Abstract
OBJECTIVE
To assess knowledge, attitudes, and practices of obstetrician–gynecologists (ob-gyns) regarding vaccination of pregnant women during the 2009 H1N1 pandemic.
METHODS
From February to July 2010, a self-administered mail survey was conducted among a random sample of American College of Obstetricians and Gynecologists (the College) members involved in obstetric care. To assess predictors of routinely offering influenza vaccination, adjusted prevalence ratios and 95% confidence intervals (CIs) were calculated from survey data.
RESULTS
Among 3,096 survey recipients, 1,310 (42.3%) responded to the survey, of whom 873 were eligible for participation. The majority of ob-gyns reported routinely offering both seasonal and 2009 H1N1 influenza vaccination to their pregnant patients (77.6% and 85.6%, respectively) during the 2009–2010 season; 21.1% and 13.3% referred patients to other specialists. Reported reasons for not offering vaccination included inadequate reimbursement, storage limitations, or belief that vaccine should be administered by another provider. Seasonal and 2009 H1N1 influenza vaccination during the first trimester was not recommended by 10.6% and 9.6% of ob-gyns, respectively. Predictors of routinely offering 2009 H1N1 influenza vaccine included: considering primary care and preventive medicine a very important part of practice (adjusted prevalence ratio 1.2, CI 1.01–1.4); observing serious conditions attributed to influenza-like illness (adjusted prevalence ratio 1.1, CI 1.02–1.1); personally receiving 2009 H1N1 influenza vaccination (adjusted prevalence ratio 1.2, CI 1.1–1.4); and practicing in multispecialty group (adjusted prevalence ratio 1.1, CI 1.1–1.2). Physicians in solo practice were less likely to routinely offer influenza vaccine (adjusted prevalence ratio 0.8, CI 0.7–0.9).
CONCLUSION
Although most ob-gyns routinely offered influenza vaccination to pregnant patients, vaccination coverage rates may be improved by addressing logistic and financial challenges of vaccine providers.
Pregnant women are at increased risk for influenza-related morbidity, adverse pregnancy outcomes, and mortality, especially during pandemics.1–9 During the 2009 H1N1 pandemic, pregnant women accounted for approximately 5% of influenza-associated deaths in the United States, although they represent only approximately 1% of the population.6
Influenza vaccination during pregnancy is the most effective way to prevent influenza virus infection among pregnant women10 and their infants younger than 6 months of age.11,12 Although administration of inactivated influenza vaccine is recommended to all women who are pregnant during the influenza season, regardless of pregnancy trimester,10,13 the vaccination coverage among pregnant women has been historically low, rarely exceeding 15% during nonpandemic years.10,14 The reasons for low uptake of vaccination during pregnancy include factors related to the lack of vaccine acceptance by pregnant women, as well as barriers among health care providers, including absence of financial incentives, liability concerns, logistic obstacles, and lack of confidence about vaccine safety and benefits.15–22
Obstetrician– gynecologists (ob-gyns), who are often the only providers of health care during pregnancy, play a critical role in preventing influenza in their patients through vaccination and implementing recommended diagnostic, treatment, and infection control practices. Understanding the barriers that prevent ob-gyns from administering influenza vaccination is critical for attaining high vaccination rates among pregnant women. In February 2010, just after the peak of the 2009 H1N1 pandemic, we conducted a survey among the national sample of U.S. ob-gyns to assess their knowledge, attitudes, and practices regarding influenza vaccination during pregnancy, and the barriers and facilitators to influenza vaccination.
MATERIALS AND METHODS
A self-administered survey was mailed to a U.S. nationally representative random sample of 3,116 ob-gyns using the American College of Obstetricians and Gynecologists database. Only ob-gyns currently involved in obstetric patient care were eligible to participate; those not eligible were instructed to return the uncompleted survey. The sampling frame consisted of 33,685 practicing ob-gyns who were College fellows or junior fellows. The survey was accompanied by a cover letter and prepaid envelope; no incentives were offered to the participants. The initial mailing was sent in February 2010. Second, third, and fourth mailings were sent to all nonrespondents at 4- to 5-week intervals. The survey included questions about the basic demographic information of respondents and their patients, respondents’ experiences with serious conditions attributed to influenza-like illness among pregnant women in their practice (during both 2008–2009 influenza season and 2009 H1N1 pandemic), and respondents’ attitudes and practices regarding influenza vaccination of pregnant women (with both seasonal and 2009 H1N1 influenza vaccines) during the 2009 H1N1 pandemic. Five weeks after the fourth mailing, a short questionnaire was sent to all nonrespondents to gather data for an assessment of possible nonresponse bias in which their responses were compared with those of study participants.
Analyses were performed using SAS 9.1 and SPSS 16.0. We calculated frequency distributions of responses to each question in the survey, excluding nonresponses from the denominators. For multilevel responses, we performed multiple tests using SAS “MULTTEST” procedure. Two-sided Cochran-Armitage linear trend tests23 and a significance level of P<.05 were used to compare differences in responses for the 2008–2009 and 2009–2010 influenza seasons, and for seasonal and 2009 H1N1 influenza vaccines.
To assess the association between selected characteristics and routinely offering 2009 H1N1 influenza vaccine by ob-gyns, we conducted log-binomial regression analyses, which included variables on the basis of their univariable association with the outcome (routinely offering 2009 H1N1 influenza vaccine); adjusted prevalence ratios and 95% confidence intervals (CIs) were calculated using SAS “GENMOD” log-binomial regression capability.24 Using this approach, log-probability link function is used, and the adjusted estimates of coefficients of the examined factors represent logarithms of the adjusted prevalence ratios. Because of multicollinearity between three variables (practice type, considers primary care or preventive medicine an important part of practice, and received 2009 H1N1 influenza vaccination themselves), three separate models were constructed. The project was reviewed for human subject concerns by the Centers for Disease Control and Prevention and the College and was determined to qualify for exempt status.
RESULTS
Of the 3,116 surveys mailed, 20 were returned as undeliverable. Among the ob-gyns who received the survey, 1,784 did not respond, 2 refused participation, and 1,310 returned the survey for a response rate of 42.3% (1,310 of 3,096). Of 1,310 providers who returned the surveys, 873 (66.6%) were providing obstetric care during the 2009–2010 influenza season and therefore were eligible to participate in the study, and their responses were included in the analyses.
The respondents had a mean age of 49 years, approximately half were female, and their average duration of clinical practice was 17 years (Table 1). The majority of respondents were practicing in a group obstetrics-gynecology practice (48.1%), followed by solo practice (16.4%), multispecialty group practice (12.4%), university full-time faculty and practice (11.2%), and other (11.9%, including Health Maintenance Organization, military, and combination of these). Almost all respondents considered primary care or preventive medicine an important part of their clinical practice. Among the patient population of the respondents, a third were eligible for Medicaid, and race or ethnicity distribution was as follows: 54.9% were non-Hispanic white, 15.2% were non-Hispanic African American, 17.8% were Hispanic, 5.3% were Asian or Pacific Islander, and 1.3% were Native American.
Table 1.
Characteristics of Obstetrician–Gynecologists Participating in the Survey (n=873)*
| Characteristics | Percentage or Mean (Range) |
|---|---|
| Sex | |
| Female | 51.1 |
| Male | 48.9 |
| Average age (y) | 49 (30–85) |
| Average years in practice | 17 (0.5–52) |
| Type of practice | |
| Group obstetrics-gynecology | 48.1 |
| Solo | 16.4 |
| Multispecialty group | 12.4 |
| University full-time faculty and practice | 11.2 |
| Other | 11.9 |
| Consider primary care, preventive medicine an important part of practice | |
| Very important | 45.8 |
| Important | 49.4 |
| Not important | 3.8 |
| Average estimated % of patients eligible for Medicaid | 33.4 |
| Average estimated % of patients by race or ethnicity† | |
| Non-Hispanic white | 54.9 |
| Non-Hispanic African American | 15.2 |
| Hispanic | 17.8 |
| Asian or Pacific Islander | 5.3 |
| Native American | 1.3 |
| Multiracial | 2.6 |
| Other | 1.0 |
Sample size reduced owing to missing values.
Numbers might not add to 100% because of rounding.
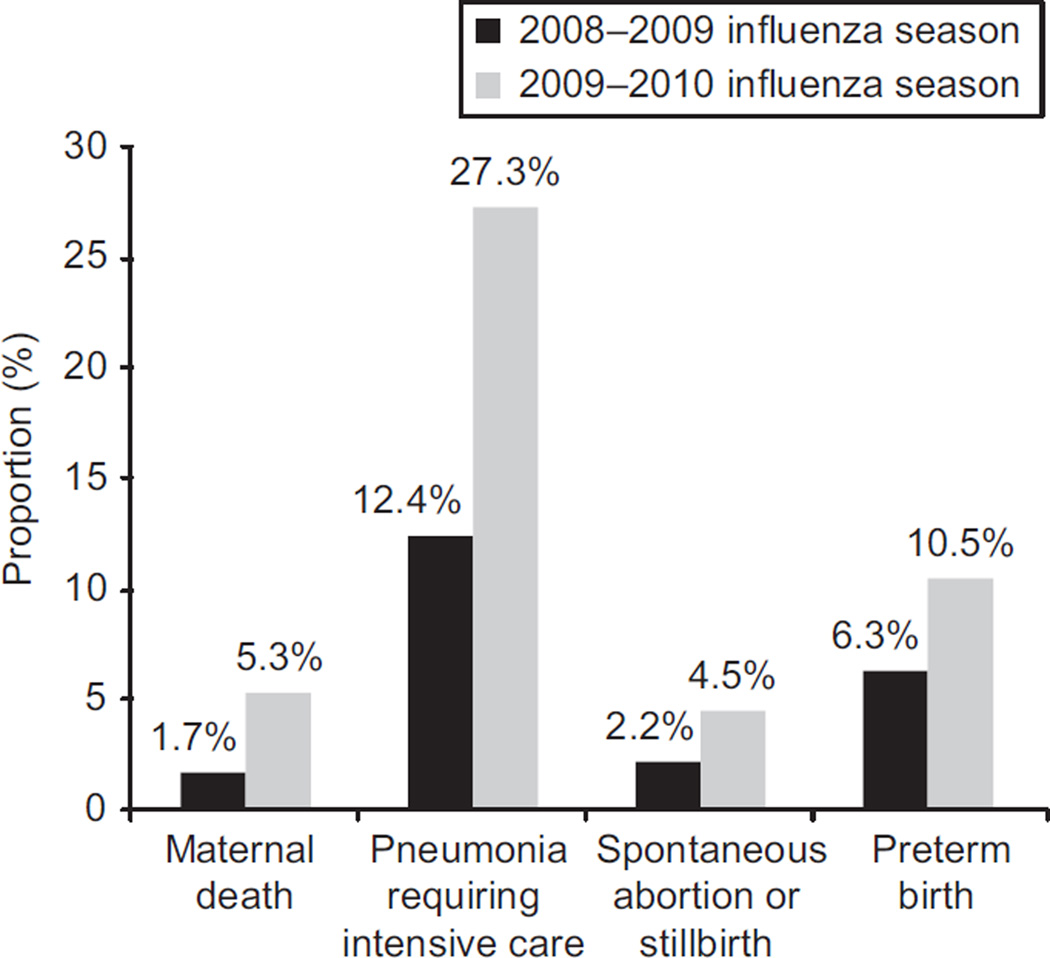
In response to the question “During last year’s (2008–2009) and this year’s (2009–2010) influenza seasons, have you seen the following conditions in your practice that you attribute to influenza-like illness,” the proportion of ob-gyns who reported observing at least one of the serious conditions (maternal death, pneumonia requiring intensive care, spontaneous abortion or stillbirth, or preterm birth) doubled from 14.6% during the 2008–2009 influenza season to 31.1% during the 2009–2010 influenza season (P<.001). During the 2009 H1N1 pandemic, survey results indicated a threefold increase in the proportion of ob-gyns who reported observing maternal deaths, twofold increase in the proportion observing pneumonias requiring intensive care, twofold increase in the proportion observing spontaneous abortions or stillbirths, and 50% increase in the proportion observing preterm births attributed to influenza-like illness (based on their clinical judgment) compared with the previous influenza season (Fig. 1).
Fig. 1.
Proportion of U.S. obstetrician– gynecologists who reported observing at least one of the serious conditions (maternal death, pneumonia requiring intensive care, spontaneous abortion or stillbirth, or preterm birth) in their practices that they attributed to influenza-like illness among pregnant women during the 2008–2009 influenza season (black bars) and 2009–2010 influenza seasons (gray bars).
Kissin. Influenza Vaccination During Pregnancy. Obstet Gynecol 2011.
During the 2009 H1N1 pandemic (2009–2010 influenza season), the majority of ob-gyns reported routinely offering influenza vaccination, both seasonal (77.6%) and 2009 H1N1 (85.6%), to their pregnant patients; most of the remaining providers reported referring their patients to other providers for seasonal (21.1%) and 2009 H1N1 (13.3%) vaccines. Only approximately 1% of providers neither offered nor referred their pregnant patients for influenza vaccination (Table 2). Pregnant patients with underlying chronic conditions were offered vaccine at approximately the same rate as low-risk patients; however, providers were slightly less likely to offer both seasonal and 2009 H1N1 influenza vaccines for pregnant patients with prepregnancy obesity. The following reasons for not offering vaccinations were reported by ob-gyns (percentages for seasonal and 2009 H1N1 influenza vaccines, respectively): not adequately reimbursed by insurance (34.9% and 31.7%); no adequate storage and handling facilities for vaccines (28.0% and 35.8%); vaccine offered by closely affiliated clinic (21.7% and 28.5%); managed care contract does not cover the cost of vaccines and vaccine administration (20.1% and 17.1%); and belief that vaccines should be administered by another provider, such as an internist or family practitioner (15.3% and 14.6%). Although the percentage of respondents offering influenza vaccination to pregnant women was significantly greater for the 2009 H1N1 influenza vaccine as compared with seasonal influenza vaccine, recommendations to use influenza vaccine did not differ by vaccine type (seasonal or 2009 H1N1). The majority of respondents recommended influenza vaccination at any trimester of pregnancy; however, 10–11% recommended influenza vaccination only during the second or third trimester of pregnancy (Table 2). Almost all respondents reported that their medical practice either required (approximately 34%) or strongly encouraged (62–63%) them to receive an influenza vaccination, and almost all (90–92%) reported having actually received an influenza vaccination during the previous influenza season. Unvaccinated respondents provided the following reasons for not getting vaccination: unable to find the vaccine; had allergic reaction to influenza vaccines in the past; had influenza before vaccine became available; had no time for vaccination; or stated that there was no particular reason. These reasons did not differ by vaccine type.
Table 2.
Attitudes and Practices of U.S. Obstetrician–Gynecologists Regarding Influenza Vaccination of Pregnant Women, 2009–2010 Influenza Season
| Attitudes and Practices | Seasonal Influenza Vaccine |
2009 H1N1 Influenza Vaccine |
P |
|---|---|---|---|
| Offering influenza vaccination to pregnant patients | |||
| Routinely offered | 77.6 | 85.6 | <.001 |
| Not offered, but referred | 21.1 | 13.3 | <.001 |
| Neither offered or referred | 1.1 | 1.2 | .98 |
| Offering influenza vaccination to specific groups of pregnant patients | |||
| Healthy low-risk pregnant patients | 75.3 | 83.4 | <.001 |
| High-risk pregnant patients with underlying chronic conditions | 75.3 | 82.4 | <.001 |
| Pregnant patients with prepregnancy obesity | 71.0 | 77.5 | <.01 |
| Recommending influenza vaccination to pregnant patients | |||
| Do not recommend | 0.5 | 0.5 | .92 |
| Recommend during any trimester | 88.9 | 89.9 | .85 |
| Recommend during second or third trimester only | 10.6 | 9.6 | .97 |
| Requirements for medical staff to receive influenza vaccination | |||
| Required | 33.8 | 33.9 | .99 |
| Strongly encouraged (but not required) | 63.2 | 62.4 | .95 |
| Not required (and not strongly encouraged) | 2.9 | 3.3 | .92 |
| Received influenza vaccination themselves | |||
| Yes | 91.7 | 89.8 | .23 |
| No | 8.3 | 10.2 | .29 |
Data are % unless otherwise specified.
The most commonly cited sources of guidance regarding influenza vaccinations were the College and the Centers for Disease Control and Prevention, cited by 60.8% and 54.1% respondents, respectively. Other sources of information included local public health departments (18.8%), their own practice (11.9%), scientific literature (5.6%), and media (3.9%). Fewer than half (46.6%) of respondents stated that they report suspected adverse events after administering influenza vaccine; when asked how adverse events should be reported, only 13.1% specified the Vaccine Adverse Event Reporting System or Centers for Disease Control and Prevention (which cosponsors Vaccine Adverse Event Reporting System).
Among ob-gyns, predictors of routinely offering the 2009 H1N1 vaccination to pregnant women included considering primary care or preventive medicine to be a very important part of practice (adjusted prevalence ratio 1.2, CI 1.01–1.4), observing serious conditions attributed to influenza-like illness in their practice (adjusted prevalence ratio 1.1, CI 1.02–1.1), and personally receiving 2009 H1N1 influenza vaccination (adjusted prevalence ratio 1.2, CI 1.1–1.4; Table 3). In addition, practice type was an independent predictor of routinely offering 2009 H1N1 vaccine; compared with providers in group obstetrics-gynecology practice, providers in solo practice were less likely (adjusted prevalence ratio 0.8, CI 0.7–0.9) and providers in multispecialty group were more likely (adjusted prevalence ratio 1.1, CI 1.1–1.2) to offer 2009 H1N1 influenza vaccine. The 202 nonrespondents who returned the short follow-up letter survey did not differ from the full survey respondents in years of clinical practice, proportion of patients eligible for Medicaid, or the likelihood of routinely offering influenza vaccinations to pregnant women.
Table 3.
Predictors of Routinely Offering 2009 H1N1 Influenza Vaccine to Pregnant Women by U.S. Obstetrician–Gynecologists, 2009–2010 Influenza Season
| Characteristics | n* | Routinely Offered Vaccine (%) |
Adjusted Prevalence Ratio† (95% CI) |
|---|---|---|---|
| All | 858 | 85.6 | - |
| Practice type‡ | |||
| Group obstetrics-gynecology | 410 | 86.6 | 1.0 (Ref) |
| Solo | 142 | 66.9 | 0.8 (0.7–0.9) |
| Multispecialty group | 107 | 98.1 | 1.1 (1.1–1.2) |
| University full-time faculty and practice | 98 | 91.8 | 1.1 (0.99–1.1) |
| Other | 100 | 88.0 | 1.0 (0.9–1.1) |
| Considers primary care, preventive medicine an important part of practice§ | |||
| Very important | 389 | 88.4 | 1.2 (1.01–1.4) |
| Important | 422 | 84.6 | 1.1 (0.96–1.4) |
| Not important | 41 | 73.2 | 1.0 (Ref) |
| Observed serious conditions attributed to influenza-like illness among pregnant women‖¶ | |||
| Yes (at least one) | 269 | 91.1 | 1.1 (1.02–1.1) |
| No | 588 | 83.0 | 1.0 (Ref) |
| Received the 2009 H1N1 influenza vaccination themselves‖ | |||
| Yes | 768 | 87.2 | 1.2 (1.1–1.4) |
| No | 79 | 69.6 | 1.0 (Ref) |
CI, confidence interval; Ref, reference.
Sample size reduced because of missing values.
Routinely offered 2009 H1N1 influenza vaccine to pregnant patients compared with not offered but referred or neither offered or referred.
Adjusted estimates derived from model that included the following variables: practice type and sex.
Adjusted estimates derived from model that included the following variables: considers primary care or preventive medicine an important part of practice, age, and sex.
Adjusted estimates derived from model that included the following variables: observed serious conditions attributed to influenza-like illness among pregnant women, received 2009 H1N1 influenza vaccination themselves, age, and sex.
Conditions include maternal death, pneumonia requiring intensive care, spontaneous abortion or stillbirth, or preterm birth.
DISCUSSION
During the 2009 H1N1 pandemic, ob-gyns were critical to the public health response for preventing severe complications of influenza virus among pregnant women. Although most ob-gyns participating in this survey routinely offered influenza vaccinations to their patients, a considerable proportion of respondents did not offer vaccination or did not recommend vaccination in the first trimester of pregnancy, which represents a missed opportunity for preventing influenza virus infection and its serious consequences.
We found that ob-gyns routinely offered seasonal and 2009 H1N1 influenza vaccines to their pregnant patients during the 2009–2010 influenza season at a higher rate than reported from surveys of U.S. obgyns in previous influenza seasons,15,18 –22,25 which could be attributable to increased awareness regarding influenza in pregnancy during the pandemic season and increased demand for vaccination among pregnant women. Our study showed that providers who observed at least one of the serious conditions attributed to influenza-like illness were more likely to offer 2009 H1N1 influenza vaccine to their pregnant patients. In addition, during the 2009 H1N1 pandemic, ob-gyns were frequently reminded about the importance of influenza vaccination during pregnancy by media, publications in scientific journals, and letters from professional associations and governmental agencies.26 Provision of 2009 H1N1 vaccine at no cost to vaccination providers could also have motivated ob-gyns to become vaccinators and may explain why more providers offered 2009 H1N1 than seasonal influenza vaccine. Recently published influenza vaccination coverage rates among pregnant women support our finding of the significant increase in providing vaccination among ob-gyns; in the 2009–2010 influenza season, approximately 50% of pregnant women received influenza vaccination,27 which is the highest coverage level ever reported in the United States, getting closer to the Healthy People 2020 goal of 80% coverage.28
Barriers to recommending and administering influenza vaccination among ob-gyns in our sample included inadequate reimbursement and absence of storage and handling facilities for vaccines (which require refrigeration and protection from light). These financial and logistic concerns are not unique for influenza vaccines and have been consistently reported in previous surveys of obstetric providers.15–19,21,22 However, concerns about the safety of influenza vaccines reported in previous studies19,22 were uncommon in our survey, which occurred toward the end of the 2009–2010 influenza season, when speculations about safety of influenza vaccination had been mitigated. Solo practice providers, which represented 16.4% of ob-gyns in our sample, were less likely to offer influenza vaccination, but more likely (compared with other practice types) to consider primary care or preventive medicine a very important part of their clinical practice (analysis not shown). This suggests that barriers to vaccination among solo practice providers are more difficult to overcome than among those who practice in partnerships and groups.
One of the limitations of the study is the relatively low response rate, which is, however, slightly higher than reported in previous random surveys of general College members (averaged 40%).29 It is also possible that characteristics of respondents are different from that of nonrespondents, although nonresponse bias analysis did not reveal statistically significant differences for comparison variables. Importantly, the characteristics of respondents in our sample are similar to those of U.S. ob-gyns in general,30 and the characteristics of their patients are similar to those of U.S. women giving birth.31 As with most surveys, our study has inherent limitations of self-reported data, which can be subject to response bias. Because we collected our data immediately after the 2009 H1N1 pandemic season, our findings may not be generalizable to a nonpandemic influenza season, when fewer patients experience serious consequences of influenza, demand for vaccination is decreased, vaccine is no longer free, and pressure from professional associations is lower. Preliminary data from the 2010–2011 influenza season suggest that observed improvement of influenza vaccination coverage rates among pregnant women could be sustainable.32
Improving vaccination coverage rates during pregnancy is one of the main public health goals during both influenza pandemics and nonpandemic influenza seasons, because of its role in decreasing influenza-related morbidity and mortality among pregnant women and their young infants. For many women, ob-gyns are the only providers of health care.33 By not offering influenza vaccination to such women, providers miss a unique opportunity for prevention. Although demand for influenza vaccination from pregnant women plays an important role, research shows that when women are offered vaccination, most tend to accept it.15,20,27,34,35 Given that influenza vaccination reduces health care, societal, and individual costs, as well as productivity losses and absenteeism associated with influenza,10 policy improvements to allow more reliable reimbursement for vaccine providers, especially those in solo practice, might be beneficial for the society. A number of strategies (eg, patient reminder systems) have been successful in improving the role of obstetric providers as vaccinators and need to be used more widely,36–38 which can become even more feasible when electronic health records are widely implemented. Obgyns played a crucial role in increasing the national influenza vaccination coverage rates among pregnant women during the 2009 H1N1 pandemic and need to sustain their role as vaccinators during coming influenza seasons.
Acknowledgments
Funded by the cooperative agreement U65PS000813-03 from the Centers for Disease Control and Prevention, Department of Health and Human Services, and by the cooperative agreement UA6MC19010 from the Maternal and Child Health Bureau, Health Resources and Services Administration, Department of Health and Human Services.
The authors thank all the obstetrician– gynecologists who participated in the survey for their time, Julia Behler for her help with the study implementation, and Dr. Michael Monsour for his help with data analysis.
The findings and conclusions in this report are those of the authors and do not necessarily represent the official position of the Centers for Disease Control and Prevention.
Footnotes
Financial Disclosure
The authors did not report any potential conflicts of interest.
REFERENCES
- 1.2009 pandemic influenza A (H1N1) in pregnant women requiring intensive care-New York City, 2009. MMWR Morb Mortal Wkly Rep. 2010 Mar;26(59):321–326. [PubMed] [Google Scholar]
- 2.Dodds L, McNeil SA, Fell DB, Allen VM, Coombs A, Scott J, et al. Impact of influenza exposure on rates of hospital admissions and physician visits because of respiratory illness among pregnant women. CMAJ. 2007;176:463–468. doi: 10.1503/cmaj.061435. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Jamieson DJ, Honein MA, Rasmussen SA, Williams JL, Swerdlow DL, Biggerstaff MS, et al. H1N1 2009 influenza virus infection during pregnancy in the USA. Lancet. 2009;374:451–458. doi: 10.1016/S0140-6736(09)61304-0. [DOI] [PubMed] [Google Scholar]
- 4.Louie JK, Acosta M, Jamieson DJ, Honein MA. Severe 2009 H1N1 influenza in pregnant and postpartum women in California. N Engl J Med. 2010;362:27–35. doi: 10.1056/NEJMoa0910444. [DOI] [PubMed] [Google Scholar]
- 5.Neuzil KM, Reed GW, Mitchel EF, Simonsen L, Griffin MR. Impact of influenza on acute cardiopulmonary hospitalizations in pregnant women. Am J Epidemiol. 1998;148:1094–1102. doi: 10.1093/oxfordjournals.aje.a009587. [DOI] [PubMed] [Google Scholar]
- 6.Siston AM, Rasmussen SA, Honein MA, Fry AM, Seib K, Callaghan WM, et al. Pandemic 2009 influenza A(H1N1) virus illness among pregnant women in the United States. JAMA. 2010;303:1517–1525. doi: 10.1001/jama.2010.479. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Harris J. Influenza occurring in pregnant women. JAMA. 1919;72:978–980. [Google Scholar]
- 8.Nishiura H. Excess risk of stillbirth during the 1918–1920 influenza pandemic in Japan. Eur J Obstet Gynecol Reprod Biol. 2009;147:115. doi: 10.1016/j.ejogrb.2009.07.009. [DOI] [PubMed] [Google Scholar]
- 9.Nuzum JW, Pilot I, Stangl FH, Bonar BE. 1918 pandemic influenza and pneumonia in a large civil hospital. IMJ Ill Med J. 1976;150:612–616. [PubMed] [Google Scholar]
- 10.Fiore AE, Uyeki TM, Broder K, Finelli L, Euler GL, Singleton JA, et al. Prevention and control of influenza with vaccines: recommendations of the Advisory Committee on Immunization Practices (ACIP), 2010. MMWR Recomm Rep. 2010;59(RR-8):1–62. [PubMed] [Google Scholar]
- 11.Zaman K, Roy E, Arifeen SE, Rahman M, Raqib R, Wilson E, et al. Effectiveness of maternal influenza immunization in mothers and infants. N Engl J Med. 2008;359:1555–1564. doi: 10.1056/NEJMoa0708630. [DOI] [PubMed] [Google Scholar]
- 12.Eick AA, Uyeki TM, Klimov A, Hall H, Reid R, Santosham M, et al. Maternal Influenza Vaccination and Effect on Influenza Virus Infection in Young Infants. Arch Pediatr Adolesc Med. 2011;165:104–111. doi: 10.1001/archpediatrics.2010.192. [DOI] [PubMed] [Google Scholar]
- 13.Influenza vaccination during pregnancy. ACOG Committee Opinion No. 468. American College of Obstetricians and Gynecologists. Obstet Gynecol. 2010;116:1006–1007. doi: 10.1097/AOG.0b013e3181fae845. [DOI] [PubMed] [Google Scholar]
- 14.Lu P, Bridges CB, Euler GL, Singleton JA. Influenza vaccination of recommended adult populations, U.S., 1989–2005. Vaccine. 2008;26:1786–1793. doi: 10.1016/j.vaccine.2008.01.040. [DOI] [PubMed] [Google Scholar]
- 15.Gonik B, Jones T, Contreras D, Fasano N, Roberts C. The obstetrician-gynecologist’s role in vaccine-preventable diseases and immunization. Obstet Gynecol. 2000;96:81–84. doi: 10.1016/s0029-7844(00)00860-7. [DOI] [PubMed] [Google Scholar]
- 16.Naleway AL, Smith WJ, Mullooly JP. Delivering influenza vaccine to pregnant women. Epidemiol Rev. 2006;28:47–53. doi: 10.1093/epirev/mxj002. [DOI] [PubMed] [Google Scholar]
- 17.Panda B, Stiller R, Panda A. Influenza vaccination during pregnancy and factors for lacking compliance with current CDC guidelines. J Matern Fetal Neonatal Med. 2011;24:402–406. doi: 10.3109/14767058.2010.497882. [DOI] [PubMed] [Google Scholar]
- 18.Power ML, Leddy MA, Anderson BL, Gall SA, Gonik B, Schulkin J. Obstetrician-gynecologists’ practices and perceived knowledge regarding immunization. Am J Prev Med. 2009;37:231–234. doi: 10.1016/j.amepre.2009.05.019. [DOI] [PubMed] [Google Scholar]
- 19.Schrag SJ, Fiore AE, Gonik B, Malik T, Reef S, Singleton JA, et al. Vaccination and perinatal infection prevention practices among obstetrician-gynecologists. Obstet Gynecol. 2003;101:704–710. doi: 10.1016/s0029-7844(03)00010-3. [DOI] [PubMed] [Google Scholar]
- 20.Silverman NS, Greif A. Influenza vaccination during pregnancy. Patients’ and physicians’ attitudes. J Reprod Med. 2001;46:989–994. [PubMed] [Google Scholar]
- 21.Wallis DH, Chin JL, Sur DK. Influenza vaccination in pregnancy: current practices in a suburban community. J Am Board Fam Pract. 2004;17:287–291. doi: 10.3122/jabfm.17.4.287. [DOI] [PubMed] [Google Scholar]
- 22.Wu P, Griffin MR, Richardson A, Gabbe SG, Gambrell MA, Hartert TV. Influenza vaccination during pregnancy: opinions and practices of obstetricians in an urban community. South Med J. 2006;99:823–828. doi: 10.1097/01.smj.0000231262.88558.8e. [DOI] [PubMed] [Google Scholar]
- 23.Agresti A. Categorical data analysis. 2nd ed. New York (NY): John Wiley & Sons; 2002. [Google Scholar]
- 24.Spiegelman D, Hertzmark E. Easy SAS calculations for risk or prevalence ratios and differences. Am J Epidemiol. 2005;162:199–200. doi: 10.1093/aje/kwi188. [DOI] [PubMed] [Google Scholar]
- 25.Influenza vaccination in pregnancy: practices among obstetrician-gynecologists–United States, 2003–04 influenza season. MMWR Morb Mortal Wkly Rep. 2005;54:1050–1052. [PubMed] [Google Scholar]
- 26.Dear colleague letter from AAFP, ACOG, AMA and CDC: vaccination of pregnant women. [Retrieved December 15, 2010]; Available at: http://www.cdc.gov/h1n1flu/clinicians/pdf/Dear_Colleague_FINAL.pdf.
- 27.Seasonal influenza and 2009 H1N1 influenza vaccination coverage among pregnant women–10 states, 2009–10 influenza season. MMWR Morb Mortal Wkly Rep. 2010;59:1541–1545. [PubMed] [Google Scholar]
- 28.U.S. Department of Health and Human Services. Healthy People 2020. [Retrieved February 18, 2011]; Available at: http://healthypeople.gov/2020/topicsobjectives2020/pdfs/HP2020objectives.pdf.
- 29.Stanwood NL, Garrett JM, Konrad TR. Obstetrician-gynecologists and the intrauterine device: a survey of attitudes and practice. Obstet Gynecol. 2002;99:275–280. doi: 10.1016/s0029-7844(01)01726-4. [DOI] [PubMed] [Google Scholar]
- 30.American College of Obstetricians and Gynecologists. 2008 Socioeconomic Survey of ACOG Fellows. [Retrieved December 16, 2010]; Available at: http://www.acog.org/departments/dept_notice.cfm?recno=19&bulletin=5099. [Google Scholar]
- 31.Martin JA, Hamilton BE, Sutton PD, Ventura SJ, Mathews Osterman MJK. National vital statistics reports. 1. Vol. 59. Hyattsville (MD): National Center for Health Statistics; 2010. Births: Final data for 2008. [PubMed] [Google Scholar]
- 32.Centers for Disease Control and Prevention. Influenza vaccination coverage estimates among pregnant women-United States, November 2010. [Retrieved July 13, 2011]; Available at: http://www.cdc.gov/flu/pdf/vaccination/DingInternetPanelSurveyPregnantWomen.pdf.
- 33.Willson JR, Burkons DM. Obstetrician-gynecologists are primary physicians to women. Am J Obstet Gynecol. 1976;126:744–754. doi: 10.1016/0002-9378(76)90663-3. [DOI] [PubMed] [Google Scholar]
- 34.Yeager DP, Toy EC, Baker B., III Influenza vaccination in pregnancy. Am J Perinatol. 1999;16:283–286. doi: 10.1055/s-2007-993873. [DOI] [PubMed] [Google Scholar]
- 35.Yudin MH, Salripour M, Sgro MD. Impact of patient education on knowledge of influenza and vaccine recommendations among pregnant women. J Obstet Gynaecol Can. 2010;32:232–237. doi: 10.1016/s1701-2163(16)34449-8. [DOI] [PubMed] [Google Scholar]
- 36.Jacobson VJ, Szilagyi P. Patient reminder and patient recall systems to improve immunization rates. The Cochrane Database of Systematic Reviews. 2005;(3) doi: 10.1002/14651858.CD003941.pub2. Art. No.: CD003941. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Ndiaye SM, Hopkins DP, Shefer AM, Hinman AR, Briss PA, Rodewald L, et al. Interventions to improve influenza, pneumococcal polysaccharide, and hepatitis B vaccination coverage among high-risk adults: a systematic review. Am J Prev Med. 2005;28(5 Suppl):248–279. doi: 10.1016/j.amepre.2005.02.016. [DOI] [PubMed] [Google Scholar]
- 38.Walsh JM, McPhee SJ. A systems model of clinical preventive care: an analysis of factors influencing patient and physician. Health Educ Q. 1992;19:157–175. doi: 10.1177/109019819201900202. [DOI] [PubMed] [Google Scholar]