Abstract
Background
Surveillance on paralysis prevalence has been conceptually and methodologically challenging. Numerous methods have been used to approximate population-level paralysis prevalence estimates leading to widely divergent prevalence estimates.
Objective/hypotheses
To describe three phases in use of the International Classification of Functioning, Disability and Health (ICF) as a framework and planning tool for defining paralysis and developing public health surveillance of this condition.
Methods
Description of the surveillance methodology covers four steps: an assessment of prior data collection efforts that included a review of existing surveys, registries and other data collection efforts designed to capture both case definitions in use and prevalence of paralysis; use of a consensus conference of experts to develop a case definition of paralysis based on the ICF rather than medical diagnostic criteria; explanation of use of the ICF framework for domains of interest to develop, cognitively test, validate and administer a brief self-report questionnaire for telephone administration on a population; and development and administration of a Paralysis Prevalence and Health Disparities Survey that used content mapping to back code items from existing national surveys to operationalize key domains.
Results
ICF coding led to a national population-based survey of paralysis that produced accurate estimates of prevalence and identification of factors related to the health of people in the U.S. living with paralysis.
Conclusions
The ICF can be a useful tool for developing valid and reliable surveillance strategies targeting subgroups of individuals with functional disabilities such as people with paralysis and others.
Keywords: Paralysis, Functional definition of disability, ICF, Surveillance
Estimates of paralysis prevalence in the U.S. vary widely, ranging from 1.4 to 5.4 million people.1 In 2009, Congress authorized a three-part effort to address the public health challenges posed by paralysis.2 The first two titles of the Christopher and Dana Reeve Paralysis Act provide the National Institutes of Health (NIH) with authority to investigate research to understand causes of paralysis in the hopes of identifying a cure, and explore clinical trials that lead to improved rehabilitation treatments. The third provision authorized the Centers for Disease Control and Prevention (CDC) to implement public health activities devoted to improving the quality of life for persons with paralysis and other physical disabilities.3 The legislation recognized the importance of conducting accurate paralysis surveillance as the first step toward establishing a quality of life public health action plan for people with paralysis.
Prior research has noted numerous difficulties in conducting population-based surveillance of conditions associated with paralysis.4 Variation in estimates can be attributed to different sampling strategies, sample size, and differing definitions of paralysis. Establishing an operational case definition of paralysis to more accurately screen for this condition is central to addressing these challenges.
One approach to developing a case definition for paralysis is to screen for diagnosed medical conditions associated with paralysis, and then query a given data source further to determine its functional expression, but this method presents challenges. The three diagnoses most directly linked to paralysis—stroke, SCI, and multiple sclerosis (MS)—can be screened for in surveys (“… have you ever received a diagnosis for …”), but each present unique difficulties in tracking paralysis. Stroke has an estimated prevalence of 7.3% in the adult U.S. population, with disability occurring in 65% of cases, but paralysis constitutes an unknown subset.5 The disabling effects of stroke are potentially reversible and severity of stroke varies over time, making stroke-related paralysis time-dependent. SCI, another example, typically results from irreversible trauma. Prevalence estimates using SCI registries approach 280,000 people in the U.S.6 but do not include non-traumatic causes of spinal cord dysfunction that can also lead to paralysis and are based on a subset of U.S. reporting sites that may not be representative of SCI experienced in all states.7 MS prevalence estimates range from 58 to 95 per 100,000 adult population, translating to as many as 285,000 people with paralysis.8–10 But symptoms of MS are frequently unpredictable, with exacerbations and remissions influenced by age, duration of disease and environmental exposures.11
An alternative approach is to base case identification on a functional definition of paralysis and then extrapolate likely etiology, but this approach is not without risks of its own. Reliability and validation procedures need to be considered to ensure credibility of the surveillance data and findings.1 In addition, there is the need to identify and then build upon a conceptual framework that supports a functional operational case definition of the condition. Non-medical disability models from which to choose can be found among disablement frameworks, where disablement is considered the impact of chronic and acute conditions on specific body system functioning as well as people’s abilities to act in necessary, usual, expected and personally desired ways in their society.12–15
When the World Health Organization released the International Classification of Functioning, Disability and Health (ICF) in 2001, it extended the disablement approach to health and health-related domains to describe changes in body function and structure, level of capacity, and level of performance.16 A 2007 Institute of Medicine report cited this framework in calling for “… increased attention to the critical roles that the physical and social environments … play in determining the extent to which individuals with chronic physical and mental conditions can function independently and participate fully in community life.”17
Since then, the ICF has been influential in providing a framework for understanding interactions of condition, environment and personal factors on influencing body function and structure, activities and participation.18 Still, the slowness with which the ICF framework has been adapted to public health practice may reflect the lack of a standardized approach that is widely understood,19 or more general “… challenges around the operationalization of the ICF’s core concepts (that) need to be resolved.”20
Despite these challenges, research has demonstrated the value of cross-mapping existing items in surveillance instruments on to the framework of the ICF.21 Often termed “content comparison” or “back coding,” it has been applied retrospectively to multiple disability-causing conditions including arthritis,22 stroke23 and dementia,24 as well as globally.25 The ICF continues to be proposed as a public health strategic planning tool,26 and for use in applying classification schema to advance health promotion in the United States and Canada.27
Objectives
Develop a case definition of paralysis based on functional limitations;
Develop valid self-report procedures for paralysis; and
Develop a questionnaire that utilizes ICF domains and codes to facilitate consistent current and future data collection.
Methods
Objectives were realized through a multi-year project that involved four steps:
An assessment of prior data collection efforts that included a review of existing surveys, registries and other data collection efforts designed to capture case definitions in use and paralysis prevalence;
Use of a consensus conference to develop a case definition of paralysis based on the ICF rather than medical diagnostic criteria;
Use of the ICF framework for domains of interest to develop, cognitively test, validate and administer a brief self-report questionnaire for telephone administration on a population basis;
Development and administration of the 2013 Paralysis Prevalence and Health Disparities Survey that used content mapping to back code items from existing national surveys to operationalize key domains.
Results
Assessment of prior data collection efforts
In 2005, with guidance from a national expert panel, academic researchers conducted a national assessment of how paralysis was defined and how paralysis data were collected.28 Tasks included a review of current surveys used to identify persons with paralysis; a survey of organizations representing persons with paralysis-related disabilities to assess their surveillance capacities; and follow up interviews with potential best practice sites. They recommended the development of “a … definition that captures the breadth of possible ways in which paralysis can manifest itself … encompass(ing) categories inclusive of all people who may experience functional limitations and decreased social participation because of these limitations.”1
Development of a functional definition of paralysis
Following this report, the CDC funded a consensus conference of experts in 2006, which led to the following conceptual definition of paralysis based on the ICF functional definition of disability, combining condition and functional outcome, as well as subsequent questions targeting etiology:29
Paralysis is a central nervous system disorder that results in difficulty or inability to move the upper or lower extremities. This conceptual definition was operationalized for survey-based surveillance as follows: (1) Do you or does anyone in this household have any difficulty moving their arms or legs?
If respondents answered “yes,” they were then asked (2) to identify one of the causes from among the following: SCI, traumatic brain injury (TBI), stroke, poisoning, complications from surgery, amyotrophic lateral sclerosis/Lou Gehrig’s, Guillain Barre syndrome, MS, neurofibromatosis, epidural infection, Chiari malformation, syringomyelia, post-polio syndrome, spinal muscular atrophy, Fredrich’s ataxia, transverse myelitis, cerebral palsy, and spina bifida. If they identified “yes” to the first question and specified a diagnosis to the second, they met the definition of paralysis.
Developing, cognitively testing, validating and administering a brief self-report questionnaire related to ICF domains
Based on results of the initial population survey, the expert panel made several changes to the paralysis items. Case ascertainment procedures were strengthened to reduce the possibility of false positives – self-reporting paralysis or paralysis conditions such as SCI when in fact they did not exist. In conjunction with SCI research consultants, a three step process to increase likelihood of reliable responses was developed:
Cognitive testing of the two items on paralysis and subsequent focus groups to gather information about the clarity and understandability of the paralysis items;
Pilot testing to further refine paralysis questions and include new items on two pilot surveys; and
Field implementation of the paralysis items and questionnaire on national, population-based surveys and additional refinement of paralysis items.
Cognitive testing
A research team organized through the Center for Development and Disability (CDD) at the University of New Mexico developed a survey that included the two paralysis questions, in addition to others intended to gain greater understanding of factors related to living with paralysis. Testing was administered by phone to English-speaking people with paralysis who were recruited from lists of people known to be paralyzed throughout New Mexico maintained by the CDD and meeting the functional case definition of paralysis, taking an average of 5 min to complete, with respondents compensated for their time. After completing the survey, participants were invited to participate in follow-up interviews in which they were queried about clarity and understandability of the questions. Approximately 30% participated in the follow-ups, with more in-depth understanding of their responses leading to further revisions of the questions developed through prompts around broad areas of body function and structure (1); activities and participation (2); and environmental factors (3) (Table 1).
Table 1.
Questions used in focus group discussions as part of cognitive testing for First Paralysis Survey (2008)
| Broad area of body functions and structures: |
| “If there are times when you have difficulty in moving your arms or legs, … ” |
| “What part of your arms or legs is affected most?” |
| “What is the underlying cause of your difficulty in moving; for example, is it caused by pain, numbness, stiffness, lack of sensation, some combination of these, or something else?” |
| “Are there other conditions that contribute to your difficulty in moving your arms or legs?” Please describe them. |
| “Have you received a medical diagnosis for the condition that makes it difficult for you to use your arms or legs?” If so, what is it? If not, why has no diagnosis been given? |
| Broad area of activities and participation: |
| “What sort of things does this difficulty prevent you from doing?” |
| “What sort of things are you able to do with some degree of difficulty?” |
| “Are you able to exercise? If so, what types of exercise do you do?” |
| “Does this difficulty prevent your working, either professionally or around the house? If so, please describe how.” |
| “Does this difficulty affect any other parts of your life? If so, please describe what activities this difficulty affects. This could include things in the home, community, or work.” |
| Broad area of environmental factors: |
| “How do you overcome difficulties in doing some things with your arms or legs? For example, how do you do things like household or professional work, transportation, shopping, and similar type things?” |
| “What types of accommodations do you use in order for you to maintain an independent lifestyle? For example, do you require a personal assistant? A wheelchair or other assistive device? Describe what it takes for you to be as independent as possible while living with the difficulty you have in moving your arms or legs. |
| “What are the major barriers you face to being able to live an independent life? What do you feel are some ways of overcoming these barriers?” |
Pilot testing
Findings from the cognitive testing led to revisions that were then included on two national random-digit pilot test surveys. Participants were recruited by a large national polling and survey group30 using randomly generated phone numbers to respond to the pilot surveys. Based on findings from these pilots, the order of some questions was revised, as well as listings of some conditions found to be redundant or inappropriate.
Field implementation
Field implementation involved two national, population-based telephone surveys in the US conducted in 2008 and then again in 2012–2013 by the same nationally-recognized research and polling firm. The surveys used a national household sampling strategy, screening on whether the person answering the phone or anyone else in the household had difficulty moving their upper or lower extremities. African–Americans and Hispanics were oversampled to assure representativeness.
Results from the first field survey were generalized to the population of the United States and weighted to reflect the population of the United States using a two-stage process, first correcting for disproportionality of the Hispanic survey and then weighting the results to 2008 Current Population Survey (CPS) estimates on education, age, region, and gender. This was done separately for each racial group, and each group was balanced to their overall proportion in the population. The second field implementation used similar methodology, but used both land lines and cell phone numbers, incorporating case identification items from the first survey as well as newly developed validation items and additional variables based on the ICF framework. A follow-up call to this second survey that averaged 10 min was conducted with respondent households meeting the case definition of paralysis, asking questions on financial aspects of health care, preventive care, and functional limitations.
Results from the second survey were also weighted to account for disproportionate probabilities of household selection due to the number of separate telephone lines and probability of random selection of an individual household member. Following this weighting, the sample was additionally weighted to the 2012 American Community Survey (ACS) on key demographics such as age, race, sex, region, and education, taking into account the distribution of phone usage in the general population (cell phone only, cell phone mostly, landline only, and mixed users).
Participants
Subject matter experts in the different components of the study included eight experts in the initial expert panel (2005–06); 30 participants in the consensus conference who had expertise in paralysis research, public health, surveillance, and the lived experience of paralysis; and five experts in the validity component, particularly for SCI.
Respondents to the surveys included approximately 100 people in the cognitive testing phase; 30 in the follow-up to the cognitive testing; approximately 1000 people participated in the pilot test surveys; 631 in the follow-up call to the second survey. In total, 103,796 households responded to the two field surveys (Fig. 1).
Fig. 1.
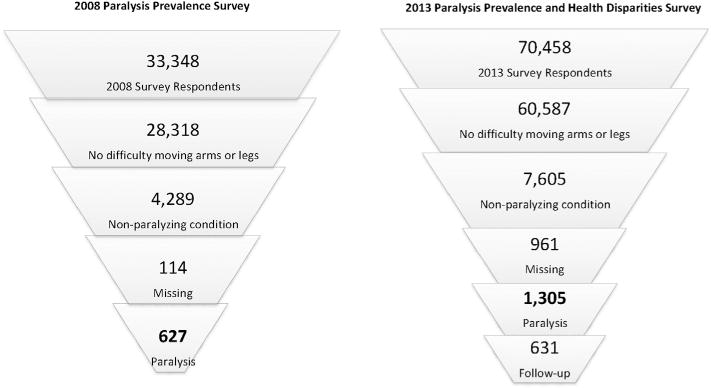
Flow diagrams for sample selection for the 2008 & 2013 paralysis surveys: N = 103,806 (total).
Development and administration of the 2013 Paralysis Prevalence and Health Disparities Survey
The focus of the second national survey, conducted in 2012–2013, was to gather information on paralysis prevalence, severity, general health, secondary conditions, and use of health care services. The planning group engaged in an iterative process of examining content domains and soliciting input for selecting questions from pre-existing surveys, while working to ensure an administration time that would not exceed 25 min. Survey items were selected from normed, standardized and frequently cited surveys that included the ACS, Behavioral Risk Factor Surveillance System (BRFSS), Survey of Income and Program Participation (SIPP), the National Health Interview Survey and the National Health and Nutrition Examination Survey (NHANES). Final items for field implementation included 7–18 questions in each of the following survey sections: prevalence, SCI validation, severity, general health, secondary conditions, utilization of health care, and financial factors. Consistent with published ICF coding methods described in the W.H.O. manual for using the ICF,18 we aligned the expert panel paralysis case definition as well as normed disability and health survey items with the ICF to develop each survey (Fig. 2 below/Fig. 3 in on-line supplement only). The substantive content of pre-existing disability and health survey items mapped to five ICF domains in 12 coding regions, forming a consistent framework for 29 of the paralysis survey items. Two ICF Body Function and Body Structure codes were consistent with the working definition of paralysis prevalence. Fourteen Body Function and Activities and Participation codes were consistent with survey measures of paralysis severity. Fifteen Body Function, Body Structure and Environmental Factor codes were consistent with survey measures of general health, secondary conditions, and use of health care services.
Fig. 2.
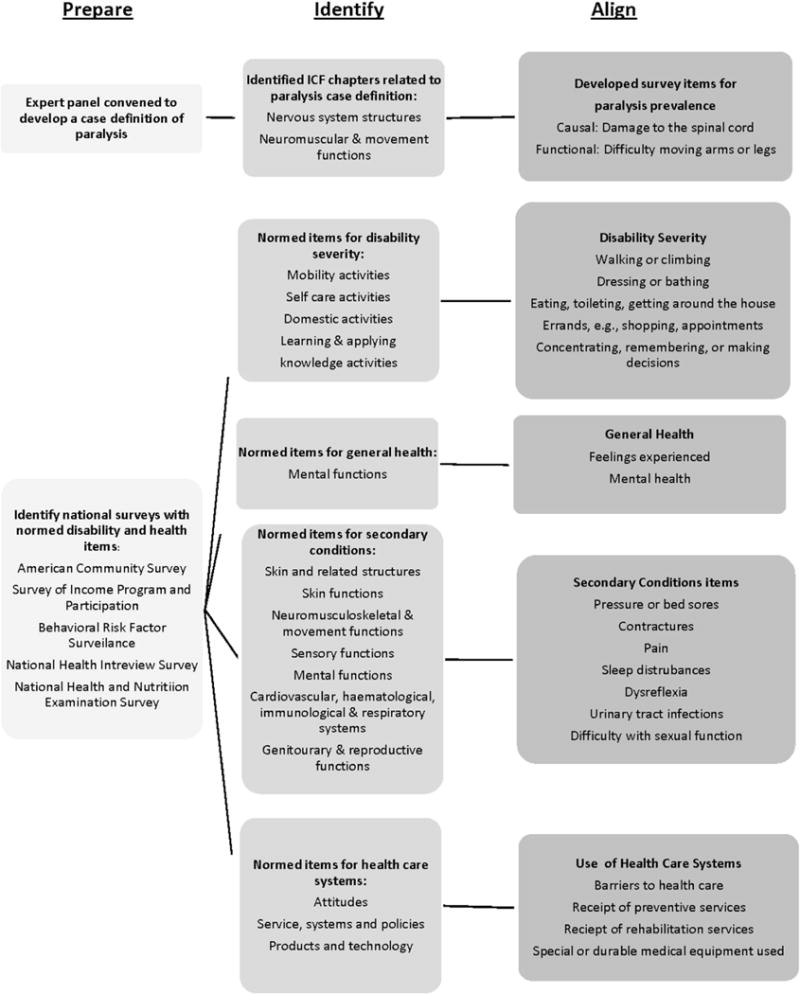
Integrating the International Classification of Functioning, Disability and Health (ICF) into National Paralysis Surveillance.
Validation of paralysis and etiology
The final validation protocol for the self-definition of paralysis included questions on what caused the difficulty (maximum 9 depending on skip pattern), type of SCI (5), and treatment received after spinal cord injury including location of treatment (11). Questions included: Currently, how difficult is it for you to move your arms and/or legs? This difficulty in movement is due to? What accident or injury caused your difficulty in moving? What condition or disease caused your difficulty in moving? What condition were you born with that caused your difficulty in moving? Which of these do you think caused your difficulty in moving? When did this happen? Complete survey is available from the authors upon request.
Prevalence rates and the epidemiology of paralysis
Prevalence estimates and characteristics of people living with paralysis were generated from each of the two field surveys. Estimates for both surveys were very similar, documenting our ability to replicate overall prevalence using the more rigorous study protocol put in place for the 2012–2013 survey, while retaining the use of the ICF framework on which both surveys were developed. Detailed findings of the 2012–2013 survey will be presented in a subsequent publication.
Discussion and conclusion
This study demonstrates that a functional definition of paralysis based on the ICF can be used as a surveillance tool. This approach can be relevant for monitoring prevalence and learning more about the epidemiology of other disabling conditions as well, such as communication or sensory impairments. For these types of disability, a functional definition can capture more useful information on independent living, which can vary considerably over the life course and at different times for individuals depending on environment and nature of the condition.
While this conceptual approach is not new,19 it can be more frequently applied in ways that complement traditional approaches to surveillance based upon diagnoses alone, and allow for improved understanding of other factors such as health care and social services use, and daily assistance of people with the specified condition.31 The use of models of disability that blend medical, functional and social models can allow public health to expand its focus to examine the complex interplay between characteristics of an individual – including medically based impairments – and the multiple environments within which people with disabilities live, while also considering physical and socio-emotional health, cost of care and quality of life issues.
Supplementary Material
Acknowledgments
This publication was made possible through grant number 90PR3001 from the Administration for Community Living and prior grant number HHS1U59DD000838 from the Centers for Disease Control and Prevention.
Footnotes
The findings and conclusions in this report are those of the authors and do not necessarily represent the official position of the Centers for Disease Control and Prevention or the Administration on Community Living.
Supplementary data
Supplementary data related to this article can be found at http://dx.doi.org/10.1016/j.dhjo.2015.03.002.
References
- 1.Fox MH, Rowland JL, Froehlich-Grobe K, Vernberg D, White GW, Haskett L. Determining paralysis prevalence in the United States. Disabil Health J. 2008;1(3):172–179. doi: 10.1016/j.dhjo.2008.05.003. [DOI] [PubMed] [Google Scholar]
- 2.United States. Congress. House. Committee on Energy and Commerce. (Report U.S. Government Printing Office).Christopher and Dana Reeve Paralysis Act: Report (To Accompany HR 1727) (Including Cost Estimate of the Congressional Budget Office) 2007;110(378) http://www.gpo.gov/fdsys/pkg/CRPT-110hrpt937/html/CRPT-110hrpt937.htm. Accessed 09.07.13. [Google Scholar]
- 3.Christopher and Dana Reeve Paralysis Act. Disability and Health Program; 2013. (Centers for Disease Control and Prevention: 10). Available at: http://www.cdc.gov/ncbddd/disabilityandhealth/programs.html. Accessed 09.07.13. [Google Scholar]
- 4.Krahn G, McCarthy M, Dean Westwood D, Powers L. Evaluation of an innovative methodology to recruit research participants with spinal cord injury through durable medical equipment suppliers. Arch Phys Med Rehabil. 2008;89(7):1341–1349. doi: 10.1016/j.apmr.2007.11.035. [DOI] [PubMed] [Google Scholar]
- 5.Prencipe M, Ferretti C, Casini AR, Santini M, Giubilei F, Culasso F. Stroke, disability, and dementia: results of a population survey. Stroke. 1997;28(3):531–536. doi: 10.1161/01.str.28.3.531. [DOI] [PubMed] [Google Scholar]
- 6.DeVivo M. Epidemiology of traumatic spinal cord injury: trends and future implications. Spinal Cord. 2012;50(5):365–372. doi: 10.1038/sc.2011.178. [DOI] [PubMed] [Google Scholar]
- 7.Blumer CE, Quine S. Prevalence of spinal cord injury: an international comparison. Neuroepidemiology. 1995;14(5):258–268. doi: 10.1159/000109801. [DOI] [PubMed] [Google Scholar]
- 8.Baum HM, Rothschild BB. The incidence and prevalence of reported multiple sclerosis. Ann Neurol. 1981;10(5):420–428. doi: 10.1002/ana.410100504. [DOI] [PubMed] [Google Scholar]
- 9.Anderson DW, Ellenberg JH, Leventhal CM, Reingold SC, Rodriguez M, Silberberg DH. Revised estimate of the prevalence of multiple sclerosis in the United States. Ann Neurol. 1992;31(3):333–336. doi: 10.1002/ana.410310317. [DOI] [PubMed] [Google Scholar]
- 10.Noonan CW, Kathman SJ, White MC. Prevalence estimates for MS in the United States and evidence of an increasing trend for women. Neurology. 2002;58(1):136–138. doi: 10.1212/wnl.58.1.136. [DOI] [PubMed] [Google Scholar]
- 11.Noonan CW, Williamson DM, Henry JP, et al. The prevalence of multiple sclerosis in 3 US communities. Prev Chronic Dis. 2010;7(1):A12. [PMC free article] [PubMed] [Google Scholar]
- 12.Verbrugge LM, Jette AM. The disablement process. Soc Sci Med. 1994;38(1):1–14. doi: 10.1016/0277-9536(94)90294-1. [DOI] [PubMed] [Google Scholar]
- 13.Areheart B. When disability isn’t “Just Right”: the entrenchment of the medical model of disability and the Goldilocks Dilemma. Indiana Law J. 83(1) Article 5. Available at: http://www.repository.law.indiana.edu/ilj/vol83/iss1/5. [Google Scholar]
- 14.Nagi SZ. Some conceptual issues in disability and rehabilitation. In: Sussman MB, editor. Sociology and Rehabilitation. Washington: American Sociological Association; 1965. pp. 100–113. [Google Scholar]
- 15.Pope AM, Tarlov AR, editors. Disability in America: Toward a National Agenda for Prevention. Washington: National Academy Press; 1991. [Google Scholar]
- 16.World Health Organization. International Classification of Functioning, Disability and Health (ICF) Geneva, Switzerland: Author; 2001. Available at: http://www.who.int/classifications/icf/en/ [Google Scholar]
- 17.Field M, Jette A, editors. The Future of Disability in America Institute of Medicine. National Academy Press; 2007. p. 30. [PubMed] [Google Scholar]
- 18.World Health Organization. How to Use the ICF: A Practical Manual for Using the International Classification of Functioning, Disability and Health (ICF). Exposure Draft for Comment. Geneva: WHO; Oct, 2013. Available at: http://www.who.int/classifications/drafticfpracticalmanual.pdf. [Google Scholar]
- 19.Bruyère S, VanLooy S, Peterson D. The international classification of functioning, disability and health (ICF): contemporary literature overview. Rehabil Psychol. 2005;50(2):113–121. [Google Scholar]
- 20.Jette A. Invited commentary. Phys Ther. 2008;88:851–853. doi: 10.2522/ptj.20070211.ic. [DOI] [PubMed] [Google Scholar]
- 21.Cieza A, Stucki G. Content comparison of health-related quality of life (HRQOL) instruments based on the international classification of functioning, disability and health (C+ICF) Qual Life Res. 2005;14:1225–1237. doi: 10.1007/s11136-004-4773-0. [DOI] [PubMed] [Google Scholar]
- 22.Stucki G, Cieza A. The International Classification of Functioning, Disability and Health (ICF) core sets for rheumatoid arthritis: a way to specify functioning. Ann Rheum Dis. 2005;63(suppl 2):ii40–ii45. doi: 10.1136/ard.2004.028233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Geyh S, Cieza A, Kollerits B, Grimby G, Stucki G. Content comparison of health-related quality of life measures used in stroke based on the international classification of functioning, disability and health (ICF): a systematic review. Qual Life Res. 2007;16:833–851. doi: 10.1007/s11136-007-9174-8. [DOI] [PubMed] [Google Scholar]
- 24.Gelinas I, Gauthier L, McIntire M, Gauthier S. Development of a functional measure for persons with Alzheimer’s disease: the disability assessment for dementia. Am J Occup Ther. 1999;53:471–483. doi: 10.5014/ajot.53.5.471. [DOI] [PubMed] [Google Scholar]
- 25.Swanson G, Corrothers L, Mulhorn K. Comparing disability survey questions in five countries: a study using the ICF to guide comparisons. Disabil Rehabil. 2003;25(11–12):665–675. doi: 10.1080/0963828031000137162. [DOI] [PubMed] [Google Scholar]
- 26.Sinclair LB, Fox MH, Betts DR. A tool for enhancing strategic planning: a modeled use of the International Classification of Functioning, Disability and Health. Int J Health Plann Manage. 2013 Apr-Jun;28(2):172–180. doi: 10.1002/hpm.2125. http://dx.doi.org/10.1002/hpm.2125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Howard D, Nieuwenhuijsen ER, Saleeby P. Health promotion and education: application of the ICF in the US and Canada using an ecological perspective. Disabil Rehabil. 2008;30(12–13):942–954. doi: 10.1080/09638280701800483. [DOI] [PubMed] [Google Scholar]
- 28.Fox MH, Rowland JL, Froelich-Grobe K, Vernberg D, White GW. Developing an Action Plan to Improve the Quality and the Quantity of Paralysis Data. Department of Health Policy and Management, University of Kansas Medical Center; Sep, 2005. Available at: http://www.rtcil.org/~rtcil/products/RTCIL%20publications/Health%20Issues/Executive%20Summary%20Developing%20an%20Action%20Plan%20to%20Improve%20the%20Quality%20and%20Quantity%20of%20Data%20About%20Paralysis.pdf. Accessed 04.08.14. [Google Scholar]
- 29.Christopher and Dana Reeve Foundation Paralysis Resource Center. First Report of the Working Group on Developing a Paralysis Survey Module and an Implementation Strategy to Gather National Level Data on Paralysis. Short Hills, NJ: Author; Nov, 2006. Available at: http://cdd.unm.edu/cms/Programs/dhpd/pdfs/actionPlanPress.pdf. Accessed 20.01.15. [Google Scholar]
- 30.ICR-SSRS. 53 West Baltimore Pike, Media, Pennsylvania. :19063. www.icrsurvey.com.
- 31.Jones GC, Sinclair LB. Multiple health disparities among minority adults with mobility limitations: an application of the ICF framework and codes. Disabil Rehabil. 2008;30(12–13):901–905. doi: 10.1080/09638280701800392. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


