rockville, MD; Telephone: (301) 427-1571.
References
- 1.Smedley BD, Stith AY, Nelson AR. Committee on Understanding and Eliminating Racial and Ethnic Disparities in Health Care, Institute of Medicine. Unequal treatment: confronting racial and ethnic disparities in healthcare. Washington DC: National Academies Press; 2003. [PubMed] [Google Scholar]
- 2.U.S. Department of Health and Human Services, Agency for Healthcare Research and Quality. [Accessed June 25, 2014];National Healthcare Disparities Report. 2013 2013 http://www.ahrq.gov/research/findings/nhqrdr/nhdr13/2013nhdr.pdf. AHRQ Publication No. 14-0006 May 2014. [Google Scholar]
- 3.HealthyPeople.gov. [Accessed June 25, 2014];Healthy People 2020. http://www.healthypeople.gov/2020/default.aspx.
- 4.U.S. Department of Health and Human Services, Centers for Disease Control and Prevention, National Center for Health Statistics. [Accessed June 25, 2014];Healthy People 2010 Final Review. 2012 http://www.cdc.gov/nchs/data/hpdata2010/hp2010_final_review.pdf.
- 5.Billings J, Zeitel L, Lukomnik J, Carey TS, Blank AE, Newman L. Impact of socioeconomic status on hospital use in New York City. Health Affairs. 1993 Spring;12(1):1162–1173. doi: 10.1377/hlthaff.12.1.162. [DOI] [PubMed] [Google Scholar]
- 6.Backus L, Moron M, Bacchetti P, Baker LC, Bindman AB. Effect of managed care on preventable hospitalization rates in California. Med Care. 2002 Apr;40(4):315–324. doi: 10.1097/00005650-200204000-00007. [DOI] [PubMed] [Google Scholar]
- 7.Basu J, Friedman B, Burstin H. Primary care, HMO enrollment, and hospitalization for ambulatory care sensitive conditions: a new approach. Med Care. 2002 Dec;40(12):1260–1269. doi: 10.1097/00005650-200212000-00013. [DOI] [PubMed] [Google Scholar]
- 8.Falik M, Needleman J, Wells BL, Korb J. Ambulatory care sensitive hospitalizations and emergency visits: experiences of Medicaid patients using federally qualified health centers. Medical Care. 2001 Jun;39(6):551–561. doi: 10.1097/00005650-200106000-00004. [DOI] [PubMed] [Google Scholar]
- 9.Li Y, Glance LG, Cai X, Mukamel DB. Mental illness and hospitalization for ambulatory care sensitive medical conditions. Med Care. 2008 Dec;46(12):1249–1256. doi: 10.1097/MLR.0b013e31817e188c. [DOI] [PubMed] [Google Scholar]
- 10.Shi L, Samuels ME, Pease M, Bailey WP, Corley EH. Patient Characteristics Associated With Hospitalizations for Ambulatory Care Sensitive Conditions in South Carolina. Southern Medical Journal. 1999 Oct;92(10):989–998. doi: 10.1097/00007611-199910000-00009. [DOI] [PubMed] [Google Scholar]
- 11.O'Neil SS, Lake T, Merrill A, Wilson A, Mann DA, Bartnyska LM. Racial disparities in hospitalizations for ambulatory care-sensitive conditions. Am J Prev Med. 2010 Apr;38(4):381–388. doi: 10.1016/j.amepre.2009.12.026. [DOI] [PubMed] [Google Scholar]
- 12.Biello KB, Rawlings J, Carroll-Scott A, Browne R, Ickovics JR. Racial disparities in age at preventable hospitalization among U.S. Adults. Am J Prev Med. 2010 Jan;38(1):54–60. doi: 10.1016/j.amepre.2009.08.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Basu J, Friedman B, Burstin H. Preventable hospitalization and medicaid managed care: does race matter? J Health Care Poor Underserved. 2006 Feb;17(1):101–115. doi: 10.1353/hpu.2006.0018. [DOI] [PubMed] [Google Scholar]
- 14.Laditka JN, Laditka SB, Mastanduno MP. Hospital utilization for ambulatory care sensitive conditions: health outcome disparities associated with race and ethnicity. Soc Sci Med. 2003 Oct;57(8):1429–1441. doi: 10.1016/s0277-9536(02)00539-7. [DOI] [PubMed] [Google Scholar]
- 15.Russo CA, Andrews RM, Coffey RM. [Accessed August 13, 2013];HCUP Statistical Brief #10: Racial and Ethnic Disparities in Potentially Preventable Hospitalizations - July 2006. 2003 http://www.hcup-us.ahrq.gov/reports/statbriefs/sb10.jsp. [PubMed]
- 16.Chang CF, Mirvis DM, Waters TM. The effects of race and insurance on potentially avoidable hospitalizations in Tennessee. Med Care Res Rev. 2008 Oct;65(5):596–616. doi: 10.1177/1077558708318283. [DOI] [PubMed] [Google Scholar]
- 17.Davis SK, Liu Y, Gibbons GH. Disparities in trends of hospitalization for potentially preventable chronic conditions among African Americans during the 1990s: implications and benchmarks. Am J Public Health. 2003 Mar;93(3):447–455. doi: 10.2105/ajph.93.3.447. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Chang CF, Troyer JL. Trends in potentially avoidable hospitalizations among adults in Tennessee, 1998–2006. Tennessee medicine : journal of the Tennessee Medical Association. 2011 Nov-Dec;104(10):35–38. 45. [PubMed] [Google Scholar]
- 19.Moy E, Chang E, Barrett M. Potentially preventable hospitalizations - United States, 2001–2009. Morbidity and mortality weekly report. Surveillance summaries (Washington, DC: 2002) 2013 Nov 22;62( Suppl 3):139–143. [PubMed] [Google Scholar]
- 20.The Dartmouth Atlas of Health Care. [Accessed May 25, 2015];Understanding of the Efficiency and Effectiveness of the Health Care System. 2015 http://www.dartmouthatlas.org/
- 21.Agency for Healthcare Research and Quality. [Accessed August 22, 2013];Healthcare Cost and Utilization Project (HCUP) http://www.ahrq.gov/research/data/hcup/index.html. [PubMed]
- 22.Coffey R, Barrett M, Houchens R, et al. Methods Applying AHRQ Quality Indicators to Healthcare Cost and Utilization Project (HCUP) Data for the Eleventh (2013) National Healthcare Quality Report (NHQR) and National Healthcare Disparities Report (NHDR) [Accessed July 25, 2014];HCUP Methods Series Report #2012–03. ONLINE November 12, 2012. http://www.hcup-us.ahrq.gov/reports/methods/methods.jsp.
- 23.Agency for Healthcare Research and Quality. [Accessed August 21, 2013];Prevention Quality Indicators Overview. http://qualityindicators.ahrq.gov/modules/pqi_overview.aspx.
- 24.Howard DL, Hakeem FB, Njue C, Carey T, Jallah Y. Racially disproportionate admission rates for ambulatory care sensitive conditions in North Carolina. Public health reports (Washington, DC: 1974) 2007 May-Jun;122(3):362–372. doi: 10.1177/003335490712200310. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Basu J, Friedman B, Burstin H. Managed care and preventable hospitalization among Medicaid adults. Health Serv Res. 2004 Jun;39(3):489–510. doi: 10.1111/j.1475-6773.2004.00241.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Basu J, Mobley LR. Do HMOs reduce preventable hospitalizations for Medicare beneficiaries? Med Care Res Rev. 2007 Oct;64(5):544–567. doi: 10.1177/1077558707301955. [DOI] [PubMed] [Google Scholar]
- 27.Culler SD, Parchman ML, Przybylski M. Factors Related to Potentially Preventable Hospitalizations Among the Elderly. Medical Care. 1998 Nov;36(6):804–817. doi: 10.1097/00005650-199806000-00004. [DOI] [PubMed] [Google Scholar]
- 28.Nayar P, Nguyen AT, Apenteng B, Yu F. Preventable hospitalizations: does rurality or non-physician clinician supply matter? Journal of community health. 2012 Apr;37(2):487–494. doi: 10.1007/s10900-011-9468-1. [DOI] [PubMed] [Google Scholar]
- 29.Thorpe JM, Van Houtven CH, Sleath BL, Thorpe CT. Rural-urban differences in preventable hospitalizations among community-dwelling veterans with dementia. The Journal of rural health : official journal of the American Rural Health Association and the National Rural Health Care Association. 2010 Summer;26(2):146–155. doi: 10.1111/j.1748-0361.2010.00276.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.PUBLIC LAW 111–148. Patient Protection and Affordable Care Act. 2010.
- 31.Sisk JE, Gorman SA, Reisinger AL, Gilied SA, DuMouchel WH. Evaluation of Medical Managed Care. Journal of the American Medical Association. 1996;276(1):50–55. [PubMed] [Google Scholar]
- 32.Weech-Maldonado R, Morales LS, Elliott M, Spritzer K, Marshall G, Hays RD. Race/ethnicity, language, and patients' assessments of care in Medicaid managed care. Health Serv Res. 2003 Jun;38(3):789–808. doi: 10.1111/1475-6773.00147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.McCormick D, Hanchate AD, Lasser KE, et al. Effect of Massachusetts healthcare reform on racial and ethnic disparities in admissions to hospital for ambulatory care sensitive conditions: retrospective analysis of hospital episode statistics. Bmj. 2015;350:h1480. doi: 10.1136/bmj.h1480. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Adashi EY, Geiger HJ, Fine MD. Health care reform and primary care--the growing importance of the community health center. N Engl J Med. 2010 Jun 3;362(22):2047–2050. doi: 10.1056/NEJMp1003729. [DOI] [PubMed] [Google Scholar]
- 35.Mukamel DB, White LM, Nocon RS, et al. Comparing the Cost of Caring for Medicare Beneficiaries in Federally Funded Health Centers to Other Care Settings. Health Services Research. 2015 doi: 10.1111/1475-6773.12339. in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Nocon RS, Lee S, Sharma R, et al. Comparing Cost and Utilization Among Medicaid Enrollees Receiving Primary Care at Federally-Funded Health Centers Relative to Other Settings. AcademyHealth Annual Research Meeting; June 9, 2014; San Diego, CA. [Google Scholar]
- 37.U.S. Department of Health & Human Services. [Accessed June 25, 2014];HHS Action Plan to Reduce Racial and Ethnic Health Disparities - A Nation Free of Disparities in Health and Health Care. 2011 Apr; [Google Scholar]