Abstract
A 1.5-year-old, spayed female, mixed-breed dog was presented for hemoabdomen associated with an abdominal mass. Upon presentation bicavitary effusion was diagnosed. A penetrating intra-abdominal wooden foreign body was identified using computed tomography. This case describes a thoracic penetrating wooden foreign body causing bicavitary effusion following migration into the retroperitoneal space.
Résumé
Diagnostic d’un corps étranger thoracique et abdominal pénétrant par tomodensitométrie chez un chien. Une chienne de race croisée stérilisée âgée de 1,5 ans a été présentée pour un hémoabdomen associé à une masse abdominale. Sur présentation, une effusion bicavitaire a été diagnostiquée. Un corps étranger en bois intra-abdominal pénétrant a été identifié par tomodensitométrie. Ce cas décrit un corps étranger en bois pénétrant dans le thorax et causant une effusion bicavitaire après la migration dans l’espace rétropéritonéal.
(Traduit par Isabelle Vallières)
Penetrating wooden foreign bodies (WFBs) have been reported numerous times in the dog and other domestic species (1). In dogs (2), the most common reported location for these is the oropharyngeal region (3–5); however, intracavitary WFBs have also been reported (6,7). In those cases a diagnosis was made through clinical history, radiographic findings, and exploratory surgery (6,7). While radiographs can provide evidence of WFBs based on the presence of indirect signs such as subcutaneous emphysema (3,4), occult wooden foreign bodies pose a diagnostic challenge (8,9). As serious morbidity has been associated with undiagnosed WFBs (8), achieving a proper diagnosis to allow removal is critical. Radiographs have been shown to be insensitive at detecting WFBs (10). Ultrasound (9,11–13), computed tomography (5,8–10,13–15), and magnetic resonance imaging (MRI) (13,14) have all been shown to be more effective imaging modalities for the detection of retained WFBs. In each of these modalities the foreign body itself can be visualized, whereas in radiography only the associated radiographic signs such as emphysema are noted. While these modalities provide an advantage over plain radiographs, the diagnosis of WFBs remains a challenge due to their variable appearance (5,8,9,16). Ultrasound is limited in its ability to diagnose WFBs within echogenic tissue (12) and limitations associated with MRI include cost and time associated with image acquisition. The appearance of WFBs with CT is variable and often heterogeneous (5) with both hypodense and hyperdense regions (5). Computed tomography has been described as a valuable tool for the diagnosis of WFBs in the oropharynx of dogs (5). In human medicine, WFBs have been described as linear air dense features on CT examination (8,14,15). The case described in this report demonstrates the utility of CT as an imaging modality for the diagnosis of intracavitary WFBs. Furthermore, to the authors’ knowledge, this is the first report in the veterinary literature of a thoracic penetrating WFB leading to bicavitary effusion following migration into the retroperitoneal space after transit through the thorax.
Case description
A 1.5-year-old, spayed female, mixed breed dog was presented for further evaluation and treatment of a hemoabdomen and a suspected abdominal mass. Three days prior to presentation, what appeared to be a superficial laceration was repaired in her right axillary region; and no deep extent to the wound was recognized. The following day the dog became lethargic and inappetent. Over the following 2 d no improvement was noted in her appetite or demeanor, and abdominal and thoracic radiographs were taken (Figure 1). These identified a soft-tissue opacity containing numerous small gas opacities throughout the retroperitoneal space. An abdominal ultrasound examination confirmed a large structure with heterogenous echotexture and areas of retroperitoneal gas at the level of the right kidney. Peritoneal fluid was noted and an abdominocentesis yielded non-clotting blood. The dog was referred to the Ontario Veterinary College for further evaluation and treatment.
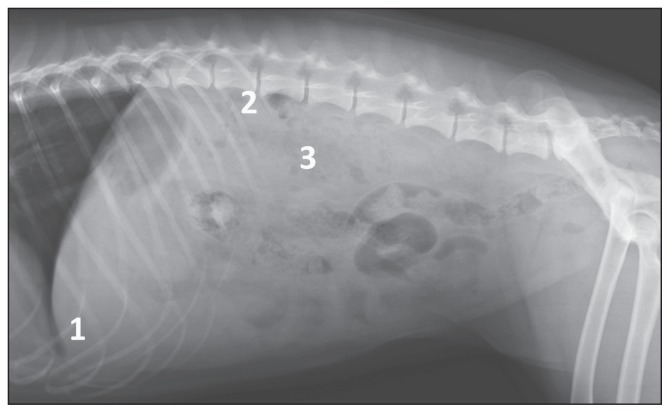
Figure 1.
Lateral abdominal radiograph with no evidence of pleural effusion (1), gas in the retroperitoneal space (2), and an ill-defined soft tissue opacity obscuring the renal silhouettes (3).
Upon presentation the dog was quiet, yet alert and responsive. Vital parameters were within normal limits. Although the dog was presented as recumbent, she was ambulatory but reluctant to stand. Electrocardiogram (ECG) at the time of presentation showed intermittent ventricular premature contractions and intermittent second-degree heart block. Abdominal and thoracic focused assessment with sonography for trauma (AFAST and TFAST) identified pleural and peritoneal fluid, which after abdomino- and thoraco-centeses yielded fluid grossly consistent with non-clotting blood. Cytology of these samples revealed predominantly red blood cells with subjectively increased numbers of neutrophils and also a population of reactive mesothelial cells in the thoracic effusion. No intracellular bacteria were noted. A population of hemosiderin laden macrophages also provided evidence consistent with a chronic bleeding process. Due to the new finding of an unexplained hemothorax, a thoracic and abdominal CT scan was performed under general anesthesia.
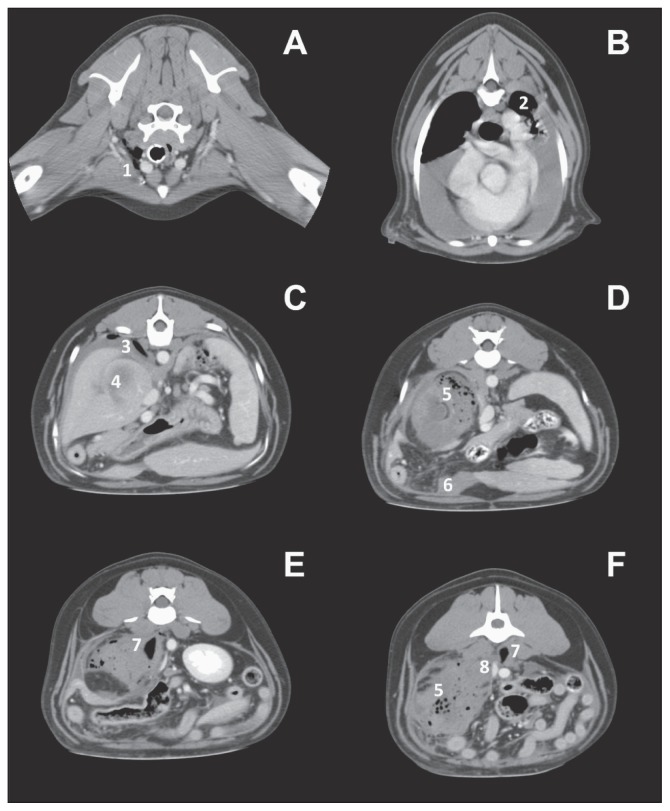
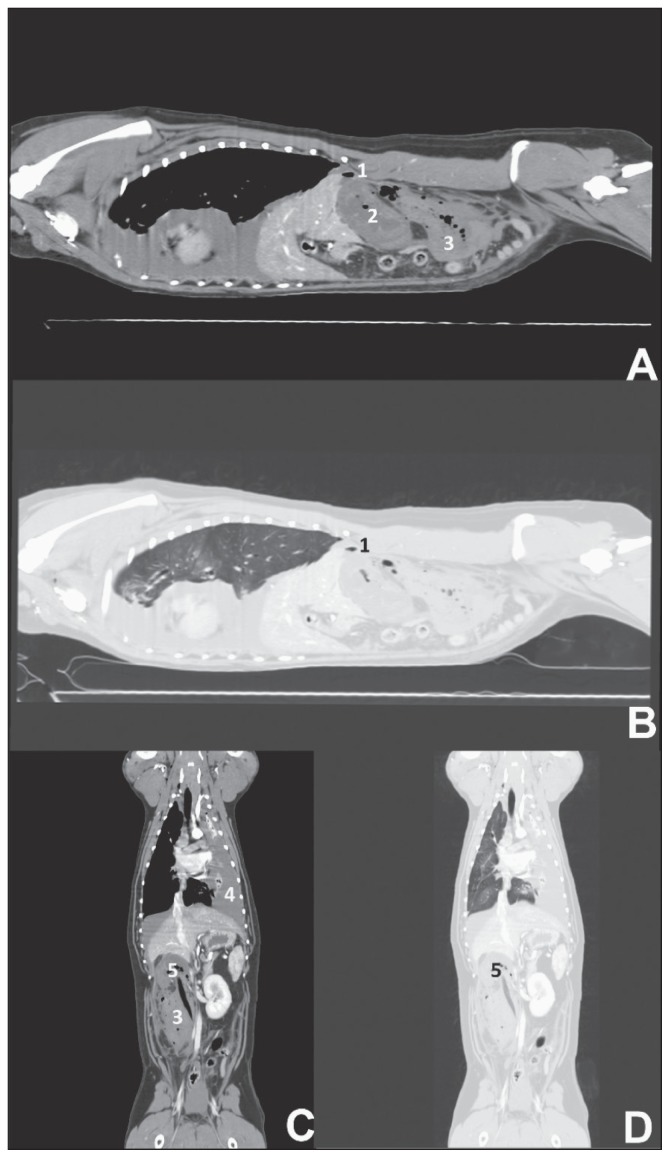
Evaluation of the CT scan revealed a small amount of gas in the right axillary subcutaneous tissues (Figure 2A), within the adjacent pleural space in the right cranial hemithorax, and in the pleural space caudodorsally adjacent to the diaphragm (Figure 2C). Gas was also present in the right side of the retroperitoneum, and in the peritoneal space. These findings were consistent with subcutaneous emphysema, a mild pneumothorax, pneumoretroperitoneum, and pneumoperitoneum. A moderate amount of non-contrast enhancing fluid was present in the pleural space, displacing the lungs (Figure 3C) and causing atelectasis of the left caudal lung lobe (Figure 2B). In the right retroperitoneal space an elongated feature slightly more dense than gas (~−275 Hounsfield Units, HU), measuring 10 cm in length (Figure 3C), extended from the right renal pelvis to the hypaxial lumbar musculature on the right side at the level of the L5 vertebral body (Figure 2F). This feature was oriented cranio-ventrally on the right side to caudo-dorsally on the midline.
Figure 2.
Transverse computed tomographic images of caudal cervical tissues (A), mid-thorax (B), cranial abdomen (C), midabdomen (D, E), caudal abdomen (F). Images are displayed in a soft tissue window (400 WW/40 WL), post-contrast administration. Free gas is present in the cervical soft tissues near the right axillary puncture site (1). Pleural effusion is noted with compression atelectasis of the left lung (2). Free air in the right costrophrenic space (3) and a soft tissue opaque mass with lack of contrast uptake (4) is observed. Free gas within the cortex of the right kidney and the associated mass (5) as well as a right kidney with no contrast uptake is observed (C,D,E,F). Mild abdominal effusion is noted (6). An angular, gas dense structure is associated with the mass (E7) and the same structure is observed penetrating the epaxial musculature (F7). The mass of necrotic hemorrhage is observed to compress the caudal vena cava (8).
Figure 3.
Sagittal (A,B) and dorsal (C, D) reconstructions of a whole body CT acquired post contrast administration. There is a mild amount of free gas on either side of the diaphragm (1). The right kidney is observed with lack of contrast uptake (2) as well as the associated soft tissue mass (3) later identified as necrotic hemorrhage. Pleural effusion is seen (4) as well as a linear structure (5) that appears gas dense in a soft tissue window (C5) and measures ~280 HU differentiating it from air on a lung window (D5). Soft tissue windows (A,C) have a window width of 400 HU and a window level of 40 HU. Lung window has window width of 1400HU and level of −500 HU.
The right kidney exhibited minimal contrast enhancement and this was delayed (Figure 2C,D,E,F; Figure 3A). The right renal artery, renal vein, and ureter were not visualized and did not contrast enhance. In the right retroperitoneal space, surrounding the elongated feature and the right kidney, was a large ill-defined, slightly heterogeneous, fluid to soft tissue dense feature that minimally contrast enhanced (Figure 3A,C), and contained several rounded gas dense features throughout. This extended up to the level of the L6 vertebral body caudally and measured at least 15.6 cm long, 6 cm wide, and 6 cm high. At this location, the caudal vena cava was severely focally flattened lateromedially (Figure 2F). Multiple gas bubbles were also present within the renal cortex (Figure 2D). These findings were consistent with a wooden stick in the right retroperitoneal space and embedded in the hypaxial musculature and right kidney with secondary renal devascularization (i.e., a non-patent renal artery) as seen by lack of contrast uptake. Based on the presence of blood in the thoracic cavity without an apparent local source of hemorrhage, and gas bubbles adjacent to the right side of the diaphragm, a diaphragmatic tear secondary to foreign body penetration was suspected.
Based on the clinical and imaging findings, our working diagnostic theory was that a WFB penetrated the axilla, passed through the thorax, and through the dorsal diaphragm into the right retroperitoneal space where it damaged the right kidney and associated musculature. A hemoretroperitoneum was suspected to have originated from damage to the renal parenchyma and/or vasculature and the hemothorax and hemoperitoneum were suspected to have developed from the movement of abdominal hemorrhage through a diaphragmatic tear into the pleural space and from the retroperitoneal space to the peritoneal space through a defect in the retroperitoneum.
An exploratory laparotomy was performed and a hemoabdomen was confirmed upon entry. The right kidney was not immediately identifiable and was surrounded by necrotic material. Vascular patency of the renal vessels could not be assessed but was unlikely due to the necrosis surrounding the kidney and the previous CT findings. Deep palpation into the region of the right kidney revealed a large stick (~10 cm long and 2 cm in diameter). A right nephrectomy was performed by a combination of sharp and blunt dissection using a vessel-sealing device (Ligasure; Valleylab, Boulder, Colorado, USA). The stick was removed along with the right kidney. The renal artery and vein were not identifiable and only scant tissue grossly consistent with renal parenchyma was identified. No significant bleeding was identified during the removal. The tissue identified as the right kidney was significantly replaced by a hematoma and inflammatory tissue. A 0.5 cm × 0.5 cm laceration in the right side of the diaphragm was visualized and was allowing blood to enter the abdomen from the pleural space. This prompted investigation to definitively rule out any possible thoracic pathology and a median sternotomy was performed. A mild-moderate hemothorax was noted; however, aside from a small defect in the intercostal muscles at the right 10th intercostal space, at the same level as the diaphragmatic tear, no other abnormalities were present in the thoracic cavity. The thoracic cavity and intercostal defect were flushed copiously with sterile saline and a chest tube was placed. The diaphragmatic laceration was then repaired. Repeat inspection of the peritoneal cavity did not reveal any further abnormalities nor any active hemorrhage and the peritoneal cavity was lavaged. Two abdominal closed suction drains (100 cc Silicone Closed Wound Suction Evacuator Kit; Bard Davol, Covington, Georgia, USA) were placed for postoperative management prior to routine closure of the sternotomy and laparotomy.
Due to a decrease in packed cell volume and corresponding increase in heart rate, a whole blood transfusion was administered both peri- and post-operatively. The patient recovered well in the ICU, and 4 d later an additional whole blood transfusion was given after an acute increase in abdominal drain production characteristic of further blood loss. Aside from this setback, recovery was smooth and the dog was discharged to her owner’s care 6 d after surgery.
Discussion
Wooden foreign bodies do not commonly penetrate both the thoracic and abdominal cavities concurrently (4). While previous reports have identified penetrating thoracic or abdominal WFBs (6,7) bicavitary involvement has not, to the authors’ knowledge, been reported in the literature.
Radiographs and ultrasound represent excellent and economical first line diagnostics that can provide evidence for, and in some cases definitively diagnose, WFBs (3,4,9–11), but their limitations become evident in complex cases. As WFBs are typically non-radiopaque (10) the utility of radiographs in the diagnosis of a penetrating foreign object is most often limited to detecting the presence of emphysema (2–4). However, radiographic evidence in cases of intracavitary penetration, such as a pneumoperitoneum with loss of serosal detail, can be almost definitive for a penetrating object when combined with the clinical history (7). In such cases, further imaging may not be required and laparotomy or thoracotomy may be indicated to obtain a definitive diagnosis and allow treatment. In the case presented here, the clinical history was suggestive of a possible migrating foreign body. However, a foreign body as the cause of the bicavitary effusion was called into doubt by the previous surgical closure identifying no deep penetration in the axilla. Moreover, the findings of massive and chronic hemorrhage in both the abdomen and thorax are not a common presentation of a penetrating WFB, therefore, further imaging was warranted to investigate the cause of the bicavitary effusion. While ultrasound is a useful tool for diagnosing WFBs (11,12), the echogenic structure seen in the retroperitoneal space along with the large amount of free gas created a diagnostic challenge in this case. Furthermore, the bicavitary involvement and the limitations of ultrasound in the thoracic cavity created a need for advanced imaging. Thus, CT offered the most accurate and cost-effective method for an accurate diagnosis and was also a time efficient method in a progressively unstable patient.
The CT appearance of wooden foreign bodies has been reported to be variable in veterinary medicine. Examples of near air dense sticks have been reported in a cadaveric canine manus model (13) and are a common computed tomographic feature in humans with penetrating WFBs (8,10,14,15). In this case, the appearance of the WFB when viewed in a soft tissue window and level gave an appearance similar to that of air. This is an example of the diagnostic challenge that is presented in cases of a penetrating WFB in an abnormal location.
The delay in clinical signs observed in this case is suspected to be related to the mechanism by which the WFB entered the abdominal cavity. While the initial trauma occurred in the right axilla, the WFB likely migrated through the subcutaneous tissues, pleural space, and finally through the diaphragm into the retroperitoneal space. This mechanism of migration has been previously described for inhaled or ingested plant awns (17). In such cases, the respiratory movements drive the caudal movement of the foreign object (17). The time required to migrate over this distance is likely responsible for the delayed clinical presentation.
The mechanism by which a hemothorax occurred in this case warrants further discussion. A previous case of pleural effusion with an abdominal source of the fluid has been reported (18). While this report identified that a traumatic uroabdomen and diaphragmatic tear led to urinothorax, it did not comment on the degree of effusion in either cavity. In the case presented here, the contrast in volume of the thoracic and abdominal hemorrhage was readily apparent at surgery. While a significant amount of blood was present in the abdominal cavity, most of it was present in the thorax. It is proposed that the diaphragmatic tear operated like a one-way valve, drawing the abdominal hemorrhage into the thoracic cavity with the negative pressure associated with each inhalation.
This case identifies the utility of CT for the diagnosis of WFBs and represents a unique progression of disease from axillary penetration to thoracic effusion secondary to abdominal hemorrhage. In cases where other imaging modalities are inconclusive for the cause of effusion, CT can be a sensitive diagnostic tool for identifying the cause and source of effusion. Therefore, whole body CT should be considered in cases suspicious of penetrating WFBs as well as those with bicavitary hemorrhage of unknown cause. The information gleaned from CT shortened the surgery time as the hemorrhage was confirmed to be abdominal in origin rather than thoracic and the minimal contrast uptake in the kidney allowed a nephrectomy to be performed without perioperative investigation of kidney perfusion.
Acknowledgments
We acknowledge the contributions of the staff at the Ontario Veterinary College for their care of the patient during her stay in hospital as well as the Mount Brydges Animal Clinic for the use of their radiographs in this report. We also extend our appreciation to Maxmillien Rosenberg for his assistance in the creation of the figures used herein. CVJ
Footnotes
Use of this article is limited to a single copy for personal study. Anyone interested in obtaining reprints should contact the CVMA office (hbroughton@cvma-acmv.org) for additional copies or permission to use this material elsewhere.
References
- 1.White RAS, Lane JG. Pharyngeal stick penetration injuries in the dog. J Small Anim Pract. 1988;29:13–35. [Google Scholar]
- 2.Laverty S, Lavoie JP, Pascoe JR, Ducharme N. Penetrating wounds of the thorax in 15 horses. Equine Vet J. 1996;28:220–224. doi: 10.1111/j.2042-3306.1996.tb03776.x. [DOI] [PubMed] [Google Scholar]
- 3.Girffiths LG, Tiruneh R, Sullivan M, Reid SWJ. Oropharyngeal penetrating injuries in 50 dogs: A retrospective study. Vet Surg. 2000;29:383–388. doi: 10.1053/jvet.2000.9140. [DOI] [PubMed] [Google Scholar]
- 4.Doran P, Wright CA, Moore AH. Acute oropharyngeal and esophageal stick injury in forty-one dogs. Vet Surg. 2008;37:781–785. doi: 10.1111/j.1532-950X.2008.00448.x. [DOI] [PubMed] [Google Scholar]
- 5.Halfacree NZ, Whatmough C, Mantis P, Baines S. Computed tomography as an aid to management of chronic oropharyngeal stick injury in the dog. J Small Anim Pract. 2008;49:451–457. doi: 10.1111/j.1748-5827.2008.00591.x. [DOI] [PubMed] [Google Scholar]
- 6.Pelosi A, Hauptman JG, Eyster GE, Beal MW, Anderson LK, Oliver NB. Myocardial perforation by a stick foreign body in a dog. J Vet Emerg Crit Care. 2008;18:184–187. [Google Scholar]
- 7.Menard J, Schoeffler L. Colonic, ureteral and vascular injuries secondary to stick impalement in a dog. J Vet Emerg Crit Care. 2011;21:387–394. doi: 10.1111/j.1476-4431.2011.00644.x. [DOI] [PubMed] [Google Scholar]
- 8.Krimmel M, Corneltus CP, Stojadinovic S, Hoffman J, Reinert S. Woodern foreign bodies in facial injury: A radiological pitfall. Int J Oral Mxillofac Surg. 2001;30:445–447. doi: 10.1054/ijom.2001.0109. [DOI] [PubMed] [Google Scholar]
- 9.Peterson JJ, Bancroft LW, Kransdorf MJ. Wooden foreign bodies: Imaging appearance. Am J Roentgenol. 2002;178:557–562. doi: 10.2214/ajr.178.3.1780557. [DOI] [PubMed] [Google Scholar]
- 10.Oikarinen KS, Nieminen TM, Makaranen H, Phytinen J. Visibility of foreign bodies in soft tissue in plain radiographs, computed tomography, magnetic resonance imaging and utrasound: An in vitro study. Int J Oral Maxillofac Surg. 1993;22:119–124. doi: 10.1016/s0901-5027(05)80818-5. [DOI] [PubMed] [Google Scholar]
- 11.Armburst LJ, Biller DS, Radlinsky MG, Hoskinson JJ. Ultrasonographic diagnosis of foreign bodies associated with chronic draining tracts and abscesses in dogs. Vet Radiol Ultrasound. 2003;44:66–70. doi: 10.1111/j.1740-8261.2003.tb01452.x. [DOI] [PubMed] [Google Scholar]
- 12.Staudte KL, Hopper BJ, Gibson NR, Read RA. Use of ultrasonography to facilitate surgical removal of non-enteric foreign bodies in 17 dogs. J Small Anim Pract. 2004;45:395–400. doi: 10.1111/j.1748-5827.2004.tb00254.x. [DOI] [PubMed] [Google Scholar]
- 13.Ober CP, Jones JC, Larson MM, Lanz OI, Were SR. Comparison of ultrasound, computed tomography and magnetic resonance imaging in detection of acute wooden foreign bodies in the canine manus. Vet Radiol Ultrasound. 2008;49:411–418. doi: 10.1111/j.1740-8261.2008.00399.x. [DOI] [PubMed] [Google Scholar]
- 14.Ho VT, McGurckin JF, Smergel EM. Intraorbital wooden foreign body: CT and MR appearance. Am J Neuroradiol. 1996;17:134–136. [PMC free article] [PubMed] [Google Scholar]
- 15.Kantarci M, Ogul H, Karsen RM. Detection of a giant wooden foreign body with multidetector computed tomography and multiplanar reconstruction imaging. Am J Emerg Med. 2006;8:211–213. doi: 10.1016/j.ajem.2006.08.006. [DOI] [PubMed] [Google Scholar]
- 16.Dobromylskyj MJ, Dennis R, Ladlow JF, Adams VJ. The use of magnetic resonance imaging in the management of pharyngeal penetration injuries in dogs. J Small Anim Pract. 2008;49:74–79. doi: 10.1111/j.1748-5827.2007.00436.x. [DOI] [PubMed] [Google Scholar]
- 17.Frendin J, Grejot C, Hellmen E, Iwarsson M, Gunnarsson A, Chryssantou E. Thoracic and abdominal wall swellings in dogs caused by foreign bodies. J Small Anim Pract. 1994;35:499–508. [Google Scholar]
- 18.Klainbart S, Merchav R, Ohad DG. Traumatic urothorax in a dog: A case report. J Small Anim Pract. 2011;52:544–546. doi: 10.1111/j.1748-5827.2011.01107.x. [DOI] [PubMed] [Google Scholar]