Abstract
Plastic bronchitis, a rare but serious clinical condition, commonly seen after Fontan surgeries in children, may be a manifestation of suboptimal adaptation to the cavopulmonary circulation with unfavorable hemodynamics. They are ominous with poor prognosis. Sometimes, infection or airway reactivity may provoke cast bronchitis as a two-step insult on a vulnerable vascular bed. In such instances, aggressive management leads to longer survival. This report of cast bronchitis discusses its current understanding.
Keywords: Bronchial casts, fontan complications, fontan surgery, maladaptation, plastic bronchitis, Trichrome stain
INTRODUCTION
Plastic bronchitis is diagnosed by expectoration of gelatinous or rubbery casts of bronchial airways.[1] It is seen in children after 1-4% of Fontan surgeries. Very rarely it is seen after Glenn shunt, Fallot's tetralogy repair, arterial switch operation and other cardiac surgeries.[2] It occurs in adults with bronchiectasis, asthma, tuberculosis, cystic fibrosis, chronic bronchitis, lung transplant, H1N1 influenza, heart failure, rheumatoid arthritis, or amyloidosis.[3] We highlight the histopathological findings and the management principles.
CASE REPORT
A 5-year-old boy weighing 18 kg with oxygen saturations of 81% and hemoglobin of 16.3 g/dl underwent off-pump fenestrated extracardiac Fontan surgery. He had right atrial isomerism, double inlet left ventricle with good systolic function, severe pulmonary stenosis, and previously palliated by nonpulsatile bidirectional Glenn shunt at 15 months of age. His mean pulmonary artery pressure was 15 mmHg, and atrial and ventricular end diastolic pressures were 10 and 14 mmHg, respectively. The pulmonary vascular resistance and Nakata indices were 1.83 wood units and 213 mm2, respectively. There were no significant aortopulmonary collaterals.
Immediate postoperative Fontan pressure was 12 mmHg, and he was discharged uneventfully with oximeter saturation of 92% due to the fenestration. He received bosentan and sildenafil, diuretics along with warfarin and aspirin. Pulmonary vasodilators were initiated, as the Glenn pressures were 15 mmHg. He presented with a wheezy respiratory infection 2 months after the surgery, with markedly reduced air entry over the right lower lobe and hyperresonant note on percussion. A chest X-ray showed a hyperinflated right lower zone due to obstructive emphysema. In the hospital, he expectorated mucoid material [Figure 1a], containing a bronchial cast [Figure 1b]. Microscopy showed entrapped leucocytes of type I inflammatory cast [Figure 2a] and abundant mucin [Figure 2b] often noted in type II casts. Echocardiogram showed optimal Fontan flows with good ventricular function. After increasing the dose of pulmonary vasodilators, he recovered well on a 9-month follow-up with normal serum proteins.
Figure 1.
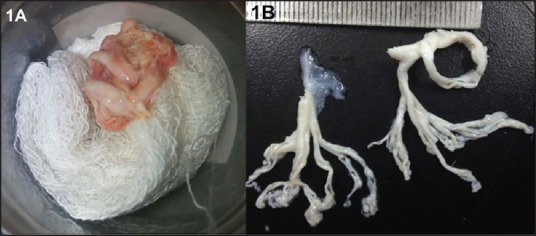
(a) Expectorated cast material in a receptacle. (b) White tenacious mucoid cast showing tree-like branching of the bronchial tree
Figure 2.
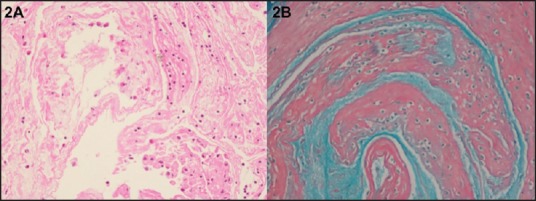
(a) Histology with hematoxylin and eosin stain at ×200 shows the proteinaceous material, entrapped lymphocytes, neutrophils, and eosinophils. (b) Trichrome stain shows both mucoid material and fibrinous material, showing features of both type I and II casts
DISCUSSION
Casts are classified as type I inflammatory casts with cellular infiltration and dense fibrin and type II acellular casts with mucin and few mononuclear cells after special stains.[4] In clinical practice, overlaps often exist. Casts form due to:
Break in mucosal integrity and alveolar capillary barrier with the a leak of proteinaceous material;
Endobronchial lymphatic seepage, and
Airway inflammation with exudation.[5]
Risk factors for plastic bronchitis include prolonged chest tube drainage, postsurgical chylothorax or ascites, need for aortopulmonary collateral coiling, and aortic arch reconstruction.[6] These indicate a suboptimal adaptation to cavopulmonary circulation. Unpredictably, it may rarely occur in patients with optimal Fontan hemodynamics.
Early occurrence of plastic bronchitis after Fontan surgery is ominous. If cast bronchitis is provoked by infection or airway reactivity, the prognosis is not too bad.[3] The current understanding suggests a two-step model of insult, with inflammation superimposed on a dysregulated mucus secretion in a vulnerable vascular bed or an endobronchial lymph leakage.[3] This model explains the favorable clinical course in few patients after symptomatic treatment. Recurrent bouts warrant a hemodynamic study to exclude any obstructions in Fontan circuit, as an echocardiogram alone may not be sufficient to exclude such obstructions.
Initial management include bronchodilators, steroids, inhaled hypertonic saline, mucolytics, antibiotics, bronchoscopic toilet, and chest physiotherapy.[7] Drugs such as carvidelol prolong ventricular relaxation, improve ventricular function, and optimize hemodynamics. Pulmonary vasodilators reduce vascular resistance, and macrolides have mucoregulatory and anti-inflammatory effect.
Topical treatment targets the cast contents such as inhaled heparin, urokinase or tissue plasminogen activator that acts on fibrin, recombinant DNAse (dornase alpha) that acts on cellular material, and nebulized N-acetyl cysteine that acts on mucin. Such targeted therapy may not always be feasible. Optimization of hemodynamics is done by fenestrating the Fontan circuit, removal of all obstructions (pulmonary artery, vein, aortic narrowing), reconversion to Glenn shunt, and innominate to atrial shunt.[7]
Before embarking on heart transplantation for refractory patients, addressing lymphatic seepage by glue embolization of lymphatic tracts identified on magnetic resonance and thoracic duct ligation may be tried.[8,9] Every patient may need an individually tailored strategy.
CONCLUSIONS
Plastic bronchitis, a rare and serious clinical problem after Fontan surgery, may even be fatal. Nonresponding patients should have the optimization of unfavorable hemodynamics. However, not all patients with bronchial casts have a uniformly poor outcome. If there is an inflammatory correctable reason for the problem, the prognosis may not be as unfavorable.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Johnson RS, Sita-Lumsden EG. Plastic bronchitis. Thorax. 1960;15:325–32. doi: 10.1136/thx.15.4.325. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Grutter G, Di Carlo D, Gandolfo F, Adorisio R, Alfieri S, Michielon G, et al. Plastic bronchitis after extracardiac Fontan operation. Ann Thorac Surg. 2012;94:860–4. doi: 10.1016/j.athoracsur.2012.04.043. [DOI] [PubMed] [Google Scholar]
- 3.Madsen P, Shah SA, Rubin BK. Plastic bronchitis: New insights and a classification scheme. Paediatr Respir Rev. 2005;6:292–300. doi: 10.1016/j.prrv.2005.09.001. [DOI] [PubMed] [Google Scholar]
- 4.Seear M, Hui H, Magee F, Bohn D, Cutz E. Bronchial casts in children: A proposed classification based on nine cases and a review of the literature. Am J Respir Crit Care Med. 1997;155:364–70. doi: 10.1164/ajrccm.155.1.9001337. [DOI] [PubMed] [Google Scholar]
- 5.Caruthers RL, Kempa M, Loo A, Gulbransen E, Kelly E, Erickson SR, et al. Demographic characteristics and estimated prevalence of Fontan-associated plastic bronchitis. Pediatr Cardiol. 2013;34:256–61. doi: 10.1007/s00246-012-0430-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Schumacher KR, Singh TP, Kuebler J, Aprile K, O’Brien M, Blume ED. Risk factors and outcome of Fontan-associated plastic bronchitis: A case-control study. J Am Heart Assoc. 2014;3:e000865. doi: 10.1161/JAHA.114.000865. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Brogan TV, Finn LS, Pyskaty DR, Jr, Redding GJ, Ricker D, Inglis A, et al. Plastic bronchitis in children: A case series and review of the medical literature. Pediatr Pulmonol. 2002;34:482–7. doi: 10.1002/ppul.10179. [DOI] [PubMed] [Google Scholar]
- 8.Shah SS, Drinkwater DC, Christian KG. Plastic bronchitis: Is thoracic duct ligation a real surgical option? Ann Thorac Surg. 2006;81:2281–3. doi: 10.1016/j.athoracsur.2005.07.004. [DOI] [PubMed] [Google Scholar]
- 9.Dori Y, Keller MS, Rychik J, Itkin M. Successful treatment of plastic bronchitis by selective lymphatic embolization in a Fontan patient. Pediatrics. 2014;134:e590–5. doi: 10.1542/peds.2013-3723. [DOI] [PubMed] [Google Scholar]


