Abstract
Abundant expression of aspartyl-(asparaginyl)-β-hydroxylase (AAH) correlates with infiltrative growth of hepatocellular carcinoma (HCC). Herein, we examine the role of phosphorylation in relation to AAH's protein expression, hydroxylase activity, promotion of cell motility, and activation of Notch signaling in human Huh7 hepatoma cells. Predicted glycogen synthase kinase-3β (GSK-3β), protein kinase A (PKA), protein kinase C (PKC), and casein kinase 2 (CK2) phosphorylation sites encoded by human AAH cDNA were ablated by S/T→A site-directed mutagenesis using N-Myc-tagged constructs in which gene expression was controlled by a cytomegalovirus promoter. Functional consequences were assessed in transiently transfected Huh7 cells. Cells transfected with wildtype AAH had significantly increased AAH expression, catalytic activity, HES-1 expression, and directional motility relative to controls. Single phosphorylation site mutations in the C-terminus largely abrogated these effects and further inhibited catalytic activity relative to that in cells transfected with empty vector, whereas the effects of single point mutations within the N-terminus were more varied. In contrast, AAH cDNAs carrying multiple phosphorylation site mutations exhibited wildtype levels of AAH catalytic activity suggesting that the effects of AAH phosphorylation are complex and non-uniform. AAH expression and function can be modulated by direct phosphorylation of the protein. These findings suggest additional strategies for inhibiting infiltrative growth of HCC.
Key Words: Aspartyl-(asparaginyl)-β-hydroxylase, Cell motility, Hepatocellular carcinoma, Notch, Phosphorylation
Introduction
Hepatocellular carcinoma (HCC) is the third leading cause of cancer-related death worldwide [1] and the fastest growing cause of cancer mortality among males in the United States [2]. The molecular pathogenesis of HCC involves dysregulation of cell cycle checkpoints, apoptosis [3,4,5], and growth factor signaling [6,7,8]. Our focus has been on the role of insulin/insulin-like growth factor (IGF) signaling because these pathways, particularly through phosphoinositide 3-kinase (PI3 K)-Akt, are highly activated in the majority of HCCs as a result of gain-of-function mutations in PI3 K [9], impaired expression/function of phosphatase and tensin homolog (PTEN) [10], and enhanced IGF-activated signaling through insulin receptor substrate type 1 (IRS-1) [8]. Importantly, insulin/IGF signaling regulates expression and function of aspartyl-(asparaginyl)-β-hydroxylase (AAH), which promotes cell motility and invasion [11,12,13,14]. Moreover, AAH could serve as a biomarker for HCC because its expression correlates with malignant transformation, aggressive histological grade, response to treatment, and prognosis [11,15,16,17].
AAH is an ∼86 kD [18] type 2 transmembrane protein located in the endoplasmic reticulum (ER) [19,20], as well as on plasma membranes of malignant neoplastic cells [14,18]. AAH is physiologically cleaved into a ∼30-34 kD N-terminal fragment that is identical to Humbug, a truncated isoform that binds to calcium and promotes adhesion [21,22], and a ∼52-56 kD catalytically active C-terminal domain that contains a 675-His residue that is essential for hydroxylation activity [23]. AAH hydroxylates β-carbons of specific aspartate (Asp) and asparagine (Asn) residues within consensus sequences of epidermal growth factor (EGF)-like domains of targets [24] such as Notch and Jagged [11,25,26]. In HCC, AAH's role in activating Notch is supported by the findings that: (1) Notch-1 and its natural ligand Jagged-1 have consensus sequences for AAH hydroxylation; (2) AAH physically interacts with Notch-1 and Jagged-1; and (3) AAH, Notch-1, and Jagged-1 are up-regulated in HCC [11].
Notch signaling is activated by binding of Jagged (or the Delta-like family of proteins) to Notch's extracellular domain. This action triggers metalloprotease-dependent cleavage of the extracellular domain from the membrane, followed by rapid presenilin protease cleavage of the intracellular domain [27]. The free Notch intracellular domain (NID) translocates from the plasma membrane to the nucleus where it complexes with the centromere binding factor 1 (CBF1) transcriptional activator, suppressor of hairless or lag-1 (CSL), and transcriptional co-activators of the Mastermind-like family of proteins. The resulting NID-complex binds to DNA containing CSL recognition sequences, recruits additional factors, and activates transcription of downstream targets, such as hairy and enhancer of split-1 (HES-1) and HES-related proteins [27,28].
AAH gene expression is regulated by insulin/IGF signaling through extracellular signal-regulated (ERK)/mitogen-activated protein kinase (MAPK) [8,29,30] and PI3 K-Akt [31]. In addition, AAH is regulated by glycogen synthase kinase-3β (GSK-3β), protein kinase A (PKA), protein kinase C (PKC), and casein kinase 2 (CK2), each of which could potentially phosphorylate AAH protein [26,31,32,33]. Thus far, most of the work done on this topic has concerned the role of GSK-3β. Previous studies showed that chemical or siRNA inhibition of GSK-3β increases AAH protein expression and cell motility, whereas increased GSK-3β activity decreases AAH protein expression and cell migration [26,32]. Additional studies demonstrated that AAH protein could be phosphorylated [31,32]. That AAH likely undergoes post-translational modification is supported by its ∼140 kD size on sodium dodecyl sulfate polyacrylamide gel electrophoresis versus its predicted ∼86 kD molecular mass. On the other hand, it has not yet been determined whether the effects of kinase manipulation on AAH expression and function are direct and due to AAH phosphorylation, or indirect and mediated by other cellular responses. The present study examines the functional consequences of mutating GSK-3β, PKA, PKC, and CK2 phosphorylation sites on AAH.
Reagents and Methods
Reagents
The QuickChange Site-directed Mutagenesis Kit was from Stratagene (La Jolla, CA, USA). Escherichia coli DH5α cells, Dulbecco's modified Eagle's medium (DMEM), Lipofectamine 2000 Transfection Reagent, TRizol, Amplex UltraRed, and 4-methylumbelliferyl phosphate (4-MUP) were purchased from Invitrogen (Carlsbad, CA, USA). The pcDNA 3 vector with a 6× Myc-tag was a gift from Dr. Y. Eugene Chin (Brown University, Providence, RI, USA) [34]. The QIAquick Gel Extraction Kit, QIAprep Spin Miniprep Kit, and RNeasy Lipid Tissue Mini Kit were purchased from Qiagen (Valencia, CA, USA). MaxiSorb plates, OptiPlates (96-well), BD Falcon culture inserts, and Nunc culture supplies were obtained from Thermo Scientific (Rochester, NY, USA). ATPlite reagents were purchased from Perkin-Elmer (Waltham, MA, USA). Myc antibody was purchased from Cell Signaling Technologies (Danvers, MA, USA). Bicinchoninic assay and enhanced chemiluminescence reagents and DyLight 547 conjugated to streptavidin were purchased from Pierce (Rockford, IL, USA). Rabbit polyclonal antibody to large acidic ribosomal protein (RPLPO) was purchased from Proteintech (Chicago, IL, USA). Alkaline phosphatase conjugated to streptavidin was purchased from Vector Laboratories (Burlingame, CA, USA). Positive-charge glass microscope slides were from Fisher Scientific (Pittsburgh, PA, USA). The Shandon Cytospin Centrifuge 3 was obtained from Thermo Shandon (Pittsburgh, PA, USA). The SpectraMax M5 microplate reader and Kodak PhosphorImager Screen S0230 with cassette were from Molecular Dynamics (Sunnyvale, CA, USA). Histofix was purchased from Amresco (Solon, Ohio, USA). The AMV First Strand cDNA Synthesis Kit, probe-based primer pairs (Universal ProbeLibrary Assay Design Center), and LightCycler 480 system were from Roche (Indianapolis, IN, USA). MacVector 10 software was purchased from MacVector, Inc. (Cary, NC, USA). Re-usable Boyden chambers were obtained from Neuro Probe (Gaithersburg, MD, USA). α-[14C]-Ketoglutaric acid was purchased from NEN Life Science (Boston, MA, USA). Glass fiber filter paper (GF/C) was purchased from Packard Instruments (Meriden, CT, USA). Other fine chemicals were purchased from CalBiochem (Carlsbad, CA, USA) or Sigma-Aldrich (St. Louis, MO, USA).
Recombinant AAH Plasmid Constructs
The coding region of human AAH was amplified from a 293T cDNA library by the polymerase chain reaction (PCR) using the forward primer 5′-cggaattcatggcccagcgtaagaatgcca-3′, reverse primer 5′-ccgctcgagctaaattgctggaaggctgc-3′, and Pfu DNA polymerase. The AAH PCR product was digested with EcoRI and XhoI restriction enzymes and gel purified with the QIAquick Gel Extraction Kit, cloned into the pcDNA 3 vector with a 5′-end 6× Myc-tag (pN-Myc-AAH), and transformed into Escherichia coli DH5α competent cells. Ampicillin-resistant clones were cultured in Luria Broth and recombinant plasmids were purified with the QIAprep Spin Miniprep Kit. Cloned inserts and their orientations were verified by DNA sequencing of both strands and Western blot analysis of recombinant protein expressed in 293 or Huh7 cells. Point mutations were made in serine and threonine codons predicted to be phosphorylated by GSK-3β, PKC, PKA, or CK2 (fig. 1) [32] using gene-specific primers (table 1) and the QuickChange Site-directed Mutagenesis kit. Serine/threonine residues were converted to alanine (S/T→A). Mutations were confirmed by direct sequencing of both cDNA strands and expression of the correct size protein was demonstrated by Western blot analysis using Myc and AAH antibodies.
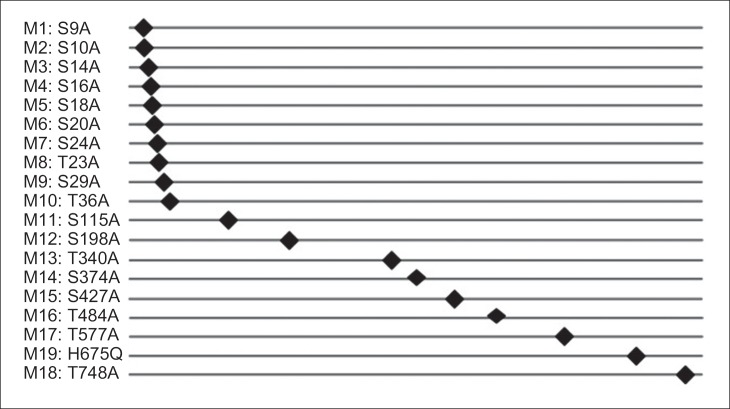
Fig. 1.
Site-directed mutants generated with the WT N-Myc-AAH construct: Ser/Thr residues within predicted phosphorylation sites were mutated to Ala using the Quick-Change Site-Directed mutagenesis kit and primer pairs listed in table 1.
Table 1.
Primer pairs for site-directed mutagenesis of N-Myc-AAH
| Primer | Sequence (5′→3′) | Primer | Sequence (5′→3′) |
|---|---|---|---|
| S9A (M1)-F | GCGTAAGAATGCCAAGGCC | S115A (M11)-F | CTTAAAGAGAGATCTACTGC |
| AGCGGCAACAGCAGCAG | AGAGCCAGCAGTCC | ||
| S9A (M1)-R | CTGCTGCTGTTGCCGCTGGC | S115A (M11)-R | GGACTGCTGGCTCTGCAGTAG |
| CTTGGCATTCTTACGC | ATCTCTCTTTAAG | ||
| S10A (M2)-F | GTAAGAATGCCAAGAGCGCC | S198A (M12)-F | GTAGATGATAGATTTGAGGCC |
| GGCAACAGCAGCAGCAG | CTGGAACCTGAAG | ||
| S10A (M2)-R | CTGCTGCTGCTGTTGCCGGC | S198A (M12)-R | CTTCAGGTTCCAGGGCCTC |
| GCTCTTGGCATTCTTAC | AAATCTATCATCTAC | ||
| S14A (M3)-F | GAGCAGCGGCAACAGCGCC | T340A (M13)-F | TAAATAAATTTGATAAGGC |
| AGCAGCGGCTCCGGCAG | TATTAAAGCTGAACTTG | ||
| S14A (M3)-R | CTGCCGGAGCCGCTGCTGGC | T340A (M13)-R | CAAGTTCAGCTTTAATAGCC |
| GCTGTTGCCGCTGCTC | TTATCAAATTTATTTA | ||
| S16A (M4)-F | GGCAACAGCAGCAGCGCCG | S374A (M14)-F | GCAAATACCCTCAGGCTCCAC |
| GCTCCGGCAGCGG | GAGCAAGATATG | ||
| S16A (M4)-R | CCGCTGCCGGAGCCGGCGCT | S374A (M14)-R | CATATCTTGCTCGTGGAGCCT |
| GCTGCTGTTGCC | GAGGGTATTTGC | ||
| S18A (M5)-F | CAGCAGCAGCGGCGCCGGC | S427A (M15)-F | GTTTGAAGCGTCGCGCAGACA |
| AGCGGTAGCAC | GGCAACAATTTC | ||
| S18A (M5)-R | GTGCTACCGCTGCCGGCGCC | S427A (M15)-R | GAAATTGTTGCCTGTCTGCG |
| GCTGCTGCTG | CGACGCTTCAAAC | ||
| S20A (M6)-F | GCAGCGGCTCCGGCGCCGGT | T484A (M16)-F | GAGGTGCTGAGTGTGGCACCT |
| AGCACGAGTGC | AATGATGGCTTTG | ||
| S20A (M6)-R | GCACTCGTGCTACCGGCGCC | T484A (M16)-R | CAAAGCCATCATTAGGTGCCA |
| GGAGCCGCTGC | CACTCAGCACCTC | ||
| S24A (M7)-F | GGCAGCGGTAGCGCGAGTG | T577A (M17)-F | CACAGCCTTGGTGGGCCCCAA |
| CGGGCAGCAG | AAGAAACGG | ||
| S24A (M7)-R | CTGCTGCCCGCACTCGCGCT | T577A (M17)-R | CCGTTTCTTTTGGGGCCCACC |
| ACCGCTGCC | AAGGCTGTG | ||
| T23A (M8)-F | GCAGCGGTAGCACGGCTGC | T748A (M18)-F | GCATCCGGAACTGGCACCACA |
| GGGCAGCAGCAG | GCAGAGAC | ||
| T23A (M8)-R | CTGCTGCTGCCCGCAGCCGT | T748A (M18)-R | GTCTCTGCTGTGGTGCCAGTT |
| GCTACCGCTGC | CCGGATGC | ||
| S29A (M9)-F | GGGCAGCAGCGCCCCCGGG | H675Q (M19)-F | CATGCACCCCGGGACTCAGGT |
| GCCCG | GTGGCCGCACACAGG | ||
| S29A (M9)-R | CGGGCCCCGGGGGCGCTGCT | H675Q (M19)-R | CCTGTGTGCGGCCACACCTGA |
| GCCC | GTCCCGGGGTGCATG | ||
| T36A (M10)-F | GCCCGGAGAGAGGCAAAGC | H675R (M20)-F | CATGCACCCCGGGACTCGCGT |
| ATGGAGGAC | GTGGCCGCACACAGG | ||
| T36A (M10)-R | GTCCTCCATGCTTTGCCTCTC | H675R (M20)-R | CCTGTGTGCGGCCACACGCGA |
| TCCGGGC | GTCCCGGGGTGCATG |
Ser/Thr residues on N-Myc-AAH predicted to be phosphorylated were mutated to Ala by site-directed mutagenesis using forward and reverse primer pairs containing a mutated nucleotide sequence (under-lined).
Cell Culture
Huh7 cells were maintained in DMEM supplemented with heat-inactivated 5% fetal bovine serum (FBS), 2 mM l-glutamine, and 1× non-essential amino acids in 5% CO2 at 37°C. To examine the effects of deleting specific phosphorylation sites on AAH, Huh7 cells were transiently transfected with wildtype or mutant pN-Myc-AAH using Lipofectamine 2000. Transfection efficiency was monitored by co-transfecting with recombinant plasmid containing green fluorescent protein (GFP) cDNA. Recombinant AAH and GFP expression were regulated by a cytomegalovirus (CMV) promoter.
Duplex Enzyme-linked Immunosorbent Assay
Duplex enzyme-linked immunosorbent assays (ELISAs) measured immunoreactivity to both target and loading control (large acidic ribosomal protein; RPLPO) proteins [35]. Huh7 cells were homogenized in radio-immunoprecipitation assay buffer supplemented with protease and phosphatase inhibitors [26]. Protein concentration was measured with the bicinchoninic acid assay. Protein homogenates (100 ng/50 µl) were adsorbed to the bottoms of FluoroNunc MaxiSorp 96-well plates by overnight incubation. Non-specific binding sites were blocked with 1% bovine serum albumin (BSA) in Tris-buffered saline (TBS). Primary antibody incubations were carried out overnight at 4°C with gentle platform rotation, and immunoreactivity was detected with horseradish peroxidase-conjugated secondary antibodies and Amplex UltraRed soluble fluorophore (Ex 530 nm/Em 590 nm). After rinsing, the protein samples were incubated with biotinylated anti-RPLPO, and immunoreactivity detected with streptavidin-conjugated alkaline phosphatase and the 4-MUP fluorophore (Ex 360 nm/Em 460 nm). Fluorescence was measured in a SpectraMax M5 microplate reader. Calculated ratios of target protein and RPLPO fluorescence were used for inter-group comparisons. Six or eight replicate samples were analyzed per group in each experiment.
Immunofluorescence
A total of 50,000 cells suspended in 10% FBS culture medium were cytocentrifuged onto positively-charged glass microscope slides using a Shandon Cytospin Centrifuge 3. The cells were fixed in Histofix and permeabilized by a 2-min incubation with 0.05% saponin in TBS. Non-specific binding sites were blocked with SuperBlock in TBS. Cells were incubated overnight with primary antibody (1:1000), and immunoreactivity was detected with biotinylated secondary antibody and streptavidin-conjugated Dy-Light 547 (Ex 557 nm/Em 574 nm) [11,14]. Cells were counterstained with 4′,6-diamidino-2-phenylindole (DAPI) and imaged by fluorescence or confocal microscopy.
14CO2 Capture Assay
The 14CO2 capture assay measures 14C-labeled CO2 released by the AAH hydroxylase reaction [36]. Briefly, MaxiSorp plates were coated with 400 ng of A85G6+A85E6+FB50 monoclonal AAH antibodies overnight at 4°C. The wells were incubated with PBS containing 1% BSA and 0.05% Tween-20 for 3 h to block non-specific binding sites. Samples containing 25 µg of Huh7 cellular protein in PBS were added to the wells to capture AAH. Negative and positive control reactions included 200 ng BSA and 200 ng recombinant AAH, respectively. To measure hydroxylase activity, 40-µl reaction cocktails containing 60 μM EGF-like peptide (60 μM), 40 μM [14C]-α-ketoglutaric acid in 50 mM PIPES pH 7.0, 100 mM NaCl, 100 μM FeCl2, and 0.2 mg/ml casein were added to each well. The plates were covered with GF/C soaked in 30 mM Ca(OH)2 and incubated for 1 h at 25°C under a heavy weight (lead brick) with a rubber dam between the plate and brick. The filter was dried and radioactivity was detected and quantified with a STORM 820 Phosphor Imager.
Quantitative Reverse Transcriptase-PCR
Huh7 cells were harvested in TRIzol and total cellular RNA was extracted with an RNeasy Lipid Tissue Mini Kit. cDNAs were generated with the AMV First Strand cDNA synthesis kit and random oligodeoxynucleotide primers. Gene expression was measured via hydrolysis probe-based duplex quantitative reverse transcriptase-PCR (qRT-PCR) using hypoxanthine-guanine phosphoribosyltransferase (HPRT) as reference gene and Taqman Gene Expression Master Mix. The final reactions (20 µl) contained 400 nM of primers for both HPRT and the gene of interest (GOI) and 200 nM of probes for HPRT (Y555 labeled) and GOI (FAM labeled). The amplification reactions were conducted for 45-50 cycles using the following program: 10 min at 95°C, 15 s at 95°C, and 1 min at 60°C. The amplifications were conducted using a LightCycler 480 and analyzed with the respective software. Fluorescence signals for the gene of interest and reference gene were acquired in the FAM Channel (Em range: 520-530 nm) and Y555/HEX channel (Em range: 550-568 nm) respectively. Primer sequences and matched probes were determined by using the ProbeFinder Software.
Directional Motility Assay
Directional motility was measured using the ATP luminescence-based motility invasion assay, which resembles the Boyden chamber assay with modifications that permit quantification of all cells [37]. Briefly, 1% FBS culture media was placed in the bottom blind well chambers, and 8-µm-pore polycarbonate membranes were inserted between the upper and lower chambers. A total of 100,000 viable cells suspended in 0.1% FBS culture media were seeded into each upper chamber. Reactions were incubated for 30 min at 37°C. Cells harvested from the upper chamber (non-motile), the under-surface of the membrane (migrated-adherent), and the lower chamber (migrated, non-adherent) were quantified using the ATPlite luminescence assay kit. Six replicate assays per condition were used for statistical analysis.
Statistical Analysis
Data depicted in the graphs represent the means ± standard error of the mean (S.E.M.) for each group. Inter-group comparisons were made using repeated measures of one-way analysis of variance (ANOVA) with the post hoc Fisher's least significant difference test. Statistical analyses were performed using GraphPad Prism 5 software. Significant p values are indicated over the bars or time-points (*p<0.05; ξp<0.05; **p<0.01; ξξp<0.01; ***p<0.001; ξξξp<0.001; ****p<0.0001; ξξξξp<0.0001).
Results
AAH S/T→A Mutations and AAH Protein Expression.
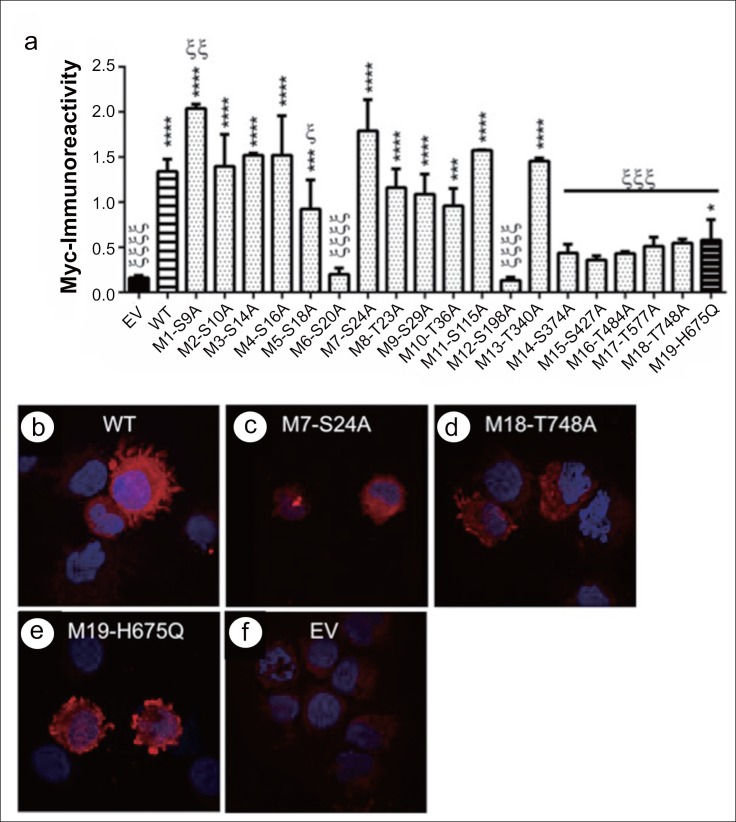
Duplex ELISAs were used to measure AAH protein expression in transfected Huh7 cells. To distinguish recombinant from endogenous AAH, immunoreactivity was detected with Myc antibody. Myc immunoreactivity was significantly higher in cells transfected with wild-type (WT) N-Myc-AAH than in cells transfected with empty vector (EV) (p<0.0001) (fig. 2a). Among the mutant N-Myc-AAH constructs, eight had very low levels of Myc immunoreactivity, only slightly higher than in EV-transfected cells; nine had Myc levels similar to WT; one had Myc levels that were significantly higher than in EV but below WT; and one had Myc levels significantly higher than WT (fig. 2a).
Fig. 2.
Effects of S/T→A mutations on AAH protein expression and subcellular localization: Huh7 cells were transiently transfected with wildtype (WT) or point-mutated (M#:S/T→A) N-Myc-AAH cDNA. Myc-empty vector (EV) served as a negative control. The M19-H675Q mutant, which disrupts AAH catalytic activity, served as a positive control. a Recombinant protein expression was measured by ELISA with the Myc antibody 24 h after transfection. The graph depicts mean (± S.E.M) levels of Myc. Inter-group comparisons were made by ANOVA with the post-hoc Fisher least significant difference (LSD) test. *p<0.05; **p<0.01; ***p<0.001; ****p<0.0001 for comparisons with EV, and ξp<0.05; ξξp<0.01; ξξξp<0.001; ξξξξp<0.0001 for comparisons with WT. (B-F) Representative results obtained by immunofluorescence staining and confocal imaging of cells transfected with (b) WT, (c) M7-S24A, (d) M18-T748A, (e) M19-H675Q, or (f) EV and stained by immunofluorescence with anti-Myc. Immunoreactivity was detected with biotinylated secondary antibody and streptavidin-conjugated DyLight 547 (red). Cells were counterstained with DAPI (blue). (Merged images: 600× magnification, 2× digital zoom).
As depicted in fig. 2a, in cells that were transfected with constructs in which the S/T→A mutations were closest to the N-terminus, Myc expression was broadly similar to WT, whereas in cells transfected with N-Myc-AAH-cDNAs in which S/T→A mutations were in the C-terminus which houses the catalytic domain, Myc immunoreactivity was comparable to the levels measured after transfection with EV. Mutation of the critical 675His residue to glutamine (M19-H675Q), which impairs AAH hydroxylase activity [15], inhibited Myc expression. Thus, M6-S20A, M12-T198A, M14-S374A, M15-S427A, M16-T484A, M17-T577A, and M19-H675Q mutations appeared to have had dominant-negative effects on AAH expression. Further analysis revealed that relative to WT, Myc expression was significantly increased in cells transfected with M1-S9A (p<0.01), but decreased in cells that overexpressed M5 (S18A; p<0.05), M6 (S20A; p<0.0001), M12 (T198A; p<0.0001), or M14 through M19 (p<0.001) (also see table 2). Taken together, except for cells that overexpressed M1-S9A, S/T→A single point mutations of AAH's predicted phosphorylation sites either decreased or failed to change AAH expression.
Table 2.
Effects of AAH Phosphorylation Site Mutations on the Protein's Subcellular Pattern of Distribution
| N-Myc-AAH Construct | ||||
|---|---|---|---|---|
| Staining Pattern | WT | M7-S24A | M18-T748A | M19-H675Q |
| Periphery/Podocyte | + | − | + | − |
| Particulate | − | + | + | + |
| Perinuclear | − | + | − | + |
Positive (+) sign represents markedly increased levels in specific staining patterns of immunofluorescence of the N-Myc-AAH construct, while the (-) sign indicates markedly reduced levels.
AAH S/T→A GSK-3β Site Mutations and Subcellular Localization of AAH
We examined the effects of S/T→A mutations on subcellular distributions of the AAH mutant constructs. Cells were cytocentrifuged onto glass slides and stained by immunofluorescence with Myc antibodies. Cells that overexpressed WT N-Myc-AAH (fig. 2b) or M1-S9A (not shown) exhibited bright red Myc immunoreactivity distributed throughout the cytoplasm and cellular processes. In contrast, overexpression of M7-S24A (fig. 2c) was associated with altered distributions of Myc immunoreactivity, manifested by loss of peripheral cytoplasmic and podocyte labeling. In cells transfected with cDNAs in which Myc immunoreactivity by ELISA was low-level and similar to EV, e.g. M18-T748A (fig. 2d), Myc immunofluorescence was mainly particulate, corresponding to microsomal or mitochondrial localizations. Finally, cells transfected with M19-H675Q exhibited a unique pattern of both peripheral/podocyte and particulate cytoplasmic labeling (fig. 2e). Cells transfected with Myc-EV constructs served as a negative control (fig. 2f).
S/T→A GSK-3β Site-directed Mutagenesis and AAH Hydroxylase Activity
AAH promotes cell migration and adhesion through hydroxylation of its target molecules. Therefore, we investigated the effects of S/T→A mutations on AAH's catalytic activity. The studies were focused on GSK-3β sites because of multiple prior evidence that phosphorylation could regulate expression and function of AAH protein. AAH catalytic activity was measured using a 14CO2 capture assay that quantifies 14C-labeled CO2 released as a by-product of hydroxylase activity [36]. Huh7 overexpressing WT N-Myc-AAH released significantly higher levels of 14CO2 (p<0.001) relative to non-transfected (NT) or EV control cells (fig. 3). Cells transfected with cDNAs that had single S/T→A mutations exhibited significantly lower levels of hydroxylase activity relative to NT and EV controls. We then considered the potential importance of having more than one site phosphorylated by generating mutant constructs with up to six GSK-3β S/T→A mutations. Inclusion of two to five S/T→A (#2, #7, #14, #15, and #17) in the construct rendered the hydroxylase activity similar to or significantly elevated relative to EV control and comparable to WT (fig. 3).
Fig. 3.
AAH catalytic activity assay results: AAH proteins expressed in transiently transfected (24 h) Huh7 cells were captured using a cocktail of monoclonal antibodies to ensure specificity of the reaction. AAH hydroxylase activity was measured with the 14CO2 capture assay using recombinant EGF peptide as the substrate. Released 14CO2 was measured with a Phosphor-Imager. The graph depicts the mean (± S.E.M.) levels of released 14CO2 (cpm)/μg protein. Inter-group comparisons with respect to EV were made using one-way repeated measures of ANOVA and the Fisher LSD post hoc test (*p<0.05; **p<0.01).
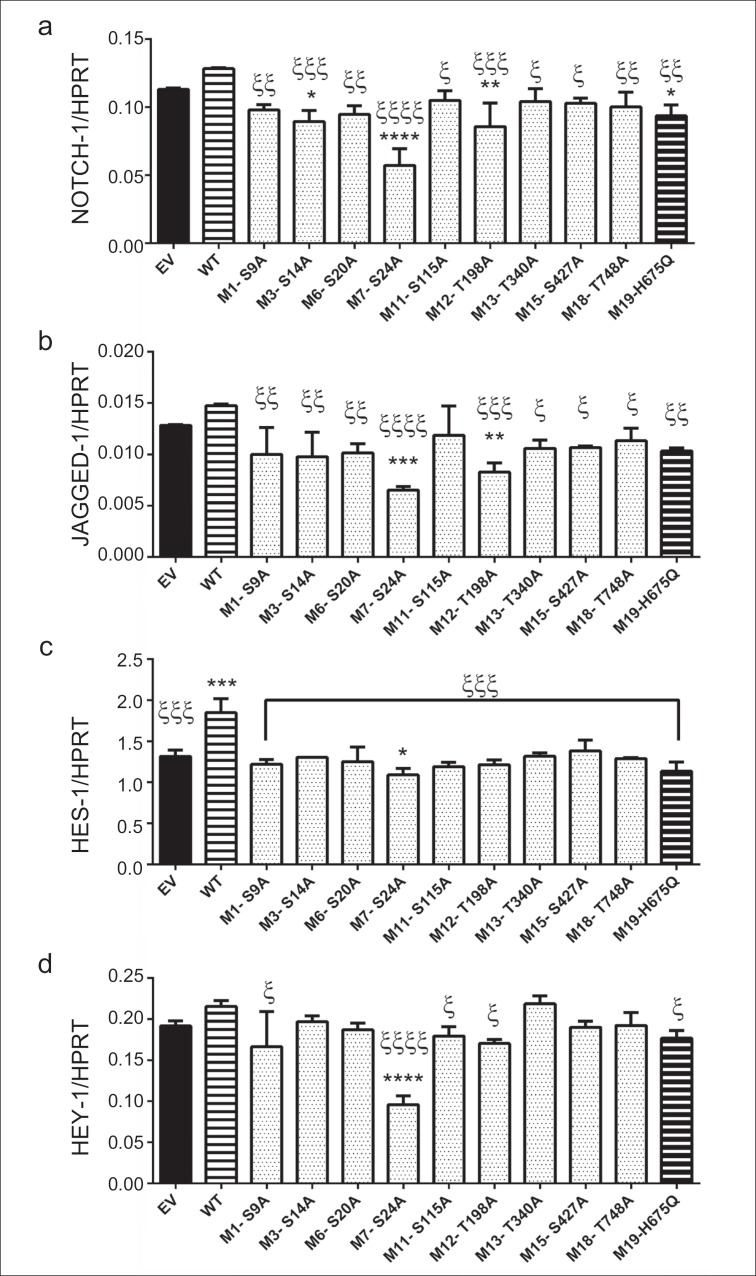
Effects on Notch Signaling Genes of GSK-3β S/T→A Site-directed Mutagenesis of AAH
We used qRT-PCR assays to examine the effects of deleting AAH GSK-3β sites on expression of critical Notch signaling genes. For comparison, we included the M19-H675Q mutant, which was previously shown to lack catalytic activity and inhibit cell motility [15]. Cells transfected with WT N-Myc-AAH had higher levels of Notch-1, Jagged-1, HES-1 and HEY-1 expression relative to EV-transfected cells, but the differences only reached statistical significance for HES-1 (fig. 4). Results of nine mutant cDNA constructs are shown in fig. 4. Notch-1 expression was significantly reduced relative to EV for three of the AAH S/T→A mutant constructs; the same was true for M19-H675Q (fig. 4a). However, the other six AAH S/T→A mutant cDNAs expressed Notch-1 at levels similar to EV, but significantly lower than with WT-AAH-transfected cells. Similar observations were made with respect to expression of Jagged-1. All the mutant constructs had HES-1 mRNA levels that were similar to the EV control except M7-S24A which was reduced, and all were significantly reduced relative to WT (fig. 4c). In contrast, only the M7-S24A mutant cDNA inhibited HEY-1 expression relative to EV and WT, whereas the other S/T→A mutant AAH cDNAs had levels of HEY-1 similar to WT or EV (fig. 4d). Note that only M7-S24A and M12-T198A significantly inhibited both Notch-1 and Jagged-1 expression, and that M7-S24A alone inhibited HES-1 (fig. 4c) and HEY-1 (fig. 4d) relative to EV and WT-AAH. This cDNA is of further interest because of its aberrant sub-cellular distribution away from the periphery and podocytes; it is found mainly in perinuclear or ER zones, away from cell surface Notch and Jagged.
Fig. 4.
WT and point-mutated AAH effects on Notch signaling genes: Huh7 cells transfected with WT or point-mutated N-Myc-AAH cDNAs were used in duplex qRT-PCR assays to measure (a) Notch-1, (b) Jagged-1, (c) HES-1, and (d) HEY-1 gene expression in which results were normalized to HPRT measured simultaneously in the same reactions. EV-transfected cells served as a negative control, while M19-H→Q-transfected cells served as a positive control for inhibiting Notch signaling due to loss of catalytic activity. Graphs depict the relative mean (± S.E.M) levels of target gene expression. Inter-group comparisons were made by one-way ANOVA with the post-hoc Fisher LSD test. *p<0.05; **p<0.01; ***p<0.001; ****p<0.0001 for comparisons with EV, and ξp<0.05; ξξp<0.01; ξξξp<0.001; ξξξξp<0.0001 for comparisons with WT.
Cell Adhesion and Motility Studies
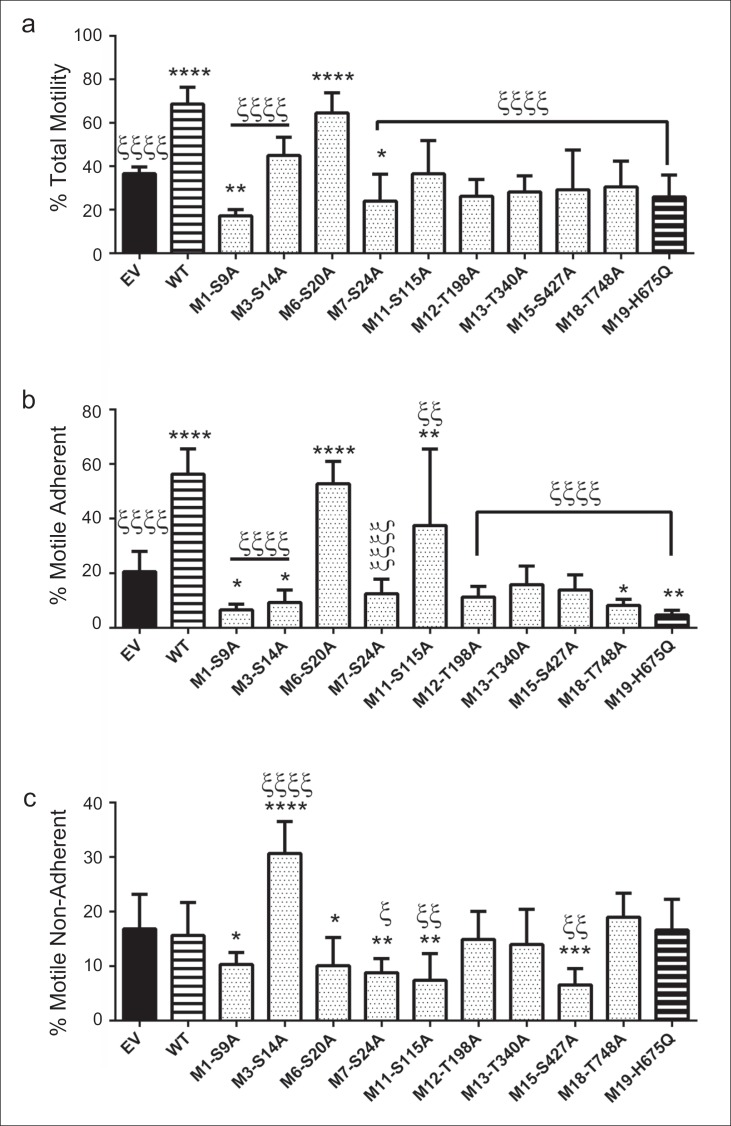
AAH hydroxylation of Notch and Jagged mediates cell adhesion and migration, which can be measured using the ATPlite-based directional motility and adhesion blind-well chamber assay [37]. Over-expression of WT N-Myc-AAH significantly increased total motility (fig. 5a) and the percentage of motile adherent cells (fig. 5b) relative to EV. In contrast, the percentages of motile non-adherent cells were similar in WT and EV assays (fig. 5c). All mutant cDNAs tested, including M19-H675Q but excluding M6-S20A, significantly reduced total motility indices relative to WT (fig. 5a). Two mutants, M1-S9A and M7-S24A, inhibited total motility relative to EV as well. Only one mutant (M6-S20A) had a similar mean total motility index compared with WT-AAH-transfected cells.
Fig. 5.
Directional motility and adhesion assays: Huh7 cells transiently transfected with EV, WT N-Myc-AAH, or point-mutated N-Myc-AAHs were used in an ATP luminescence-based assay that measures both directional cell motility and adhesion. In this Boyden-chamber type assay, 1% FBS was supplied as the trophic factor in the lower chamber (see Methods). Graphs depict mean (± S.E.M) percentages of (a) all motile cells, (b) motile-adherent cells, and (c) motile non-adherent cells in each assay chamber (see Methods). Inter-group comparisons were made by one-way ANOVA with post-hoc Fisher LSD tests. *p<0.05; **p<0.01; ***p<0.001; ****p<0.0001 for comparisons with EV, and ξp<0.05; ξξp<0.01; ξξξp<0.001; ξξξξp<0.0001 for comparisons with WT.
Motile adherent populations correspond to cells that are both motile and adherent. All but one (M6-S20A) mutant AAH cDNA construct significantly impaired cell adhesion relative to WT, and four mutants, including M19-H675Q, impaired cellular adhesion and motility relative to EV-transfected cells (fig. 5b). Motile non-adherent cells reflect populations prone to metastasize (migrate) to distant sites as a result of increased mobility vis-à-vis lack of adhesion. The M3-S14A cDNA mutant construct was the only one to exhibit significantly higher percentages of motile non-adherent cells relative to both EV and WT-AAH-transfected cells (fig. 5c). All other mutant constructs exhibited either reduced or similar percentages of motile non-adherent cell populations relative to the EV- and/or WT-AAH-transfected cells.
Discussion
AAH can be regarded as a distinct biomarker of hepatocellular carcinoma and a prognosticator of aggressiveness or responsiveness to treatment [11,12,17]. Insulin and IGF-1 stimulate AAH expression and function, resulting in increased cell adhesion and motility [11,12,13,31,32,38,39]. Although inhibition of GSK-3β [26,32] enhances AAH protein expression without altering its mRNA levels, further investigations showed that: (1) AAH protein has intrinsic phosphorylation sites, many of which correspond to GSK-3β motifs; (2) AAH protein can be phosphorylated by GSK-3β [26,32]; and (3) inhibition of other kinases predicted to phosphorylate AAH, i.e., PKC, PKA, and CK2, increased insulin/IGF-stimulated AAH expression/immunoreactivity and cell motility [31]. Despite the fact that AAH can be phosphorylated, in all previous studies, the effects of kinase activation or inhibition on AAH were indirect and therefore could have resulted from other cellular events. The novel aspect of the present work is that we examine whether AAH can be regulated by direct phosphorylation of its protein, and assess the effects of constitutively inhibiting phosphorylation on AAH expression, subcellular localization, and catalytic activity and on cell adhesion and directional motility. Moreover, since AAH promotes cell motility by activating Notch, we determined the impact of expressing AAH proteins mutated in specific phosphorylation sites on Notch-associated signaling proteins.
The use of a Myc-tagged AAH construct was invaluable for distinguishing recombinant from endogenous AAH protein, particularly since AAH is physiologically cleaved and its half-life is approximately 30 min, based on metabolic labeling studies [26]. Transfection studies using Huh7 cells demonstrated that the recombinant protein was highly expressed. Mutation of individual phosphorylation sites had two opposing effects that were largely driven by their positions within the molecule. Point mutations close to the N-terminus mainly resulted in similar or higher levels of AAH expression relative to WT, whereas those within the C-terminus were inhibitory. Mutation of the predicted GSK-3β site closest to the N-terminus was most effective in increasing AAH expression above WT, supporting our hypothesis that inhibition of GSK-3β-mediated phosphorylation of AAH can increase AAH expression. On the other hand, transfection with constructs carrying point mutations within the C-terminal region, which contains the catalytic domain, caused profound inhibition of AAH expression, corresponding to a dominant-negative effect. One possible interpretation of these findings is that AAH protein expression may be differentially regulated by site-specific phosphorylation. Although additional studies are needed for validation, we hypothesize that phosphorylation of AAH's N-terminus has different regulatory effects on AAH compared with C-terminus phosphorylation. For example, since deleting individual phosphorylation sites within the C-terminus broadly inhibited Myc-tagged AAH, Notch-1, HES-1, cell motility (motile-adherent population), and catalytic activity, physiological phosphorylation of these sites may have positive effects on AAH function. In contrast, the consequences of constitutively inhibiting phosphorylation of one or more GSK-3β sites within the N-terminus were more complex. Further studies are needed to assess the effects of short-term dynamic shifts in phosphorylation in relation to AAH expression and function.
In addition to altering the levels of protein expression, constitutive inhibition of AAH phosphorylation changed the patterns of its subcellular localization. Corresponding with ELISA and Western blot (not shown) results, Myc-AAH mutant cDNAs that substantially inhibited AAH protein expression resulted in low levels of AAH immunoreactivity by immunofluorescence. In addition, in contrast to the peripheral cellular and podocyte labeling, the patterns were more particulate, corresponding to the appearance of microsomal localization. One potential interpretation is that the C-terminal mutated Myc-AAH undergoes rapid degradation, accounting for the low levels of protein expression. Although mutation of the 675His residue also resulted in decreased Myc-AAH immunoreactivity, the cellular effects differed from those associated with reduced phosphorylation. Immunofluorescence/confocal imaging demonstrated that cells expressing M19-H675Q had peripheral cellular and podocyte labeling but with contraction of and blunting of podocytes. Therefore, the effects of the phosphorylation site and 675-His site mutations were dissimilar, most likely reflecting their different mechanisms of inhibiting AAH expression and function. Finally, observations with M7-S24A were of particular interest because, despite high levels of Myc-AAH expression, the sub-cellular localization of AAH was rendered highly abnormal, with AAH being mainly localized in the perinuclear zone rather than at the cell periphery and in podocytes. The functional consequences were demonstrated in subsequent experiments in which this pattern of immunofluorescence was associated with impairments in catalytic activity, Notch activation, and cell motility.
One of the key functions of AAH is its catalytic/hydroxylase activity that activates Notch signaling [15,18]. Previous studies showed that large increases in AAH expression were not required to confer increased cell motility and invasiveness, and that catalytic activity was most important [15]. Therefore, it was important to interpret the effects of phosphorylation site mutations in the context of AAH's function. Using the 14CO2 capture assay that quantifies 14C-labeled CO2 released with hydroxylase activity [36], we demonstrated significantly increased levels of catalytic activity in WT Myc-AAH-transfected cells, and reduced levels of catalytic activity (relative to EV) associated with most of the other point-mutated cDNAs. However, the finding that cells transfected with constructs carrying between two and five GSK-3β mutations exhibited higher or similar levels of catalytic activity compared with WT, suggests that dephosphorylation of multiple sites mediates AAH hydroxylase activity. Note that these effects were abrogated by the addition of the H675Q mutation, confirming its inhibitory effect on catalytic activity. These results support the hypothesis that phosphorylation of AAH protein regulates expression and function. An important mechanistic consideration is that conformational changes in AAH protein caused by phosphorylation/or dephosphorylation may alter AAH protein expression, sub-cellular distribution, and catalytic activity. Further studies are needed to address this question.
With regard to Notch signaling, WT Myc-AAH stimulated Notch-1, Jagged-1, HES-1 and HEY-1 gene expression, whereas the point-mutated Myc-AAH constructs did not, and instead resulted in gene expression similar to levels measured in Myc-EV-transfected cells. The effects on HEY-1 were less clear, in part due to the relatively low levels of expression compared with HES-1. However, results obtained with M7-S24A were especially notable because the significantly reduced levels of Notch-1, Jagged-1, HES-1, and HEY-1 expression correlated with the perinuclear rather than peripheral/podocyte distribution of immunoreactivity and with impairments in directional motility and adhesion. Reduced peripheral/surface localization of the protein would impair its ability to interact with Notch and the attendant activation of HES-1 and HEY-1 target genes.
The directional motility and adhesion studies confirmed that over-expression of WT Myc-AAH stimulates these functions in Huh7 cells. Point mutation of GSK-3β phosphorylation sites within the N-terminus of AAH had variable effects on overall motility and adhesion, whereas for the most part, point mutations in the C-terminus of AAH inhibited overall motility and adhesion, corresponding with the effects on AAH protein expression and catalytic activity. However, discordant results of note include: (1) M1-S9A, which exhibited the highest levels of AAH protein, produced the lowest levels of overall cell motility and was among the lowest with respect to cell adhesion; (2) M6-S20A had one of the lowest levels of AAH protein, but near WT levels of motility and adhesion; and (3) M3-S14A, which had WT levels of AAH, exhibited among the lowest levels of cell adhesion and the highest levels of non-adherent cell motility.
Altogether, the findings suggest that site-specific phosphorylation states of AAH can differentially modulate AAH protein expression, subcellular localization, catalytic activity, cell motility, and cell adhesion. Similar or more robust effects were observed using a human neuronal cell line transfected with the same cDNAs and analyzed using the same approaches (data not shown). In transfected Huh7 cells, variability with respect to specific aspects of AAH expression and function that were altered by expression of one or more of the constructs could reflect heterogeneity with respect to the impact phosphorylation has on AAH conformation, its ability to localize within the ER or plasma membranes, and its capacity to interact with and hydroxylate Notch. One unexpected finding was the dominant-negative effect several mutant constructs had on AAH. This result could be exploited for targeted treatment of HCCs to limit their tendency to infiltrative and metastatic spread.
Acknowledgements
Supported by AA11431, AA12908, and 5T32DK060415-10 from the National Institutes of Health.
References
- 1.El-Serag HB, Rudolph KL. Hepatocellular carcinoma: epidemiology and molecular carcinogenesis. Gastroenterology. 2007;132:2557–2576. doi: 10.1053/j.gastro.2007.04.061. [DOI] [PubMed] [Google Scholar]
- 2.Mittal S, El-Serag HB. Epidemiology of hepatocellular carcinoma: consider the population. J Clin Gastroenterol. 2013;47(Suppl):S2–S6. doi: 10.1097/MCG.0b013e3182872f29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Bressac B, Kew M, Wands J, Ozturk M. Selective G to T mutations of p53 gene in hepatocellular carcinoma from southern Africa. Nature. 1991;350:429–431. doi: 10.1038/350429a0. [DOI] [PubMed] [Google Scholar]
- 4.Galle PR, Krammer PH. CD95-induced apoptosis in human liver disease. Semin Liver Dis. 1998;18:141–151. doi: 10.1055/s-2007-1007150. [DOI] [PubMed] [Google Scholar]
- 5.Wright WE, Shay JW. The two-stage mechanism controlling cellular senescence and immortalization. Exp Gerontol. 1992;27:383–389. doi: 10.1016/0531-5565(92)90069-c. [DOI] [PubMed] [Google Scholar]
- 6.Chang L, Karin M. Mammalian MAP kinase signalling cascades. Nature. 2001;410:37–40. doi: 10.1038/35065000. [DOI] [PubMed] [Google Scholar]
- 7.Desbois-Mouthon C, Cacheux W, Blivet-Van Eggelpoël MJ, Barbu V, Fartoux L, Poupon R, Housset C, Rosmorduc O. Impact of IGF-1R/EGFR cross-talks on hepatoma cell sensitivity to gefitinib. Int J Cancer. 2006;119:2557–2566. doi: 10.1002/ijc.22221. [DOI] [PubMed] [Google Scholar]
- 8.Tovar V, Alsinet C, Villanueva A, Hoshida Y, Chiang DY, Solé M, Thung S, Moyano S, Toffanin S, Mínguez B, Cabellos L, Peix J, Schwartz M, Mazzaferro V, Bruix J, Llovet JM. IGF activation in a molecular subclass of hepatocellular carcinoma and pre-clinical efficacy of IGF-1R blockage. J Hepatol. 2010;52:550–559. doi: 10.1016/j.jhep.2010.01.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Lee JW, Soung YH, Kim SY, Lee HW, Park WS, Nam SW, Kim SH, Lee JY, Yoo NJ, Lee SH. PIK3CA gene is frequently mutated in breast carcinomas and hepatocellular carcinomas. Oncogene. 2005;24:1477–1480. doi: 10.1038/sj.onc.1208304. [DOI] [PubMed] [Google Scholar]
- 10.Hu TH, Huang CC, Lin PR, Chang HW, Ger LP, Lin YW, Changchien CS, Lee CM, Tai MH. Expression and prognostic role of tumor suppressor gene PTEN/MMAC1/TEP1 in hepatocellular carcinoma. Cancer. 2003;97:1929–1940. doi: 10.1002/cncr.11266. [DOI] [PubMed] [Google Scholar]
- 11.Cantarini MC, de la Monte SM, Pang M, Tong M, D'Errico A, Trevisani F, Wands JR. Aspartyl-asparagyl beta hydroxylase over-expression in human hepatoma is linked to activation of insulin-like growth factor and notch signaling mechanisms. Hepatology. 2006;44:446–457. doi: 10.1002/hep.21272. [DOI] [PubMed] [Google Scholar]
- 12.de la Monte SM, Tamaki S, Cantarini MC, Ince N, Wiedmann M, Carter JJ, Lahousse SA, Califano S, Maeda T, Ueno T, D'Errico A, Trevisani F, Wands JR. Aspartyl-(asparaginyl)-beta-hydroxylase regulates hepatocellular carcinoma invasiveness. J Hepatol. 2006;44:971–983. doi: 10.1016/j.jhep.2006.01.038. [DOI] [PubMed] [Google Scholar]
- 13.Maeda T, Sepe P, Lahousse S, Tamaki S, Enjoji M, Wands JR, de la Monte SM. Antisense oligodeoxynucleotides directed against aspartyl (asparaginyl) beta-hydroxylase suppress migration of cholangiocarcinoma cells. J Hepatol. 2003;38:615–622. doi: 10.1016/s0168-8278(03)00052-7. [DOI] [PubMed] [Google Scholar]
- 14.Sepe PS, Lahousse SA, Gemelli B, Chang H, Maeda T, Wands JR, de la Monte SM. Role of the aspartyl-asparaginyl-beta-hydroxylase gene in neuroblastoma cell motility. Lab Invest. 2002;82:881–891. doi: 10.1097/01.lab.0000020406.91689.7f. [DOI] [PubMed] [Google Scholar]
- 15.Ince N, de la Monte SM, Wands JR. Overexpression of human aspartyl (asparaginyl) β-hydroxylase is associated with malignant transformation. Cancer Res. 2000;60:1261–1266. [PubMed] [Google Scholar]
- 16.Xian ZH, Zhang SH, Cong WM, Yan HX, Wang K, Wu MC. Expression of aspartyl beta-hydroxylase and its clinicopathological significance in hepatocellular carcinoma. Mod Pathol. 2006;19:280–286. doi: 10.1038/modpathol.3800530. [DOI] [PubMed] [Google Scholar]
- 17.Wang K, Liu J, Yan ZL, Li J, Shi LH, Cong WM, Xia Y, Zou QF, Xi T, Shen F, Wang HY, Wu MC. Overexpression of aspartyl-(asparaginyl)-beta-hydroxylase in hepatocellular carcinoma is associated with worse surgical outcome. Hepatology. 2010;52:164–173. doi: 10.1002/hep.23650. [DOI] [PubMed] [Google Scholar]
- 18.Lavaissiere L, Jia S, Nishiyama M, de la Monte S, Stern AM, Wands JR, Friedman PA. Overexpression of human aspartyl(asparaginyl)beta-hydroxylase in hepatocellular carcinoma and cholangiocarcinoma. J Clin Invest. 1996;98:1313–1323. doi: 10.1172/JCI118918. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Jia S, VanDusen WJ, Diehl RE, Kohl NE, Dixon RA, Elliston KO, Stern AM, Friedman PA. cDNA cloning and expression of bovine aspartyl (asparaginyl) beta-hydroxylase. J Biol Chem. 1992;267:14322–14327. [PubMed] [Google Scholar]
- 20.Wang QP, VanDusen WJ, Petroski CJ, Garsky VM, Stern AM, Friedman PA. Bovine liver aspartyl beta-hydroxylase. Purification and characterization. J Biol Chem. 1991;266:14004–14010. [PubMed] [Google Scholar]
- 21.Lee JH. Overexpression of humbug promotes malignant progression in human gastric cancer cells. Oncol Rep. 2008;19:795–800. [PubMed] [Google Scholar]
- 22.Treves S, Feriotto G, Moccagatta L, Gambari R, Zorzato F. Molecular cloning, expression, functional characterization, chromosomal localization, and gene structure of junctate, a novel integral calcium binding protein of sarco(endo)plasmic reticulum membrane. J Biol Chem. 2000;275:39555–39568. doi: 10.1074/jbc.M005473200. [DOI] [PubMed] [Google Scholar]
- 23.Dinchuk JE, Henderson NL, Burn TC, Huber R, Ho SP, Link J, O'Neil KT, Focht RJ, Scully MS, Hollis JM, Hollis GF, Friedman PA. Aspartyl beta-hydroxylase (Asph) and an evolutionarily conserved isoform of Asph missing the catalytic domain share exons with junctin. J Biol Chem. 2000;275:39543–39554. doi: 10.1074/jbc.M006753200. [DOI] [PubMed] [Google Scholar]
- 24.McGinnis K, Ku GM, VanDusen WJ, Fu J, Garsky V, Stern AM, Friedman PA. Site-directed mutagenesis of residues in a conserved region of bovine aspartyl (asparaginyl) beta-hydroxylase: evidence that histidine 675 has a role in binding Fe2+ Biochemistry. 1996;35:3957–3962. doi: 10.1021/bi951520n. [DOI] [PubMed] [Google Scholar]
- 25.Gundogan F, Elwood G, Longato L, Tong M, Feijoo A, Carlson RI, Wands JR, de la Monte SM. Impaired placentation in fetal alcohol syndrome. Placenta. 2008;29:148–157. doi: 10.1016/j.placenta.2007.10.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Silbermann E, Moskal P, Bowling N, Tong M, de la Monte SM. Role of aspartyl-(asparaginyl)-β-hydroxylase mediated notch signaling in cerebellar development and function. Behav Brain Funct. 2010;6:68. doi: 10.1186/1744-9081-6-68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Greenwald I, Kovall R. Notch signaling: genetics and structure. WormBook. 2013;17:1–28. doi: 10.1895/wormbook.1.10.2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Weng AP, Aster JC. Multiple niches for Notch in cancer: context is everything. Curr Opin Genet Dev. 2004;14:48–54. doi: 10.1016/j.gde.2003.11.004. [DOI] [PubMed] [Google Scholar]
- 29.Boyault S, Rickman DS, de Reyniès A, Balabaud C, Rebouissou S, Jeannot E, Hérault A, Saric J, Belghiti J, Franco D, Bioulac-Sage P, Laurent-Puig P, Zucman-Rossi J. Transcriptome classification of HCC is related to gene alterations and to new therapeutic targets. Hepatology. 2007;45:42–52. doi: 10.1002/hep.21467. [DOI] [PubMed] [Google Scholar]
- 30.Dürr R, Caselmann WH. Carcinogenesis of primary liver malignancies. Langenbecks Arch Surg. 2000;385:154–161. doi: 10.1007/s004230050259. [DOI] [PubMed] [Google Scholar]
- 31.Lahousse SA, Carter JJ, Xu XJ, Wands JR, de la Monte SM. Differential growth factor regulation of aspartyl-(asparaginyl)-beta-hydroxylase family genes in SH-Sy5y human neuroblastoma cells. BMC Cell Biol. 2006;7:41. doi: 10.1186/1471-2121-7-41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Carter JJ, Tong M, Silbermann E, Lahousse SA, Ding FF, Longato L, Roper N, Wands JR, de la Monte SM. Ethanol impaired neuronal migration is associated with reduced aspartyl-asparaginyl-beta-hydroxylase expression. Acta Neuropathol. 2008;116:303–315. doi: 10.1007/s00401-008-0377-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.de la Monte SM, Tong M, Carlson RI, Carter JJ, Longato L, Silbermann E, Wands JR. Ethanol inhibition of aspartyl-asparaginyl-beta-hydroxylase in fetal alcohol spectrum disorder: potential link to the impairments in central nervous system neuronal migration. Alcohol. 2009;43:225–240. doi: 10.1016/j.alcohol.2008.09.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Yuan ZL, Guan YJ, Chatterjee D, Chin YE. Stat3 dimerization regulated by reversible acetylation of a single lysine residue. Science. 2005;307:269–273. doi: 10.1126/science.1105166. [DOI] [PubMed] [Google Scholar]
- 35.Lizarazo D, Zabala V, Tong M, de la Monte SM. Myriocin-ceramide inhibitor modulates insulin/IGF and ER stress pathways in experimental alcohol-related steatohepatitis. J Biochem Pharmacol Res. 2013;1:148–160. [Google Scholar]
- 36.Zhang JH, Qi RC, Chen T, Chung TD, Stern AM, Hollis GF, Copeland RA, Oldenburg KR. Development of a carbon dioxide-capture assay in microtiter plate for aspartyl-beta-hydroxylase. Anal Biochem. 1999;271:137–142. doi: 10.1006/abio.1999.4135. [DOI] [PubMed] [Google Scholar]
- 37.de la Monte SM, Lahousse SA, Carter J, Wands JR. ATP luminescence-based motility-invasion assay. Biotechniques. 2002;33:98–100. doi: 10.2144/02331rr01. 102, 104 passim. [DOI] [PubMed] [Google Scholar]
- 38.Gundogan F, Elwood G, Greco D, Rubin LP, Pinar H, Carlson RI, Wands JR, de la Monte SM. Role of aspartyl-(asparaginyl) beta-hydroxylase in placental implantation: Relevance to early pregnancy loss. Hum Pathol. 2007;38:50–59. doi: 10.1016/j.humpath.2006.06.005. [DOI] [PubMed] [Google Scholar]
- 39.Lawton M, Tong M, Gundogan F, Wands JR, de la Monte SM. Aspartyl-(asparaginyl) β-hydroxylase, hypoxia-inducible factor-α and Notch cross-talk in regulating neuronal motility. Oxid Med Cell Longev. 2010;3:347–356. doi: 10.4161/oxim.3.5.13296. [DOI] [PMC free article] [PubMed] [Google Scholar]