Abstract
Inhibition of fear generalization with new learning is an important process in treatments for anxiety disorders. Generalization of maladaptive cognitions related to traumatic experiences (overgeneralized beliefs) have been demonstrated to be associated with posttraumatic stress disorder (PTSD) in adult populations, whereas more balanced, accommodated beliefs are associated with symptom improvement. It is not yet clear whether: 1) overgeneralization and accommodation are associated with PTSD treatment outcome in youth, or 2) whether accommodated beliefs can interact with or inhibit cognitive overgeneralization, as has been demonstrated in research on behavior-based fear generalization. The current study examined the relationships between overgeneralized and accommodated beliefs, child age, and symptom reduction in a sample of 81 youth (age 7-17 years), who received Trauma-Focused Cognitive Behavioral Therapy. Overgeneralized and accommodated beliefs expressed during the exposure phase of treatment were coded in audio-recorded therapy sessions. Overgeneralization predicted (a) higher internalizing symptom scores at post-treatment, particularly for younger children, and less improvement over treatment, and (b) higher externalizing scores at 1 year follow-up and steeper symptom increases over this period. In contrast, accommodation was associated with (a) lower post-treatment internalizing symptoms and greater improvement over treatment, and (b) lower externalizing scores at 1 year follow-up, particularly for younger children. High levels of accommodation moderated the relationship between overgeneralization and worse symptom outcomes, except when predicting the slope of internalizing scores over treatment, and age did not moderate these effects. There were no significant predictors of child-reported PTSD-specific symptoms, although PTSD symptoms did decrease significantly over the course of treatment and maintain one year after treatment.
Keywords: Overgeneralization, Posttraumatic Stress Disorder, Cognitive Processing, Trauma-Focused Cognitive Behavioral Therapy, Children and Adolescent
Research on behavioral fear generalization has historically focused on learned fear associations that spread across stimuli sharing perceptual (e.g., shape, color, sound) and contextual similarities. Fear learning and generalization in humans extends to higher-order thought processes, such as semantic, symbolic, and conceptual associations, which can also contribute to overgeneralization (e.g., Dunsmoor, Martin, & LaBar, 2012; Hermans & Baeyens, 2013).
Cognitive theories of PTSD share similarities with these more conceptual types of fear generalization, particularly given their emphasis on processing or “making meaning” of the traumatic experience and associated stimuli (e.g., Ehlers & Clark, 2000; Park, 2010; Resick, Monson, & Chard, 2014). Cognitive theories have long emphasized the role of exaggerated, global beliefs in PTSD, whereby conceptual associations from the traumatic experience (e.g., trusted individual perpetrates an assault) spread across people, places, and situations (e.g., “you cannot trust anyone but yourself”). This phenomenon is similar to the concept of ‘overgeneralization’ in depression research, which involves the perception of broad, abstract, and global patterns (e.g., “I'm a failure”) rather than discrimination of specific and isolated events (e.g., a small mistake at work in the context of overall good performance;Watkins, Baeyens, & Read, 2009). These cognitive theories also highlight the importance of balanced, “accommodated” beliefs as alternatives to overgeneralized thinking and as necessary for recovery and relapse prevention (e.g., Resick et al., 2014). Accomodated beliefs include concrete, factual information that can enhance discrimination between stimuli and increase specificity of trauma-related beliefs.
Cognitive overgeneralization processes might have implications for understanding fear generalization in humans and provide a useful framework for applied examinations of fear generalization in anxiety disorders. Such translational research in the context of treatment has been limited, especially with child populations. The present study examined the associations between cognitive overgeneralization, accommodation, and symptom change in a sample of youth engaged in Trauma-Focused Cognitive Behavioral Therapy (Cohen, Mannarino, & Deblinger, 2006) for PTSD.
Overgeneralization in Posttraumatic Stress Disorder
Cognitive theorists hypothesize that PTSD symptoms develop when individuals perceive their traumatic experiences to have broad implications about themselves, others, and the world, and there is little discrimination between specific traumatic experience(s), memories about the trauma, and non-threatening or unrelated people, places, objects, situations, and activities (e.g., Ehlers & Clark, 2000; Moore & Zoellner, 2007; Park, 2010; Resick et al., 2014). Cognitive overgeneralization also includes overly global memories about traumatic events that are poorly elaborated, have little context specificity, and are organized around abstract, generalized themes (e.g., danger, helplessness, trust; Ehlers & Clark, 2000; Moore & Zoellner, 2007).
Thus, like fear generalization, overgeneralization of beliefs involves too little discrimination and specificity, and vague and abstract themes can easily spread across stimuli, contexts, and time frames. For instance, a sexual assault survivor who was physically restrained and threatened with a knife reports feeling terrified and helpless. Her fear might generalize to people who look like the assailant, people of the same gender, knife-related stimuli, and to movies with rape-related themes. The belief that she is helpless could similarly spread into overly general and abstract themes with thoughts such as, “I am utterly powerless” and “The world is dangerous, so I must never let my guard down.” Both cognitive and behavioral treatments attempt to reduce overgeneralization by increasing context specificity of trauma memories to improve discrimination, increasing attention and awareness toward information that is inconsistent with maladaptive beliefs, and generating more realistic beliefs about self, others, and the world (e.g., Ehlers & Clark, 2000; Resick et al., 2014; Zalta et al., 2013).
The role of cognitive overgeneralization has received consistent support in the psychopathology and treatment literature on PTSD. In a review of research on overgeneralized autobiographical memories, Moore and Zoellner (2007) identified numerous studies showing that trauma-related overgeneralization is more strongly associated with PTSD symptoms than exposure to the trauma alone and that overgeneralization can differentiate those who develop PTSD from those who are more resilient (e.g., Ali, Dunmore, Clark, & Ehlers, 2002; Moore & Zoellner, 2007). In addition, such global negative beliefs mediate the relationships between traumatic experiences and PTSD symptoms (Elwood, Mott, Williams, Lohr, & Schroeder, 2009) and low social support (an established risk factor) and PTSD symptoms (Belsher, Ruzek, Bongar, & Cordova, 2012). Another set of studies reported that negative appraisals of traumatic experiences (Ehring, Ehlers, & Glucksman, 2008) and negative beliefs about the self (Engelhard, Huijding, van den Hout, & de Jong, 2007) predict PTSD symptoms 6 months and 15 months after trauma exposure, but they also highlight the importance of pre-trauma levels of neuroticism as a partial mediator of the association between negative self-beliefs and PTSD.
Less is known about overgeneralization in child and adolescent PTSD. Similar to findings on adult fear generalization, anxious youth exhibit impaired extinction learning and response inhibition to safety cues (e.g., Waters, Henry, & Neumann, 2009), suggesting that overgeneralization might have relevance to PTSD in youth. In a sample of war-exposed Palestinian children, Palosaari and colleagues (Palosaari, Punamäki, Diab, & Qouta, 2013) reported that changes in overgeneralization from 3 to 5 months after trauma exposure predicted subsequent changes in PTSD symptoms 5 to 11 months later, whereas changes in PTSD symptoms did not predict changes in cognitions. Overgeneral negative appraisals (child PTCI) have also been shown to predict PTSD symptoms one month (Salmon, Sinclair, & Bryant, 2007) and six months post-trauma in a non-treatment seeking sample (ages 7-13; Bryant, Salmon, Sinclair, & Davidson, 2007). Similar results have been reported in adolescent populations (ages 10-16; e.g., Meiser-Stedman, Dalgleish, Glucksman, Yule, & Smith, 2009). Together, these findings suggest that overgeneralization processes contribute to the development and maintenance of PTSD symptoms in adults and children, although the potential association between developmental level and cognitive overgeneralization in children remains unknown (e.g., Salmon & Bryant, 2002).
Findings from treatment studies for PTSD provide further support regarding the role of cognitive overgeneralization in the maintenance of and recovery from PTSD. Trauma-related overgeneralization is directly targeted in Cognitive Processing Therapy (CPT; Resick et al., 2014). At the beginning and end of treatment, individuals receiving CPT write narratives about their traumatic experience(s), including the cause and the overall impact on their lives. Sobel, Resick, and Rabalais (2009) coded these essays for ‘overaccommodated’ beliefs (defined as exaggerated, global, overgeneralized beliefs about self, others, and the world) and ‘accommodated’ beliefs (defined as adaptive, balanced beliefs about self, others, and the world). Participants showed significant pre- to post-treatment decreases in overaccommodated beliefs and increases in accommodated beliefs, which were both associated with concurrent decreases in PTSD symptoms. Overaccommodated beliefs have also been shown to be correlated with more PTSD symptoms at pre-treatment, post-treatment, and one year follow-up assessments (Owens, Pike, & Chard, 2001). Although these studies do not demonstrate that changes in overaccommodation precede symptom reduction, they do highlight that broad, overgeneralized beliefs can change in treatment and that these changes are associated with improvements in PTSD symptoms.
Two studies shed more light on the temporal precedence of overgeneralized beliefs in the therapeutic change process. Kleim et al. (2013) reported that session-by-session decreases in overgeneralized beliefs predicted subsequent decreases in PTSD symptoms during Cognitive Therapy, whereas change in PTSD symptoms did not predict subsequent change in beliefs. This same pattern of findings on cognitive overgeneralization has been reported in Prolonged Exposure (PE), a behavior-based exposure treatment for PTSD (Zalta et al., 2013). It is important to note that these two studies measured overgeneralized beliefs using the Post-Traumatic Cognitions Inventory (PTCI; Foa, Ehlers, Clark, Tolin, & Orsillo,1999), a measure that assesses overgeneralized beliefs but also includes five items about self-blame for the specific traumatic event; thus the unique role of overgeneralization in the change process is not clear. In addition, there have been no studies that have examined changes in overgeneralization as a predictor of outcomes in treatments for PTSD in youth.
Overgeneralized Beliefs and New, More Adaptive Beliefs
Traditionally, the primary mechanism of recovery from PTSD was hypothesized to be the challenging of maladaptive, overgeneralized fear associations through gradual exposure to feared stimuli and the introduction of corrective information (e.g., Foa & Kozak, 1986). More recently, behavioral research on extinction learning has added that extinction occurs when new learning inhibits the previous anxiety-based learning, which remains intact (e.g., Bouton, 2000; Craske, Liao, Brown, & Vervliet, 2012; Foa, Huppert, & Cahill, 2006). It is also possible to increase the repertoire of available responses to feared stimuli such that more adaptive, alternative responses can come on-line when fear is activated, a concept called “defusion” (Masuda, Hayes, Sackett, & Twohig, 2004). Integration across cognitive and behavioral theories of PTSD treatment suggests that, as with behaviorally conditioned fear responses, overgeneralized cognitions might stay intact but be inhibited or lessened by the development of alternative, balanced beliefs. To our knowledge, there have been no direct examinations of this hypothesis in adult or child populations with PTSD. Sobel et al. (2009) did report that CPT was associated not only with decreases in overaccommodation (overgeneralization), but also with increases in accommodation (adaptive, balanced beliefs), although these authors did not examine whether the more adaptive, balanced beliefs served an inhibitory function. In addition, no studies have evaluated the long-term effects of change in overgeneralization and accommodation during treatment.
The Current Study
Trauma-Focused Cognitive Behavioral Therapy (TF-CBT; Cohen et al., 2006) provides a useful context for examining the relationships between cognitive overgeneralization, accommodation (balanced beliefs), and symptom change in youth with PTSD. TF-CBT is one of the most widely studied and efficacious treatments for childhood PTSD (e.g., Silverman et al., 2008), and it is similar to adult interventions that involve gradual exposure and processing of these memories. TF-CBT facilitates processing by having youth recount their traumatic experience(s) and explore trauma-related beliefs in session. Despite evidence regarding the efficacy of TF-CBT, relatively little is known about how this treatment facilitates change, and the roles of overgeneralization and accommodation have not been examined.
Sessions from the trauma narrative phase of treatment were coded for overgeneralization and accommodation to capture these cognitive processes as they unfold during this phase. These cognitive variables were examined as predictors of symptom-specific outcome (e.g., PTSD symptoms) and broadband measures of functioning (e.g., internalizing problems and externalizing behaviors, which have been identified as important indicators of treatment outcome in youth; Becker, Chorpita, & Daleiden, 2011) assessed at pretreatment, mid-treatment, post-treatment, 9 month follow-up, and 1 year follow-up. Overgeneralization and accommodation alone and in combination (i.e., cognitive overgeneralization*accommodation interaction) were examined as predictors of change in symptoms across the course of treatment and over the follow-up period. Age was also examined as a moderator to better understand potential developmental differences in the associations between overgeneralization, accommodation, and symptom outcomes (e.g., Salmon & Bryant, 2002). More overgeneralization was hypothesized to predict worse treatment outcomes, whereas more accommodation was expected to predict better outcomes. In addition, accommodation was expected to weaken or inhibit overgeneralization, as indicated by a significant interaction. Analyses on age were exploratory.
Method
Participants
Participants were recruited as part of a larger treatment effectiveness trial. Youth were between the ages of 7 and 17, English-speaking, and qualified for publicly-funded treatment. They also had to have a legal guardian who was English-speaking and willing to co-participate in treatment and a year-long follow-up. Youth were excluded if caregivers reported that: 1) the child had an intellectual disability or untreated psychosis or current substance abuse, 2) the child required frequent hospitalizations or a higher level of care, or 3) a sibling was already in the study. Qualified youth were administered the UCLA PTSD Reaction Index for DSM-IV-Abbreviated (UPID-A) at their residence. Those scoring 17 or more on the UPID-A or endorsing 3 of 9 PTSD symptoms based on an independently verified (e.g., through child welfare) trauma were included in the study (e.g., Steinberg, Brymer, Decker, & Pynoos, 2004 and A. Steinberg, personal communication, August 2006). One hundred and nine participants met inclusion criteria for the effectiveness trial.
Overgeneralization and accommodation during the trauma narrative phase of treatment were the main focus of the current study, and therefore only cases with at least one session in the trauma narrative phase of treatment were included in the analyses. These 81 youth did not differ significantly in terms of demographics from the 28 youth who attritted before the trauma narrative phase. Mean age of these 81 youth was 12.56 years (SD=2.83), and youth were racially diverse (52% White, 41% African-American, 4% Hispanic/Latino, and 3% Biracial), mostly female (67%), and about one-third of youth were in foster care (38%). Youth reported an average of 3.5 types of traumatic experiences (SD=1.72) in their lifetime, including sexual abuse (51%), physical abuse (58%), domestic violence (54%), traumatic loss of a loved one (51%), community violence (experienced: 26%; witnessed: 32%), car accident or other traumatic accident (25%), fire (5%), witnessing a disaster (6%), or other abuse (11%). According to the UCLA PTSD Reaction Index, 68% of the participants met full criteria for PTSD, 17% met criteria for partial PTSD (i.e., met criteria for two of the three symptom clusters: re-experiencing, avoidance or hyperarousal), and 15% showed elevated symptom severity scores but met criteria for one or fewer symptom clusters.
Measures
In an examination of 435 randomized control trials targeted at treating childhood mental health problems, Becker et al. (2011) recommend using broadband measures of youth functioning over symptom-specific measures to best capture therapeutic change over the course of treatment. In addition to broadband measures of internalizing and externalizing functioning, the current study also included a symptom-specific measure to directly examine changes in PTSD symptoms over time.
Broadband measures of functioning
The Child Behavior Checklist (CBCL) is a 113-item parent-report measure that assesses a range of child emotional and behavioral problems. Items are rated on a 3-point Likert scale (0=not true, 1= somewhat or sometimes true, 2= very true or often true). The current study focused on the Internalizing and Externalizing scales of the CBCL to provide a measure of broadband symptom change over time. Raw scores were used in all analyses, as T-scores can truncate the range of data and be less sensitive to gradual changes in symptom trajectories over the course of treatment and the follow-up (Achenbach, 1991). The CBCL is a well-established measure with good reliability and validity as a measure of mental health problems in children (Achenbach, 2001). In the current sample, reliability across treatment and follow-up was excellent for the Internalizing scale (Cronbach's α = .89 to .90) and for the Externalizing scale (Chronbach's α = .92 to .95). Response rates across all assessment periods were high, with 5 or fewer youth missing data for any of the assessment periods from baseline through 1 year follow-up.1
Symptom-specific measure of PTSD
The UCLA PTSD Reaction Index for DSM-IV (UPID; Steinberg et al., 2004) was used to assess changes in PTSD symptoms. The UPID, administered as a questionnaire or structured interview, inventories 13 types of trauma, assesses objective and subjective aspects of the most bothersome trauma, and includes questions about the frequency of re-experiencing, avoidance, and hyperarousal symptoms in children ages 7-18. Test-retest reliability is 0.84, and the UPID shows good convergent validity, sensitivity (0.93), and specificity (0.87) in diagnosing PTSD (Steinberg et al., 2004). The full version was used to measure symptom level and change at pre-treatment, mid-treatment, post-treatment, and 9 month and 1 year follow-up. An abbreviated version (only 23 items) was used for initial screening. The UPID demonstrated good reliability in this sample across treatment and follow-up (Chronbach's α = .87 to .90). Response rates across all assessment periods were high, with 4 or fewer youth missing data for any of the assessment periods from baseline through 1 year follow-up.1
Therapists
Therapists included 25 clinicians who either held a professional degree or were doctoral students in clinical psychology programs. Clinicians were either licensed or supervised by a licensed practitioner. A majority of the therapists were Caucasian women (84%), although one clinician identified as Asian, one as Latina, and two clinicians were Caucasian males.
Trauma-Focused Cognitive Behavioral Therapy (TF-CBT)
TF-CBT is an evidence-based treatment for children, adolescents, and their non-offending caregivers that is designed to address PTSD, depression, and other trauma-related behavioral difficulties. TF-CBT has been successfully applied to a wide range of childhood traumas, including sexual abuse, physical abuse, domestic violence, and traumatic loss. TF-CBT includes an emphasis on both exposure and cognitive restructuring, with a third of treatment typically devoted to gradual exposure to traumatic memories through the creation and processing of a narrative (e.g., Cohen et al., 2006). The structure of TF-CBT can be divided into three phases:
The stabilization and skills building phase focuses on therapeutic engagement and psychoeducation about the prevalence, impact, and treatment (i.e. TF-CBT) of the traumatic event(s), as well as coping skills for managing emotional distress. The therapist also works directly with the caregiver to provide education, strategies, and feedback for assisting the child by learning, modeling, and encouraging the practicing of the coping skills learned in session.
The trauma narration and processing phase of therapy focuses directly on gradual exposure to traumatic memories through the creation of a narrative. During this phase, the child creates his or her trauma narrative orally or through the use of writing/pictures. The therapist then assists the child in identifying and challenging maladaptive beliefs about the traumatic event, its meaning, and its consequences.
The consolidation and closure phase of treatment helps to consolidate and integrate learning from previous sessions through in vivo mastery activities when needed, trauma-focused parent-child conjoint sessions to share the narrative when clinically appropriate, and the development of personal safety skills to support the child's future development. Skill building in this phase often includes assertiveness training, creating and rehearsing safety plans, and personal safety skills to prevent revictimization.
Treatment adherence
Coders were trained to use a 10-item adherence checklist developed by Dr. Esther Deblinger, coauthor of the original TF-CBT treatment manual (Cohen et al., 2006). Coders were trained to criterion by Dr. Deblinger and her research team, and after training, coders achieved good to excellent interrater agreement (dichotomous ratings of present or absent) on all categories (median κ = 0.92, range κ = 0.89 to 1.00). Adherence ratings were conducted by coding one to two sessions for each participant from the skill-building phase of treatment (sessions 1-4); two to three sessions from the narrative phase (sessions 5-10); and another one to two from the final phase of treatment (sessions 11-end of treatment). Consistent with the TF-CBT protocol, 100% of the sessions sampled during the introductory phase of treatment focused on skills building content. The trauma narrative phase primarily focused on discussions and processing of the child's trauma (86% of the sessions). Enhancing safety occurred throughout treatment but was more concentrated in the final sessions (14% of sessions in Phase 1, 16% in Phase 2, and 30% in Phase 3). These adherence ratings suggest that therapists delivered the TF-CBT components in the correct sequence.
Session Coding
All therapy sessions during the trauma narrative phase of TF-CBT were coded (mean trauma narrative sessions completed = 5.1, SD = 2.1). Sessions were coded for accommodation and overgeneralization using an adaptation of the Impact Statement Coding System, which was originally developed by Sobel et al., (2009) to examine processes of change in Cognitive Processing Therapy for adult PTSD. These categories were adapted for children and for inclusion in a broader coding system of therapy change processes, the CHANGE (Hayes, Feldman, & Goldfried, 2007). Ratings were changed from dichotomous to continuous, ranging from absent to very low (0), low (1), medium (2), and high (3). Ratings of overgeneralization and accommodation considered degree of conviction and elaboration of beliefs expressed directly by youth, with higher levels required for higher ratings. Variables are not mutually exclusive and can co-occur. Detailed descriptions and examples of each category are provided in Table 1.
Table 1.
Descriptions of CHANGE Coding Categories
| Coding Category | Description | Example |
|---|---|---|
| Accommodation | The extent to which the person shows a balanced view of self, others, or the world. This includes integrating new information learned from the traumatic experience into pre-existing beliefs, reconstruing pre-existing beliefs to arrive at realistic perspectives, and discriminating between the traumatic experience and current experiences. This category also captures the degree of realistic acceptance or resolution provided by these new beliefs. |
From a trauma narrative session with an 8-year old girl (sexual abuse): “I felt like it [the sexual abuse] was my fault, but now I know it's not my fault. He did it, he started it. It feels ok, it feels like it's not my fault. I'm the good guy, he's the bad guy. I think it [negative affect] is going to get better and better.” From an 11 year old boy (recurrent physical abuse): “As I face the memory, it starts to go away. She [abuser] doesn't get the right to abuse me, it's not ok to beat a child....I just say to myself the past is over and all the bruises went away. I'm in a safe place now. I have a scar on my heart, but it's healing.” |
| Overgeneralization | Global, exaggerated beliefs of self, others, or the world related to the traumatic event. Instead of integrating information from the traumatic experience to arrive at a clear and balanced view specific to the trauma, the person broadly applies information from the traumatic event across time and life situations. |
From an 8 year old girl (sexual abuse): “Guys scare me because of what happened with my cousin [the abuser]. I get scared when guys come into the house, I get scared that it [sexual abuse] will happen again.” From an 11 year old boy (recurrent physical abuse): “My aunt [the abuser] left a scar on my heart that will never heal. I just can't take the pain anymore, my life is nothing but pain.” |
Overgeneralization captures global, exaggerated beliefs of self, others, or the world related to the traumatic experience(s) and that are broadly applied across time and life situations. This category includes the features of the overaccommodation variable from the Sobel et al, (2009) scale, but also includes a specific focus on lack of discrimination, difficulty attending to information inconsistent with beliefs, and an overly general level of abstraction.
Accommodation captures the extent to which the person shows a balanced view of self, others, or the world. This includes integrating new information learned from the traumatic experience into pre-existing beliefs, reconstruing pre-existing beliefs to arrive at realistic perspectives, and discriminating between the traumatic experience and current experiences. This category also captures the degree of realistic acceptance and resolution provided by these new beliefs.
Coders
A team of 16 coders rated accommodation and overgeneralization for all sessions from the trauma narrative phase for all youth. Two coders rated each session. Coders were trained to criterion and met as a group each week to a.) prevent rater drift and to b.) discuss and reach consensus on coding discrepancies greater than one point on the 4-point coding measure. Interclass correlation coefficients (ICC; Shrout & Fleiss, 1979) were calculated on the raw coding (before consensus) for 25% of the total sample (ICC accommodation=.71; ICC overgeneralization=.69). These estimates fall into the acceptable to good range of agreement (Shrout & Fleiss, 1979), but there was some restriction of range in the coding, which can contribute to underestimates of agreement. Finn's r (Finn, 1970) is recommended to address the common problem of restricted range, and this yielded estimates in the excellent range of agreement (accommodation=.97, overgeneralization=.99). Consistent with these estimates, the percent agreement within 1 point across all sessions was 93% for accommodation and 94% for overgeneralization. The ratings of the two coders per transcript were averaged, and these averaged ratings were used in all analyses.
Results
Data from the 81 youth who completed at least one trauma narrative session were analyzed with piecewise latent growth curve modeling using Hierarchical Linear Modeling 7 software (HLM 7; Raudenbush, Bryk, Cheong, Congdon, & du Toit, 2011). A piecewise approach allows for an examination of processes that contribute to the reduction of symptoms during treatment, as well as those that might help maintain treatment gains over the follow-up period. The relationships between predictor variables and symptom change across these two time periods may differ. Piecewise regression analyses provide a more precise examination of which predictor variables are associated with symptom change across which time period. Such information is often lost in analyses that combine time periods (Flora, 2008). In addition, these analyses allow for an examination of predictors of endpoint symptom levels at the post-treatment and follow-up assessments and also of the slope of change. Descriptive statistics and correlations for study variables are presented in Table 2.
Table 2.
Correlation matrix and descriptive statistics of study variables
| Measure | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | 13 | 14 | 15 | 16 | 17 | 18 |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1. Internalizing Pre | ||||||||||||||||||
| 2. Internalizing 3 months | .536*** | |||||||||||||||||
| 3. Internalizing 6 months | .566*** | .700*** | ||||||||||||||||
| 4. Internalizing 9 months | .459*** | .503*** | .825*** | |||||||||||||||
| 5. Internalizing 12 months | .550*** | .507*** | .785*** | .839*** | ||||||||||||||
| 6. Externalizing Pre | .637*** | .370*** | .360*** | .343* | .376** | |||||||||||||
| 7. Externalizing 3 months | .319** | .611*** | .504*** | .540*** | .470*** | .694*** | ||||||||||||
| 8. Externalizing 6 months | .277* | .450*** | .607*** | .579*** | .495*** | .539*** | .820*** | |||||||||||
| 9. Externalizing 9 months | .345* | .415** | .499*** | .659*** | .614*** | .560*** | .706*** | .642*** | ||||||||||
| 10. Externalizing 12 months | .347* | .368** | .548*** | .667*** | .726*** | .495*** | .600*** | .644*** | .795*** | |||||||||
| 11. PTSD Pre | .250* | .099 | −.019 | −.051 | −.126 | .114 | −.037 | −.097 | −.002 | −.146 | ||||||||
| 12. PTSD 3 months | .053 | .064 | .075 | −.075 | −.030 | −.020 | .003 | −.007 | −.073 | −.180 | .325** | |||||||
| 13. PTSD 6 months | −.013 | −.046 | .038 | .068 | .108 | .028 | .081 | .136 | −.017 | .141 | .200+ | .662*** | ||||||
| 14. PTSD 9 months | .035 | .030 | .044 | .097 | .157 | .015 | .090 | .039 | .040 | −.002 | .115 | .552*** | .691*** | |||||
| 15. PTSD 12 months | .061 | .050 | .096 | .149 | .279* | .137 | .219 | .090 | .130 | .208 | −.008 | .534*** | .710*** | .812*** | ||||
| 16. Age | .106 | .018 | .057 | .205 | .157 | .169 | .058 | −.018 | .269+ | .255+ | .084 | .147 | .093 | −.219 | .020 | |||
| 17. Mean Accommodation | −.071 | −.250* | −.231* | −.223 | −.208 | .098 | −.079 | −.123 | .121 | −.033 | −.052 | −.122 | −.156 | .088 | .190 | −.013 | ||
| 18. Mean Overgeneralization | .115 | .098 | .132 | .137 | .120 | .086 | −.053 | −.043 | .125 | .433** | .026 | .146 | .243* | −.120 | .079 | .267* | −.008 | |
| Mean | 14.86 | 11.68 | 8.90 | 8.97 | 9.74 | 16.98 | 13.22 | 12.03 | 14.92 | 14.94 | 33.64 | 21.88 | 18.16 | 17.60 | 15.96 | 12.56 | .62 | .38 |
| SD | 9.00 | 9.35 | 7.92 | 7.77 | 8.69 | 13.17 | 11.28 | 11.12 | 14.10 | 13.87 | 13.20 | 11.91 | 11.93 | 13.10 | 13.06 | 2.83 | .50 | .48 |
| Range of Measure | 0-64 | 0-64 | 0-64 | 0-64 | 0-64 | 0-70 | 0-70 | 0-70 | 0-70 | 0-70 | 0-68 | 0-68 | 0-68 | 0-68 | 0-68 | 7-17.9 | 0-3 | 0-3 |
| Range of Scores | 0-36 | 0-42 | 0-34 | 0-31 | 0-29 | 0-49 | 0-47 | 0-44 | 0-53 | 0-49 | 7-65 | 0-50 | 0-46 | 0-47 | 0-45 | 7.2-17.3 | 0-2.25 | 0-2.5 |
Note.
p<.10
p<.05
p<.01
p<.001
Symptom Change Over Treatment and Follow-Up
Initial piecewise analyses were conducted to examine level-1 within-person symptom reduction from pre- to post- treatment (Time A: 0, 3, and 6 months) and from post-treatment through 12-month follow-up (Time B: 6, 9, and 12 months), consistent with recommendations from Flora (2008). The resulting level-1 equation includes two time pieces that represent the time periods of interest:
In this equation, OUTCOMEti is the observed value of symptoms at time t within youth i. β0i represents youth i's symptom level at pre-treatment (time=0); β1i and β2i represent the rate of linear change in symptoms over TimeA (treatment) and TimeB (follow-up) for youth i; and rti represents within-individual variance in youth i's symptoms not accounted for by pre-treatment symptoms or by linear change in symptoms. Intercepts and slopes were allowed to vary, allowing the model to estimate intercepts and rate of symptom change for each individual. In addition, these random intercepts and random slope terms were allowed to correlate by fitting a covariance between the terms. In a linear case, positive covariance indicates that participants with higher levels at baseline (intercept) have steeper rates of change (more positive). Negative covariance indicates that participants with lower levels at baseline (intercept) have steeper rates of change. Similar conclusions can be made with piecewise analyses.
There was a significant reduction in PTSD symptoms (β = −2.55, SE= .29, p<.001), internalizing (β = −.98, SE=.15 p<.001), and externalizing (β = −.76, SE=.21, p<.001) across the treatment period. Improvements were maintained over the 6-, 9-, and 12-month follow-up period for PTSD and internalizing symptoms, but there was a significant increase in externalizing symptoms (β = .65, SE=.27, p = .018) over the follow-up period.
Predictors of Symptom Change
Next, overgeneralization, accommodation, and their interaction were entered in the equation as level-2 between-person predictors of symptoms at posttreatment (endpoint) and the slope of symptom change over the treatment period. Given that externalizing symptoms increased over the follow-up period, we also examined externalizing symptoms at 1 year follow-up (endpoint) and the slope of change during this period. Because there were no statistically significant changes in PTSD symptoms and internalizing problems over the follow-up period (change was maintained), and the variance estimates of their slopes were not statistically significant, PTSD and internalizing symptoms over follow-up were not examined further. To examine possible contributions of developmental differences, age was included as a moderator 1.
The resulting level-2 equations included cognitive processes (overgeneralization, accommodation), child age, and their interactions as predictors of the slope for each time piece, controlling for baseline symptoms and are presented below. An explanation of these equations can be found in Appendix A.
Intercept (Post-Treatment Outcome):
β0i = γ00 + γ01 (BASELINE SYMPTOMSi) +γ02 (OVERGENERALIZATIONi) + γ03 (ACCOMODATIONi) +γ04 (CHILDAGEi) +γ05 (OVERGENERALIZATION *AGEi) + γ06(ACCOMODATION *AGEi)+ γ07(OVERGENERALIZATION*ACCOMODATIONi) +γ08 (OVERGENERALIZATION*ACCOMODATION*AGEi) + u0i
TimeA (Treatment) Slope:
β1i = γ10 + γ11 (BASELINE SYMPTOMSi) +γ12 (OVERGENERALIZATIONi) + γ13 (ACCOMODATIONi) +γ14 (CHILDAGEi) +γ15 (OVERGENERALIZATION *AGEi) + γ16(ACCOMODATION *AGEi) + γ17(OVERGENERALIZATION*ACCOMODATIONi) +γ18 (OVERGENERALIZATION*ACCOMODATION*AGEi) + u1i
TimeB (Follow-up) Slope:
β2i = γ20 + γ21 (BASELINE SYMPTOMSi) +γ22 (OVERGENERALIZATIONi) + γ23 (ACCOMODATIONi) +γ24 (CHILDAGEi) +γ25 (OVERGENERALIZATION *AGEi) + γ26 (ACCOMMODATION*AGEi)+γ27(OVERGENERALIZATION*ACCOMODATIONi) +γ28 (OVERGENERALIZATION*ACCOMODATION*AGEi) + u2i
Accommodation, overgeneralization, and child age were grand-centered so that the variable means across all 81 youth were set to zero and interaction terms were calculated using centered variables. This approach allows for interpretation of the significance of main effects with the interaction terms in the model (Aiken & West, 1991). Following Preacher, Curran, & Bauer's (2006) method, we dismantled significant interaction effects by examining significance of the conditional effects of the predictor variable on outcome by testing the simple slopes of participants with high levels (1 SD above the mean) and low levels (1 SD below the mean) of the moderator variable. Significance of these simple slopes was calculated using the variances and covariances of the independent variable, the moderator, and their interaction from the asymptotic covariance matrix. To dismantle interactions with age, the significance of the conditional effects of accommodation and overgeneralization on outcome were examined by testing simple slopes of youth at higher (+1 SD; 15.39 years) and lower (−1 SD; 9.73 years) ages. To dismantle the overgeneralization*accommodation interaction, significance of the conditional effects of overgeneralization on outcome was examined by testing simple slopes of youth with high (+1 SD) and low (−1 SD) levels of accommodation. Findings from the piecewise hierarchical regressions are presented in Table 3.
Table 3.
Piecewise growth curve modeling examining age, overgeneralization, accommodation, and their interactions as predictors of change over the course of treatment and 1 year follow-up
| Outcome | |||
|---|---|---|---|
| Independent Variable | γ | SE | 95% CI |
| Internalizing Symptoms | |||
| Post-Treatment Symptoms | |||
| Baseline Symptoms | .41*** | .09 | .24 – .57 |
| Overgeneralization | 5.33* | 2.03 | 1.35 – 9.32 |
| Accommodation | −5.66*** | 1.67 | −8.93 – −2.40 |
| Age | −.38 | .28 | −.92 – .17 |
| Overgeneralization × Age | −1.65* | .68 | −2.97 – −.32 |
| Accommodation × Age | 1.50* | .60 | .32 – 2.68 |
| Overgeneralization × Accommodation | −11.48* | 4.40 | −20.10 – −2.86 |
| Overgeneralization × Accommodation × Age | 1.21 | 1.48 | −1.69 – 4.11 |
| Change in Symptoms over Treatment (0, 3, 6 months) | |||
| Baseline Symptoms | −.09*** | .02 | −.12 – −.06 |
| Overgeneralization | .78* | .38 | .04 – 1.53 |
| Accommodation | −.77* | .31 | −1.37 – −.16 |
| Age | −.05 | .05 | −.15 – .06 |
| Overgeneralization × Age | −.23+ | .13 | −.48 – .02 |
| Accommodation × Age | .23* | .11 | .01 – .45 |
| Overgeneralization × Accommodation | −1.47+ | .82 | −3.08 – .14 |
| Overgeneralization × Accommodation × Age | .13 | .28 | −.41 – .67 |
| Externalizing Behaviors | |||
| 1 Year Follow-Up Symptoms | |||
| Baseline Symptoms | .64*** | .11 | .42 – .86 |
| Overgeneralization | 15.13** | 4.90 | 5.53 – 24.73 |
| Accommodation | −4.02 | 3.53 | −10.93 – 2.90 |
| Age | .04 | .62 | −1.18 – 1.26 |
| Overgeneralization × Age | .50 | 1.83 | −3.10 – 4.09 |
| Accommodation × Age | 3.46* | 1.44 | .64 – 6.28 |
| Overgeneralization × Accommodation | −33.24** | 11.18 | −55.16 – −11.33 |
| Overgeneralization × Accommodation × Age | .39 | 4.11 | −7.67 – 8.45 |
| Change in Symptoms over Treatment (0, 3, 6 months) | |||
| Baseline Symptoms | −.08*** | .01 | −.10 – −.05 |
| Overgeneralization | .11 | .51 | −.89 – 1.12 |
| Accommodation | −.68 | .42 | −1.51 – .15 |
| Age | −.07 | .07 | −.22 – .07 |
| Overgeneralization × Age | −.18 | .17 | −.52 – .15 |
| Accommodation × Age | .23 | .15 | −.06 – .52 |
| Overgeneralization × Accommodation | −.63 | 1.12 | −2.81 – 1.56 |
| Overgeneralization × Accommodation × Age | −.14 | .37 | −.87 – .59 |
| Change in Symptoms over Follow-Up (6, 9, 12 months) | |||
| Baseline Symptoms | .02 | .02 | −.01 – .06 |
| Overgeneralization | 2.46** | .77 | .94 – 3.97 |
| Accommodation | .14 | .54 | −.93 – 1.21 |
| Age | .09 | .10 | −.10 – .28 |
| Overgeneralization × Age | .28 | .29 | −.29 – .85 |
| Accommodation × Age | .32 | .23 | −.12 – .77 |
| Overgeneralization × Accommodation | −4.55* | 1.77 | −8.02 – −1.08 |
| Overgeneralization × Accommodation × Age | .12 | .66 | −1.16 – 1.41 |
| PTSD Symptoms | |||
| Post-Treatment Symptoms | |||
| Baseline Symptoms | .09 | .10 | −.11 – .29 |
| Overgeneralization | 3.16 | 3.66 | −4.01 – 10.34 |
| Accommodation | −3.55 | 3.01 | −9.44 – 2.35 |
| Age | .15 | .51 | −.85 – 1.14 |
| Overgeneralization × Age | 1.54 | 1.23 | −.87 – 3.95 |
| Accommodation × Age | .15 | 1.08 | −1.96 – 2.26 |
| Overgeneralization × Accommodation | .10 | 7.93 | −15.43 – 15.64 |
| Overgeneralization × Accommodation × Age | −3.70 | 2.66 | −8.91 – 1.50 |
| Change in Symptoms over Treatment (0, 3, 6 months) | |||
| Baseline Symptoms | −.13*** | .02 | −.17 – −.10 |
| Overgeneralization | .51 | .67 | −.79 – 1.82 |
| Accommodation | −.59 | .55 | −1.66 – .48 |
| Age | −.01 | .09 | −.19 – .18 |
| Overgeneralization × Age | .25 | .22 | −.19 – .69 |
| Accommodation × Age | .04 | .20 | −.35 – .42 |
| Overgeneralization × Accommodation | −.28 | 1.44 | −3.11 – 2.55 |
| Overgeneralization × Accommodation × Age | −.48 | .48 | −1.43 – .47 |
Note.
p<.10
p<.05
p<.01
p<.001
Broadband measures of functioning
Internalizing symptoms: Post-treatment endpoint
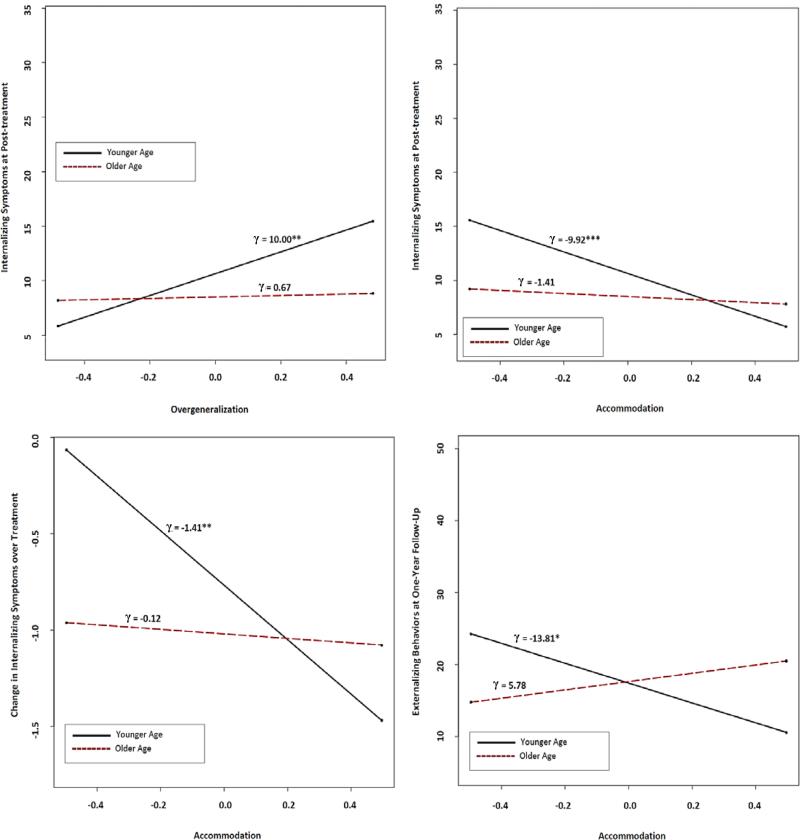
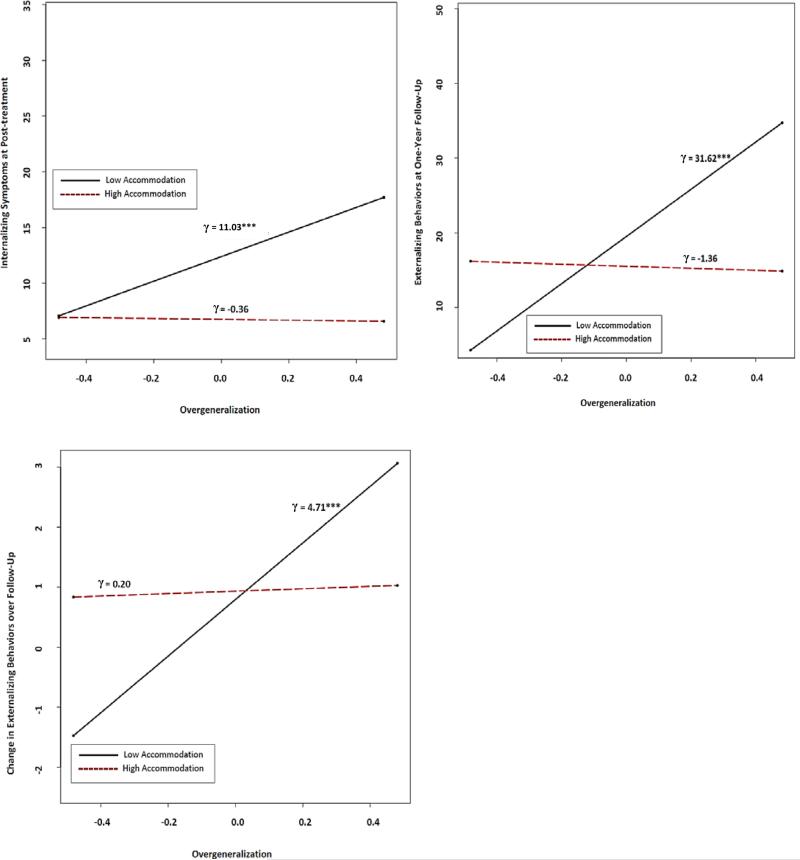
Significant main effects for overgeneralization and accommodation indicated that higher levels of accommodation and lower levels of overgeneralization during the narrative phase of treatment were associated with lower internalizing symptoms at post-treatment. These effects were qualified by significant age interactions, such that accommodation and overgeneralization were associated with post-treatment internalizing symptoms for younger (accommodation, γ = −9.92, p <.001; overgeneralization, γ = 10.00, p =.01) but not for older children (accommodation, γ = −1.41, ns; overgeneralization, γ = 0.67, ns; see Figure 1). In addition, accommodation significantly moderated overgeneralization, such that higher levels of overgeneralization were associated with higher post-treatment internalizing symptoms when accommodation was low (γ = 11.03, p <.001), but not when accommodation was high (γ = −0.36, ns). This effect was significant across all ages, as indicated by the non-significant three-way interaction (Figure 2).
Figure 1.
Simple slopes showing the conditional association between cognitive processes (e.g., accommodation or overgeneralization; x-axis) and outcome (y-axis) at younger (1 SD below mean; 9.73 years) and older ages (1 SD above mean; 15.39 years). Overgeneralization, accommodation, and age are grand-centered so that a score of zero represents the average level of each variable across all 81 youth. γ = unstandardized coefficient representing simple slopes of children at younger and older ages. ** p = .01, *** p ≤ .001.
Figure 2.
Simple slopes showing the conditional association between overgeneralization (x-axis) and outcome (y-axis) at high (1 SD above the mean) and low (1 SD below the mean) levels of accommodation Overgeneralization and accommodation are grand-centered so that a score of zero represents the average level of each variable across all 81 youth. γ = unstandardized coefficient representing the simple slope of children with high and low levels of accommodation. *** p ≤ .001.
Internalizing symptoms: Slope of change over treatment
As with the endpoint analyses, main effects of overgeneralization, accommodation, and the age*accommodation interaction were also significant predictors of change in the slope of internalizing symptoms over the course of treatment. Higher accommodation and lower overgeneralization predicted more improvement in internalizing symptoms. Younger children experienced particular benefit from accommodation (γ = −1.41, p =.01) compared to older children (γ = −0.12, ns). See Figure 1. Unlike endpoint analyses, the moderation effect of age on overgeneralization and the overgeneralization*accommodation interaction were not significant predictors of change in internalizing symptoms, although these variables approached statistical significance.
Externalizing symptoms: Post-treatment endpoint and slope of change over treatment
None of the predictors (overgeneralization, accommodation, child age, and their interactions) predicted externalizing symptoms at the end of treatment or the slope of externalizing symptoms during the course of treatment.
Externalizing symptoms: 1 year follow-up endpoint
Given the significant increase in externalizing symptoms over the follow-up period, we were particularly interested in the 1 year follow-up endpoint and conducted a second analysis to examine this question (in which B0i was recoded to represent the 1 year follow-up endpoint instead of the post-treatment endpoint. The slope of change over treatment and follow-up, Β1i & Β2i, are identical to the first analysis). To minimize redundancy, we report only the second piecewise equation (Β0i = 1 year follow-up endpoint) in Table 3.
Higher levels of overgeneralization predicted higher externalizing symptoms at the 1 year follow-up assessment, regardless of child age. There was no significant main effect for accommodation, but a significant accommodation*age interaction indicated that accommodation was associated with fewer externalizing symptoms at 1 year follow-up for younger children (γ = −13.81, p =.02), but not for older children (γ = 5.78, ns; see Figure 1). Accommodation significantly moderated the relationship between overgeneralization and externalizing symptoms, such that overgeneralization was not associated with worse externalizing symptoms when accommodation was also high (γ = −1.36, ns; low accommodation, γ = 31.62, p <.001). This moderation effect was consistent across child age, as indicated by the non-significant three-way interaction between overgeneralization, accommodation, and age (see Figure 2).
Externalizing symptoms: Slope of change over follow-up
As with the follow-up endpoint findings, overgeneralization was significantly associated with worsening (increase in the slope) of externalizing symptoms, regardless of child age. This relationship was moderated by accommodation, such that higher levels of overgeneralization were not associated with greater worsening of externalizing symptoms when accommodation was high (γ = 0.20, ns; low accommodation, γ = 4.71, p < .001). This interaction effect did not differ across age (see Figure 2). Unlike the endpoint findings, age did not moderate the association between accommodation and less worsening (increase in slope) of externalizing symptoms over the follow-up period.
Symptom-specific measure of PTSD
Overgeneralization, accommodation, and child age nor their interactions predicted post-treatment PTSD symptoms or change in symptoms over the course of treatment.
Discussion
The current study examined cognitive overgeneralization as a predictor of worse outcomes during Trauma-Focused Cognitive Behavioral Therapy in a sample of underserved youths. Similar to research with adult PTSD (e.g., Sobel et al., 2009), findings across broadband measures showed that more overgeneralization during the trauma narrative phase of treatment was a consistent predictor of worse treatment response. More overgeneralization not only predicted higher internalizing symptom scores at the post-treatment endpoint in younger children and less improvement in these symptoms over the course of treatment, but this cognitive variable also predicted higher externalizing symptoms at the 1-year endpoint and a greater return of externalizing symptoms in this same follow-up period. More balanced, accommodated beliefs were particularly beneficial for children of younger ages and predicted lower internalizing scores at post-treament and greater improvement in symptoms across treatment, as well as lower externalizing symptoms at the 1-year follow-up endpoint for younger children. Consistent with study hypotheses, overgeneralization was not associated with symptoms when accommodation was high, and this effect was consistent across all ages. These findings suggest that accommodated beliefs (e.g., alternative explanations for previously threatening stimuli) might weaken the relationship between overgeneralization and symptom change, similar to the way that new learning can inhibit the expression of behavioral fear generalization (e.g., Bouton, 2000; Craske et al., 2012). It is important to note that neither accommodation nor overgeneralization during the narrative phase was significantly correlated with any measure of symptoms at pretreatment, which suggests that these variables capture more than initial symptom severity.
Accommodation seemed to lessen the impact of overgeneralization on treatment outcomes, which raises the question of whether these two variables represent aspects of a single dimension of adaptive/maladaptive trauma-related reactions. However, overgeneralization was not significantly correlated with accommodation (r = −.01, ns), suggesting that these variables might be separate constructs. Conceptually, overgeneralization represents global, abstract thoughts that do not consider contextual or contradictory information. Accommodation represents concrete, factual beliefs that integrate contextual nuance, account for contradictory information, and facilitate discrimination across similar but different stimuli. In the context of treatment, patients can simultaneously hold abstract, overgeneralized beliefs related to PTSD and also factual, contextually-specific information (e.g., accommodation) that develops over the course of treatment and can be used to disengage from or challenge pathological overgeneralized beliefs. This notion has been discussed in therapeutic contexts (e.g., Linehan, 1993), in which patients can simultaneously hold alternative, opposing views and are encouraged to practice accommodated beliefs until these thoughts become automatic (theoretically overriding engrained overgeneralized beliefs and providing an alternative response to overergeneralization; cf., Masuda et. al, 2004; Resick et al., 2014). This is also similar to behavioral research on extinction learning, which has demonstrated that anxiety-based learning and new learning can co-exist and that extinction occurs when new learning inhibits the pathological learning, even though the latter remains intact (e.g., Bouton, 2000; Craske et al., 2012; Foa et al., 2006; Lissek, 2012).
For example, one participant in the study reported acting out in his foster home when he became upset, which he later reported was related to thoughts that he could never trust others and must always “watch his back” (related to previous physical abuse). Fortunately, more accommodated, balanced beliefs (“when you're feeling bad, you should talk to someone and not let the anger build inside you” and positive beliefs about his foster mother's love for him) were concurrently activated. The child's responses implied that these balanced beliefs seemed to contain the spread of overgeneralization, minimize the escalation of negative behaviors and emotions, and to encourage more adaptive behavioral responses, such as re-engaging rather than withdrawing from his foster family.
Age as a Moderator of Overgeneralization and Accommodation
Age moderated the associations between accommodation, overgeneralization and treatment outcomes, such that higher levels of accommodation and lower levels of overgeneralization were more strongly associated with internalizing symptom improvement in younger children than in older children. This effect was particularly pronounced for accommodation, as age also moderated the association between accommodation and externalizing at the 1 year follow-up assessment. Interestingly, accommodation moderated the association between overgeneralization and worse symptoms across youth of all ages.
Older children might be expected to benefit most from accommodation during the narrative phase because of their more developed cognitive abilities and metacognitive awareness, as Deblinger and colleagues have speculated (Deblinger, Mannarino, Cohen, Runyon, & Steer, 2011). However, it is also possible that the more concrete thinking style of younger children can facilitate greater processing of their traumatic experience and readiness for accommodation. For instance, a concrete processing style has been shown to be beneficial for counteracting overgeneralized memories and improving treatment outcomes in adults with depressive symptoms (e.g., Watkins et al., 2009), and this concreteness may have similar effects for youth with PTSD symptoms. In addition, younger children are likely to have less entrenched beliefs and thus may be more responsive and open to alternative ways of interpreting their traumatic experiences, thereby facilitating accommodation. However, these findings will need to be replicated and causal conclusions about the benefits of concrete processing cannot be made.
Implications for TF-CBT
This is the first study to our knowledge that identified a relationship between the trauma narrative and long-term changes in externalizing behavior. A previous dismantling study found greater improvement in externalizing behaviors when the exposure-based trauma narrative component was replaced with additional parenting skills training (Deblinger et al., 2011). Our findings, however, identified both overgeneralization and accommodation during the trauma narrative phase as important predictors of treatment change in internalizing symptoms at post-treatment and of long-term change in externalizing behaviors following TF-CBT. Taken together, findings from the previous dismantling literature and current study suggest both parenting skills and the trauma narration and processing phase of TF-CBT might be important for long term reductions in externalizing behavior.
Limitations and Future Directions
The pattern of findings for internalizing and externalizing symptoms was generally consistent for endpoint and slope analyses, although a few of the significant interaction effects did not hold when examining the slopes over treatment and follow-up. It is possible that overgeneralization and accommodation may be better predictors of youth endpoint outcomes than of the rate and slope of the change. Alternatively, it is possible that some youth may have demonstrated non-linear change trajectories within the treatment or follow-up periods, which might have minimized associations between the predictor variables and the linear slopes analyzed in the current study.
Contrary to study hypotheses and previous research with adult PTSD treatment, overgeneralization and accommodation were not associated with symptom change in PTSD-specific symptoms. This finding, in part, may be attributed to our sample. Children enrolled in the study were not required to meet full criteria for PTSD, and PTSD symptoms primarily depended upon youth self-report and self-disclosure. This is different from previous research, such as the Deblinger et al. (2011) dismantling study, which used a structured diagnostic interview that combined parent- and child-report to measure PTSD symptoms. In addition, parent-report may be particularly beneficial for accurate measurement of youth PTSD, especially given that high avoidance is characteristic of this disorder and may bias youth-report. Recent research has highlighted the importance of using broadband measures of functioning to assess symptom change in treatment studies for children, as symptom-specific measures, such as the UPID, may not always provide an accurate or comprehensive reflection of improvement in children (e.g., Becker et al., 2011). Utilizing parent- and youth-report on measures of both broadband functioning and symptom-specific measures can help address these limitations in future studies.
The current study used a longitudinal, within-subjects design to examine symptom change over the course of TF-CBT and did not include a control group. Although the temporal order of variables revealed some important predictors of therapeutic change (e.g., cognitive processes measured during treatment predicted subsequent symptom reduction at post-treatment and 1 year follow-up), it is possible that observed associations between overgeneralization, accommodation, and symptom reduction could also occur naturally outside the context of treatment and could be influenced by non-treatment related factors. The lack of a control condition does not allow for examination of these possibilities.
This study was unique in its use of an observational coding measure to assess overgeneralization and accommodation as these processes unfold during treatment. Previous literature relied heavily on between-session self-report measures, such as the PTCI, to measure overgeneralization. Although self-report measures can be biased by client characteristics (e.g., self-awareness and reporter honesty), self-report also draws upon the client's comprehensive knowledge of his or her own beliefs. It is possible that self-report measures may assess a different concept (awareness of beliefs) than the coding measure (verbal expression of beliefs). Future research utilizing a multi-method assessment of overgeneralization and accommodation could clarify their relationships with treatment outcomes.
The current findings represent an initial examination of cognitive overgeneralization in PTSD and accommodated beliefs as a variable that might moderate the impact of cognitive overgeneralization. Future research manipulating these processes within a randomized control trial would help increase knowledge regarding the role of these processes in treatment as potential mechanisms of change. A particularly interesting direction for future study would be to explore variables that predict individual differences in child overgeneralization, accommodation, and their associations with symptom change, such as parent-level variables, dose of trauma narrative (e.g., number of trauma narrative sessions), therapist-level variables, neuroticism (e.g., Engelhard et al., 2007), and facets of cognitive development (e.g., IQ, memory, language skills, metacognitive awareness; Salmon & Bryant, 2002).
Conclusions
Overgeneralization and accommodation during the narrative exposure phase of TF-CBT were important predictors of symptom outcome over the course of this effectiveness trial, which was delivered by clinicians in community settings to a diverse sample of underserved youth. The findings suggest that: 1) overgeneralized beliefs are associated with poorer treatment outcomes, whereas accommodated beliefs are associated with better outcomes, particularly for younger children; 2) balanced, accommodated beliefs moderate the relationship between overgeneralization and outcome; and 3) overgeneralization and accommodation are associated with longer-term changes in externalizing symptoms up to a year after starting treatment. These findings add to the growing literature that identifies overgeneralized beliefs and cognitive change (e.g. Kleim et al., 2013; Sobel et al., 2009, & Zalta et al., 2013) as therapeutically-relevant processes in the treatment of PTSD across childhood, adolescence, and adulthood.
Highlights.
□ Cognitive overgeneralization was examined in youth receiving Trauma-Focused CBT
□ Overgeneralization was associated with worse internalizing and externalizing symptoms
□ Balanced, accommodated beliefs were associated with greater symptom improvement
□ These effects were particularly beneficial for younger children
□ Accommodation moderated the relationship between overgeneralization and worse
Acknowledgments
This research was supported by grants from the Substance Abuse and Mental Health Services Administration (SAMHSA: SM57145) to the Delaware Division of Prevention and Behavioral Health Service and the National Institute of Mental Health (NIMH: R01-MH086558) to Adele M. Hayes. The authors would like to thank Patricia Resick and Kate Iverson for sharing their coding system and providing consultation throughout the coding process and Thomas McCauly, Vanniesha Bennett, Keith Brown, Alyssa Fazio, Caitlin Wilson, Ben Barnes, Garret Sacco, and Joanna Osborne for their assistance with data collection and coding.
Appendix A
Description of the level-2 piecewise hierarchical linear modeling equations which examine overgeneralization, accommodation, child age, and their interactions as predictors of post-treatment endpoint and slopes of change for treatment and follow-up, controlling for baseline symptoms.
B0i represents individual symptom levels at post-treatment (6 Months), and the coefficient γ00 estimates the average symptom level at post-treatment. The coefficients γ01, γ02, γ03, and γ04 represent variation in post-treatment symptoms as baseline symptoms, overgeneralization, accommodation, and child age increase. The terms γ05 and γ06 represent the interactions of age with overgeneralization and accommodation, γ07 represents the overgeneralization*accommodation interaction, and the term γ08 represents the three-way interaction (overgeneralization*accommodation*age) as a predictor of post-treatment symptoms.
β1i and β2i represent individual rates of linear change in symptoms over the course of each time period. The coefficients γ10 and γ20 estimate the average rate of change in symptoms over the corresponding time period (γ10: treatment; γ20: follow-up). The coefficients γ11, γ12, γ13, γ14 and γ21, γ22, γ23, γ24 represent variation in the rate of symptom change as baseline symptoms, overgeneralization, accommodation, and child age increase. The terms γ15, γ16 and γ25, γ26 represent the interactions of age with overgeneralization and accommodation, the terms γ17 and γ27 represent the overgeneralization*accommodation interaction, and the terms γ18 and γ28 represent the three way interaction (overgeneralization*accommodation*age) as a predictor of the rate of symptom change. Intercepts and slopes were allowed to vary so that intercepts and rate of symptom change for each individual could be estimated.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
CBCL: Baseline: 81; 3 month: 80; 6 month: 80; 9 month: 52 (of 56 youth); 12 month: 51 (of 56)
All HLM analyses used the full intent-to-treat sample of 81 youth and were conducted using Full Information Maximum Likelihood (FIML) to account for the missing 9- and 12-month data (e.g., Arbuckle, 1996). Although the data are not technically Missing at Random (MAR), a series of logistic regressions were conducted to examine whether youth with and without 9- and 12-month follow-up differed on the outcome variables and relevant demographics variables. Results indicated that there were no significant differences between youth with and without follow-up data on pre-treatment symptoms, post-treatment symptoms, and demographics variables. Therefore, we conducted analyses on the full sample. It is also important to note that analyses conducted with only youth who received 9- and 12-month follow-up assessments showed the same pattern of results as the full sample, including a significant increase in externalizing behaviors from post-treatment through 12-month follow-up (β = .68, SE = .28, p =.017). In addition, a main effect for overgeneralization (γ = 12.23, SE = 5.38, p = .028), overgeneralization*accommodation interaction (γ = −30.81, SE = −2.5, p = .013), and trend towards accommodation*age interaction (γ = 3.13, SE = 1.98, p = .054) emerged as predictors of externalizing behaviors at 1 year follow-up. Similarly, a main effect for overgeneralization (γ = 2.72, SE = .77, p = .001) and the overgeneralization*accommodation interaction (γ = −4.65, SE = 1.78, p =.012) again emerged as predictors of the increase in externalizing behaviors over the follow-up period.UPID: Baseline: 81; 3 month: 80; 6 month: 79; 9 month: 52 (of 56 youth); 12 month: 52 (of 56)
References
- Achenbach TM. Manual for the Child Behavior Checklist 4-18 and 1991 profile. Department of Psychiatry, University of Vermont; Burlington: 1991. [Google Scholar]
- Achenbach TM. The Child Behavior Checklist. ASEBA, University of Vermont; Burlington: 2001. [Google Scholar]
- Aiken LS, West SG. Multiple regression: Testing and interpreting interactions. Sage; Newbury Park: 1991. [Google Scholar]
- Ali T, Dunmore E, Clark D, Ehlers A. The role of negative beliefs in posttraumatic stress disorder: A comparison of assault victims and non victims. Behavioural and Cognitive Psychotherapy. 2002;30(3):249–257. doi: http://dx.doi.org/10.1017/S1352465802003016. [Google Scholar]
- Arbuckle JL. Full information estimation in the presence of incomplete data. In: Marcoulides GA, Schumacker RE, editors. Advanced structural equation modeling: Issues and techniques. Lawrence Erlbaum Associates; Mahwah, NJ: 1996. pp. 243–278. [Google Scholar]
- Becker KD, Chorpita BF, Daleiden EL. Improvement in symptoms versus functioning: How do our best treatments measure up? Administration and Policy in Mental Health and Mental Health Services Research. 2011;38(6):440–458. doi: 10.1007/s10488-010-0332-x. doi: http://dx.doi.org/10.1007/s10488-010-0332-x. [DOI] [PubMed] [Google Scholar]
- Belsher BE, Ruzek JI, Bongar B, Cordova MJ. Social constraints, posttraumatic cognitions, and posttraumatic stress disorder in treatment-seeking trauma survivors: Evidence for a social-cognitive processing model. Psychological Trauma: Theory, Research, Practice, and Policy. 2012;4(4):386–391. doi: http://dx.doi.org/10.1037/a0024362. [Google Scholar]
- Bouton ME. A learning theory perspective on lapse, relapse, and the maintenance of behavior change. Health Psychology. 2000;19(1,Suppl):57–63. doi: 10.1037/0278-6133.19.suppl1.57. doi: http://dx.doi.org/10.1037/0278-6133.19.Suppl1.57. [DOI] [PubMed] [Google Scholar]
- Bryant RA, Salmon K, Sinclair E, Davidson P. A prospective study of appraisals in childhood posttraumatic stress disorder. Behaviour Research and Therapy. 2007;45(10):2502–2507. doi: 10.1016/j.brat.2007.04.009. doi: http://dx.doi.org.udel.idm.oclc.org/10.1016/j.brat.2007.04.009. [DOI] [PubMed] [Google Scholar]
- Cohen JA, Mannarino AP, Deblinger E. Treating trauma and traumatic grief in children and adolescents. Guilford Press, New York, NY.; New York, NY, US: 2006. [Google Scholar]
- Craske MG, Liao B, Brown L, Vervliet B. Role of inhibition in exposure therapy. Journal of Experimental Psychopathology. 2012;3(3):322–345. doi: http://dx.doi.org/10.5127/jep.026511. [Google Scholar]
- Deblinger E, Mannarino AP, Cohen JA, Runyon MK, Steer RA. Trauma-focused cognitive behavioral therapy for children: Impact of the trauma narrative and treatment length. Depression and Anxiety. 2011;28(1):67–75. doi: 10.1002/da.20744. doi: http://dx.doi.org/10.1002/da.20744. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dunsmoor JE, Martin A, LaBar KS. Role of conceptual knowledge in learning and retention of conditioned fear. Biological Psychology. 2012;89(2):300–305. doi: 10.1016/j.biopsycho.2011.11.002. doi: http://dx.doi.org.udel.idm.oclc.org/10.1016/j.biopsycho.2011.11.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ehlers A, Clark DM. A cognitive model of posttraumatic stress disorder. Behaviour Research and Therapy. 2000;38(4):319–345. doi: 10.1016/s0005-7967(99)00123-0. doi: http://dx.doi.org.udel.idm.oclc.org/10.1016/S0005-7967(99)00123-0. [DOI] [PubMed] [Google Scholar]
- Ehring T, Ehlers A, Glucksman E. Do cognitive models help in predicting the severity of posttraumatic stress disorder, phobia, and depression after motor vehicle accidents? A prospective longitudinal study. Journal of Consulting and Clinical Psychology. 2008;76(2):219–230. doi: 10.1037/0022-006X.76.2.219. doi: http://dx.doi.org.udel.idm.oclc.org/10.1037/0022-006X.76.2.219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Elwood LS, Mott J, Williams NL, Lohr JM, Schroeder DA. Attributional style and anxiety sensitivity as maintenance factors of posttraumatic stress symptoms: A prospective examination of a diathesis–stress model. Journal of Behavior Therapy and Experimental Psychiatry. 2009;40(4):544–557. doi: 10.1016/j.jbtep.2009.07.005. doi: http://dx.doi.org/10.1016/j.jbtep.2009.07.005. [DOI] [PubMed] [Google Scholar]
- Engelhard IM, Huijding J, van den Hout MA, de Jong PJ. Vulnerability associations and symptoms of post-traumatic stress disorder in soldiers deployed to iraq. Behaviour Research and Therapy. 2007;45(10):2317–2325. doi: 10.1016/j.brat.2007.04.005. doi: http://dx.doi.org.udel.idm.oclc.org/10.1016/j.brat.2007.04.005. [DOI] [PubMed] [Google Scholar]
- Finn RH. A note on estimating the reliability of categorical data. Educational and Psychological Measurement. 1970;30:70–76. doi: http://dx.doi.org/10.1177/001316447003000106. [Google Scholar]
- Flora DB. Specifying piecewise latent trajectory models for longitudinal data. Structural Equation Modeling. 2008;(15):513–533. [Google Scholar]
- Foa EB, Kozak MJ. Emotional processing of fear: Exposure to corrective information. Psychological Bulletin. 1986;99(1):20–35. doi: http://dx.doi.org.udel.idm.oclc.org/10.1037/0033-2909.99.1.20. [PubMed] [Google Scholar]
- Foa EB, Huppert JD, Cahill SP. Pathological anxiety: Emotional processing in etiology and treatment. Guilford Press, New York, NY.; New York, NY, US: 2006. Emotional processing theory: An update. pp. 3–24. [Google Scholar]
- Foa EB, Ehlers A, Clark DM, Tolin DF, Orsillo SM. The posttraumatic cognitions inventory (PTCI): Development and validation. Psychological Assessment. 1999;11(3):303–314. doi: http://dx.doi.org/10.1037/1040-3590.11.3.303. [Google Scholar]
- Hayes AM, Feldman GC, Goldfried MR. In: The change and growth experiences scale: A measure of insight and emotional processing. Castonguay LG, Hill C, editors. American Psychological Association; Washington, DC, US: 2007. pp. 231–253. doi:10.1037/11532-011. [Google Scholar]
- Hermans D, Baeyens F. Generalization as a basis for emotional change: Perceptual and non-perceptual processes. In: Hermans D, Rimé B, Mesquita B, editors. Changing emotions. Psychology Press; Hove, UK: 2013. pp. 67–73. [Google Scholar]
- Kleim B, Grey N, Wild J, Nussbeck FW, Stott R, Hackmann A, Ehlers A. Cognitive change predicts symptom reduction with cognitive therapy for posttraumatic stress disorder. Journal of Consulting and Clinical Psychology. 2013;81(3):383–393. doi: 10.1037/a0031290. doi: http://dx.doi.org.proxy.nss.udel.edu/10.1037/a0031290. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Linehan MM. Cognitive-behavioral treatment of borderline personality disorder. Guilford Press; New York, NY, US: 1993. [Google Scholar]
- Lissek S. Toward an account of clinical anxiety predicated on basic, neurally mapped mechanisms of Pavlovian fear-learning: The case for conditioned overgeneralization. Depression and Anxiety. 2012;29(4):257–263. doi: 10.1002/da.21922. doi: http://dx.doi.org/10.1002/da.21922. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Masuda A, Hayes SC, Sackett CF, Twohig MP. Cognitive defusion and self-relevant negative thoughts: Examining the impact of a ninety year old technique. Behaviour Research and Therapy. 2004;42(4):477–485. doi: 10.1016/j.brat.2003.10.008. doi: http://dx.doi.org.udel.idm.oclc.org/10.1016/j.brat.2003.10.008. [DOI] [PubMed] [Google Scholar]
- Meiser-Stedman R, Dalgleish T, Glucksman E, Yule W, Smith P. Maladaptive cognitive appraisals mediate the evolution of posttraumatic stress reactions: A 6-month follow-up of child and adolescent assault and motor vehicle accident survivors. Journal of Abnormal Psychology. 2009;118(4):778–787. doi: 10.1037/a0016945. doi: http://dx.doi.org.udel.idm.oclc.org/10.1037/a0016945. [DOI] [PubMed] [Google Scholar]
- Moore SA, Zoellner LA. Overgeneral autobiographical memory and traumatic events: An evaluative review. Psychological Bulletin. 2007;133(3):419–437. doi: 10.1037/0033-2909.133.3.419. doi: http://dx.doi.org/10.1037/0033-2909.133.3.419. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Owens GP, Pike JL, Chard KM. Treatment effects of cognitive processing therapy on cognitive distortions of female child sexual abuse survivors. Behavior Therapy. 2001;32(3):413–424. doi: http://dx.doi.org/10.1016/S0005-7894(01)80028-9. [Google Scholar]
- Palosaari E, Punamäki R, Diab M, Qouta S. Posttraumatic cognitions and posttraumatic stress symptoms among war-affected children: A cross-lagged analysis. Journal of Abnormal Psychology. 2013;122(3):656–661. doi: 10.1037/a0033875. doi: http://dx.doi.org/10.1037/a0033875. [DOI] [PubMed] [Google Scholar]
- Park CL. Making sense of the meaning literature: An integrative review of meaning making and its effects on adjustment to stressful life events. Psychological Bulletin. 2010;136(2):257–301. doi: 10.1037/a0018301. doi: http://dx.doi.org.udel.idm.oclc.org/10.1037/a0018301. [DOI] [PubMed] [Google Scholar]
- Preacher KJ, Curran PJ, Bauer DJ. Computational tools for probing interaction effects in multiple linear regression, multilevel modeling, and latent curve analysis. Journal of Educational and Behavioral Statistics. 2006;31:437–448. [Google Scholar]
- Raudenbush SW, Bryk AS, Cheong YF, Congdon RT, du Toit M. HLM 7. Scientific Software International, Inc.; 2011. [Google Scholar]
- Resick PA, Monson CM, Chard KM. Cognitive processing therapy: Veteran/military version. Department of Veterans Affairs; Washington, DC: 2014. [Google Scholar]
- Salmon K, Bryant RA. Posttraumatic stress disorder in children: The influence of developmental factors. Clinical Psychology Review. 2002;22(2):163–188. doi: 10.1016/s0272-7358(01)00086-1. doi: http://dx.doi.org.udel.idm.oclc.org/10.1016/S0272-7358(01)00086-1. [DOI] [PubMed] [Google Scholar]
- Salmon K, Sinclair E, Bryant RA. The role of maladaptive appraisals in child acute stress reactions. British Journal of Clinical Psychology. 2007;46(2):203–210. doi: 10.1348/014466506X160704. doi: http://dx.doi.org.udel.idm.oclc.org/10.1348/014466506X160704. [DOI] [PubMed] [Google Scholar]
- Shrout PE, Fleiss JL. Intraclass correlations: Uses in assessing rater reliability. Psychological Bulletin. 1979;86(2):420–428. doi: 10.1037//0033-2909.86.2.420. [DOI] [PubMed] [Google Scholar]
- Silverman WK, Ortiz CD, Viswesvaran C, Burns BJ, Kolko DJ, Putnam FW, Amaya-Jackson L. Evidence-based psychosocial treatments for children and adolescents exposed to traumatic events. Journal of Clinical Child and Adolescent Psychology. 2008;37(1):156–183. doi: 10.1080/15374410701818293. doi: http://dx.doi.org/10.1080/15374410701818293. [DOI] [PubMed] [Google Scholar]
- Sobel AA, Resick PA, Rabalais AE. The effect of cognitive processing therapy on cognitions: Impact statement coding. Journal of Traumatic Stress. 2009;22(3):205–211. doi: 10.1002/jts.20408. doi: http://dx.doi.org/10.1002/jts.20408. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Steinberg AM, Brymer MJ, Decker K, Pynoos RS. The University of California at Los Angeles Post-Traumatic Stress Disorder Reaction Index. Current Psychiatry Reports. 2004;(6):96–100. doi: 10.1007/s11920-004-0048-2. [DOI] [PubMed] [Google Scholar]
- Waters AM, Henry J, Neumann DL. Aversive pavlovian conditioning in childhood anxiety disorders: Impaired response inhibition and resistance to extinction. Journal of Abnormal Psychology. 2009;118(2):311–321. doi: 10.1037/a0015635. doi: http://dx.doi.org.udel.idm.oclc.org/10.1037/a0015635. [DOI] [PubMed] [Google Scholar]
- Watkins ER, Baeyens CB, Read R. Concreteness training reduces dysphoria: Proof-of-principle for repeated cognitive bias modification in depression. Journal of Abnormal Psychology. 2009;118(1):55–64. doi: 10.1037/a0013642. doi: http://dx.doi.org/10.1037/a0013642. [DOI] [PubMed] [Google Scholar]
- Zalta AK, Gillihan SJ, Fisher AJ, Mintz J, McLean CP, Yehuda R, Foa EB. Change in negative cognitions associated with PTSD predicts symptom reduction in prolonged exposure. Journal of Consulting and Clinical Psychology. 2013;82(1):171–175. doi: 10.1037/a0034735. doi: http://dx.doi.org.proxy.nss.udel.edu/10.1037/a0034735. [DOI] [PMC free article] [PubMed] [Google Scholar]