Abstract
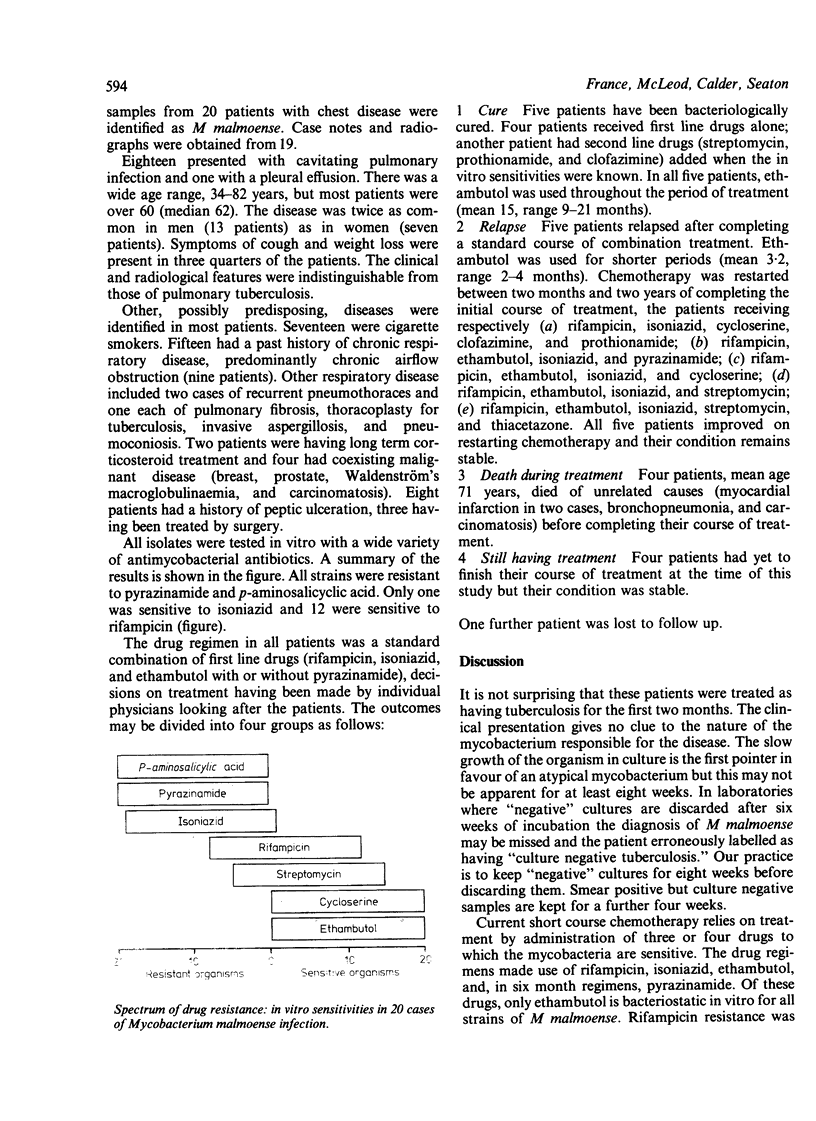
During 1982-4 20 cases of Mycobacterium malmoense infection were identified in Scotland (13 male, seven female; age 34-82, median 62 years). Features of the disease were obtained from case notes and radiographs of 19 patients and were found to be indistinguishable from those of patients with pulmonary tuberculosis. Chronic chest disease, predominantly chronic airflow obstruction, was the most frequent associated disease. The organisms showed in vitro resistance in eight patients to rifampicin, in 19 patients to isoniazid, and in all patients to pyrazinamide and p-aminosalicylic acid. Nevertheless, all patients showed an early response to standard combination chemotherapy with rifampicin, isoniazid, and ethambutol, with or without pyrazinamide. Five have been cured and none had died of the infection, although four died of unrelated disease. Of nine patients still having treatment, five had relapsed after completing a course of antituberculosis drugs. All had received ethambutol for less than five months. The response to standard drugs was more satisfactory when the course included administration of ethambutol for at least nine months. Currently one new infection with M malmoense occurs in Scotland for every 40 with tuberculosis, and the incidence appears to be rising. In view of this, it is suggested that when tuberculosis is suspected the chemotherapeutic regimen should include ethambutol until the culture results are reported. If these then show M malmoense, ethambutol should be continued in the combination for at least nine months.
Full text
PDF

Images in this article
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Banks J., Jenkins P. A., Smith A. P. Pulmonary infection with Mycobacterium malmoense--a review of treatment and response. Tubercle. 1985 Sep;66(3):197–203. doi: 10.1016/0041-3879(85)90037-6. [DOI] [PubMed] [Google Scholar]
- Barclay J., Stanbridge T. N., Doyle L. Pneumonectomy for drug resistant mycobacterium malmoense. Thorax. 1983 Oct;38(10):796–797. doi: 10.1136/thx.38.10.796. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grange J. M., Yates M. D. Infections caused by opportunist mycobacteria: a review. J R Soc Med. 1986 Apr;79(4):226–229. doi: 10.1177/014107688607900411. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jenkins P. A. Mycobacterium malmoense. Tubercle. 1985 Sep;66(3):193–195. doi: 10.1016/0041-3879(85)90036-4. [DOI] [PubMed] [Google Scholar]
- Jenkins P. A., Tsukamura M. Infections with Mycobacterium malmoense in England and Wales. Tubercle. 1979 Jun;60(2):71–76. doi: 10.1016/0041-3879(79)90038-2. [DOI] [PubMed] [Google Scholar]
- Roberts C., Clague H., Jenkins P. A. Pulmonary infection with Mycobacterium malmoense: a report of 4 cases. Tubercle. 1985 Sep;66(3):205–209. doi: 10.1016/0041-3879(85)90038-8. [DOI] [PubMed] [Google Scholar]
- Warren N. G., Body B. A., Silcox V. A., Matthews J. H. Pulmonary disease due to Mycobacterium malmoense. J Clin Microbiol. 1984 Aug;20(2):245–247. doi: 10.1128/jcm.20.2.245-247.1984. [DOI] [PMC free article] [PubMed] [Google Scholar]