Abstract
Double outlet atrium is a rare cardiac anomaly wherein one of the atriums, most frequently the right atrium, opens into both the ventricles. Although seen more commonly in the setting of atrioventricular septal defect, this arrangement can also be found when one of the atrioventricular connections is atretic due to absence of the atrioventricular connection and the other atrioventricular valve straddles the muscular ventricular septum. It is the specific anatomy and connections of the atrioventricular junction that clarifies the situation and distinguishes between these two types of double outlet atrium. In this report, we present a case of double outlet right atrium co-existing with the absence of left atrioventricular connection. We then discuss the morphologic aspects of this interesting anomaly.
Keywords: Atrioventricular junction, atrioventricular septal defect, double outlet atrium, x plane imaging
INTRODUCTION
It is rare to find absence of the left atrioventricular connection co-existing with a straddling right atrioventricular valve. In this setting, the left atrium drains only to the right atrium either through a defect within the oval fossa or through a patent oval foramen, the left atrial cavity having no direct connection to the ventricular mass [Figure 1, left hand panel]. In the majority of hearts with such absence of the left atrioventricular connection, the right atrium connects either to a dominant right ventricle as found in one form of hypoplastic left heart syndrome or to a dominant left ventricle, as in so-called “tricuspid atresia with l-transposition”. The arrangement in which the right atrioventricular junction overrides the crest of the deficient ventricular septum such that the right atrium drains to both ventricles is called double outlet right atrium.[1] A similar appearance can be seen in the setting of an atrioventricular septal defect with common atrioventricular junction.[1,2,3,4,5,6,7,8,9,10,11,12] The interatrial communication, however, is then through an ostium primum defect, rather than being found at the level of the oval fossa [Figure 1, right hand panel]. There is but one atrioventricular junction in both these situations. The junction, nonetheless, is common in the setting of the ostium primum defect but solitary in the hearts with the straddling right atrioventricular valve.[13,14,15,16] The essence of the variant found with the ostium primum defect is malalignment of the primary atrial septum such that the only exit from the left atrium is through the atrioventricular septal defect. Imaging the atrioventricular junction itself is obviously the key to precise diagnosis of patients with these lesions. The diagnosis, however, is challenging in patients with such complex cardiac anatomy. We report here the use of “X plane imaging” during echocardiography in clarifying the diagnosis in our patient. The situation was the more complicated in our patient in that the straddling atrioventricular valve was itself divided into dual orifices. Each orifice, furthermore, was committed to its own ventricle due to fusion of the dividing valvar bridge to the crest of the deficient ventricular septum. This arrangement produced the paradoxical situation of the ventricular septum seemingly being intact, despite the obvious presence of a ventricular septal deficiency [Figure 2]. This apparent lack of a potential for interventricular shunting proves to be a favorable aspect of the anatomy, as it potentially permits biventricular repair despite the complex anatomical arrangement.
Figure 1.
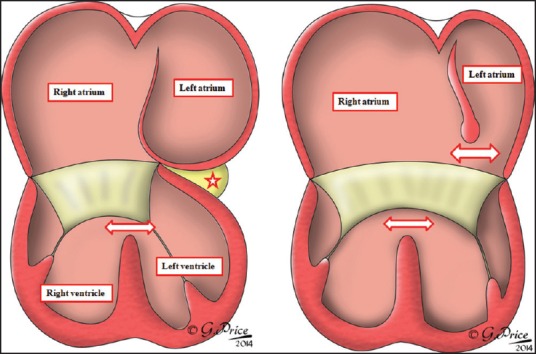
The cartoon shows the two different variants of so-called “double outlet right atrium”. The left hand panel shows the situation when there is absence of the left atrioventricular connection (white star with red borders). In this setting, the double outlet exists because the right atrioventricular valve straddles the crest of the muscular ventricular septum, with a ventricular septal defect between its ventricular surface and the septal crest (white arrow with red borders). The right hand panel shows the arrangement with common atrioventricular junction and atrioventricular septal defect (paired white arrows with red borders). This variant is due to malalignment of the primary atrial septum, with the left atrium exiting through an ostium primum defect (upper white arrow in right hand panel)
Figure 2.
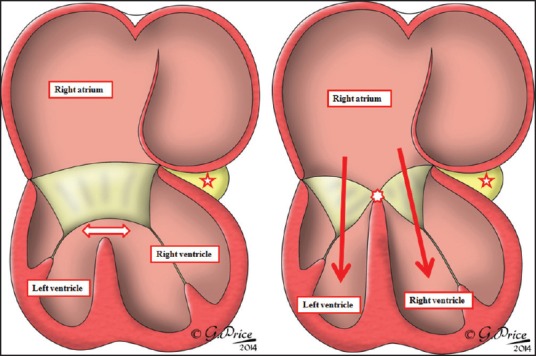
The cartoons show the anatomy to be described in our patient. There was left-handed ventricular topology, so the right atrioventricular valve straddled between a right-sided morphologically left ventricle and a left-sided morphologically right ventricle. Unlike the anticipated situation with a ventricular septal defect, however, (left hand panel) there were dual orifices in the straddling valve. The connecting tongue separating the orifices (white star with red borders) was bound down to the crest of the ventricular septum (right hand panel), so that each valvar orifice connected to a separate ventricle, with the ventricular septum seeming to be intact
CASE REPORT
Our patient, a four and half month-old female infant, presented with mild cyanosis. She had exhibited rapid breathing since birth. Tachycardia and tachypnea were evident on examination, and her systemic saturation was measured at 74%. The second heart sound was loud, and a faint systolic murmur was audible over the infraclavicular area. There was no hepatomegaly. No cardiomegaly was evident on the chest radiograph, but pulmonary venous congestion was present bilaterally. The transthoracic echocardiogram showed usual arrangement of the abdominal organs and atrial appendages with dilation of the tube-like morphologically left appendage [Figure 3a]. The pulmonary and systemic venous connections were normal. The coronary sinus, however, was not identified, and the left atrioventricular connection was absent [Figure 3b]. The cavity of the left atrium drained into the right atrium across a restrictive patent oval foramen, with continuous left-to-right flow, with the measured gradient of 16 mm Hg suggesting elevated left atrial pressures. The cavity of the right atrium connected not only to the right-sided morphologically left ventricle, but also to a smaller morphologically right ventricle which was positioned leftward and superiorly relative to the dominant left ventricle [Figure 3c and Online Video 1]. The right atrioventricular valve itself exhibited dual atrioventricular orifices with the bridge of valvar tissue separating the orifices bound down to the crest of the deficient and malaligned ventricular septum. Because of this arrangement, there was no potential for interventricular shunting [Figure 3c]. The ventriculo-arterial connections were discordant, with the aorta lying to the left and anterior relative to the pulmonary trunk. The aortic arch was left-sided with a narrowing to about two-fifth of its ascending dimensions observed at the aortic isthmus. There was a large tubular patent arterial duct, permitting flow from pulmonary artery to descending aorta.
Figure 3.
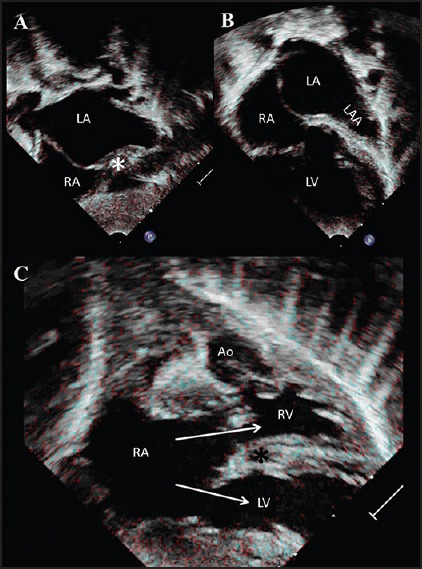
The panels show the salient features of trans-thoracic echocardiography obtained in subcostal. There is usual arrangement of atriums, with absent left atrioventricular connection (*) (a). The left atrial appendage is well-seen (b), with the right atrium connecting to both the ventricles (LV, RV) through two well-formed orifice in the straddling right atrioventricular valve (c). The ventricles themselves are mirror-imaged, showing left-handed ventricular topology. The valvar tissue separating the orifices within the straddling valve is attached to the crest of the misaligned muscular ventricular septum, thus obliterating the ventricular septal deficiency (*). The aorta arises from the smaller right ventricle, producing discordant ventriculoarterial connections. Ao = aorta; LA = left atrium; LAA = left atrial appendage; LV = left ventricle; RA = right atrium; RV = right ventricle
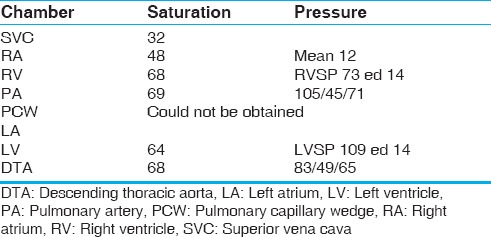
Cardiac catheterization was then performed to provide better delineation of the anatomy, and to permit balloon dilation of the restrictive oval foramen so as to relieve the left atrial hypertension. Pressures in the morphologically left ventricle and pulmonary arteries were greater than those in the morphologically right ventricle and aorta, in keeping with the lack of any substrate for interventricular shunting [Table 1]. Attempts made to enter the left atrium in order to dilate the oval fossa, however, were unsuccessful. The angiograms made in the superior caval vein and in both ventricles confirmed absence of the left atrioventricular connection revealing a uniatrial but biventricular connection, supero-inferior relationship of the ventricles, no substrate for interventricular shunting despite the malalignment between the atrial and ventricular septal structures and discordant ventriculo-arterial connections. The descending aorta filled through the arterial duct, while there was retrograde filling of the aortic arch and ascending aorta.
Table 1.
Cardiac catheterization data
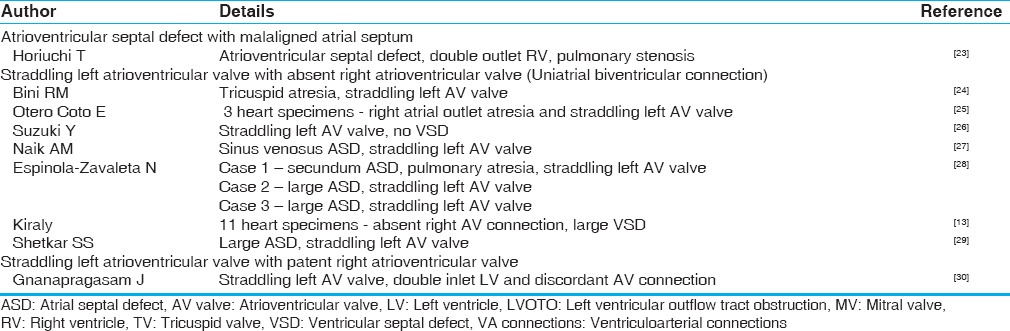
Although two separate and well-formed orifices had been shown within the right atrioventricular valve, the precise anatomy of the overriding right atrioventricular junction was far from clear. Despite multiple attempts, it was not possible to obtain an “en-face” view of the right atrioventricular junction. Acquisition of 3D data, furthermore, was not possible due to breathing artifacts. We therefore used X plane imaging, using the X7-2 matrix transducer of Philips iE33 echocardiography machine (Philips medical systems, Netherlands), with the other plane perpendicular to the imaging plane. In this way, it proved possible to obtain a short axis view of the right atrioventricular junction. This confirmed its solitary nature, seen best during diastole and showed how it divided during systole to form two separate orifices, each committed independently to one or other of the ventricles [Figure 4 and Online Video 2].
Figure 4.
The panels show X plane imaging, with the secondary plane (shown to the right) almost perpendicular to the primary imaging plane. This reveals the “enface” view of the solitary atrioventricular junction in early diastole (panel A) and mid diastole (panel B). In Panel C, taken at end diastole, and panel D in systole, it is possible to recognize two well-formed valvar orifices, each committed to its own ventricle. The electrocardiographic signal at the bottom of each panel shows the timing of the cardiac cycle
Since we had demonstrated two well-formed and separate atrioventricular orifices, in the absence of interventricular shunting, we considered that a biventricular surgical repair, incorporating wide atrial septectomy and the double switch operation would be a potential therapeutic option. In view of young age of the patient, nonetheless, coupled with the borderline size of the morphologically right ventricle and doubt concerning the competence of the right-sided component of the solitary atrioventricular valve, we opted to confine initial treatment to atrial septectomy and ligation of the arterial duct. The cardiac anatomy was confirmed intraoperatively. The patient made a good postoperative recovery, with systemic saturations measured at 85%. She is currently progressing well, and is planned for reassessment of the right ventricular size prior to giving further consideration to a subsequent double switch operation.
DISCUSSION
There has been tremendous growth and development in the field of cardiac imaging over the recent decades. Some cases, nonetheless, remain challenging. This is especially true in the assessment of the atrioventricular junctions and valves in patients with so-called complex congenital heart disease. Three-dimensional (3D) echocardiography has improved our ability to understand the morphology of the atrioventricular valves, but this technique has limited utility in younger children. So-called “X plane imaging” allows the operator simultaneously to image the heart in two orthogonal planes. Such simultaneous imaging provides better understanding of the anatomy of the atrioventricular junctions, and their relationship to the atrial and ventricular cavities, thus providing (3D) perspectives even when, as in our patient, 3D echocardiography was not possible. The presence of this additional modality is then a boon for the echocardiographer when performing subsequent interrogations. Had X-plane imaging not been available in our patient, it would not have been possible to assess the atrioventricular junction in its short axis, our interrogation confirming it to be a solitary rather than a common structure.
Our patient was all the more unusual in that the valve guarding the overriding solitary atrioventricular junction was divided into separate right and left atrioventricular orifices with each valvar orifice then committed to its own ventricle [Figure 2, right hand panel]. A comparable situation is seen in the so-called standard ostium primum defect, in which the bridging tongue which divides the common atrioventricular junction into separate right and left valvar orifices is bound down to the ventricular septal crest. Because of this feature, shunting through the ostium primum defect is confined at atrial level, the channel permitting shunting being an atrioventricular rather than an atrial septal defect. In our patient, the binding-down of the separating tongue of valvar tissue produced the apparently paradoxical situation in which there was no potential for ventricular shunting, despite the obvious gap between. The atrial and ventricular septal structures [Figure 2]. Some might consider this to represent an “intact ventricular septum”. Comparison with the more typical cases of absent left atrioventricular connection with straddling atrioventricular valve, in the absence of dual valvar orifices, however, reveals the obvious feature of deficient ventricular septation. Cardiac magnetic resonance imaging (MRI) and computed tomography are alternative imaging techniques. Both present difficulties, since general anesthesia is required for optimal MRI in infants, while computed tomography (CT) involves exposure to ionizing radiation. It is cardiac catheterization that still provides the perfect mix of hemodynamic, functional, and anatomic data. It remains best suited for clinical situations such as produced by our patient. It too, nonetheless, has major limitations in being invasive and dependent on the projections achieved to provide two-dimensional imaging. Although not ideal for evaluating the atrioventricular valves, catheter angiography can demonstrate the anatomy in acceptable manner, especially when performed in a biplane catheterization laboratory.
What is a double outlet atrium?
If we return to the morphologic aspects of the anatomy revealed in our patient, then it should be recognized that double outlet atrium is a rare cardiac anomaly in which one of the atriums connects to both ventricles. It was Van Mierop and his colleagues[1] who provided the initial description as a variant of the so-called “endocardial cushion defect”, now better understood as an atrioventricular septal defect in the setting of common atrioventricular junction. In this setting, it is the malalignment of the atrial septum relative to the muscular ventricular septum that results in double outlet from either the left or the right atrium. In such hearts, nonetheless, because of the commonality of the atrioventricular junctions, the atriums themselves must communicate through an ostium primum defect.[2,3,4,5,6,7,8,9,10,11,12] Double outlet atrium, however, is a non-specific term. It is always present, for example, when there is straddling and overriding of one or other of the two separate atrioventricular valves. Should the straddling orifice itself be divided in this arrangement, there can seemingly be three atrioventricular valves.[17,18,19,20,21,22] The presence of the straddling valve is again the consequence of malalignment between the atrial and ventricular septal structures, but with separate atrioventricular junctions rather than a common atrioventricular junction. Depending of the extent of overriding of the straddling valve, there will be variable hypoplasia of one of the ventricles.
Straddling and overriding of an atrioventricular valve, nonetheless, can also be found when one of the atrioventricular junctions is absent, as was the situation in our patient. This produces the very rare arrangement of the uniatrial but biventricular connection [Figure 2]. Unlike the situation in the patients with atrioventricular septal defects, shunting between the atriums when one atrioventricular connection is absent will perforce be through the oval fossa. The atrioventricular junction, furthermore, is solitary, and not common as in hearts with atrioventricular septal defect. It is this distinction of the solitary atrioventricular junction, as opposed to a common junction, that is the key to understanding. It clarifies the nomenclature, as well as influencing the choice of surgical repair. The very presence of multiple attempts at classification [Tables 2 and 3] shows that distinction of the varied forms of “double outlet atrium” remains far from clear.[29,31] The feature that differentiates the solitary junction from the common junction is the location and attachment of the leading edge of the atrial septum. If the leading edge of the atrial septum fails to reach the parietal part of the atrioventricular junction then there must be an ostium primum defect, and by definition, there will be a common atrioventricular junction. Should the leading edge of the atrial septum be fused with the parietal component of the atrioventricular junction then the left-sided atrioventricular connection will be absent, and the persisting atrioventricular junction will drain only one of the atriums.[13,14,15,16] In their study of 14 autopsied specimens with uniatrial but biventricular connections, Kiraly and colleagues[13] emphasized the varied morphology of the right and left components of the solitary atrioventricular junction. In most of the hearts, the morphology of the valve closely resembled that of a common atrioventricular valve, despite the fact that it was supported by only one atrioventricular junction. Only rarely did the gross appearance resemble that of either the normal mitral or tricuspid valves. Because of this the investigators[13] suggested that the valves were best labelled as being right and left rather than tricuspid or mitral. In none of the hearts, furthermore, was there evidence of the other phenotypic features of atrioventricular septal defect with common atrioventricular junction such as elongation of the left ventricular outflow tract.
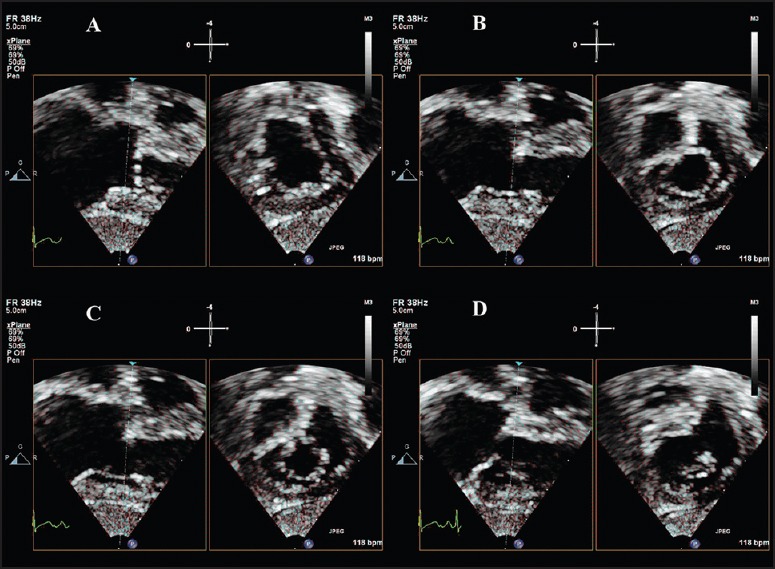
Table 2.
Reported examples of various types of double outlet right atrium
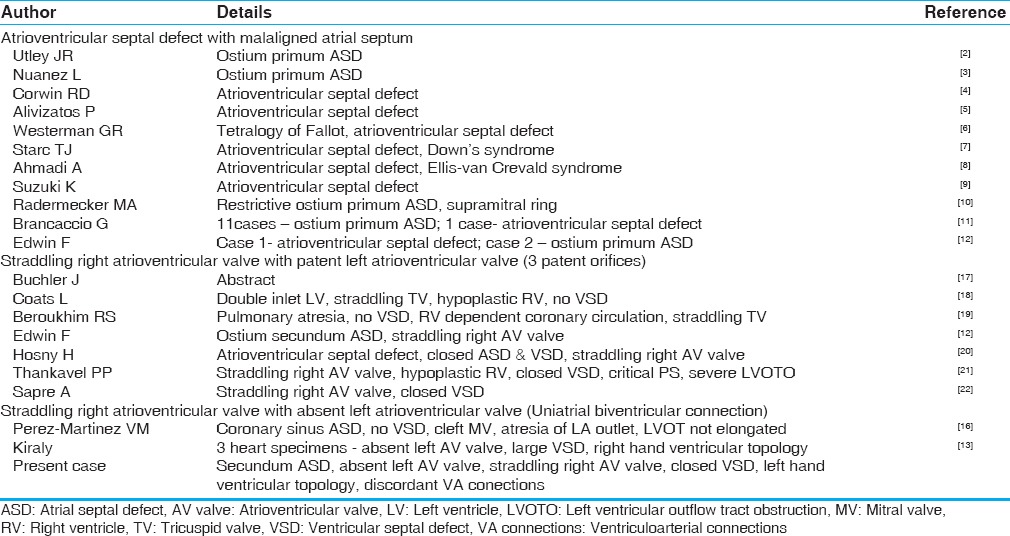
Table 3.
Reported examples of various types of double outlet left atrium
Is the ventricular septum intact?
It seems counter-intuitive in our patient to suggest that there can be a ventricular septal defect despite the absence of any potential for interventricular shunting. The malalignment between the atrial and ventricular septal structures, nonetheless, points unequivocally to the presence of deficient ventricular septation [Figure 2]. This apparently paradoxical situation is also found in the setting of the ostium primum defect in which the bridging leaflets of the common atrioventricular valve are fused to the crest of the muscular interventricular septum. Because of this feature shunting across the atrioventricular septal defect is confined at atrial level, despite the fact that the large part of the septal defect itself is distal relative to the plane of the atrioventricular junction. It is a comparable situation that is present in our patient, with each of the dual orifices in the right-sided atrioventricular valve being connected to its own ventricle, with the dividing tongue separating the orifices closing the deficiency of the ventricular septum.
Why is this distinction so important?
The outcomes of surgery for atrioventricular septal defect have been impressive with achievement of successful biventricular repair in the majority. Straddling atrioventricular valve on the other hand is a challenging subset to manage during surgical repairs for various cardiac anomalies. It is essential for proper understanding, therefore, to distinguish double outlet atrium due to straddling atrioventricular valve as opposed to the arrangement found with atrioventricular septal defect and common atrioventricular junction. It is our hope that in our patient, each of the dual orifices will eventually function as a separate atrioventricular valve subsequent to biventricular surgical repair. The current absence of any regurgitation or stenosis makes the option of biventricular repair very appealing. The situation is further complicated, however, by the presence of left handed ventricular topology and discordant ventriculoarterial connections. Any subsequent attempt at biventricular repair will require a double switch operation.
CONCLUSION
Double outlet atrium is generic term that described hearts in which one of the atriums connects to both the ventricles. Uncommonly, this occurs in the setting of atresia of one of the atrioventricular connections, with straddling of the other atrioventricular valve. Detailed evaluation of the atrioventricular junctional anatomy serves to differentiate this arrangement from the more common variant of double outlet atrium found with atrioventricular septal defect and common atrioventricular junction. The differentiation is important for accurate nomenclature, as well as for appropriate surgical management.
Videos available on www.annalspc.com
Footnotes
Source of Support: Nil
Conflict of Interest: None declared
REFERENCES
- 1.Van Mierop LH. Pathology and pathogenesis of endocardial cushion defects: Surgical implications. In: Davila JC, editor. Second Henry Ford Hospital International Symposium on Cardiac Surgery. New York: Applenton-Century-Crofts; 1977. pp. 201–7. [Google Scholar]
- 2.Utley JR, Noonan JA, Walters LR, Frist RA. Anomalous position of atrial septum with anomalous pulmonary and systemic drainage. Correction including ligation of persistent left superior vena cava. J Thorac Cardiovasc Surg. 1974;67:730–2. [PubMed] [Google Scholar]
- 3.Nunez L, Aguado MG, Sanz E, Perez-Martinez V. Surgical repair of double-outlet right atrium. Ann Thorac Surg. 1984;37:164–6. doi: 10.1016/s0003-4975(10)60308-6. [DOI] [PubMed] [Google Scholar]
- 4.Corwin RD, Singh AK, Karison KE. Double-outlet right atrium: A rare endocardial cushion defect. Am Heart J. 1983;106:1156–7. doi: 10.1016/0002-8703(83)90667-1. [DOI] [PubMed] [Google Scholar]
- 5.Alivizatos P, Anderson RH, Macartney FJ, Zuberbuhler JR, Stark J. Atrioventricular septal defect with balanced ventricles and malaligned atrial septum: Double-outlet right atrium: Report of two cases. J Thorac Cardiovasc Surg. 1985;89:295–7. [PubMed] [Google Scholar]
- 6.Westerman GR, Norton JB, Van Devanter SH. Double-outlet right atrium associated with tetralogy of Fallot and common atrioventricular valve. J Thorac Cardiovasc Surg. 1986;91:205–7. [PubMed] [Google Scholar]
- 7.Starc TJ, Bierman FZ, Bowman FO, Jr, Steeg CN, Wang NK, Krongrad E. Pulmonary venous obstruction and atrioventricular canal abnormalities: Role of cor triatriatum and double outlet right atrium. J Am Coll Cardiol. 1987;9:830–3. doi: 10.1016/s0735-1097(87)80239-5. [DOI] [PubMed] [Google Scholar]
- 8.Ahmadi A, Mocellin R, Spillner G, Gildein HP. Atrioventricular septal defect with double-outlet right atrium. Pediatr Cardiol. 1989;10:170–3. doi: 10.1007/BF02081683. [DOI] [PubMed] [Google Scholar]
- 9.Suzuki K. DORA and complete AVSD with abnormal findings of the biopsied lung. Cardiol Young. 1994;4:402. [Google Scholar]
- 10.Radermecker MA, Chauvaud S, Carpentier A. Double-outlet right atrium with restrictive ostium primum and incomplete supravalvular ring presenting as congenital mitral valve stenosis. J Thorac Cardiovasc Surg. 1995;109:804–5. doi: 10.1016/S0022-5223(95)70364-0. [DOI] [PubMed] [Google Scholar]
- 11.Brancaccio G, Amodeo A, Rinelli G, Filippelli S, Sanders SP, Di Donato RM. Double-outlet right atrium: Anatomic and clinical considerations. Ann Thorac Surg. 2007;83:619–21. doi: 10.1016/j.athoracsur.2006.09.080. [DOI] [PubMed] [Google Scholar]
- 12.Edwin F, Kinsley RH, Mamorare HM, Govendrageloo K. The spectrum of double-outlet right atrium including hearts with three atrioventricular valves. Eur J Cardiothorac Surg. 2012;41:947–9. doi: 10.1093/ejcts/ezr073. [DOI] [PubMed] [Google Scholar]
- 13.Kiraly L, Hubay M, Cook AC, Ho SY, Anderson RH. Morphologic features of the uniatrial but biventricular atrioventricular connection. J Thorac Cardiovasc Surg. 2007;133:229–34. doi: 10.1016/j.jtcvs.2006.08.067. [DOI] [PubMed] [Google Scholar]
- 14.Ho SY, Anderson RH, Macartney FJ, Goodwin A, Becker AE, Wenink AC, et al. Straddling atrioventricular valve with absent atrioventricular connection: Report of 10 cases. Br Heart J. 1982;47:344–52. doi: 10.1136/hrt.47.4.344. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Aiello V, Ho SY, Anderson RH. Absence of one atrioventricular connection associated with straddling atrioventricular valve: Distinction of a solitary from a common valve and further considerations on the diagnosis of ventricular topology. Am J Cardiovasc Pathol. 1990;3:107–13. [PubMed] [Google Scholar]
- 16.Pérez-Martínez VM, García-Fernandez F, Oliver-Ruiz J, Nuñez-Gonzalez L. Double-outlet right atrium with two atrioventricular valves and left atrial outlet atresia. J Am Coll Cardiol. 1984;3:375–80. doi: 10.1016/s0735-1097(84)80022-4. [DOI] [PubMed] [Google Scholar]
- 17.Buchler J, Rabelo R, Marino R, David I, Van Praagh R. Vol. 223. London: World congress of paediatric cardiology; 1980. Double outlet right atrium: Autopsied case of newly recognised entity (abstr). Book of abstracts. [Google Scholar]
- 18.Coats L, Runnett C, Satchithananda DK. Double outlet right atrium with coexisting double inlet left ventricle and concordant ventriculoarterial connections: A fascinating variant of the Holmes heart. Cardiol Young. 2010;20:587–9. doi: 10.1017/S1047951110000946. [DOI] [PubMed] [Google Scholar]
- 19.Beroukhim RS, Geva T. Echocardiographic features of double-outlet right atrium and straddling tricuspid valve with intact ventricular septum: A rare cardiac anomaly associated with pulmonary atresia and single coronary artery ostium. J Am Soc Echocardiogr. 2010;23:580.e5–10. doi: 10.1016/j.echo.2009.09.027. [DOI] [PubMed] [Google Scholar]
- 20.Hosny H, Abdel Salam S, Wally H, Yacoub M. Double outlet right atrium with three atrioventricular valves. Glob Cardiol Sci Pract. 2014;2014:117–22. doi: 10.5339/gcsp.2014.32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Thankavel PP, Gabbert B, Ramaciotti C. Double outlet right atrium associated with hypoplastic right heart structures and aortic stenosis: Echocardiographic features. Echocardiography. 2014;31:E163–5. doi: 10.1111/echo.12565. [DOI] [PubMed] [Google Scholar]
- 22.Sapre A, Gopalraj SS, Kottayil BP, Raman KK. An unusual example of isolated double-orifice tricuspid valve. Ann Pediatr Cardiol. 2013;6:162–3. doi: 10.4103/0974-2069.115269. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Horiuchi T, Saji K, Osuka K, Sato K, Okada Y. Successful correction of double outlet left atrium associated with complete atrioventricular canal and l-loop double outlet right ventricle with stenosis of the pulmonary artery. J Cardiovasc Surg (Torino) 1976;17:157–61. [PubMed] [Google Scholar]
- 24.Bini RM, Pellegrino PA, Mazzucco A, Gallucci V, Milanesi O, Maddalena F, et al. Tricuspid atresia with double-outlet left atrium. Chest. 1980;78:109–11. doi: 10.1378/chest.78.1.109. [DOI] [PubMed] [Google Scholar]
- 25.Coto EO, Calabro R, Marsico F, Lopez Arranz JS. Right atrial outlet atresia with straddling left atrioventricular valve. A form of double outlet atrium. Br Heart J. 1981;45:317–24. doi: 10.1136/hrt.45.3.317. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Suzuki Y, Hamada Y, Miura M, Handa K, Horiuchi T, Ogata H. Double-outlet left atrium with intact ventricular septum. Ann Thorac Surg. 1988;45:332–4. doi: 10.1016/s0003-4975(10)62476-9. [DOI] [PubMed] [Google Scholar]
- 27.Naik AM, Nabar AA, Dalvi BV. Double outlet left atrium. Indian Heart J. 1997;49:418–20. [PubMed] [Google Scholar]
- 28.Espinola-Zavaleta N, Vargas-Barron J, Hernandez-Morales G, Keirns C, Roemro-Cardenas A, Roldan J. Clinical and echocardiographic aspects of double outlet left atrium. J Am Soc Echocardiogr. 2002;15:86–9. doi: 10.1067/mje.2002.115888. [DOI] [PubMed] [Google Scholar]
- 29.Shetkar SS, Kothari SS. Double-outlet left atrium: Ventriculo-atrial malalignment defect. Ann Pediatr Cardiol. 2013;6:158–61. doi: 10.4103/0974-2069.115266. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Gnanapragasam J, Houston A, Anderson RH. Double outlet left atrium with double inlet left ventricle and discordant atrioventricular connection. Cardiol Young. 1991;1:155–7. [Google Scholar]
- 31.Anderson RH. How best to explain unexpected arrangements of the atrioventricular valves? Ann Pediatr Cardiol. 2013;6:152–4. [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


