Abstract
Background
The aim of this study was to examine the awareness of a recent mass media campaign, and its influence on knowledge and prehospital times, in a cohort of acute coronary syndrome (ACS) patients admitted to an Australian hospital.
Methods and Results
We conducted 199 semistructured interviews with consecutive ACS patients who were aged 35 to 75 years, competent to provide consent, and English speaking. Questions addressed the factors known to predict prehospital delay, awareness of the campaign, and whether it increased knowledge and influenced actions. Multivariable logistic regression was used to examine the association between campaign awareness and a 1-hour delay in deciding to seek medical attention (patient delay) and a 2-hour delay in presenting to hospital (prehospital delay). The median age was 62 years (IQR=53 to 68 years), and 68% (n=136) were male. Awareness of the campaign was reported by 127 (64%) patients, with most of these patients stating the campaign (1) increased their understanding of what is a heart attack (63%), (2) increased their awareness of the signs and symptoms of heart attack (68%), and (3) influenced their actions in response to symptoms (43%). After adjustment for other predictors, awareness of the campaign was significantly associated with patient delay time of ≤1 hour (adjusted odds ratio [AOR]=2.25, 95% CI: 1.03 to 4.91, P=0.04) and prehospital delay time ≤2 hours (AOR=3.11, 95% CI: 1.36 to 7.08, P=0.007).
Conclusions
Our study showed reasonably high awareness of the warning signs campaign, which was significantly associated with shorter prehospital decision-making and faster presentation to hospital.
Keywords: acute coronary syndrome, emergency medical services, health education, mass media, prehospital delay
Definitive interventions, such as thrombolytic therapy, and coronary revascularization, can improve clinical outcomes for patients with acute coronary syndromes (ACS), but the benefits to mortality and morbidity of these interventions are time critical.1 Significant gains have been made in reducing inhospital times for ACS patients.2 However, many ACS patients do not receive the maximal benefit from these treatments because they delay in presenting to hospital in response to acute symptoms.3,4 This prehospital delay is also associated with preventable complications and worse patient outcomes.5–7
Prehospital delay is usually the result of the failure to recognize symptoms and/or act quickly and appropriately.8 Reviews of the extensive research undertaken to explore factors associated with delay have identified a wide range of sociodemographic, clinical, cognitive, emotional, and behavioral barriers that contribute to inappropriate responses to ACS symptoms.8,9 Ideally, patients should quickly recognize symptoms suggestive of ACS and immediately call emergency medical services (EMS) for timely intervention and transport to a hospital offering appropriate treatment. However, current evidence suggests there has been little change to prehospital delay times over the past decade,10 with less than half of ACS patients attributing their symptoms to the heart11 and most still not using EMS systems.12
In response, many organizations have launched awareness campaigns to educate the public. For example, in Australia, the Heart Foundation launched the Warning Signs of Heart Attack Strategy in 2009, which continued nationally until 2013. This multifaceted strategy included social marketing campaigns aimed to create greater relevance in the community about the risk of heart attack, improve knowledge of warning signs and symptoms, improve confidence to know what to do when experiencing the warning signs, and make it more likely that people would call an ambulance as a first-line response. The campaign also addressed some of the known barriers to taking appropriate action, such as ignoring symptoms or waiting for them to go away, poor awareness of nonclassic symptoms (eg, jaw pain, shortness of breath), concerns about burdening others or the ambulance service, and being embarrassed if it is a false alarm.8,13 Previous research has shown mass media campaigns can improve patient knowledge, but evidence of the actual impact on patient behavior is insufficient and has shown mixed findings.14 Our study therefore aims to address this gap by examining the awareness of the Heart Foundation’s campaign in a cohort of Australian ACS patients and to determine whether the campaign influenced prehospital behavior and times.
Methods
Study Design and Setting
We conducted a prospective, single-center observational study over 2 time periods (July to November 2013 and February to April 2014). Semistructured interviews were conducted with consecutive eligible ACS patients admitted to a metropolitan tertiary hospital located in Melbourne, Australia. The study was approved by ethics committees at Monash University and the Alfred Hospital, and all participants gave informed consent.
Current Campaign
Between May and August 2013, a fully paid mass media campaign across television and radio was conducted in the Melbourne metropolitan area, with digital advertising run nationally across the whole of 2013. This paid media activity was built on an intermittent campaign strategy conducted between 2009 and 2013, including paid and pro bono advertising on television, radio, and websites. Other pro bono community-based activities, such as stories in community newspapers and promotional materials distributed to community groups and hospitals, also took place in some parts of Melbourne. A campaign-specific website was established to provide comprehensive information about the warning signs of heart attack and the appropriate actions to take.15
Participants
Patients were identified from reviewing the daily cardiology admission lists for ACS patients: ST-elevation myocardial infarction (STEMI), non-STEMI (NSTEMI), and unstable angina (UA). To be eligible, patients had to have a confirmed primary diagnosis of out-of-hospital ACS defined as a rise in a cardiac biomarker (troponin I) above the 99th percentile upper reference limit (URL) and/or clinical symptoms consistent with myocardial ischemia, with ≥1 of the following: new or presumed new significant ST-segment–T-wave changes or new left bundle branch block on the ECG; development of pathological Q waves on the ECG; imaging evidence of new loss of viable myocardium or new regional wall motion abnormality; or identification of an intracoronary thrombus by angiography.16 Other eligibility criteria included: aged between 35 and 75 years; competent to provide consent; English-speaking; community dwelling resident (ie, not residential care); and medically stable and able to participate in a 30-minute interview.
Data Collection
Data were collected from an audit of the patient’s medical record and from semistructured interviews.
To examine the representativeness of the final sample, deidentified demographic (age, sex) and clinical (ACS subtype) data were collected from the medical record for patients who were ineligible and eligible patients who declined to participate.
For participating patients, data collected from the medical record, and patient interviews if missing, included (1) sociodemographic data (age, sex, marital status, country of birth, level of education, first aid, medical or nursing training, and EMS insurance cover); (2) clinical history (previous ACS, risk factors, and major comorbid conditions); and (3) current presentation (time of symptom onset and presentation to hospital, and ACS subtype).
Face-to-face interviews were conducted by using the modified Response To Symptoms Questionnaire (mRTSQ), with additional questions to specifically address the awareness and effect of the campaign. The mRTSQ was developed17 and modified18 to collect data about the symptoms (type, context, antecedents, and appraisal) and subsequent response (behavioral, cognitive, and emotional). Awareness of the campaign was first tested unprompted (by asking “Prior to this hospitalization, had you seen any television commercials and/or advertising about heart attacks?”) and prompted by showing video stills of campaign advertising (by asking “Prior to this hospitalization, had you seen any of the following television commercials and/or advertising?”). The mRTSQ contained 30 multiple choice questions and 3 open-ended questions. The open-ended questions captured (1) the symptoms experiences in the patient’s own words, (2) how the experience was different to what they expected a heart attack to be like, and (3) reasons for delay. The responses to open-ended questions were content analyzed by 2 experience researchers with nursing training. Disagreements in coding were resolved by discussion. Copies of the mRTSQ are available from the authors.
Statistical Analysis
The quantitative analysis of data used both descriptive and multivariate statistics. Descriptive statistics were performed to compare the demographic and clinical data of participants and nonparticipants. Descriptive statistics were also used to compare the demographic and clinical data of ACS patients who indicated that they were aware of the campaign (exposed group) with those of the patients who were not aware of the campaign (unexposed group). Mann–Whitney and t tests were used to analyze continuous variables, and the χ2 test was used for categorical variables.
Two time periods were calculated: prehospital delay time (time interval from symptom onset to arrival at hospital) and patient delay (time interval from symptom onset to the decision to seek medical attention). Prehospital times were established from medical record review and information given by the patient in the interview. Prompts and detailed questioning were used to aid recall of times.11,14 Patients were carefully interviewed to determine the time of onset of the symptom that was the reason they went to the hospital.14 The decision to seek medical attention was defined as the time the patient realized they need to seek medical care and was obtained during the interview and where possible confirmed with times recorded in the medical record (eg, time ambulance called). The time of arrival at hospital was taken as the time of arrival in the emergency department as recorded in the nursing triage notes.
Multivariable logistic regression models were developed to examine the association between campaign awareness and (1) a patient delay time of ≤1 hour and (2) a prehospital delay time of ≤2 hours.19,20 Given the sample size and large number of potential variables, propensity scores were estimated to adjust for the conditional probability that an individual was aware of the campaign.21 The propensity score included variables significantly associated with campaign awareness and prehospital delay time (Tables1 and 2) and was used as a covariate in the subsequent multivariable models. Propensity scores and final models were adjusted for variables that are consistently reported as associated with delay times in the literature: patient delay (level of education,21 recognized symptoms as heart related,20,22 choosing to wait and see if symptoms would go away,18 sudden onset,23 intermittent symptoms18,21,23 and STEMI20,23,24) and prehospital delay (recognized symptoms as heart related,22–24 choosing to wait and see if symptoms would go away,18 didn’t want to alarm or trouble others,18,21 STEMI,20,23,24 wanted to see local doctor first23,25). Statistical analysis was conducted in STATA and P-values <0.05 were considered statistically significant.
Table 1.
Demographics of the Overall Sample and a Comparison by Campaign Awareness
| Demographics | Patients Interviewed (n=199) | Aware of Campaign | P Value | |
|---|---|---|---|---|
| Yes (n=127) | No (n=72) | |||
| Age in y, median (IQR) | 62 (53 to 68) | 60 (52 to 67) | 65 (55 to 70) | 0.04 |
| Female, n (%) | 63 (32) | 39 (31) | 24 (33) | 0.70 |
| Born | ||||
| Australia, n (%) | 111 (56) | 80 (63) | 31 (43) | 0.007 |
| English-speaking country, n (%) | 134 (67) | 95 (75) | 39 (54) | 0.003 |
| Melbourne resident, n (%) | 160 (80) | 101 (80) | 59 (82) | 0.68 |
| Education, n (%) | ||||
| Primary/some high school | 59 (30) | 36 (28) | 23 (32) | 0.90 |
| Completed high school | 36 (18) | 23 (18) | 13 (18) | |
| Technical or some university | 47 (24) | 32 (25) | 15 (21) | |
| Completed university | 57 (29) | 36 (28) | 21 (29) | |
| Prior training, n (%) | ||||
| None | 106 (53) | 61 (48) | 45 (63) | 0.05 |
| Medical/nursing | 5 (2) | 3 (2) | 2 (3) | |
| First aid | 88 (44) | 63 (50) | 25 (35) | 0.04 |
| EMS insurance, n (%) | 139 (70) | 89 (70) | 50 (69) | 0.86 |
| Prior risk factors, n (%) | ||||
| Diabetes | 51 (26) | 35 (28) | 16 (22) | 0.41 |
| Hypertension | 118 (59) | 78 (61) | 40 (56) | 0.42 |
| Dyslipidemia | 124 (62) | 80 (63) | 44 (61) | 0.79 |
| Smoking (current or previous) | 71 (36) | 50 (39) | 21 (29) | 0.15 |
| Depression | 47 (24) | 35 (28) | 12 (17) | 0.08 |
| Any IHD | 82 (41) | 55 (43) | 27 (38) | 0.42 |
| MI | 57 (29) | 37 (29) | 20 (28) | 0.84 |
| Angina | 72 (36) | 46 (36) | 26 (36) | 0.99 |
| PCI | 50 (25) | 29 (23) | 21 (29) | 0.32 |
| CABG | 18 (9) | 20 (8) | 8 (11) | 0.44 |
| Any cardiac risk factor, n (%) | 174 (87) | 112 (88) | 62 (86) | 0.67 |
CABG indicates coronary artery bypass grafting; EMS, emergency medical services; IHD, ischemic heart disease; MI, myocardial infarction; PCI, percutaneous coronary intervention.
Table 2.
Univariate Analysis of Factors Related to Patients Delay of ≤1 Hour and Prehospital Delay of ≤2 Hours
| Patient Delay ≤1 Hour OR (95% CI) | Prehospital Delay ≤2 Hours OR (95% CI) | |
|---|---|---|
| Age >65 years | 0.94 (0.53 to 1.65) | 0.67 (0.36 to 1.22) |
| Female, n | 0.72 (0.40 to 1.32) | 0.62 (0.32 to 1.19) |
| Born in English-speaking country | 0.94 (0.52 to 1.71) | 0.84 (0.45 to 1.55) |
| 10 or more years education | 1.83 (1.04 to 3.22) | 1.80 (0.99 to 3.27) |
| EMS insurance | 1.48 (0.80 to 2.73) | 1.05 (0.55 to 2.00) |
| Nursing/first aid training | 0.96 (0.55 to 1.68) | 0.93 (0.52 to 1.68) |
| Prior risk factors | ||
| Diabetes | 0.74 (0.39 to 1.41) | 0.66 (0.33 to 1.33) |
| Hypertension | 0.91 (0.52 to 1.60) | 0.97 (0.54 to 1.76) |
| Dyslipidemia | 1.00 (0.57 to 1.78) | 1.17 (0.64 to 2.15) |
| Smoking (current or previous) | 1.83 (1.02 to 3.28) | 1.91 (1.04 to 3.49) |
| Depression | 0.80 (0.41 to 1.55) | 1.12 (0.57 to 2.22) |
| Any IHD | 0.90 (0.51 to 1.58) | 0.83 (0.46 to 1.51) |
| MI | 0.94 (0.51 to 1.74) | 1.06 (0.56 to 2.02) |
| Angina | 0.87 (0.48 to 1.55) | 0.86 (0.46 to 1.58) |
| PCI | 0.96 (0.51 to 1.83) | 0.78 (0.39 to 1.55) |
| CABG | 1.15 (0.44 to 3.04) | 0.96 (0.34 to 2.67) |
| Any cardiac risk factor | 1.66 (0.70 to 3.96) | 2.27 (0.81 to 6.34) |
| Experienced severe pain at onset | 1.30 (0.74 to 2.26) | 1.14 (0.64 to 2.06) |
| Experienced central/left-sided chest pain | 1.15 (0.61 to 2.16) | 0.97 (0.50 to 1.89) |
| STEMI | 2.18 (1.08 to 4.39) | 2.06 (1.03 to 4.13) |
| Recognized symptoms as heart related | 2.20 (1.24 to 3.87) | 2.17 (1.19 to 3.94) |
| Sudden onset | 2.67 (1.46 to 4.86) | 2.99 (1.53 to 5.83) |
| Similar symptoms before that went away | 0.33 (0.18 to 0.59) | 0.21 (0.11 to 0.42) |
| Symptoms came and went | 0.18 (0.10 to 0.35) | 0.18 (0.09 to 0.38) |
| Didn’t know any heart attack symptoms | 0.62 (0.29 to 1.31) | 0.20 (0.07 to 0.60) |
| Out of hours onset | 1.86 (1.05 to 3.27) | 1.45 (0.80 to 2.63) |
| Onset in public place | 1.03 (0.58 to 1.84) | 1.52 (0.83 to 2.78) |
| Alone at onset | 1.07 (0.59 to 1.91) | 0.99 (0.54 to 1.83) |
| Perceived control over symptoms | 0.37 (0.17 to 0.80) | 0.51 (0.23 to 1.16) |
| Felt embarrassed to get help | 0.69 (0.34 to 1.43) | 0.54 (0.24 to 1.21) |
| Anxious at symptom onset | 2.24 (1.25 to 4.01) | 2.77 (1.46 to 5.31) |
| Fear of what might happen | 0.83 (0.40 to 1.73) | 0.73 (0.33 to 1.63) |
| Didn’t want to alarm or trouble others* | 0.38 (0.22 to 0.68) | 0.29 (0.15 to 0.53) |
| Didn’t think symptoms were important enough to go to the hospital | 0.15 (0.08 to 0.29) | 0.20 (0.10 to 0.37) |
| Dislike of hospitals/previous bad experience | 0.46 (0.19 to 1.11) | 0.42 (0.15 to 1.16) |
| Choosing to wait and see if symptoms would go away | 0.36 (0.19 to 0.67) | 0.32 (0.17 to 0.61) |
| Wanted to see local physician first | — | 0.08 (0.02 to 0.34) |
| Called EMS | — | 1.64 (0.90 to 2.98) |
CABG indicates coronary artery bypass grafting; EMS, emergency medical services; IHD, ischemic heart disease; MI, myocardial infarction; OR, odds ratio; PCI, percutaneous coronary intervention; STEMI, ST-elevation myocardial infarction.
Combined as highly correlated.
Results
Participants
Over the 2 study periods, there were 323 ACS patients admitted and screened for inclusion in the study. Of these, 214 (66%) were eligible: 199 (93%) consented and were interviewed and 15 declined to participate. Reasons for exclusion in screened patients included age outside 35 to 75 years (n=77), non–English speaking (n=15), medically unstable (n=8), inpatient event (n=5), cognitive impairment (n=3), and previously interviewed and readmitted (n=1). Although the study intentionally included a younger subset of patients (aged 35 to 75 years), there was no difference in ACS subtypes or in the proportion of males between those interviewed and those excluded.
The median age of the patients interviewed was 62 years, and 68% were males (Table1). Just over half of the patients (56%) were born in Australia (67% born in an English-speaking country), with the majority (80%) currently residing in the city of Melbourne. Most of those interviewed had received a high school level or higher education (70%), and almost half had previously undergone either first-aid (44%) or nursing (2%) training. Patients presented with NSTEMI (44%), UA (35%), and STEMI (21%).
Awareness of the Campaign
Overall, two-thirds of patients (n=127) recalled seeing or hearing the campaign advertising either unprompted or after viewing screen shots of the advertising (Figure1). Over half of those aware of the campaign estimated they had seen the campaign during the period of paid advertising (May to August 2013): unprompted=55% and prompted=66%. Those aware of the campaign were more likely to be: younger (median age 60 years versus 65 years, P=0.04); born in Australia (63% versus 43%, P=0.007) or an English-speaking country (75% versus 54%, P=0.003); and first aid trained (50% versus 35%, P=0.04) (Table1). No other demographics or cardiac risk factors were associated with campaign awareness, including a history of previous ACS events or being a Melbourne resident.
Figure 1.
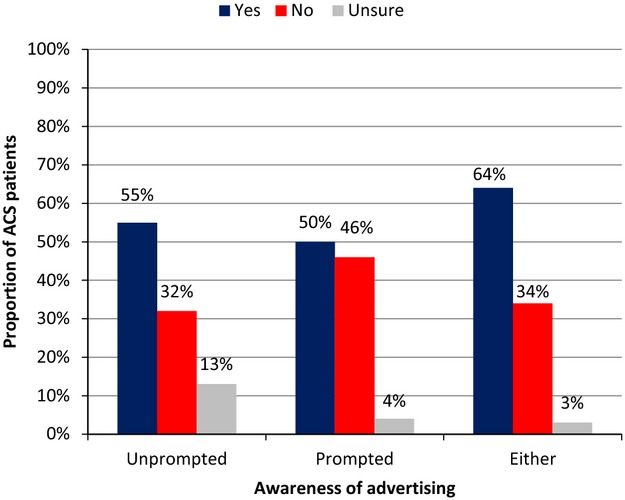
The proportion of ACS patients who recalled seeing commercials or advertising about heart attacks unprompted or after viewing screen shots of the advertising (n=199). ACS indicates acute coronary syndrome.
Influence of the Campaign on Knowledge
The majority of patients (91%) stated they knew at least 1 symptom or sign of heart attack (symptom knowledge) prior to this admission to hospital. Sources of this knowledge included the media (47%), personal experience (29%), first-aid training (19%), family members (21%), friends (11%), and local physicians (9%).
Campaign awareness was not associated with increased symptom knowledge (91% versus 90%, P=0.80). However, the majority of those aware stated that the campaign increased their awareness of what is a heart attack (63%) and the signs and symptoms of a heart attack (68%) (Figure2). Patients who stated the campaign influenced their knowledge of what is a heart attack were more likely to attribute their symptoms for this hospitalization to the heart (58% versus 41%, P=0.016).
Figure 2.
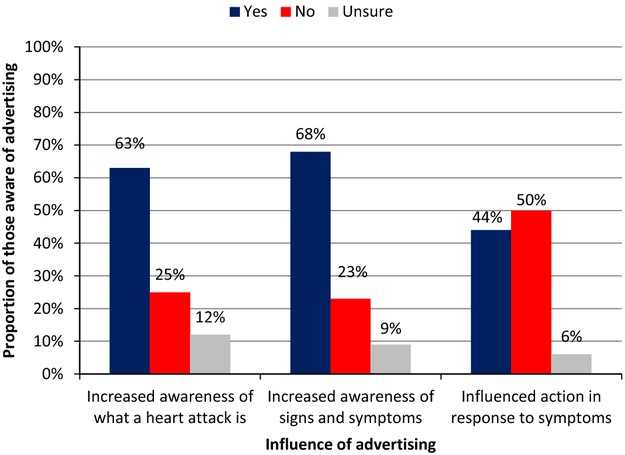
The influence of the campaign material on (1) awareness of what is a heart attack, (2) awareness of signs and symptoms, and (3) actions taken in response to symptoms (restricted to those aware of the campaign (n=127).
Influence of the Campaign on Prehospital Delay and Behavior
Almost half (43%) of the patients who were aware of the campaign said it influenced their actions in response to symptoms (Figure2). This was highest among patients who were admitted for a STEMI (62%), compared with NSTEMI (45%) and UA (30%). Those who stated the campaign influenced their behavior were more likely to be younger than 65 years (44% versus 24%, P=0.02).
The median patient delay time was 90 minutes (IQR=20 to 661), with almost half of patients (47%) deciding to seek medical attention within 1 hour of symptom onset. Factors significantly associated with a patient delay time of ≤1 hour at the univariate level are given in Table2. After adjustment for other important predictors and the propensity score, awareness of the campaign was significantly associated with patient delay time of ≤1 hour (adjusted odds ratio [AOR]=2.25, 95% CI:1.03 to 4.91, P=0.04) (Table3).
Table 3.
Models Testing the Association of Campaign Awareness and Patient Delay of ≤1 Hour and Prehospital Delay of ≤2 Hours
| Model | Covariates | OR (95% CI) | P Value |
|---|---|---|---|
| Patient delay ≤1 hour* | Aware of campaign | 2.25 (1.03 to 4.91) | 0.04 |
| ≥10 years’ education | 1.99 (1.03 to 4.91) | 0.05 | |
| Recognize symptoms as heart related | 4.52 (2.11 to 9.68) | <0.001 | |
| Symptoms came and went | 0.17 (0.08 to 0.36) | <0.001 | |
| Choosing to wait and see if symptoms would go away | 0.39 (0.18 to 0.86) | 0.019 | |
| STEMI | 3.22 (1.30 to 7.96) | 0.011 | |
| Sudden onset | 3.22 (1.53 to 6.80) | 0.002 | |
| Prehospital delay ≤2 hours* | Aware of campaign | 3.10 (1.36 to 7.09) | 0.007 |
| Wanted to see local doctor first | 0.08 (0.02 to 0.38) | 0.002 | |
| Choosing to wait and see if symptoms would go away | 0.28 (0.13 to 0.61) | 0.001 | |
| STEMI | 2.54 (1.09 to 5.95) | 0.03 | |
| Didn’t want to alarm or trouble others | 0.44 (0.21 to 0.89) | 0.02 | |
| Recognize symptoms as heart related | 3.27 (1.52 to 7.00) | 0.002 |
OR indicates odds ratio; STEMI, ST-elevation myocardial infarction.
Adjusted for propensity score.
The median prehospital delay was 210 minutes (IQR=100 to 1035), with 34% presenting to hospital within 2 hours of symptom onset. Table2 provides the factors significantly associated with a prehospital delay time of ≤2 hours. After adjustment, awareness of the campaign was significantly associated with a prehospital delay time ≤2 hours (AOR=3.10, 95% CI: 1.36 to 7.09, P=0.007) (Table3).
Overall, 18% of patients visited their general practitioner (GP) before presenting to hospital. Patients admitted with unstable angina (26%) or NSTEMI (20%) were more likely to visit their GP than were patients experiencing STEMI (2%, P=0.007). Campaign awareness was not associated with lower rates of visiting a GP (20% versus 14%, P=0.24), although those aware of the campaign who stated the campaign influenced their behavior were less likely to visit a GP (7% versus 22%, P=0.017).
The EMS system was used by 53% of patients, although 8% of these patients first attempted transport in a car or drove to a GP who called EMS. EMS use was highest among patients admitted with STEMI (69%), compared with NSTEMI (52%) and UA (47%). No difference was seen in EMS use by campaign awareness (52% versus 57%, P=0.50) or in those who stated the campaign influenced their behavior (56% versus 53%, P=0.78).
Discussion
This study found ACS patients who were aware of the Heart Foundation campaign were more than twice as likely to decide to seek medical attention and present to hospital in the first hours after symptom onset. However, use of the EMS system was not increased. Our study also confirmed previous published findings of factors related to prehospital delay and identified the characteristics of those with lower awareness of the campaign.
Given the campaign was aimed at the general public and competing with other health care messages, awareness of the campaign at 64% among ACS patients is reasonably high. This is particularly so when considered in the context of a recent evaluation of a stroke awareness campaign, in which only 12% of patients or bystanders recalled exposure to campaign advertising.26 Another Australian report evaluating a Heart Attack campaign in late 1980s found similar campaign reach (72%) among ACS patients in a multicenter study.27 In our sample, campaign awareness was lower in older ACS patients and those born in non–English-speaking countries. These groups could be targeted in future campaigns, along with the other factors associated with prehospital delay.
The factors associated with prehospital delay in our study are similar to those of previous Australian and international reports.18,20,21,28 Our study also confirms that a broad range of factors influence delay times,8,9 including sociodemographic (eg, level of education), clinical (eg, intermittent symptoms), perceptual (eg, recognizing symptoms as heart related), behavioral (eg, wanting to see a local doctor first), and emotional/psychological (eg, not wanting to alarm or trouble others). However, our multivariable models were unable to test the association of all factors at an individual level, as this would have resulted in overfit in both models. These factors were instead represented in the model in the propensity score, and therefore there may be additional factors independently associated with delays times to those identified by our study.
Of particular interest is the prehospital experience of STEMI patients, who benefit the most from reduced delay times. Similar to previous studies,20,24 STEMI was strongly associated with deciding to seek medical attention within 1 hour of symptom onset and present to hospital within 2 hours of onset. STEMI patients were also more likely to state the campaign influenced their actions in response to symptoms and to use EMS as transport (69% versus 50%, P=0.02).
Overall our study found only half of patients presented to hospital by EMS, 57% in those experiencing an acute myocardial infarction. These percentages are unchanged from earlier Australian reports.21,28,29 Most studies to date have found no impact of mass media campaigns on EMS use in patients admitted with ACS.30,31 Only 1 study using a multifaceted and community-based approach (eg, targeted mass media, community engagement, and education for professionals, the public, and patients) has been effective.32 EMS use has also been shown to increase following campaigns for other acute conditions, including stroke33—particularly when EMS use was highlighted in all campaign materials and included in the main message of the campaign. Barriers to calling EMS for ACS symptoms include thinking self-transport would be faster, having a lower perceived seriousness of symptoms, embarrassment, and thinking it is not necessary to use ambulance.25,34 The Warning Signs advertisements sought to overcome some of these barriers by highlighting the consequences of waiting (“I didn’t realize my heart muscle had already started to die,” “The longer you wait, the more your heart muscle dies”) and to call an ambulance even if unsure (“The [emergency] operator will work out if you need an ambulance”). However, our study suggests this approach did not increase EMS use in ACS patients. A qualitative study describes the decision to call EMS for symptoms as multifactorial and identified the immediate access to care and the safety of transport as important in making this decision.35 Further research is needed to understand this decision-making process for ACS symptoms and to identify what campaign messages can highlight the need and important benefits of EMS use to increase ambulance use.
The prehospital delay times in our study (median 210 minutes) are comparable to those of recent international reports for all ACS patients and in ACS subgroups.19 However, when we compared our times with those in earlier Australian reports of patient27,36 and total prehospital28,36 delay, we saw no reduction over the last 2 decades. This may be explained by differences in the definitions of the timeframes and starting points between studies.37 We did note an upward trend in Australian data for the percentage of patients who (1) decided to seek medical attention within 1 hour (38% in 1988,27 42% in 1989 precampaign,27 45% in 1989 postcampaign,27 to 47% in our 2013-2014 study) and (2) who presented to hospital within 2 hours of symptom onset (28% in 199521 to 34% in our study).
Other large interventional and observational studies have shown a mixed influence of campaigns on prehospital delay times.14 The largest randomized control trial, the Rapid Early Action for Coronary Treatment (REACT) study conducted across 20 cities in the United States, found no impact of a community-based intervention on prehospital delay, although an increased use in EMS was seen among ACS patients.32 Most other studies conducted in the United States have also failed to show any impact,31,32 whereas those in Europe have been more favorable.30,38,39 This difference could be attributed to differences in the duration of data collection, healthcare systems, media environments, and insurance coverage.14,32,39 Bett et al evaluated earlier Australian campaigns and found no change in median prehospital delay in the weeks following 3 separate campaigns.27,36 In those evaluations, which were conducted across a large number of Australian hospitals, there was no adjustment for important differences between samples or for other factors that are now known to influence prehospital delay.8 That study, as well as the international evaluations, also did not evaluate the awareness of the campaign among patients studied—a major strength of our study.
Another potential explanation for the success of the current campaign was that it was the first Australian campaign to go beyond awareness of symptoms and action, which has also been the focus of most international campaigns that have been evaluated,14 and specifically address known barriers. The first of the recent Australian television advertisements (It’s Ok to Call) shows a cardiologist discussing the need to call an ambulance and that false alarms are ok. The second advertisement (I wish I could have my heart attack again) uses a white, male actor as a deceased heart attack patient reliving what he would do differently if he could have his heart attack again. This is the first Australian campaign to use patient experience to illustrate lesser known symptoms and highlight the risk of ignoring symptoms, the need for early action, and to use EMS. The use of a white male in the advertising and having it only available in English may explain the lower campaign awareness seen in non–English-speaking Australians. Future and international campaigns may need to consider using a broader ethnic demographic in advertising and using subtitles. International campaigns may also need to address the barriers to seeking treatment specific to their own ACS population, which are known to vary by region and cultural norms.11
Limitations
Our findings must be considered in light of the following limitations. Data for our study were collected at only 1 site. However, the hospital where recruitment occurred received patients from both metropolitan (80%) and rural regions (20%) during the study period; thus, our findings are not restricted to metropolitan cases. Further, the demographics, risk factor profile, and proportion of ACS subtypes of our sample were similar to those reported in the 2365 confirmed ACS patients captured in the ACS SNAPSHOT audit of 286 Australian hospitals.40 Nonetheless, our findings will require confirmation in a larger multicenter evaluation. The campaign and our evaluation deliberately targeted a younger audience, so the findings may not apply to older ACS patients. The other limitations of the study relate to the collection of data on a retrospective event; thus, the findings are subject to recall bias and prehospital delay may be related to other factors not measured.
In summary, our study found awareness of the Heart Foundation’s Warning Signs mass media campaign was reasonably high in a cohort of Australian ACS patients, and this was associated with shorter patient and prehospital delay times but not EMS use. Future campaigns could target groups in whom awareness was low (older patients and those not born in Australia) and highlight the need and important benefits of EMS use.
Acknowledgments
We would like to thank Dr Jathushan Palasubramaniam for his assistance with data collection and Alyse Lennox for assistance with data entry.
Sources of Funding
This study was commissioned by the Heart Foundation. The Heart Foundation was not involved in the data collection or statistical analysis. Drs Bray, Cartledge, and Finn receive salary support from the National Health and Medical Research Council (NHMRC) Centre for Research Excellence: Australian Resuscitation Outcomes Consortium (No. 1029983). Drs Bray and Stub are supported by co-funded NHMRC/Heart Foundation Research Fellowships (No. 1090302/100516 and No. 1069985/100136). Dr Finn receives salary support from St John Ambulance Western Australia.
Disclosures
Drs Stewart, Keech, and Patsamanis were employed by the Heart Foundation at the time of this study. Drs Bray and Finn provide unpaid consultation to the Heart Foundation. Drs Bray and Stub receive Research Fellowships co-funded by the Heart Foundation.
References
- O’Connor RE, Brady W, Brooks SC, Diercks D, Egan J, Ghaemmaghami C, Menon V, O’Neil BJ, Travers AH, Yannopoulos D. Part 10: acute coronary syndromes: 2010 American Heart Association Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care. Circulation. 2010;122:S787–S817. doi: 10.1161/CIRCULATIONAHA.110.971028. [DOI] [PubMed] [Google Scholar]
- Krumholz HM, Herrin J, Miller LE, Drye EE, Ling SM, Han LF, Rapp MT, Bradley EH, Nallamothu BK, Nsa W, Bratzler DW, Curtis JP. Improvements in door-to-balloon time in the United States, 2005 to 2010. Circulation. 2011;124:1038–1045. doi: 10.1161/CIRCULATIONAHA.111.044107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sivagangabalan G, Ong AT, Narayan A, Sadick N, Hansen PS, Nelson GC, Flynn M, Ross DL, Boyages SC, Kovoor P. Effect of prehospital triage on revascularization times, left ventricular function, and survival in patients with ST-elevation myocardial infarction. Am J Cardiol. 2009;103:907–912. doi: 10.1016/j.amjcard.2008.12.007. [DOI] [PubMed] [Google Scholar]
- Sorajja P, Gersh BJ, Cox DA, McLaughlin MG, Zimetbaum P, Costantini C, Stuckey T, Tcheng JE, Mehran R, Lansky AJ, Grines CL, Stone GW. Impact of delay to angioplasty in patients with acute coronary syndromes undergoing invasive management: analysis from the ACUITY (Acute Catheterization and Urgent Intervention Triage strategY) trial. J Am Coll Cardiol. 2010;55:1416–1424. doi: 10.1016/j.jacc.2009.11.063. [DOI] [PubMed] [Google Scholar]
- Al-Mallah MH, Bazari RN, Khanal S. Delay in invasive risk stratification of women with acute coronary syndrome is associated with worse outcomes. J Thromb Thrombolysis. 2007;23:35–39. doi: 10.1007/s11239-006-9013-8. [DOI] [PubMed] [Google Scholar]
- De Luca G, Suryapranata H, Ottervanger JP, Antman EM. Time delay to treatment and mortality in primary angioplasty for acute myocardial infarction: every minute of delay counts. Circulation. 2004;109:1223–1225. doi: 10.1161/01.CIR.0000121424.76486.20. [DOI] [PubMed] [Google Scholar]
- Steg PG, Bonnefoy E, Chabaud S, Lapostolle F, Dubien PY, Cristofini P, Leizorovicz A, Touboul P. Impact of time to treatment on mortality after prehospital fibrinolysis or primary angioplasty: data from the CAPTIM randomized clinical trial. Circulation. 2003;108:2851–2856. doi: 10.1161/01.CIR.0000103122.10021.F2. [DOI] [PubMed] [Google Scholar]
- Moser DK, Kimble LP, Alberts MJ, Alonzo A, Croft JB, Dracup K, Evenson KR, Go AS, Hand MM, Kothari RU, Mensah GA, Morris DL, Pancioli AM, Riegel B, Zerwic JJ. Reducing delay in seeking treatment by patients with acute coronary syndrome and stroke: a scientific statement from the American Heart Association Council on Cardiovascular Nursing and Stroke Council. Circulation. 2006;114:168–182. doi: 10.1161/CIRCULATIONAHA.106.176040. [DOI] [PubMed] [Google Scholar]
- Dracup K, Moser DK, Eisenberg M, Meischke H, Alonzo AA, Braslow A. Causes of delay in seeking treatment for heart attack symptoms. Soc Sci Med. 1995;40:379–392. doi: 10.1016/0277-9536(94)00278-2. [DOI] [PubMed] [Google Scholar]
- Flynn A, Moscucci M, Share D, Smith D, LaLonde T, Changezi H, Riba A, Gurm HS. Trends in door-to-balloon time and mortality in patients with ST-elevation myocardial infarction undergoing primary percutaneous coronary intervention. Arch Intern Med. 2010;170:1842–1849. doi: 10.1001/archinternmed.2010.381. [DOI] [PubMed] [Google Scholar]
- McKinley S, Dracup K, Moser DK, Ball C, Yamasaki K, Kim CJ, Barnett M. International comparison of factors associated with delay in presentation for AMI treatment. Eur J Cardiovasc Nurs. 2004;3:225–230. doi: 10.1016/j.ejcnurse.2004.06.004. [DOI] [PubMed] [Google Scholar]
- Thang ND, Karlson BW, Bergman B, Santos M, Karlsson T, Bengtson A, Johanson P, Rawshani A, Herlitz J. Characteristics of and outcome for patients with chest pain in relation to transport by the emergency medical services in a 20-year perspective. Am J Emerg Med. 2012;30:1788–1795. doi: 10.1016/j.ajem.2012.02.014. [DOI] [PubMed] [Google Scholar]
- Dracup K, Bryan-Brown CW. Reducing patient delay in seeking treatment. Am J Crit Care. 1997;6:415–417. [PubMed] [Google Scholar]
- Mooney M, McKee G, Fealy G, O’Brien F, O’Donnell S, Moser D. A review of interventions aimed at reducing pre-hospital delay time in acute coronary syndrome: what has worked and why? Eur J Cardiovasc Nurs. 2012;11:445–453. doi: 10.1016/j.ejcnurse.2011.04.003. [DOI] [PubMed] [Google Scholar]
- Heart Foundation. Warning signs campaign website. Available at: www.heartattackfacts.org.au. Accessed 1/12/2014.
- Thygesen K, Alpert JS, Jaffe AS, Simoons ML, Chaitman BR, White HD, Katus HA, Lindahl B, Morrow DA, Clemmensen PM, Johanson P, Hod H, Underwood R, Bax JJ, Bonow RO, Pinto F, Gibbons RJ, Fox KA, Atar D, Newby LK, Galvani M, Hamm CW, Uretsky BF, Steg PG, Wijns W, Bassand JP, Menasche P, Ravkilde J, Ohman EM, Antman EM, Wallentin LC, Armstrong PW, Januzzi JL, Nieminen MS, Gheorghiade M, Filippatos G, Luepker RV, Fortmann SP, Rosamond WD, Levy D, Wood D, Smith SC, Hu D, Lopez-Sendon JL, Robertson RM, Weaver D, Tendera M, Bove AA, Parkhomenko AN, Vasilieva EJ, Mendis S. Third universal definition of myocardial infarction. Circulation. 2012;126:2020–2035. doi: 10.1161/CIR.0b013e31826e1058. [DOI] [PubMed] [Google Scholar]
- Burnett RE, Blumenthal JA, Mark DB, Leimberger JD, Califf RM. Distinguishing between early and late responders to symptoms of acute myocardial infarction. Am J Cardiol. 1995;75:1019–1022. doi: 10.1016/s0002-9149(99)80716-4. [DOI] [PubMed] [Google Scholar]
- Dracup K, Moser DK. Beyond sociodemographics: factors influencing the decision to seek treatment for symptoms of acute myocardial infarction. Heart Lung. 1997;26:253–262. doi: 10.1016/s0147-9563(97)90082-0. [DOI] [PubMed] [Google Scholar]
- Goldberg RJ, Spencer FA, Fox KA, Brieger D, Steg PG, Gurfinkel E, Dedrick R, Gore JM. Prehospital delay in patients with acute coronary syndromes (from the global registry of acute coronary events [GRACE]) Am J Cardiol. 2009;103:598–603. doi: 10.1016/j.amjcard.2008.10.038. [DOI] [PubMed] [Google Scholar]
- Perkins-Porras L, Whitehead DL, Strike PC, Steptoe A. Pre-hospital delay in patients with acute coronary syndrome: factors associated with patient decision time and home-to-hospital delay. Eur J Cardiovasc Nurs. 2009;8:26–33. doi: 10.1016/j.ejcnurse.2008.05.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dracup K, McKinley SM, Moser DK. Australian patients’ delay in response to heart attack symptoms. Med J Aust. 1997;166:233–236. doi: 10.5694/j.1326-5377.1997.tb140101.x. [DOI] [PubMed] [Google Scholar]
- Ottesen MM, Dixen U, Torp-Pedersen C, Kober L. Prehospital delay in acute coronary syndrome—an analysis of the components of delay. Int J Cardiol. 2004;96:97–103. doi: 10.1016/j.ijcard.2003.04.059. [DOI] [PubMed] [Google Scholar]
- McKee G, Mooney M, O’Donnell S, O’Brien F, Biddle MJ, Moser DK. Multivariate analysis of predictors of pre-hospital delay in acute coronary syndrome. Int J Cardiol. 2013;168:2706–2713. doi: 10.1016/j.ijcard.2013.03.022. [DOI] [PubMed] [Google Scholar]
- Thuresson M, Jarlov MB, Lindahl B, Svensson L, Zedigh C, Herlitz J. Thoughts, actions, and factors associated with prehospital delay in patients with acute coronary syndrome. Heart Lung. 2007;36:398–409. doi: 10.1016/j.hrtlng.2007.02.001. [DOI] [PubMed] [Google Scholar]
- Ingarfield SL, Jacobs IG, Jelinek GA, Mountain D. Patient delay and use of ambulance by patients with chest pain. Emerg Med Australas. 2005;17:218–223. doi: 10.1111/j.1742-6723.2005.00726.x. [DOI] [PubMed] [Google Scholar]
- Bray JE, O’Connell B, Gilligan A, Livingston PM, Bladin C. Is FAST stroke smart? Do the content and language used in awareness campaigns describe the experience of stroke symptoms? Int J Stroke. 2010;5:440–446. doi: 10.1111/j.1747-4949.2010.00484.x. [DOI] [PubMed] [Google Scholar]
- Bett N, Aroney G, Thompson P. Impact of a national educational campaign to reduce patient delay in possible heart attack. Aust N Z J Med. 1993;23:157–161. doi: 10.1111/j.1445-5994.1993.tb01810.x. [DOI] [PubMed] [Google Scholar]
- McKinley S, Aitken LM, Marshall AP, Buckley T, Baker H, Davidson PM, Dracup K. Delays in presentation with acute coronary syndrome in people with coronary artery disease in Australia and New Zealand. Emerg Med Australas. 2011;23:153–161. doi: 10.1111/j.1742-6723.2011.01385.x. [DOI] [PubMed] [Google Scholar]
- Lozzi L, Carstensen S, Rasmussen H, Nelson G. Why do acute myocardial infarction patients not call an ambulance? An interview with patients presenting to hospital with acute myocardial infarction symptoms. Intern Med J. 2005;35:668–671. doi: 10.1111/j.1445-5994.2005.00957.x. [DOI] [PubMed] [Google Scholar]
- Herlitz J, Blohm M, Hartford M, Karlson BW, Luepker R, Holmberg S, Risenfors M, Wennerblom B. Follow-up of a 1-year media campaign on delay times and ambulance use in suspected acute myocardial infarction. Eur Heart J. 1992;13:171–177. doi: 10.1093/oxfordjournals.eurheartj.a060142. [DOI] [PubMed] [Google Scholar]
- Ho MT, Eisenberg MS, Litwin PE, Schaeffer SM, Damon SK. Delay between onset of chest pain and seeking medical care: the effect of public education. Ann Emerg Med. 1989;18:727–731. doi: 10.1016/s0196-0644(89)80004-6. [DOI] [PubMed] [Google Scholar]
- Luepker RV, Raczynski JM, Osganian S, Goldberg RJ, Finnegan JR, Jr, Hedges JR, Goff DC, Jr, Eisenberg MS, Zapka JG, Feldman HA, Labarthe DR, McGovern PG, Cornell CE, Proschan MA, Simons-Morton DG. Effect of a community intervention on patient delay and emergency medical service use in acute coronary heart disease: the Rapid Early Action for Coronary Treatment (REACT) Trial. JAMA. 2000;284:60–67. doi: 10.1001/jama.284.1.60. [DOI] [PubMed] [Google Scholar]
- Bray JE, Straney L, Barger B, Finn J. Effect of public awareness campaigns on calls to ambulance across Australia. Stroke. 2015;46:1377–1380. doi: 10.1161/STROKEAHA.114.008515. [DOI] [PubMed] [Google Scholar]
- Meischke H, Ho MT, Eisenberg MS, Schaeffer SM, Larsen MP. Reasons patients with chest pain delay or do not call 911. Ann Emerg Med. 1995;25:193–197. doi: 10.1016/s0196-0644(95)70323-3. [DOI] [PubMed] [Google Scholar]
- Ahl C, Nystrom M, Jansson L. Making up one’s mind:—patients’ experiences of calling an ambulance. Accid Emerg Nurs. 2006;14:11–19. doi: 10.1016/j.aaen.2005.10.002. [DOI] [PubMed] [Google Scholar]
- Bett JH, Tonkin AM, Thompson PL, Aroney CN. Failure of current public educational campaigns to impact on the initial response of patients with possible heart attack. Intern Med J. 2005;35:279–282. doi: 10.1111/j.1445-5994.2004.00798.x. [DOI] [PubMed] [Google Scholar]
- Mackay MH, Ratner PA, Nguyen M, Percy M, Galdas P, Grunau G. Inconsistent measurement of acute coronary syndrome patients’ pre-hospital delay in research: a review of the literature. Eur J Cardiovasc Nurs. 2014;13:483–493. doi: 10.1177/1474515114524866. [DOI] [PubMed] [Google Scholar]
- Gaspoz JM, Unger PF, Urban P, Chevrolet JC, Rutishauser W, Lovis C, Goldman L, Heliot C, Sechaud L, Mischler S, Waldvogel FA. Impact of a public campaign on pre-hospital delay in patients reporting chest pain. Heart. 1996;76:150–155. doi: 10.1136/hrt.76.2.150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Naegeli B, Radovanovic D, Rickli H, Erne P, Seifert B, Duvoisin N, Pedrazzini G, Urban P, Bertel O. Impact of a nationwide public campaign on delays and outcome in Swiss patients with acute coronary syndrome. Eur J Cardiovasc Prev Rehabil. 2011;18:297–304. doi: 10.1177/1741826710389386. [DOI] [PubMed] [Google Scholar]
- Chew DP, French J, Briffa TG, Hammett CJ, Ellis CJ, Ranasinghe I, Aliprandi-Costa BJ, Astley CM, Turnbull FM, Lefkovits J, Redfern J, Carr B, Gamble GD, Lintern KJ, Howell TE, Parker H, Tavella R, Bloomer SG, Hyun KK, Brieger DB. Acute coronary syndrome care across Australia and New Zealand: the SNAPSHOT ACS study. Med J Aust. 2013;199:185–191. doi: 10.5694/mja12.11854. [DOI] [PubMed] [Google Scholar]


