Abstract
Background
We assessed high cholesterol (HC) awareness, treatment, and control rates among US Hispanic/Latino adults and describe factors associated with HC awareness and management.
Methods and Results
Baseline data (collected 2008–2011) from a multisite probability sample of Hispanic/Latino adults in the Hispanic Community Health Study/Study of Latinos (18 to 74 years old; N=16 207) were analyzed. HC was defined as low-density lipoprotein-cholesterol ≥130 mg/dL and/or total cholesterol ≥240 mg/dL or use of cholesterol-lowering medication. Among Hispanic/Latino adults with HC, almost half (49.3%) were not aware of their condition and only 29.5% were receiving treatment. Men had a higher HC prevalence than women (44.0% versus 40.5%) but a lower rate of treatment (28.1% versus 30.6%). Younger adults were significantly less likely to be HC aware compared to those who were older. Those with hypertension, diabetes, and high socioeconomic position were more likely to be HC aware. US-born Hispanic/Latino were more likely to be HC unaware than foreign-born Hispanics/Latinos, but longer US residency was significantly associated with being HC aware, treated, and controlled. Cholesterol control was achieved among 64.3% of those who were HC treated. However, younger adults, women, those with lower income, those uninsured, and more recent immigrants were less likely to be HC controlled. Individuals of Puerto Rican or Dominican background were most likely to be HC aware and treated, whereas those of Mexican or Central American background were least likely to be HC treated. Individuals of Cuban and South American background had the lowest rates of HC control, whereas Puerto Ricans had the highest.
Conclusions
Understanding gaps in HC awareness, treatment, and control among US Hispanic/Latino adults can help inform physicians and policymakers to improve disease management and patient education programs.
Keywords: cholesterol, epidemiology, health disparities, high-risk populations
According to 2005–2008 National Health and Nutrition Examination Survey data, Mexican Americans ages 20 and older, have a high prevalence (between 30% and 50%) of high cholesterol (HC) defined by total cholesterol (TC) and low-density lipoprotein cholesterol (LDL-C) levels.1,2 The 1982–1984 Hispanic Health and Nutrition Examination Survey demonstrated variation in HC prevalence among the 3 Hispanic background groups studied—Mexicans, Cubans, and Puerto Ricans.3 Substantially lower rates of HC screening, awareness, treatment, and control have been described among Hispanics compared to non-Hispanic whites.4–7 Unfortunately, Hispanic cohorts in these prior studies were relatively small, lacked adequate representation of diverse Hispanic background groups for comparisons, and were not necessarily representative of nor generalizable to the Hispanic population. Fifty-two million Hispanics residing in the United States represent the largest and fastest-growing racial/ethnic minority group. Given the impact of HC on cardiovascular disease outcomes, further knowledge of HC awareness, treatment, and control rates among Hispanics could inform public health strategies and facilitate prevention guidelines.
The landmark Hispanic Community Health Study/Study of Latinos (HCHS/SOL) is the largest and most comprehensive multicenter community-based cohort study of US Hispanic adults. We assessed HC awareness, treatment, and control prevalence rates among US Hispanics in the baseline HCHS/SOL and evaluated whether HC awareness, treatment, and control patterns vary according to Hispanic background groups. Lastly, we compared rates of awareness, treatment, and control of HC according to demographic, clinical, acculturation, and socioeconomic factors.
Methods
Study Population
The HCHS/SOL is a multicenter epidemiologic study of US Hispanic/Latino adults living in 4 specific communities in the United States. Participants were examined at 4 field centers affiliated with San Diego State University, Northwestern University in Chicago, Albert Einstein College of Medicine in the Bronx area of New York, and the University of Miami. The University of North Carolina serves as the coordinating center. Details of the sampling methods and design have been published.8,9
HCHS/SOL recruited a total of 16 415 participants (9835 women and 6580 men) aged 18 to 74 years at the time of screening from June 2008 to July 2011. The HCHS/SOL sampling design ensured significant representation of major US Hispanic/Latino background groups including Mexicans, Puerto Ricans, Cubans, Central Americans, Dominicans, and South Americans (by self-reported national origin). Participants were recruited through a stratified multistage area probability sample design from communities surrounding the 4 field centers listed above. Eligibility criteria included Hispanic/Latino ethnicity, ability to travel to the local field center, English or Spanish language proficiency, and no plans to move from the area. There were no other exclusion criteria based upon health status, comorbidities, legal residency, or other factors, making HCHS/SOL representative of the noninstitutionalized Hispanic/Latino adult population at these 4 major US communities.
HCHS/SOL procedures and examination during the baseline visit have been previously described.10,11 Information pertaining to demographic characteristics and medical history was obtained using interviewer-administered questionnaires by trained staff. Medication use was assessed by participants bringing all medications and supplements used during the last 4 weeks; these were reviewed and coded by clinic staff. Diabetes was defined based on American Diabetes Association definition12 using 1 or more of the following criteria: (1) fasting serum glucose ≥126 mg/dL, (2) oral glucose tolerance test ≥200 mg/dL, (3) self-reported diabetes, (4) Hb A1C ≥6.5%, or (5) taking antidiabetic medication or insulin. Trained and certified clinic staff obtained blood samples, anthropometric and blood pressure measurements on all HCHS/SOL participants. Height was measured to the nearest 0.1 cm and weight was measured to the nearest 0.1 kg with the use of a balanced scale. Body mass index was calculated as weight in kilograms divided by height in meters squared. After a 5-minute rest, blood pressure was measured 3 times at 1-minute intervals using an automated oscillometric device with the participant in a seated position. The average of the second and third blood pressure measurements was used for this analysis. Hypertension was defined as a systolic blood pressure of 140 mm Hg or higher, diastolic blood pressure of 90 mm Hg or higher, or on antihypertensive treatment.
Blood lipids and lipoproteins were measured on samples obtained after an overnight fast. Specimens were stored at −20°C and shipped weekly to the Lipoprotein Analytical Laboratory at the HCHS/SOL Central Lab at the University of Minnesota Medical Center. This laboratory participates in the Lipid Standardization Program of the Centers for Disease Control and Prevention. TC was measured using a cholesterol oxidase enzymatic method and high-density lipoprotein cholesterol with a direct magnesium/dextran sulfate method. Triglyceride levels were measured in EDTA plasma with the use of TG GB reagent (Roche Diagnostics) on a centrifugal analyzer. High-density lipoprotein cholesterol was measured with an enzymatic method after precipitation of non–high-density lipoprotein cholesterol with heparin and magnesium dextran sulfate. Low-density lipoprotein cholesterol (LDL-C) was calculated using the Friedewald equation.13
Laboratory measurements of TC and LDL-C were obtained for all participants at baseline. Participants were classified as having prevalent HC if they were currently using of cholesterol-lowering medication or if their LDL-C and/or TC exceeded risk thresholds defined by the National Cholesterol Education Program/Adult Treatment Panel III (NCEP/ATP III),14,15 as LDL-C ≥130 mg/dL and/or TC ≥240 mg/dL. NCEP/ATP III defined individuals with normal LDL-C levels as those with <130 mg/dL. Consequently, prevalent HC includes participants who were treated with a lipid-lowering drug and those who qualified for treatment according to above thresholds but were not treated. Awareness of HC was defined as an affirmative response to the question, “Have you ever been told by a doctor or other healthcare professional that you had high cholesterol?” Treatment of HC was defined as a positive response to the question, “Because of your high cholesterol, are you now taking prescribed medicine?” This was verified using information collected on medications brought in by participants. Control of HC was defined as meeting NCEP/ATP III guideline levels for TC and LDL-C among those who were HC treated.
Socioeconomic position (SEP) was assessed using years of educational attainment defined as highest degree or level of school completed (less than high school; completed high school or high school equivalent; and education beyond high school) and household income level, classified into groups (<$20 000; $20 000 to $39 999; $40 000 to $75 000 and >$75 000). Acculturation was defined using multiple proxy indicators, including nativity, duration of residence in the United States, and language preference based on language used for the interviews (English versus Spanish). Greater years of residence in the United States and English language preference indicated higher levels of acculturation.
Statistical Analysis
We applied survey methods using sampling weights to provide weighted frequencies of descriptive variables and population estimates of HC prevalence rates, as well as HC awareness, treatment, and control rates in the HCHS/SOL target population. Descriptive characteristics are age-standardized to the Census 2010 US population. We compared rates of awareness, treatment, and control of HC by demographic factors, anthropometric measurements, lifestyle factors, and clinical and sociocultural profiles. Continuous variables were compared using regression analysis and categorical variables were compared using Rao–Scott χ2. We used Rao–Scott χ2 analysis to explore whether the prevalence of established HC awareness, treatment, and control varied significantly among Hispanic/Latino groups and across categories of SEP and acculturation. To assess whether health insurance status confounds the association of SEP on HC awareness, treatment, and control, we constructed logistic regression models controlling for the effect of health insurance. To examine whether interrelations exists between acculturative factors (language, nativity, and length of time in the United States) and HC status, we performed additional sensitivity analysis looking at the association of time in the United States and HC control stratified by language preference and nativity, as well as looking at the inverse association of language and HC awareness stratified by time in the United States and nativity.
The above analyses were performed with SAS version 9.3 (SAS Institute Inc, Cary, NC) and SUDAAN release 10.0.0 (RTI). All analyses were weighted to adjust for sampling probability and nonresponse, to make the estimates applicable to the target population from which the HCHS/SOL sample was drawn in accordance with guidelines suggested by the HCHS/SOL Steering and Data Analysis Committees.
Results
Of 39 384 individuals who were screened, selected, and met eligibility criteria, 41.7% were enrolled, representing 16 415 persons from 9872 households. Baseline demographics of the HCHS/SOL population have been previously described.10 In the target population, the prevalence of hypertension was 25%; 40% were obese and 17% had diabetes. Mean levels of TC, non-high-density lipoprotein cholesterol, and LDL-C were 196.0, 145.8, and 120.9 mg/dL, respectively. Forty-eight percent of the population had no health insurance coverage. Among those insured, most were at least partially covered by public health insurance (Medicaid and/or Medicare). Seventeen percent of those ages 65 years and older were uninsured compared to 45% to 58% of those in younger age groups (Table1). There was differential health insurance coverage across Hispanic background group ranging from 33% to 80%; it was highest among Puerto Ricans and lowest among South Americans. Acculturation factors also varied, preferential English being highest among Puerto Ricans and lowest among Cubans; time residing in the mainland United States being highest among Puerto Ricans and lowest among Cubans. Health Insurance coverage was more common among preferential English speakers; among those participants residing in the mainland US >10 years and among the US born (Table2).
Table 1.
Prevalence of High Cholesterol* Among Hispanics According to Descriptive Characteristics
| Characteristic | Sample Size† (N) | High Cholesterol‡ (N=7837) | P-Value | |
|---|---|---|---|---|
| Age (y) | ||||
| 18 to 44 | 9815 | 2000 | 29% | <0.001 |
| 45 to 64 | 5202 | 4905 | 59% | |
| 65+ | 1401 | 932 | 71% | |
| Hispanic/Latino background group | 0.126 | |||
| Dominican | 1472 | 690 | 43% | |
| Central American | 1731 | 798 | 46% | |
| Cuban | 2347 | 1304 | 48% | |
| Mexican | 6468 | 2995 | 45% | |
| Puerto Rican | 2727 | 1300 | 43% | |
| South American | 1071 | 520 | 45% | |
| Mixed/other | 503 | 197 | 48% | |
| Gender | ||||
| Female | 9829 | 4652 | 43% | ≤0.001 |
| Male | 6577 | 3185 | 47% | |
| Hypertension | ||||
| Yes | 4460 | 2899 | 53% | <0.001 |
| No | 11 944 | 4938 | 43% | |
| BMI, kg/m2 | ||||
| <25 | 3320 | 1162 | 38% | <0.001 |
| 25 to 29.9 | 6113 | 3153 | 47% | |
| 30+ | 6902 | 3496 | 48% | |
| Diabetes | ||||
| Yes | 3210 | 2146 | 58% | <0.001 |
| No | 13 174 | 5691 | 43% | |
| Prevalent CHD | ||||
| Yes | 856 | 528 | 44% | 0.561 |
| No | 15 473 | 7283 | 45% | |
BMI indicates body mass index; CHD, coronary heart disease; HCHS/SOL, Hispanic Community Health Study/Study of Latinos; LDL, low-density lipoprotein; TC, total cholesterol.
Defined as LDL ≥130, TC ≥240, or on cholesterol medications.
N’s presented are unweighted counts of total participants in the HCHS/SOL with respective characteristic.
N’s presented are unweighted counts of participants with high cholesterol. Percentages are weighted row percentages and age-adjusted to a standardized population using 2010 US Census.
Table 2.
Differential Insurance Status and Measures of Acculturation Across Hispanic Background Group*
| Dominican | Central American | Cuban | Mexican | Puerto Rican | South American | |
|---|---|---|---|---|---|---|
| Health insurance coverage | 511 (71.5%) | 267 (33.0%) | 535 (45.2%) | 1385 (43.6%) | 1075 (80.4%) | 197 (42.9%) |
| Acculturation factors | ||||||
| Preferential Spanish speaker | 54 (12.0%) | 37 (8.8%) | 45 (4.3%) | 355 (15.9%) | 572 (51.5%) | 25 (5.4%) |
| Years in the US ≥10 | 554 (80.3%) | 580 (68.4%) | 690 (52.2%) | 2484 (78.7%) | 1261 (95.4%) | 371 (65.3%) |
| US born | 26 (7.5%) | 17 (3.7%) | 35 (3.7%) | 322 (15.4%) | 416 (37.8%) | 13 (3.1%) |
N’s presented are unweighted counts of total participants in the Hispanic Community Health Study/Study of Latinos; weighted row percentages.
The overall prevalence of HC was 45%; 15% had a high TC, 35% had elevated non-high-density lipoprotein cholesterol levels, and 37% had elevated LDL-C levels. HC was seen in significantly higher proportions among males and those in older age groups. In addition, proportions of those with HC were significantly higher among those with concomitant hypertension, diabetes, and those who were overweight/obese compared to those without. Proportions of those with HC were not significantly different across the Hispanic/Latino background groups or among those with or without self-reported coronary heart disease (Table1).
HC Awareness
HC awareness was defined as ever being told by a health professional of having HC. Among those with HC, almost half (49%) were not aware of their condition. Among those with LDL-C ≥190 mg/dL, only 63% were HC aware. A significantly higher proportion of Hispanic/Latinos were HC aware in the older age groups. Despite a higher prevalence of HC in men, rates of HC awareness were higher among women than men across all age groups, but this difference was most pronounced among those middle-aged and older (Figure1A). Significantly higher proportions of those who have hypertension, higher body mass index, or diabetes were HC aware. US-born Hispanic/Latinos had significantly lower rates of being HC aware compared to those who were foreign born. A proportion of those who were HC aware was significantly higher among preferential Spanish speakers compared to those who preferred English. The lowest and highest SEP categories (by educational attainment or income) had the highest rates of HC awareness. Those with insurance coverage had significantly higher rates of being HC aware compared to those who were insured (Table3). Logistic regression models controlling for health insurance to address confounding did not attenuate the effect of SEP (either income or education) on HC awareness. Individuals of Central American and Cuban heritage had the lowest rates of being HC aware, while those of Puerto Rican and Dominican backgrounds were more likely to be aware than other groups (Figure2).
Figure 1.
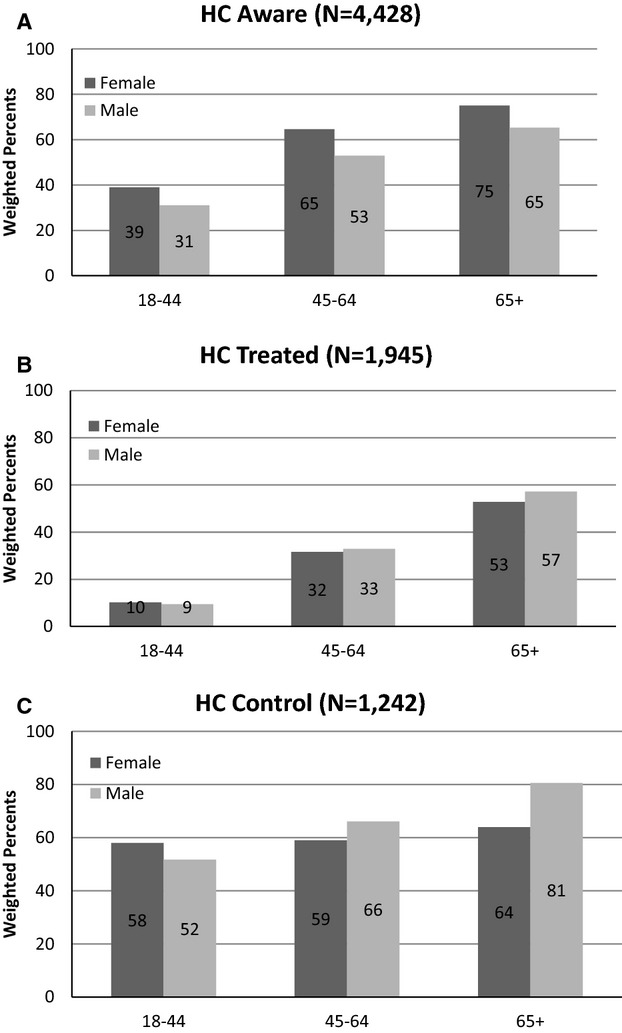
Percentage of participants (stratified by age and sex) who were (A) HC aware; (B) HC treated; and (C) HC controlled. HC indicates high cholesterol, defined as treated with a lipid-lowering drug or those who qualified for treatment according to LDL-C ≥130 mg/dL and/or TC ≥240 mg/dL but were not treated; LDL-C, low-density lipoprotein cholesterol; TC, total cholesterol.
Table 3.
High Cholesterol Awareness, Treatment, and Control Rates According to Descriptive Characteristics*
| Awareness | P- Value | Treatment | P- Value | Control | P- Value | ||||
|---|---|---|---|---|---|---|---|---|---|
| Yes (n) | % | Yes (n) | % | Yes (n) | % | ||||
| Mean age (SE) | 52.1 (0.35) | <0.001 | 58.7 (0.37) | <0.001 | 59.4 (0.41) | 0.003 | |||
| Men | 1564 | 43 | <0.001 | 685 | 28 | 0.12 | 470 | 69 | 0.009 |
| Women | 2864 | 58 | 1260 | 31 | 772 | 61 | |||
| Hypertension | 2022 | 66 | <0.001 | 1276 | 49 | <0.001 | 837 | 65 | 0.49 |
| No hypertension | 2406 | 43 | 669 | 16 | 405 | 63 | |||
| BMI | |||||||||
| <25 | 582 | 46 | 0.02 | 207 | 24 | 0.003 | 128 | 61 | 0.64 |
| 25 to 29.9 | 1733 | 51 | 728 | 29 | 451 | 64 | |||
| 30+ | 2096 | 53 | 996 | 32 | 655 | 66 | |||
| Diabetes | 1572 | 71 | <0.001 | 1059 | 54 | <0.001 | 742 | 70 | <0.001 |
| No diabetes | 2856 | 45 | 886 | 19 | 500 | 57 | |||
| Education | |||||||||
| <High school | 1862 | 55 | <0.001 | 956 | 39 | <0.001 | 623 | 66 | 0.31 |
| High school | 946 | 45 | 377 | 26 | 240 | 65 | |||
| >High school | 1524 | 50 | 565 | 24 | 349 | 61 | |||
| Income | |||||||||
| <20 K | 2059 | 53 | 0.006 | 970 | 33 | <0.001 | 628 | 66 | 0.002 |
| 20 to 40 K | 1268 | 46 | 504 | 26 | 297 | 57 | |||
| 40 to 75 K | 531 | 50 | 203 | 24 | 147 | 74 | |||
| >75 K | 179 | 55 | 79 | 28 | 55 | 76 | |||
| Health insurance | |||||||||
| Yes | 2710 | 61 | <0.001 | 1483 | 41 | <0.001 | 1002 | 68 | <0.001 |
| No | 1654 | 40 | 430 | 13 | 220 | 49 | |||
| Language | |||||||||
| Spanish | 3802 | 52 | 0.02 | 1649 | 30 | 0.17 | 1032 | 64 | 0.28 |
| English | 626 | 46 | 296 | 27 | 210 | 68 | |||
| Years in US (foreign born) | |||||||||
| <10 years | 784 | 43 | <0.001 | 226 | 17 | <0.001 | 119 | 53 | <0.001 |
| 10+ years | 3184 | 57 | 1518 | 36 | 988 | 67 | |||
| US born | |||||||||
| Yes | 447 | 41 | <0.001 | 190 | 24 | 0.007 | 128 | 62 | 0.59 |
| No | 3978 | 52 | 1748 | 30 | 1109 | 65 | |||
BMI indicates body mass index; HCHS/SOL, Hispanic Community Health Study/Study of Latinos.
N’s presented are unweighted counts of total participants in the HCHS/SOL; percentages are weighted row percentages.
Figure 2.
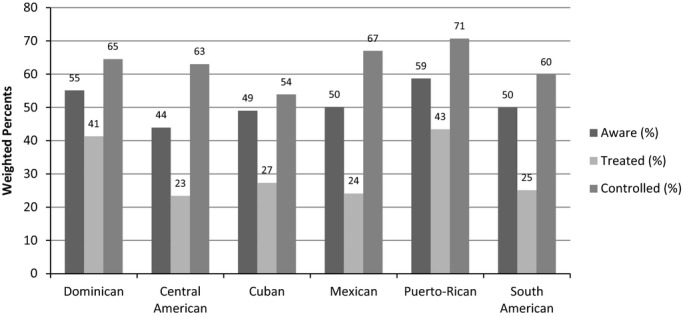
High cholesterol awareness, treatment, and control rates according to Hispanic background group.
HC Treated
Treatment of HC was defined as taking prescribed cholesterol medicine. Among those who either had laboratory values indicating HC or had been told by a health professional that they had HC, less than a third (30%) were HC treated. Among those with an LDL-C ≥190 mg/dL, only 14% were HC treated. Although the likelihood of being HC treated increased with age, only 32% and 54% of middle-aged and older Hispanic/Latinos, respectively, with HC were actually being treated. A larger proportion (>90%) of HC-eligible Hispanic/Latinos <45 years of age were not receiving HC treatment. A trend was observed where rates of HC treatment were higher among Hispanic/Latino men versus women in the older age groups, particularly among those 65+ years of age (Figure1B). Those with diabetes, the lowest SEP (by either education or income), and insurance coverage were more likely to be among those HC treated. Controlling for health insurance did not attenuate the effect of SEP on HC treatment. US-born Hispanic/Latinos had lower rates of being HC treated than those who were foreign born. Among the foreign born, rates of being HC treated increased with longer duration of US residence (Table2). Higher proportions of individuals of Dominican or Puerto Rican background were receiving treatment for HC, whereas Hispanic/Latinos of Mexican or Central American background had lower rates of treatment (Figure2).
HC Control
HC control was defined as meeting NCEP/ATP III guidelines for TC and LDL-C. Among those with HC using cholesterol-lowering medications, 64.3% were HC controlled. Older Hispanic/Latinos tended to have a higher rate of being HC controlled than those who were younger. Women had lower rates of being HC controlled than men. This sex difference persisted across all ages but was most pronounced among those 65 years and older (Figure1C). The presence of diabetes, higher income levels, and insurance coverage was associated with being HC controlled. Controlling for health insurance did attenuate the effect of SEP on HC control. Those with greater duration of US residence had significantly higher rates of HC control than more recent immigrants (Table2). Rates of adequate HC control varied significantly across Hispanic/Latinos background groups ranging from 54% to 71%, with Cubans and South Americans having the lowest HC control rates, whereas Puerto Ricans had the highest (Figure2).
Discussion
To our knowledge, there have been no previous studies of diverse Hispanic/Latino representation comparing HC awareness, treatment, and control among diverse Hispanic/Latino background groups. Our findings show that HC is highly prevalent among US Hispanic/Latino adults and that less than half of those with HC were aware of their condition (ie, reported being told by a doctor or health professional that their cholesterol level was high). Moreover, less than a third of those with HC were being treated. Among those receiving treatment, only 64% had cholesterol concentrations that were adequately controlled. Gender disparities were observed in that men had higher HC prevalence rates than women but were less likely to be HC aware. Although Hispanic/Latino women with HC had similar rates of HC treatment compared to men, women were less likely to be HC controlled. Hispanic/Latinos ages 18 to 44 years with HC were more likely to be unaware of having HC and to be untreated for this condition compared to those ages 45 and older. HC treatment rates and optimal cholesterol goal attainment rates for all Hispanic/Latino background groups were suboptimal.
Our study found that among Hispanic/Latino adults, prevalence of HC was higher among those with hypertension or diabetes, and the presence of these comorbid conditions increased the likelihood of being HC aware, treated, and controlled. Both diabetes and hypertension are associated with substantially increased risk of developing coronary heart disease.16 Thus, it is encouraging that among Hispanic/Latinos with these comorbid conditions, rates of HC treatment and control were among the highest. The presence of more comorbidities probably increases the likelihood of having received the attention of the healthcare system and being HC treated. However, it creates a gap with regard to primary prevention, making those with HC and fewer comorbidities less likely to be among those HC aware, treated, or controlled. Furthermore, our findings showed that even among Hispanic/Latino individuals with these comorbid conditions, only slightly more than half of those with diabetes and two thirds of those with hypertension were HC aware.
Several studies have examined awareness, treatment, and control of HC in the United States (Table4) but most have focused on non-Hispanic whites or blacks. The Cardiovascular Health Study18 found that among adults ages 65 to 75 years, HC treatment was 8.1% in men and 10.0% in women in 1995–1996. The Minnesota Heart Survey19 showed that among non-Hispanic whites in 2002, 55% were HC unaware, and 33% were aware and untreated. The Genoa Study20 looked at 2 US communities of non-Hispanic/Latino whites and blacks and found that fewer than 1 in 3 of these adults were HC treated and fewer than half of those treated had achieved recommended goals. Studies that included Hispanic/Latinos primarily involved Mexican heritage participants or considered Hispanic/Latinos as a single aggregate group. Data from the National Health and Nutrition Examination Survey demonstrated substantially lower rates of awareness, diagnosis, treatment, and control among Mexican Americans compared to non-Hispanic whites.6,7 Less than half of National Health and Nutrition Examination Survey Mexican Americans had been screened for HC compared to 65.2% and 57.7% of non-Hispanic whites and non-Hispanic blacks, respectively.6 In the Multiethnic Study of Atherosclerosis,5 Hispanic participants were significantly less likely to be HC treated and controlled than non-Hispanic whites; however, these differences were attenuated by adjustment for healthcare access variables. We also noted HC gender disparities in our study. There is prior data suggesting less intensive cholesterol management in women than men, resulting in a similar disparity in cholesterol control24,25; however data across racial/ethnic groups are somewhat limited. In National Health and Nutrition Examination Survey 2005–2006, women were less likely to be HC controlled than men (56.9% versus 72.1%), and this trend was present across non-Hispanic whites, non-Hispanic blacks, and Mexican Americans (although seemingly most disparate among non-Hispanic blacks).6
Table 4.
Prior Studies of High Cholesterol Awareness, Treatment, and Control in the United States
| Reference | Year | Sample Size/Population | Age Range/Mean | Major Findings |
|---|---|---|---|---|
| Studies that did not include Hispanics | ||||
| The Atherosclerosis Risk in Communities study17 | 1995 | African Americans and Caucasians | 15 739 individuals aged 45 to 64 years | 25% of African American men and 27% of African American women with hypercholesterolemia were aware of their condition; of these, only 20% and 21%, respectively, were undergoing treatment, and only 32% and 45%, respectively, achieved treatment goals |
| Cardiovascular Health Study18 | 1995–1996 | African Americans and whites | 65 to 75 | The prevalence of cholesterol-lowering drug use in 1995–1996 was 8.1% among men and 10.0% among women |
| Minnesota Heart Survey19 | 2000–2002 | Whites | 35 to 74 | The mean prevalence of hypercholesterolemia in 2000 to 2002 was 54.9% for men and 46.5% for women. More than half of those at borderline-high risk remain unaware of their condition |
| Genoa Study20 | 2004 | Non-Hispanic hypertensive blacks and whites | Women, 59.8±9.4 vs 57.8±10.0; and men, 60.8±9.5 vs 57.4±10.1 years | Dyslipidemia prevalence ranges 50% to 78% and more prevalent among whites than blacks. Less than one third are treated (treatment was more common among whites than blacks), and fewer than half of those treated achieve goal (control was seen more among black men vs white men) |
| Studies that did include Hispanics | ||||
| MESA5 | 2000 | Non-Hispanic whites, blacks, Chinese, and Hispanic Americans | 45 to 84 | Hispanic Americans had prevalence of dyslipidemia that was comparable to that of non-Hispanic whites but were less likely to be treated and controlled |
| NHANES6 | 1999–2006 | Non-Hispanic whites, African Americans, and Mexican Americans | ≥20 years | Lower rates of having cholesterol check, reporting being told about hypercholesterolemia; hypercholesterolemia treatment and control among Mexican Americans than whites |
| NHANES7 | 1988–1994 | Non-Hispanic whites, African Americans, and Mexican Americans | ≥25 years | Mexican Americans were less likely to report cholesterol screening than whites. Even when identified as having high cholesterol, Mexican Americans were less likely to be on cholesterol-lowering agents |
| NHANES23 | 1999–2000 to 2009–2010 | Non-Hispanic whites, African Americans, and Mexican Americans | ≥25 years | Prevalence of high cholesterol did not change from 1999–2000 (37.2%) to 2009–2010 (37.8%). Awareness increased from 48.9% in 1999–2000 to 61.5% in 2009–2010 (61.5%). Treatment increased from 41.3% in 1999–2000 to 70.0% in 2009–2010. The percentage with controlled cholesterol increased from 45.0% in 1999–2000 to 63.6% by 2009–2010 |
MESA indicates Multi-Ethnic Study of Atherosclerosis; NHANES, National Health and Nutrition Examination Survey.
Our study illustrates that among Hispanic/Latinos who are HC treated, the rates of HC control are fairly high (ranging from 54% to 71% among the various Hispanic/Latino background groups). However, a sizeable gap between HC awareness and HC treatment exists. Studies suggest that gaps in HC treatment and control are often related to gaps in availability of, access to, or continuity of health care.26–28 The Affordable Care Act is intended to reduce some of these gaps29 by both increasing insurance coverage among the nonelderly US population and by providing coverage for cholesterol screening with no cost-sharing. However, access to care alone may not resolve gaps in HC treatment and control completely. Other factors that may affect HC treatment and control in the US Hispanic/Latino population include primordial risks (eg, diet), language barriers, poor patient–provider communication, and insufficient treatment (eg, provider clinical inertia) and/or patient medication adherence.30,31 Lower out-of-pocket costs, improved patient–provider communication, and simplification of the drug regimen generally are associated with better adherence.32 The fact that there is a large gap between HC awareness and subsequent treatment and control underscores the need to go beyond screening programs and health fairs to improve the health of the Hispanic/Latino population.
Those with the lowest SEP (by household income), while more likely to be HC aware, had a markedly lower prevalence of HC control. Furthermore, the lowest and highest SEP groups (by educational attainment or income) had the highest rates of HC awareness, suggesting a disparity gap among “working poor” and “middle-class” Hispanic/Latinos. It may be that Hispanic/Latinos in the lowest and highest SEP categories are more likely to have health insurance, due to Medicaid for those with low SEP and more wealth resources for those with higher SEP, respectively. Hispanic/Latinos in the middle SEP group, however, may be more likely to fall through gaps. Higher rates of HC awareness, treatment, and control were related to having health insurance. Controlling for health insurance did not remove the effect of SEP on HC awareness and treatment but did remove the effect of SEP on HC control. Compared with non-Hispanic whites, Hispanics are less likely to have health insurance or a regular source of care, and less likely to receive preventive services.33 Increased acculturation (by nativity and preferential English speaking) was associated with decreased HC awareness. However, among immigrants, increasing years in the United States did increase the likelihood of HC treatment and control, perhaps due to increasing ability to navigate the US healthcare system and establishment a social support system to do so. This highlights a complicated relationship of acculturation and health. Being a more recent immigrant was a more dominant acculturative factor in determining HC awareness than being able to dominate the English language. Similarly, increasing time in the United States portends a greater likelihood of HC control among those who were less acculturated (preferential Spanish speakers and those foreign born) but was not a factor among the more acculturated (preferential English speakers and those US born). This acculturation–health relationship differential effect was also seen in a prior study.34
Our findings of variation in HC awareness, treatment, and control across the different background groups provide further evidence of the complexity and heterogeneity of the Hispanic/Latino population; thus, HC awareness, treatment, or control rates for 1 group cannot be extrapolated to represent all Hispanic/Latinos. Hispanic/Latinos of Puerto Rican and Dominican background seem to fare better with regard to higher rates of HC awareness, treatment, and control whereas those of Mexican, Cuban, and Central and South American backgrounds seem to fare worse. US Hispanic/Latinos have differential regional patterns of settlement in the United States, with Mexicans concentrated in the Southwest, Cubans in the Southeast, Central/South Americans in the Midwest and South, and Puerto Ricans and Dominicans in the Northeast. Thus, some of these differences in HC treatment and control observed among Hispanic/Latino background groups may be geographical in nature, given differences in medical coverage across state lines. State laws governing medical coverage for low-income individuals vary and these differences are likely to worsen, with some states having declined to adopt the Medicaid expansion provisions of the Affordable Care Act.
Our results should be interpreted in light of several limitations. While HCHS/SOL is the largest epidemiologic study of diverse community-dwelling US Hispanic/Latinos, it was not designed to be nationally representative but is representative of the communities sampled; thus, our findings may not be generalizable to all US Hispanic/Latinos. Our findings may underestimate the prevalence of HC, since older persons residing in nursing homes or other institutions (with potentially a higher prevalence of age-related HC) were not included in the HCHS/SOL. Data regarding awareness was based on self-report and could be subject to recall bias. The NCEP/ATP III report identifies concentrations of LDL-C rather than TC as the primary target of treatment. However, insights about TC are still of value and participants may not have been able to distinguish between TC and LDL-C when asked whether they had their cholesterol checked and/or had been told by a physician that their cholesterol is high. Our definition of treatment included coding of medications reviewed by study staff; thus, our measure is more robust than that of several prior studies of HC treatment that used medication self-report only. This study was initiated, laboratory samples were collected, and management strategies examined under the older NCEP/ATP III guidelines, which focused on target levels rather than atherosclerotic risk to determine who is treated. It is likely that under the new, broader American Heart Association/American College of Cardiology cholesterol treatment guidelines,35 an even larger number of Hispanic/Latinos will be undertreated, further highlighting this health disparity.
In conclusion, we found high rates of HC and a very low prevalence of HC awareness among Hispanic/Latino adults and a major gap between HC awareness and HC treatment that bodes poorly for the public health of this large and growing segment of the US population. Not surprisingly, our observational data indicated that once treated, achievement of optimal HC control is possible among Hispanic/Latinos. Complementary and targeted public health programs to raise HC awareness and increase the proportion of Hispanic/Latinos receiving HC treatment and achieving HC control are needed to reduce healthcare disparities in this population. Our findings fill major gaps in understanding HC awareness, treatment, and control among US Hispanic/Latino adults, and will help guide and inform physicians and policymakers toward improving patient education programs and disease management.
Acknowledgments
The authors thank the staff and participants of the Hispanic Community Health Study/Study of Latinos for their important contributions.
Sources of Funding
The Hispanic Community Health Study/Study of Latinos was carried out as a collaborative study supported by contracts from the National Heart, Lung, and Blood Institute (NHLBI) to the University of North Carolina (N01-HC65233), University of Miami (N01-HC65234), Albert Einstein College of Medicine (N01-HC65235), Northwestern University (N01-HC65236), and San Diego State University (N01-HC65237). This study was partially supported by NHLBI grant R01 HL104199 (Epidemiologic Determinants of Cardiac Structure and Function Among Hispanic/Latinos: Carlos J. Rodriguez, MD, MPH Principal Investigator).
Disclosures
Dr Rodriguez has received consulting agreement/honorariums from Alnylam and Amgen Research Support from the National Institutes of Health and the American Heart Association.
References
- Mozaffarian D, Benjamin EJ, Go AS, Arnett DK, Blaha MJ, Cushman M, de Ferranti S, Després J-P, Fullerton HJ, Howard VJ, Huffman MD, Judd SE, Kissela BM, Lackland DT, Lichtman JH, Lisabeth LD, Liu S, Mackey RH, Matchar DB, McGuire DK, Mohler ER, Moy CS, Muntner P, Mussolino ME, Nasir K, Neumar RW, Nichol G, Palaniappan L, Pandey DK, Reeves MJ, Rodriguez CJ, Sorlie PD, Stein J, Towfighi A, Turan TN, Virani SS, Willey JZ, Woo D, Yeh RW, Turner MB. Heart disease and stroke statistics—2015 update: a report from the American Heart Association. Circulation. 2015;131:e29–e322. doi: 10.1161/CIR.0000000000000152. [DOI] [PubMed] [Google Scholar]
- Rodriguez CJ, Brenes J. Hypercholesterolemia in minorities. In: Chavez-Tapia NC, Uribe M, editors. Topics in Prevalent Diseases: A Minority’s Perspective. Hauppauge, NY: Nova Science Publishers; 2008. pp. 125–136. [Google Scholar]
- Crespo C, Loria C, Burt V. Hypertension and other cardiovascular disease risk factors among Mexican Americans, Cuban Americans, and Puerto Ricans from the Hispanic Health and Nutrition Examination Survey. Public Health Rep. 1996;111(suppl 2):7–10. [PMC free article] [PubMed] [Google Scholar]
- Jurkowski JM, Johnson TP. Acculturation and cardiovascular disease screening practices among Mexican Americans living in Chicago. Ethn Dis. 2005;15:411–417. [PubMed] [Google Scholar]
- Goff DC, Jr, Bertoni AG, Kramer H, Bonds D, Blumenthal RS, Tsai MY, Psaty BM. Dyslipidemia prevalence, treatment, and control in the Multi-Ethnic Study of Atherosclerosis (MESA): gender, ethnicity, and coronary artery calcium. Circulation. 2006;113:647–656. doi: 10.1161/CIRCULATIONAHA.105.552737. [DOI] [PubMed] [Google Scholar]
- Ford ES, Li C, Pearson WS, Zhao G, Mokdad AH. Trends in hypercholesterolemia, treatment and control among United States adults. Int J Cardiol. 2010;140:226–235. doi: 10.1016/j.ijcard.2008.11.033. [DOI] [PubMed] [Google Scholar]
- Nelson K, Norris K, Mangione CM. Disparities in the diagnosis and pharmacologic treatment of high serum cholesterol by race and ethnicity: data from the third National Health and Nutrition Examination Survey. Arch Intern Med. 2002;162:929–935. doi: 10.1001/archinte.162.8.929. [DOI] [PubMed] [Google Scholar]
- Sorlie PD, Aviles-Santa LM, Wassertheil-Smoller S, Kaplan RC, Daviglus ML, Giachello AL, Schneiderman N, Raij L, Talavera G, Allison M, Lavange L, Chambless LE, Heiss G. Design and implementation of the Hispanic Community Health Study/Study of Latinos. Ann Epidemiol. 2010;20:629–641. doi: 10.1016/j.annepidem.2010.03.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lavange LM, Kalsbeek WD, Sorlie PD, Aviles-Santa LM, Kaplan RC, Barnhart J, Liu K, Giachello A, Lee DJ, Ryan J, Criqui MH, Elder JP. Sample design and cohort selection in the Hispanic Community Health Study/Study of Latinos. Ann Epidemiol. 2010;20:642–649. doi: 10.1016/j.annepidem.2010.05.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Daviglus ML, Talavera GA, Aviles-Santa ML, Allison M, Cai J, Criqui MH, Gellman M, Giachello AL, Gouskova N, Kaplan RC, LaVange L, Penedo F, Perreira K, Pirzada A, Schneiderman N, Wassertheil-Smoller S, Sorlie PD, Stamler J. Prevalence of major cardiovascular risk factors and cardiovascular diseases among Hispanic/Latino individuals of diverse backgrounds in the United States. JAMA. 2012;308:1775–1784. doi: 10.1001/jama.2012.14517. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sorlie PD, Allison MA, Aviles-Santa ML, Cai J, Daviglus ML, Howard AG, Kaplan R, Lavange LM, Raij L, Schneiderman N, Wassertheil-Smoller S, Talavera GA. Prevalence of hypertension, awareness, treatment, and control in the Hispanic Community Health Study/Study of Latinos. Am J Hypertens. 2014;27:793–800. doi: 10.1093/ajh/hpu003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- American Diabetes A. Diagnosis and classification of diabetes mellitus. Diabetes Care. 2010;33(suppl 1):S62–S69. doi: 10.2337/dc10-S062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Friedewald WT, Levy RI, Fredrickson DS. Estimation of the concentration of low-density lipoprotein cholesterol in plasma, without use of the preparative ultracentrifuge. Clin Chem. 1972;18:499–502. [PubMed] [Google Scholar]
- Executive summary of the third report of the National Cholesterol Education Program (NCEP) expert panel on detection, evaluation, and treatment of high blood cholesterol in adults (Adult Treatment Panel III) JAMA. 2001;285:2486–2497. doi: 10.1001/jama.285.19.2486. [DOI] [PubMed] [Google Scholar]
- Grundy SM, Cleeman JI, Merz CN, Brewer HB, Jr, Clark LT, Hunninghake DB, Pasternak RC, Smith SC, Jr, Stone NJ National Heart L, Blood I, American College of Cardiology F, American Heart A. Implications of recent clinical trials for the National Cholesterol Education Program Adult Treatment Panel III guidelines. Circulation. 2004;110:227–239. doi: 10.1161/01.CIR.0000133317.49796.0E. [DOI] [PubMed] [Google Scholar]
- Wilson PW, D’Agostino RB, Levy D, Belanger AM, Silbershatz H, Kannel WB. Prediction of coronary heart disease using risk factor categories. Circulation. 1998;97:1837–1847. doi: 10.1161/01.cir.97.18.1837. [DOI] [PubMed] [Google Scholar]
- Nieto FJ, Alonso J, Chambless LE, Zhong M, Ceraso M, Romm FJ, Cooper L, Folsom AR, Szklo M. Population awareness and control of hypertension and hypercholesterolemia. The Atherosclerosis Risk in Communities study. Arch Intern Med. 1995;155:677–684. [PubMed] [Google Scholar]
- Lemaitre RN, Furberg CD, Newman AB, Hulley SB, Gordon DJ, Gottdiener JS, McDonald RH, Jr, Psaty BM. Time trends in the use of cholesterol-lowering agents in older adults: the Cardiovascular Health Study. Arch Intern Med. 1998;158:1761–1768. doi: 10.1001/archinte.158.16.1761. [DOI] [PubMed] [Google Scholar]
- Arnett DK, Jacobs DR, Jr, Luepker RV, Blackburn H, Armstrong C, Claas SA. Twenty-year trends in serum cholesterol, hypercholesterolemia, and cholesterol medication use: the Minnesota Heart Survey, 1980–1982 to 2000–2002. Circulation. 2005;112:3884–3891. doi: 10.1161/CIRCULATIONAHA.105.549857. [DOI] [PubMed] [Google Scholar]
- O’Meara JG, Kardia SL, Armon JJ, Brown CA, Boerwinkle E, Turner ST. Ethnic and sex differences in the prevalence, treatment, and control of dyslipidemia among hypertensive adults in the GENOA study. Arch Intern Med. 2004;164:1313–1318. doi: 10.1001/archinte.164.12.1313. [DOI] [PubMed] [Google Scholar]
- Huang Y, Gao L, Xie X, Tan SC. Epidemiology of dyslipidemia in Chinese adults: meta-analysis of prevalence, awareness, treatment, and control. Popul Health Metr. 2014;12:28. doi: 10.1186/s12963-014-0028-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee YH, Lee SG, Lee MH, Kim JH, Lee BW, Kang ES, Lee HC, Cha BS. Serum cholesterol concentration and prevalence, awareness, treatment, and control of high low-density lipoprotein cholesterol in the Korea National Health and Nutrition Examination Surveys 2008–2010: beyond the Tip of the Iceberg. J Am Heart Assoc. 2014;3:e000650. doi: 10.1161/JAHA.113.000650. doi: 10.1161/JAHA.113.000650. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Muntner P, Levitan EB, Brown TM, Sharma P, Zhao H, Bittner V, Glasser S, Kilgore M, Yun H, Woolley JM, Farkouh ME, Rosenson RS. Trends in the prevalence, awareness, treatment and control of high low density lipoprotein-cholesterol among United States adults from 1999–2000 through 2009–2010. Am J Cardiol. 2013;112:664–670. doi: 10.1016/j.amjcard.2013.04.041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Persell SD, Maviglia SM, Bates DW, Ayanian JZ. Ambulatory hypercholesterolemia management in patients with atherosclerosis. Gender and race differences in processes and outcomes. J Gen Intern Med. 2005;20:123–130. doi: 10.1111/j.1525-1497.2005.40155.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen CY, Chuang SY, Fang CC, Huang LC, Hsieh IC, Pan WH, Yeh HI, Wu CC, Yin WH, Chen JW. Gender disparities in optimal lipid control among patients with coronary artery disease. J Atheroscler Thromb. 2014;21(suppl 1):S20–S28. doi: 10.5551/jat.21_sup.1-s20. [DOI] [PubMed] [Google Scholar]
- Kang-Kim M, Betancourt JR, Ayanian JZ, Zaslavsky AM, Yucel RM, Weissman JS. Access to care and use of preventive services by Hispanics: state-based variations from 1991 to 2004. Med Care. 2008;46:507–515. doi: 10.1097/MLR.0b013e31816dd966. [DOI] [PubMed] [Google Scholar]
- Winters P, Tancredi D, Fiscella K. The role of usual source of care in cholesterol treatment. J Am Board Fam Med. 2010;23:179–185. doi: 10.3122/jabfm.2010.02.090084. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kocher R, Emanuel EJ, DeParle NA. The Affordable Care Act and the future of clinical medicine: the opportunities and challenges. Ann Intern Med. 2010;153:536–539. doi: 10.7326/0003-4819-153-8-201010190-00274. [DOI] [PubMed] [Google Scholar]
- Cassidy A. Health policy brief: preventive services without cost sharing. Health Aff . Accessed December 28, 2010. [Google Scholar]
- Mann DM, Woodward M, Muntner P, Falzon L, Kronish I. Predictors of nonadherence to statins: a systematic review and meta-analysis. Ann Pharmacother. 2010;44:1410–1421. doi: 10.1345/aph.1P150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gonzalez HM, Vega WA, Tarraf W. Health care quality perceptions among foreign-born Latinos and the importance of speaking the same language. J Am Board Fam Med. 2010;23:745–752. doi: 10.3122/jabfm.2010.06.090264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schedlbauer A, Davies P, Fahey T. Interventions to improve adherence to lipid lowering medication. Cochrane Database Syst Rev. 2010:CD004371. doi: 10.1002/14651858.CD004371.pub3. [DOI] [PubMed] [Google Scholar]
- DeNavas-Walt C, Proctor BD, Smith JC. 2012. Income, poverty, and health insurance coverage in the United States: 2011 current population reports; P60–243.
- Gonzalez HM, Ceballos M, Tarraf W, West BT, Bowen ME, Vega WA. The health of older Mexican Americans in the long run. Am J Public Health. 2009;99:1879–1885. doi: 10.2105/AJPH.2008.133744. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stone NJ, Robinson JG, Lichtenstein AH, Bairey Merz CN, Blum CB, Eckel RH, Goldberg AC, Gordon D, Levy D, Lloyd-Jones DM, McBride P, Schwartz JS, Shero ST, Smith SC, Jr, Watson K, Wilson PW, Eddleman KM, Jarrett NM, LaBresh K, Nevo L, Wnek J, Anderson JL, Halperin JL, Albert NM, Bozkurt B, Brindis RG, Curtis LH, DeMets D, Hochman JS, Kovacs RJ, Ohman EM, Pressler SJ, Sellke FW, Shen WK, Smith SC, Jr, Tomaselli GF American College of Cardiology/American Heart Association Task Force on Practice G. 2013 ACC/AHA guideline on the treatment of blood cholesterol to reduce atherosclerotic cardiovascular risk in adults: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. Circulation. 2014;129:S1–S45. doi: 10.1161/01.cir.0000437738.63853.7a. [DOI] [PubMed] [Google Scholar]


