Abstract
Background
Recent estimates of the global burden of rheumatic heart disease (RHD) have highlighted the paucity of reliable RHD mortality data from populations most affected by RHD.
Methods and Results
We investigated RHD mortality rates and trends for Indigenous and non-Indigenous Australians in the Northern Territory (NT) for the period 1977–2005 and seminationally (NT plus 4 other states, covering 89% of Indigenous Australians) from 1997 to 2005 using vital statistics data. All analysis was undertaken by Indigenous status, sex, and age at death. In the NT, 90% of all deaths from RHD were among Indigenous persons; however, the Indigenous population makes up only 30.4% of the NT population. The death rate ratio (Indigenous compared with non-Indigenous) was 54.80 in the NT and 12.74 in the other 4 states (estimated at the median age of 50 years). Non-Indigenous death rates were low for all age groups except ≥65 years, indicating RHD deaths in the elderly non-Indigenous population. Death rates decreased at a more rapid rate for non-Indigenous than Indigenous persons in the NT between 1997 and 2005. Indigenous persons in other parts of Australia showed lower death rates than their NT counterparts, but the death rates for Indigenous persons in all states were still much higher than rates for non-Indigenous Australians.
Conclusions
Indigenous Australians are much more likely to die from RHD than other Australians. Among the Indigenous population, RHD mortality is much higher in the NT than elsewhere in Australia, exceeding levels reported in many industrialized countries more than a century ago. With the paucity of data from high-prevalence areas, these data contribute substantially to understanding the global burden of RHD mortality.
Keywords: Australia, epidemiology, Indigenous population, mortality, rheumatic heart disease, risk factors
Rheumatic heart disease (RHD) is a disease of social disadvantage and deprivation. Over the past 60 years there have been impressive declines in the prevalence of RHD throughout the industrialized world, including Australia, mainly as a result of improvements in socioeconomic conditions (including reduced household crowding) and access to health services. These improvements have yet to be seen in many developing countries and in Indigenous populations in developed countries. Indigenous populations in developed countries frequently live in deprived settings and face issues of lower living standards similar to populations in developing countries.1
An RHD systematic review done as part of the Global Burden of Disease Study 2010 found very few RHD mortality data sets available globally, and only 4 countries—Australia, New Zealand, India, and Ethiopia—had any recent population-based data.2–6 Attempts to determine global RHD mortality have relied on mathematical models to infer global estimates using data either from the United States in the 1950s7 or from the above 4 countries.8 Australia is one of the few settings with a high-RHD-incidence population (Indigenous Australians) that also has access to good cause-specific mortality data, which could assist with global understanding of RHD mortality in the 21st century. Nonetheless, there are few data with which to examine mortality in the Indigenous population and only a limited number of reports examining RHD mortality internationally.4,9–11
Indigenous Australians make up ≈2.5% of the total Australian population; live predominantly in conditions of social, economic, and environmental disadvantage; and often have poor health status compared with non-Indigenous Australians. Life expectancy of Aboriginal and Torres Strait Islander men is estimated to be 10.6 years lower than that of non-Indigenous men, and life expectancy of Aboriginal and Torres Strait Islander women is 9.5 years lower than that of non-Indigenous women.12 Approximately 89% of the total Australian Indigenous population lives in 5 states of Australia: the Northern Territory (NT), Queensland, South Australia, Western Australia, and New South Wales. The NT population has the highest proportion of Indigenous Australians (30.4%) compared with all other Australian states or territories, in which Indigenous Australians compose <4% of the population. In the NT, 92% of those with RHD are Indigenous, and 85% of those live in remote communities and towns. Indigenous persons living in the NT have the highest reported RHD incidence globally.13,14
Australia has a comprehensive system of recording mortality and has produced accurate and detailed statistics on RHD mortality for several decades.15 This system has demonstrated a decline in total RHD death rates in Australia over the past 4 decades; however, these RHD mortality statistics disguise the excess mortality from RHD among Indigenous persons because specific mortality rates are not reported for Indigenous Australians. In addition, Indigenous status is not always recorded, or recorded correctly, in death registrations in most states and territories, meaning that the number of deaths registered as Indigenous is an underestimate of the actual number of deaths among the Indigenous population. In the NT, Indigenous death identification has been at a consistently high level since at least 1977, meaning that mortality rates in the Indigenous population for RHD can be determined accurately for the NT Indigenous population since that time.16 This study was undertaken to provide a comprehensive examination of RHD mortality rates and trends in Indigenous Australians.
Methods
Australia has almost complete registration of deaths and reliable classification of cause of death. Reliable Indigenous identification data have been available for the NT since 1977 and for 4 other jurisdictions since 1997 (New South Wales, Queensland, South Australia, and Western Australia, referred to hereafter as the 4 states). Indigenous identification in death registrations remains unreliable in 3 jurisdictions (Australian Capital Territory, Tasmania, and Victoria), which were not included in this study. The 4 states plus the NT (the 5 states) account for 89% of the total Australian Indigenous population.16
We undertook 3 separate analyses using vital statistics data from Australian death certificates. The first was a comparison of Indigenous and non-Indigenous death rates and time trends in RHD mortality in the NT for the 29-year period 1977–2005. The second was a comparison of RHD mortality for the NT Indigenous population with that of the Indigenous population of the 4 states and with that of the non-Indigenous population of the 5 states for the 9-year period 1997–2005. The third was a comparison of RHD mortality between the Indigenous and non-Indigenous populations of the 5 states for 1997–2005, including a description of the proportion of deaths attributed to RHD as an underlying or associated cause of death.
Statistical Analysis
We calculated the number of RHD deaths, the age-specific death rate (in age groups 0 to 4, 5 to 24, 25 to 44, 45 to 64 and ≥65 years), and the age-adjusted death rate. The population data used to calculate mortality rates was the Estimated Resident Population (by Indigenous status, sex, 5-year age group, and calendar year) of each state or territory, published by the Australian Bureau of Statistics.17 The age distribution of the 2001 Australian Estimated Resident Population was used as the standard weight for calculation of age-adjusted rates. Ratios of age-standardized death rates are not presented because of the large differences in mortality rate ratios between age groups. We tested for but did not find evidence of linearity in time trends, particularly in terms of changes in International Classification of Diseases (ICD) coding.
RHD death rates for Indigenous populations were compared with those for non-Indigenous populations by age group and sex. Time trends were examined by calculating mortality rates for 3 periods (1977–1986, 1987–1996, and 1997–2005). Death rate ratios (DRR) were calculated using the age-specific mortality of the NT Indigenous population compared with the non-Indigenous population of the 5 states.
Multivariate negative binomial regression was also used to analyze RHD mortality. The regression model for the NT between 1977 and 2005 included terms for Indigenous status (Indigenous compared with non-Indigenous population), age of death (per single year of age), sex (female compared with male), and year of death (in single calendar years) and 2 interaction terms, Indigenous status by age at death and Indigenous status by year of death. The interaction terms were included because the effects of age at death and year of death were found to be different for Indigenous and non-Indigenous persons. In the regression analysis, the term for age at death was based at age 50 years (the median death age), and year of death was based at 1991 (the midpoint of the study period).
The regression model for other analysis (ie, 1997–2005) was the same except that age was included in 5-year age groups and year of death was not included because analysis of time trends was not feasible for the shorter 9-year period.
For most analyses, we included only deaths in which the underlying cause of death was RHD (including acute rheumatic fever (ARF)). The underlying cause of death was coded using ICD version 8 (until 1978), version 9 (1978–1998), and version 10 (1998 onward). Only ICD-10 death data were coded for both associated and underlying cause of death. Death data were not available after 2005. We undertook a separate analysis comparing RHD as the underlying cause of death with RHD as the associated cause of death across all 5 states to investigate the extent to which RHD was contributing to deaths but was not identified as the single underlying cause.
All data were analyzed using Stata software (version 11; StataCorp). All mortality rates are expressed per 100 000 person-years. Ethics approval was granted by the human research ethics committee of the NT Department of Health and Menzies School of Health Research, including its Indigenous subcommittee (HREC number 10-1488); the human research ethics committee approved the use of statutory death data without participant consent.
Results
RHD Mortality in the NT, 1977–2005
For the period 1977–2005, there were 280 deaths in the NT due to RHD as the underlying cause; 253 (90%) were among Indigenous persons, and 164 (59%) were among women. The difference in age-specific death rates was higher for all age groups when comparing Indigenous and non-Indigenous persons, with the largest difference seen in the 5- to 24-year age group with a rate ratio of 43.1 (95% CI 14.7 to 143.2). For Indigenous persons, RHD death rates increased with increasing age and were higher for women than for men in all age groups. Non-Indigenous women had a higher death rate than non-Indigenous men at all ages, at 19.2 compared with 10.5, respectively, in the those aged ≥65 years (Table1). For non-Indigenous persons, death rates were low for all age groups except those aged ≥65 years. The highest DRR (206.2) was seen in Indigenous women aged 25 to 44 years. Over the 29 years of the study period, a decline in the age-adjusted death rates was evident for both Indigenous and non-Indigenous persons. The Indigenous rate (men and women combined) decreased from 33.5 per 100 000 in 1977–1986 to 25.3 per 100 000 in 1997–2005 (Table2).
Table 1.
Northern Territory Age-Specific RHD* Deaths,* 1977–2005
| Sex | Indigenous | Non-Indigenous | Rate Ratio† | |||||
|---|---|---|---|---|---|---|---|---|
| Age Group, y | n | Rate‡ | CI | n | Rate | CI | RR | CI |
| Male | ||||||||
| 0 to 4 | 1 | 1.0 | 0.2 to 7.3 | 0 | 0.0 | na | — | na |
| 5 to 24 | 34 | 10.7 | 7.6 to 14.9 | 3 | 0.5 | 0.2 to 1.7 | 19.7 | 6.2 to 100.2 |
| 25 to 44 | 42 | 22.8 | 16.9 to 30.9 | 1 | 0.1 | 0.0 to 1.0 | 162.4 | 27.6 to 6565.8 |
| 45 to 64 | 20 | 30.1 | 19.4 to 46.7 | 4 | 1.2 | 0.4 to 3.1 | 26.0 | 8.7 to 104.8 |
| ≥65 | 5 | 31.4 | 13.1 to 75.4 | 6 | 10.5 | 4.7 to 23.1 | 3.0 | 0.7 to 11.7 |
| Female | ||||||||
| 0 to 4 | 2 | 2.1 | 0.5 to 8.4 | 0 | 0.0 | na | — | na |
| 5 to 24 | 26 | 8.2 | 5.6 to 12.0 | 1 | 0.2 | 0.0 to 1.4 | 40.5 | 6.6 to 1659.0 |
| 25 to 44 | 64 | 33.6 | 26.3 to 42.9 | 1 | 0.2 | 0.2 to 1.2 | 206.2 | 35.7 to 8269.5 |
| 45 to 64 | 45 | 57.2 | 42.7 to 76.6 | 2 | 0.8 | 0.2 to 3.28 | 69.7 | 18.2 to 592.7 |
| ≥65 | 14 | 67.4 | 39.9 to 113.8 | 9 | 19.2 | 10.0 to 36.8 | 3.5 | 1.1 to 9.2 |
| Persons | ||||||||
| 0 to 4 | 3 | 1.6 | 0.5 to 4.8 | 0 | 0.0 | na | — | na |
| 5 to 24 | 60 | 9.4 | 7.3 to 12.1 | 4 | 0.4 | 0.1 to 1.0 | 24.7 | 9.2 to 93.6 |
| 25 to 44 | 106 | 28.3 | 23.4 to 34.2 | 2 | 0.2 | 0.0 to 0.6 | 187.6 | 50.7 to 1568.8 |
| 45 to 64 | 65 | 44.8 | 35.1 to 57.1 | 6 | 1.0 | 0.5 to 2.3 | 44.0 | 19.2 to 124.3 |
| ≥65 | 19 | 51.8 | 33.0 to 81.1 | 15 | 14.2 | 8.7 to 23.9 | 3.6 | 1.7 to 7.5 |
na indicates not applicable; RHD, rheumatic heart disease.
Underlying cause.
Indigenous compared with non-Indigenous.
Per 100 000.
Table 2.
Northern Territory Rheumatic Heart Disease* Deaths by Period, 1977–2005
| Indigenous Status | Male | Female | Total | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Period | n | Rate† | CI | n | Rate | CI | n | Rate | CI |
| Indigenous | |||||||||
| 1977–1986 | 32 | 23.2 | 13.7 to 32.8 | 49 | 43.5 | 27.6 to 59.5 | 81 | 33.5 | 24.2 to 42.8 |
| 1987–1996 | 40 | 25.5 | 15.4 to 35.6 | 49 | 31.2 | 21.8 to 40.6 | 89 | 28.2 | 21.5 to 35.0 |
| 1997–2005 | 30 | 14.8 | 0.80 to 21.6 | 53 | 33.1 | 22.3 to 44.0 | 83 | 25.3 | 18.3 to 32.2 |
| 1977–2005 | 102 | 20.5 | 15.6 to 25.4 | 151 | 35.2 | 28.4 to 42.1 | 253 | 28.4 | 24.1 to 32.7 |
| Non-Indigenous | |||||||||
| 1977–1986 | 6 | 2.9 | 0.0 to 5.8 | 6 | 10.6 | 0.1 to 21.0 | 12 | 6.9 | 1.3 to 12.6 |
| 1987–1996 | 7 | 2.1 | 0.5 to 3.8 | 2 | 1 | 0.0 to 2.4 | 9 | 1.6 | 0.5 to 2.8 |
| 1997–2005 | 1 | 0.1 | 0.0 to 0.4 | 5 | 2.5 | 0.2 to 4.9 | 6 | 1.3 | 0.1 to 2.6 |
| 1977–2005 | 14 | 1.3 | 0.6 to 2.1 | 13 | 3.1 | 1.2 to 4.9 | 27 | 2.3 | 1.3 to 2.4 |
Underlying cause.
Per 100 000.
On multivariable analysis, the RHD death rate for women was 34% higher than for men (Table3). The effect of age at death and year of death was found to be different for Indigenous and non-Indigenous persons. For non-Indigenous persons, RHD death rates increased by 10% per 1-year increase in age and decreased by 7% per year between 1977 and 2005. For Indigenous persons, the increase in death rates with year of age was much less (4% per year of age), and there was minimal if any decrease in RHD death rates between 1977 and 2005 (DRR 0.98, 95% CI 0.97 to 1.00).
Table 3.
Multivariate Analysis, Rheumatic Heart Disease Deaths in the Northern Territory, 1977–2005
| Variable | Death Rate Ratio | 95% CI |
|---|---|---|
| Indigenous status* | 24.18 | 15.61 to 37.46 |
| Female† | 1.34 | 1.06 to 1.71 |
| Age‡ | ||
| Non-Indigenous | 1.10 | 1.07 to 1.13 |
| Indigenous | 1.04 | 1.03 to 1.04 |
| Year* | ||
| Non-Indigenous | 0.93 | 0.88 to 0.97 |
| Indigenous | 0.98 | 0.97 to 1.00 |
Estimated at the median age of 50 years in 1991.
Compared with male.
Single year of age.
RHD Mortality in NT Indigenous Versus Other Indigenous and Non-Indigenous Australians, 1997–2005
For the period 1997–2005, RHD death rates were much higher for Indigenous persons in the NT than in the 4 states combined (Figure1), and both were much higher than rates for non-Indigenous persons. Age-specific death rates were higher for Indigenous persons in the NT than in the 4 states combined for all age groups and for both men and women, with the largest relative differences in the younger age groups (Table4).
Figure 1.
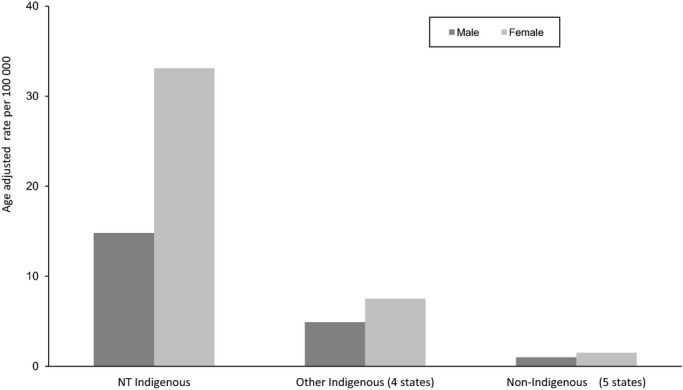
Age-adjusted mortality rate in the period 1997–2005 for Indigenous persons in the NT compared with Indigenous persons in the 4 states and non-Indigenous persons in the 5 states (male and female). 4 states indicates New South Wales, Queensland, South Australia, and Western Australia; 5 states, New South Wales, Queensland, South Australia, Western Australia, and the Northern Territory; NT, Northern Territory.
Table 4.
Age-Specific Rheumatic Heart Disease* Deaths in the Period1997–2005 in Indigenous Persons in the NT and the 4 States and in Non-Indigenous Persons in the 5 States
| Sex | NT Indigenous‡ | 4 States Indigenous† | 5 States Non-Indigenous | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Age Group, y | n | Rate§ | CI | DRR | CI | n | Rate | CI | DRR | CI | n | Rate | CI |
| Male | |||||||||||||
| 0 to 4 | 0 | 0 | na | 0 | na | 0 | 0 | na | 0 | na | 1 | 0 | 0.0 to 0.2 |
| 5 to 24 | 7 | 6.1 | 2.9 to 12.8 | 342.2 | 78.1 to 2051.0 | 5 | 0.7 | 0.3 to 1.7 | 39.6 | 7.7 to 255.0 | 3 | 0 | 0.0 to 0.1 |
| 25 to 44 | 17 | 22.5 | 14.0 to 36.2 | 193.7 | 95.9 to 385.4 | 16 | 3.8 | 2.3 to 6.1 | 32.3 | 15.8 to 65.0 | 21 | 0.2 | 0.1 to 0.2 |
| 45 to 64 | 5 | 18.1 | 7.5 to 43.5 | 25.8 | 8.2 to 62.3 | 13 | 7.2 | 4.2 to 12.4 | 10.8 | 5.3 to 18.4 | 100 | 0.7 | 0.6 to 0.9 |
| ≥65 | 1 | 18.1 | 2.5 to 128.2 | 3.0 | 0.1 to 17.1 | 5 | 12.7 | 5.3 to 30.5 | 2.1 | 0.7 to 5.0 | 405 | 5.9 | 5.9 to 6.5 |
| Female | |||||||||||||
| 0 to 4 | 1 | 3 | 0.4 to 21.6 | 0 | na | 0 | 0 | na | 0 | na | 0 | 0 | na |
| 5 to 24 | 7 | 6.2 | 2.9 to 12.9 | 331.2 | 75.6 to 1984.8 | 6 | 0.9 | 0.4 to 2.0 | 47.4 | 10.1 to 292.7 | 3 | 0 | 0.0 to 0.1 |
| 25 to 44 | 22 | 27.9 | 18.4 to 42.3 | 168.6 | 92.6 to 302.1 | 25 | 5.5 | 3.7 to 8.2 | 33.4 | 18.8 to 58.8 | 30 | 0.2 | 0.1 to 0.2 |
| 45 to 64 | 15 | 46.1 | 27.8 to 76.5 | 46.9 | 25.5 to 80.0 | 19 | 9.8 | 6.3 to 15.4 | 10.0 | 5.8 to 16.2 | 138 | 1 | 0.8 to 1.8 |
| ≥65 | 8 | 92.5 | 46.6 to 184.9 | 9.1 | 3.9 to 18.1 | 15 | 29.1 | 17.6 to 48.3 | 2.9 | 1.6 to 4.8 | 865 | 10.1 | 9.5 to 10.8 |
| Persons | |||||||||||||
| 0 to 4 | 1 | 1.5 | 0.2 to 10.5 | 114.8 | 1.5 to 9008.5 | 0 | 0 | na | 0 | na | 1 | 0 | na |
| 5 to 24 | 14 | 6.1 | 3.6 to 10.4 | 336.8 | 121.6 to 1069.2 | 11 | 0.8 | 0.4 to 1.4 | 43.1 | 14.7 to 143.2 | 6 | 0 | na |
| 25 to 44 | 39 | 25.2 | 18.4 to 34.5 | 179.3 | 115.0 to 277.4 | 41 | 4.7 | 3.4 to 6.3 | 33.1 | 21.4 to 51.0 | 51 | 0.1 | 0.1 to 0.2 |
| 45 to 64 | 20 | 33.2 | 21.4 to 51.5 | 39.5 | 23.7 to 62.4 | 32 | 8.7 | 6.1 to 12.1 | 10.2 | 6.8 to 14.8 | 238 | 0.8 | 0.7 to 1.0 |
| ≥65 | 9 | 63.4 | 33.0 to 121.9 | 7.7 | 3.5 to 14.6 | 20 | 22 | 14.2 to 34.1 | 2.7 | 1.6 to 4.1 | 1270 | 8.3 | 7.8 to 8.7 |
4 states indicates New South Wales, Queensland, South Australia, and Western Australia; 5 states, New South Wales, Queensland, South Australia, Western Australia, and the Northern Territory; DRR, death rate ratio; na, not applicable; NT, Northern Territory.
Underlying cause only.
Four states Indigenous compared with 5 states non-Indigenous.
NT Indigenous compared with 5 states non-Indigenous.
Per 100 000.
On multivariable analysis, between 1997 and 2005, the RHD death rate (estimated at the median age of 50 years) was much higher for Indigenous Australians in the NT (54.8 times higher, 95% CI 41.6 to 72.3) and in the 4 states combined (12.7 times higher, 96% CI 10.1 to 16.1) than for non-Indigenous Australians (Table5). The increases in death rates with age and for women compared with men were similar for the NT and the 4 states in both analyses.
Table 5.
Multivariate Regression Analysis of Indigenous Persons in the NT and the 4 States Compared With Non-Indigenous Persons in the 5 States, 1997–2005
| Variable | NT | 4 States | ||
|---|---|---|---|---|
| DRR | CI | DRR | CI | |
| Indigenous status* | 54.80 | 41.58 to 72.24 | 12.74 | 10.09 to 16.09 |
| Female† | 1.52 | 1.35 to 1.72 | 1.52 | 1.34 to 1.71 |
| Age | ||||
| Non-Indigenous | 1.12 | 1.11 to 1.13 | 1.12 | 1.11 to 1.13 |
| Indigenous | 1.04 | 1.03 to 1.05 | 1.05 | 1.04 to 1.06 |
4 states indicates New South Wales, Queensland, South Australia, and Western Australia; 5 states, New South Wales, Queensland, South Australia, Western Australia, and the Northern Territory; DRR, death rate ratio; NT, Northern Territory.
Base age of 50 years.
Compared with male.
RHD Mortality in the 5 States, 1997–2005
Between 1997 and 2005 there were 1753 deaths with RHD as the underlying cause of death, of which 187 (10.7%) were among Indigenous persons (69 men and 118 women) and 1157 (66%) were among women. The age-specific rates were higher for Indigenous persons in all age groups (Table6). The DRR peaked in those aged 5 to 24 years and remained considerably elevated in those aged 25 to 44 years. The DRR remained elevated, although less so, in the older age groups. Multivariate analysis of the 5 states (estimated at the median age of 50 years) showed that the RHD death rate for the Indigenous population of the 5 states combined was 18.9 times higher than that of non-Indigenous Australians.
Table 6.
Age-Specific Rheumatic Heart Disease Deaths and Death Rate Ratio in the 5 States *, 1997–2005
| Sex | Indigenous | Non-Indigenous | Rate Ratio | |||||
|---|---|---|---|---|---|---|---|---|
| Age Group, y | n | Rate | CI | n | Rate | CI | DRR | CI |
| Male | ||||||||
| 0 to 4 | 0 | 0.0 | na | 1 | 0.0 | 0.0 to 0.2 | na | — |
| 5 to 24 | 12 | 1.5 | 0.8 to 2.6 | 3 | 0.0 | 0.0 to 0.1 | 39.2 | 7.6 to 252.2 |
| 25 to 44 | 33 | 6.6 | 4.7 to 9.3 | 21 | 0.2 | 0.1 to 0.2 | 31.9 | 15.5 to 64.1 |
| 45 to 64 | 18 | 8.7 | 5.5 to 13.8 | 100 | 0.7 | 0.6 to 0.9 | 10.3 | 5.3 to 18.4 |
| ≥65 | 6 | 13.5 | 6.0 to 30.0 | 405 | 5.9 | 5.9 to 6.5 | 2.1 | 0.7 to 5.0 |
| Female | ||||||||
| 0 to 4 | 1 | 0.9 | 0.1 to 2.8 | 0 | 0.0 | na | na | — |
| 5 to 24 | 13 | 1.6 | 1.0 to 2.8 | 3 | 0.02 | 0.0 to 0.1 | 46.9 | 10.0 to 289.7 |
| 25 to 44 | 47 | 8.9 | 6.7 to 11.8 | 30 | 0.17 | 0.1 to 0.2 | 33 | 18.6 to 58.1 |
| 45 to 64 | 34 | 15.1 | 10.8 to 21.1 | 138 | 0.98 | 0.8 to 1.2 | 10 | 5.8 to 16.2 |
| ≥65 | 23 | 38.4 | 25.5 to 57.9 | 865 | 10.13 | 9.5 to 10.8 | 2.9 | 1.6 to 4.8 |
| Persons | ||||||||
| 0 to 4 | 1 | 0.19 | 0.0 to 1.4 | 1 | 0.0 | na | — | — |
| 5 to 24 | 25 | 1.55 | 1.0 to 2.3 | 6 | 0.0 | na | 39.2 | 7.6 to 252.2 |
| 25 to 44 | 80 | 7.75 | 6.2 to 9.7 | 51 | 0.1 | 0.1 to 0.2 | 31.9 | 15.6 to 64.2 |
| 45 to 64 | 52 | 12.04 | 9.2 to 15.8 | 238 | 0.84 | 0.7 to 1.0 | 10.3 | 5.3 to 18.4 |
| ≥65 | 29 | 27.76 | 19.9 to 40.0 | 1270 | 8.26 | 7.8 to 8.7 | 2.1 | 0.7 to 5.0 |
DRR indicates death rate ratio; na, not applicable.
Underlying cause.
RHD mortality by underlying and associated cause in the 5 states, 1997–2005
The majority of Indigenous persons who died from RHD had RHD recorded as the underlying cause of death rather than as an associated cause of death; 64% of RHD deaths in the NT and 58% in the other 4 states were among Indigenous persons. Only a small proportion of RHD deaths in Indigenous persons occurred in those aged ≥65 years. The opposite was the case for non-Indigenous persons with RHD: The majority of deaths occurred in those aged ≥65 years (81%), and among those patients, only 17% of deaths were recorded with RHD as the underlying cause. Overall, in the non-Indigenous population, the majority of deaths were due to RHD as an associated rather than an underlying cause.
Discussion
Indigenous Australians are much more likely to die from RHD than other Australians. Rates of death from RHD among Indigenous persons in the NT exceed those of other states in Australia and those reported in many industrialized countries more than a century ago.18 An Indigenous person living in the NT of Australia is 54.8 times more likely to die of RHD than a non-Indigenous person. RHD mortality was ≈50% higher for women than for men among both Indigenous and non-Indigenous persons, and that finding is consistent with other evidence of higher RHD mortality in women.10,19,20
The excess RHD mortality of the NT Indigenous population (compared with the non-Indigenous population) is at least partly due to poorer living conditions and household overcrowding.21 Poorer access to health care for the large proportion of the NT Indigenous population that lives in remote areas may also play a role.22,23 These same factors may also explain the excess RHD mortality of Indigenous persons in the NT compared with those elsewhere in Australia; the disparities between Indigenous and non-Indigenous Australians in living conditions, overcrowding, and proportion of people living in remote areas is greatest in the NT.22 Excess mortality is mostly due to higher incidence of RHD and partly due to more severe disease, both of which contribute to the increased disease burden among Indigenous persons.
The disparity in the distribution of the burden of RHD disease contributes to the gap in life expectancy of Indigenous persons in the NT. In recent years, a number of initiatives have been undertaken to address this disparity including the establishment of the NT Rheumatic Heart Disease Register in 1996 and the commitment of the Australian government to a seminational RHD control program: RHDAustralia.
Increased mortality from RHD in young people is seen elsewhere in high-prevalence, resource-poor countries, although limited population-based mortality data are available to quantify this observation, and further studies are required.5,24,25 A recent examination of the Fiji RHD national register and clinical data has shown that the risk of death of patients with RHD is increased 8.8 times compared with the general population; this risk is greatest among young Indigenous men (DRR 50, 95% CI 35.0 to 69.2) compared with the non-Indigenous Fijian population.26
Over time, RHD mortality in Australia has decreased much more for the non-Indigenous population (7.4% per year) than for the Indigenous population (1.8% per year). Non-Indigenous Australians were also more likely to die from other causes, with RHD contributing as an associated, rather than the underlying, cause of death. This example highlights how health indicators are improving more slowly for Indigenous persons than for non-Indigenous Australians, contributing to a widening of the gap in health outcomes such as life expectancy. Non-Indigenous persons were more likely to die in their elderly years of associated-cause RHD mortality (59% of total non-Indigenous RHD deaths were from RHD as an associated cause). RHD deaths among Indigenous persons occurred in much larger proportions at younger ages and as the underlying cause. These data suggest that non-Indigenous persons are living longer with disease and die from associated factors, possibly because those affected with severe disease as children died many years ago when RHD was prevalent in the non-Indigenous population, whereas Indigenous young people are still dying with RHD as a direct cause of disease.27,28
In the NT during the study period, the accuracy of death certification was high, demonstrated by studies with linked data sets of census and mortality data.29 The accuracy of death certification data for the 4 other states studied is less certain. In the NT, RHD awareness is greater than in other jurisdictions because of the high RHD prevalence and the RHD control program that has been in existence since the late 1990s. The NT RHD control program has seen many cases of preexisting but undiagnosed RHD identified and registered. This suggests that there may be similar cases in Western Australia, Queensland, South Australia, and New South Wales because none of those states had registers or control programs in place during the data analysis period. There may be people with RHD who died or whose RHD was either unknown or not thought to have contributed to their death, and this proportion may be greater in the other 4 states than in the NT.
This study has a number of limitations relating to data access, Indigenous identification, and ICD coding. The most recent year for which complete data (by year of death, not year of registration) were available for this study was 2005 because access to Australian cause-of-death data for deaths registered after 2007 has not been possible because of legal and bureaucratic issues that have taken many years to resolve. A new process to request access for research and population health-monitoring purposes commenced in mid-2014. We relied on vital statistics data, and cause of death may not be perfect on death certificates.
Due to the relatively small number of deaths from RHD, the confidence intervals presented are wide (Table1). The difference in rates of mortality from RHD among the Indigenous and non-Indigenous populations studied was large, but ratios should be interpreted with this limitation considered.
The accuracy of Indigenous identification in death data is less reliable in the 4 states than it is in the NT, and the NT is the only state or territory with reliable Indigenous identification since the 1970s. Indigenous identification in death data from the NT has a reported accuracy of 98.8%, whereas Indigenous status in the other states’ death data may be underestimated by ≈15%.30
Another factor that may have influenced the accuracy of the data for the 29-year period in the NT were the 2 changes in ICD coding. In 1997 there was a change in ICD coding from ICD-9 to ICD-10, which resulted in some artifactual variation in disease coding. The comparability with ICD-9 has been assessed by the Australian Bureau of Statistics.31,32 Changes in coding may contribute to an underestimation of mortality rate and may falsely suggest a decline. The change in ICD-10 coding appears to have produced a step in the decline in mortality from 1997 to 1999, but we found that the effect of the change in coding was less than expected and did not appear to produce a statistically significant change.
There were inherent limitations in the multivariate analysis model. The model makes assumptions that the linear effect of age and time and the effect for all predictors are assumed to be constant over time, except for the effect of Indigenous status. Our model, however, did not account for the change over time in the relative rates for various age categories or for sex.
This mortality study provided a comprehensive review of RHD mortality in Australia, with a focus on understanding the disparity in mortality between Indigenous and non-Indigenous populations. As shown by the 2005 study of the global burden of group A streptococcal disease7 and the recent Global Burden of Disease Study 2010,33 very few RHD data are available to measure actual RHD in either high- and low-prevalence regions. Current published global mortality estimates are based largely on estimates extrapolated from expected numbers of deaths of persons living with RHD, not on vital statistics or register-based mortality data. Further research is required to determine the rates of RHD mortality in Indigenous populations of developed countries and in developing countries with known high prevalence of RHD.
Sources of Funding
This research was undertaken as part of Dr. Colquhoun’s doctoral work. No additional funding was sourced to undertake this study.
Disclosures
None.
References
- Canberra: AIHW; Comparing life expectancy of indigenous people in Australia, New Zealand, Canada and the United States: conceptual, methodological and data issues. Australian Institute of Health and Welfare 2011. Cat. no. 47. [Google Scholar]
- Gunther G, Asmera J, Parry E. Death from rheumatic heart disease in rural Ethiopia. Lancet. 2006;367:391. doi: 10.1016/S0140-6736(06)68128-2. [DOI] [PubMed] [Google Scholar]
- Craig E, McDonald G, Wicken A, Reddington A, Tafua S. 2010. University of Otago The determinants of health for Pacific children and young people in New Zealand. New Zealand Child and Youth Epidemiology Service.
- Carapetis JR, Currie BJ. Mortality due to acute rheumatic fever and rheumatic heart disease in the Northern Territory: a preventable cause of death in aboriginal people. Aust N Z J Public Health. 1999;23:159–163. doi: 10.1111/j.1467-842x.1999.tb01227.x. [DOI] [PubMed] [Google Scholar]
- Oli K, Asmera J. Rheumatic heart disease in Ethiopia: could it be more malignant? Ethiop Med J. 2004;42:1–8. [PubMed] [Google Scholar]
- Kumar R, Raizada A, Aggarwal AK, Ganguly NK. A community-based rheumatic fever/rheumatic heart disease cohort: twelve-year experience. Indian Heart J. 2002;54:54–58. [PubMed] [Google Scholar]
- Carapetis JR, Steer AC, Mulholland EK, Weber M. The global burden of group A streptococcal diseases. Lancet Infect Dis. 2005;5:685–694. doi: 10.1016/S1473-3099(05)70267-X. [DOI] [PubMed] [Google Scholar]
- Lozano R, Naghavi M, Foreman K, Lim S, Shibuya K, Aboyans V, Abraham J, Adair T, Aggarwal R, Ahn SY, Alvarado M, Anderson HR, Anderson LM, Andrews KG, Atkinson C, Baddour LM, Barker-Collo S, Bartels DH, Bell ML, Benjamin EJ, Bennett D, Bhalla K, Bikbov B, Abdulhak AB, Birbeck G, Blyth F, Bolliger I, Boufous S, Bucello C, Burch M, Burney P, Carapetis J, Chen H, Chou D, Chugh SS, Coffeng LE, Colan SD, Colquhoun S, Colson KE, Condon J, Connor MD, Cooper LT, Corriere M, Cortinovis M, Courville de Vaccaro K, Couser W, Cowie BC, Criqui MH, Cross M, Dabhadkar KC, Dahodwala N, De Leo D, Degenhardt L, Delossantos A, Denenberg J, Jarlais DCD, Dharmaratne SD, Dorsey ER, Driscoll T, Duber H, Ebel B, Erwin PJ, Espindola P, Ezzati M, Feigin V, Flaxman AD, Forouzanfar MH, Fowkes FGR, Franklin R, Fransen M, Freeman MK, Gabriel SE, Gakidou E, Chem FG, Gillum RF, Gonzalez-Medina D, Halasa YA, Haring D, Harrison JE, Rasmus Havmoeller R, Hay RJ, Hoen B, Hotez PJ, Hoy D, Jacobsen KH, James SL, Jasrasaria R, Jayaraman S, Johns N, Karthikeyan G, Kassebaum N, Keren A, Khoo J-P, Knowlton LM, Kobusingye O, Koranteng A, Krishnamurthi R, Lipnick M, Lipshultz SE, Ohno SL, Mabweijano J, MacIntyre MF, Mallinger L, March L, Marks GB, Marks R, Matsumori A, Matzopoulos R, Mayosi BM, McAnulty JH, McDermott MM, McGrath J, Mensah GA, Merriman TR, Michaud C, Miller M, Miller TR, Mock C, Mocumbi AO, Mokdad AA, Moran A, Mulholland K, Nair MN, Naldi L, Narayan KMV, Nasseri K, Norman P, O’Donnell M, Omer SB, Ortblad K, Osborne R, Ozgediz D, Pahari B, Pandian JD, Rivero AP, Padilla RP, Perez-Ruiz F, Perico N, Phillips D, Pierce K, Pope AC,III, Porrini E, Pourmalek F, Raju M, Ranganathan D, Rehm JT, Rein DB, Remuzzi G, Rivara FP, Roberts T, Rodriguez De León F, Rosenfeld LC, Rushton L, Sacco RL, Salomon JA, Sampson U, Sanman E, Schwebel DC, Segui-Gomez M, Shepard DS, Singh D, Singleton J, Sliwa K, Smith E, Steer A, Taylor JA, Thomas B, Tleyjeh IM, Towbin JA, Truelsen T, Eduardo A, Undurraga EA, Venketasubramanian N, Vijayakumar L, Vos T, Wagner GR, Wang M, Wang W, Watt K, Weinstock MA, Weintraub R, Wilkinson JD, Woolf AD, Wulf S, Yeh P-H, Yip P, Zabetian A, Zheng Z-J, Lopez AD, Murray CJL. Global and regional mortality from 235 causes of death for 20 age groups in 1990 and 2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet. 2012;380:2095–2128. doi: 10.1016/S0140-6736(12)61728-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Penm E. AIHW. Canberra: AIHW; 2008. Cardiovascular disease and its associated risk factors in Aboriginal and Torres Strait Islander peoples 2004–05. Cardiovascular disease series no. 29. Cat. no. CVD 41. [Google Scholar]
- NT Department of Health and Community Services; 1995. Northern Territory Health Outcomes Report: Morbidity and Mortality 1979–1991. [Google Scholar]
- MacDonald M, Brown A, Noonan S. Preventing recurrent rheumatic fever: the role of register based programmes. Heart. 2005;91:1131–1133. doi: 10.1136/hrt.2004.057570. [DOI] [PMC free article] [PubMed] [Google Scholar]
- The Health and Welfare of Australia’s Aboriginal and Torres Strait Islander Peoples. Canberra: Australian Institute of Health and Welfare; 2010. . Contract No: 4704. [Google Scholar]
- Carapetis JR, Currie BJ. Clinical epidemiology of rheumatic fever and rheumatic heart disease in tropical Australia. Adv Exp Med Biol. 1997;418:233–236. doi: 10.1007/978-1-4899-1825-3_56. [DOI] [PubMed] [Google Scholar]
- Carapetis JR, Wolff DR, Currie BJ. Acute rheumatic fever and rheumatic heart disease in the top end of Australia’s Northern Territory. Med J Aust. 1996;164:146–149. doi: 10.5694/j.1326-5377.1996.tb122012.x. [DOI] [PubMed] [Google Scholar]
- Australian Institute of Health and Welfare (AIHW) GRIM (General Record of Incidence of Mortality) Books. Canberra: AIHW; 2008. [Google Scholar]
- Australian Bureau of Statistics. 2006. Canberra Experimental Estimates of Aboriginal and Torres Strait Islander Australians. Contract No: 3238.0.55.001.
- Information Paper: External Causes of Death: Data Quality 2005. Canberra: Australian Bureau of Statistics; 2007. . Catalogue no.3317.055.001. Available at: http://www.abs.gov.au/ausstats/abs@.nsf/mf/3317.0.55.001. [Google Scholar]
- 2002. Canberra Australian Bureau of Statistics Mortality and Morbidity: Cardiovascular Disease: 20th Century Trends. Australian Social Trends: Contract no: 4102.0.
- 2002. Canberra Australian Bureau of Statistics Assessment of methods for developing life tables. Discussion Paper.. Contract no. 3302.0.55.002.
- Haddad N, Silva MB. Mortality due to cardiovascular disease in women during the reproductive age (15 to 49 years), in the State of Sao Paulo, Brazil, from 1991 to 1995. Arq Bras Cardiol. 2000;75:375–379. doi: 10.1590/s0066-782x2000001100002. Nov; [DOI] [PubMed] [Google Scholar]
- McDonald MI, Towers RJ, Andrews R, Benger N, Fagan P, Currie BJ, Carapetis JR. The dynamic nature of group A streptococcal epidemiology in tropical communities with high rates of rheumatic heart disease. Epidemiol Infect. 2008;136:529–539. doi: 10.1017/S0950268807008655. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Biddle N, Yap M. Demographic and Socioeconomic Outcomes Across the Indigenous Australian Lifecourse: Evidence From the 2006 Census. Canberra: Centre of Aboriginal Economic Policy Research, Australian National University; 2010. . Contract No: 31. [Google Scholar]
- Closing the Gap Clearinghouse (AIHW, AIFS) 2012. What works to overcome Indigenous disadvantage: key learnings and gaps in the evidence 2010–11. Produced for the Closing the Gap Clearinghouse. Canberra: Australian Institute of Health and Welfare & Melbourne: Australian Institute of Family Studies.
- Sliwa K, Carrington M, Mayosi BM, Zigiriadis E, Mvungi R, Stewart S. Incidence and characteristics of newly diagnosed rheumatic heart disease in urban African adults: insights from the heart of Soweto study. Eur Heart J. 2010;31:719–727. doi: 10.1093/eurheartj/ehp530. [DOI] [PubMed] [Google Scholar]
- Milne RJ, Lennon D, Stewart JM, Vander Hoorn S, Scuffham PA. Mortality and hospitalisation costs of rheumatic fever and rheumatic heart disease in New Zealand. J Paediatr Child Health. 2012;48:692–697. doi: 10.1111/j.1440-1754.2012.02446.x. [DOI] [PubMed] [Google Scholar]
- Parks T, Kado J, Miller AE, Ward B, Heenan RC, Colquhoun SM, Tukana I, Steer A. Mortality amongst patients with rheumatic heart disease in Fiji: a national historic data-linkage cohort study. Glob Heart J. 2014;9:158. [Google Scholar]
- Lawrence JG, Carapetis JR, Griffiths K, Edwards K, Condon JR. Acute rheumatic fever and rheumatic heart disease incidence and progression in the Northern Territory of Australia, 1997 to 2010. Circulation. 2013;128:492–501. doi: 10.1161/CIRCULATIONAHA.113.001477. [DOI] [PubMed] [Google Scholar]
- Brown A, McDonald MI, Calma T. Rheumatic fever and social justice. Med J Aust. 2007;186:557–558. doi: 10.5694/j.1326-5377.2007.tb01052.x. [DOI] [PubMed] [Google Scholar]
- Australian Bureau of Statistics. Census Data Enhancement—Indigenous Mortality Quality Study 2006–07. Canberra: 2008. . Contract No: 4723. [Google Scholar]
- Australian Bureau of Statistics. Discussion Paper: Assessment of Methods for Developing Life Tables for Aboriginal and Torres Strait Islander Australians, 2006. Cat. no. 3302.0.55.002.
- Zhao YD, Dempsey K. Causes of inequality in life expectancy between Indigenous and non-Indigenous people in the Northern Territory, 1981–2000: a decomposition analysis. Med J Aust. 2006;184:490–494. doi: 10.5694/j.1326-5377.2006.tb00340.x. [DOI] [PubMed] [Google Scholar]
- Australian Bureau of Statistics. Australian Standard Geographical Classification (ASGC), July 2010. No. 1216.0. Available at: http://www.abs.gov.au/AUSSTATS/abs@.nsf/Lookup/1216.0Main+Features1July%202010.
- Colquhoun S, Karthikeyan G, Condon J, Mayosi B, Steer A, Parks T, Mensah G, Forouzanfar M, Ezzati M, Carapetis J. The global burden of rheumatic heart disease: the tip of the iceberg. Glob Heart J. 2014;9:158. [Google Scholar]


