Abstract
Aim
The aim of this study was to analyze which variables predicted nursing home admission (NHA) and death.
Methods
1,001 recipients of domiciliary care were assessed three times in a 3-year period. Through bivariate and multivariate Cox proportional hazards regression models, associations between a covariate and the outcomes were analyzed.
Results
Participants with dementia had a higher risk of NHA (odds ratio 3.88, 95% confidence interval 2.92-5.16) compared to participants without dementia. The Neuropsychiatric Inventory sub-syndrome psychosis, poorer functional impairment and age were associated with NHA. Female sex, age, worse medical health and functional impairment were associated with death.
Conclusion
Support to the caregiver and education on how to meet and cope with behavioral disturbance, depressive mood and sub-syndrome psychosis will probably enable the family to better adapt to late life changes.
Key Words: Neuropsychiatric syndrome, Dementia, Community-dwelling, Older people, Domiciliary care
Introduction
Dementia is a common and serious disorder in later life that has profound consequences for individuals, their families and caregivers. It is a major cause for nursing home admission (NHA) with admission rates subsequent to dementia diagnosis around 20% after 1 year up to 50% after 5 years [1,2,3]. The median time from dementia diagnosis to NHA varies between 36 and 42 months [4]. Predictors for NHA are explained by individual characteristics, but also by the physical and social environment [5]. Co-living with people with dementia is reported to be challenging because of care dependency, impaired cognition and neuropsychiatric symptoms such as depression, anxiety, apathy and irritability [6]. Interventions among community-dwelling older people need to address the patient-caregiver dyad as a whole.
Neuropsychiatric syndromes (NPSs) are highly prevalent (up to 65%) among people with dementia [7]. NPSs are increasingly recognized as a major risk factor for caregiver burden, greater functional impairment, more rapid cognitive decline and poorer quality of life [8]. Depression, anxiety and irritability are likely risk factors for functional impairment because they are associated with decline in physical capacity in multiple cohorts [9].
Many reports show that age, general medical health, frailty, daily functioning, NPS and dementia are associated with both NHA and death [2,10,11,12,13,14,15]. Hallucinations and depression are associated with higher mortality [15], and major depression [16], delusions and agitation are reported to be associated with a higher risk of NHA [17,18]. However, Gaugler et al. [12] found no association between the presence of psychosis and earlier NHA. A number of studies have found overall behavioral symptoms to predict NHA [17,19,20,21].
This study targeted community-dwelling older people receiving domiciliary care. This is a vulnerable group with expected higher rates of NHA and death than in the normal population. In Norway, most people admitted to nursing homes have previously received some kind of domiciliary care [22]. Norwegian legislation makes domiciliary care a mandatory service in all municipalities. The service offered can be medical or practical [22].
Knowledge on how families and domiciliary services can manage and diminish risk factors for NHA is warranted. To our knowledge, no previous research has been performed among users of domiciliary care in order to map risk factors for NHA and death. Therefore, a study with a 3-year follow-up of 1,001 older people receiving domiciliary care was designed. The aim of the study was to analyze which variables predicted NHA and death among older people receiving domiciliary care.
Materials and Methods
This is a 3-year prospective study of community-dwelling older people receiving domiciliary care.
Sample
Nineteen municipalities of small, medium and large size in the eastern part of Norway recruited participants to the study. The inclusion criteria required recipients of domiciliary care aged ≥70 years who had a next of kin who saw them at least once a week. Participants were both established and new users of domiciliary care. Established users were drawn from the lists of the domiciliary care services and new users were included successively. These services could typically include ‘meals on wheels’, safety alarm, practical aid, daycare center, mental health care or in-home nursing.
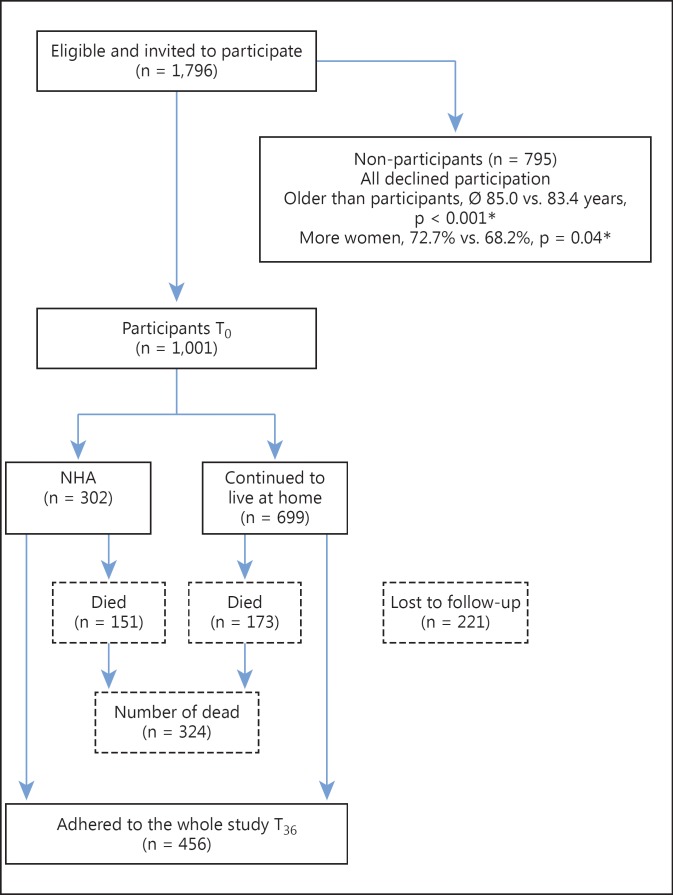
A total of 1,796 people were eligible for inclusion. Of these, 795 (44.3%) declined participation. Those who declined were more often women (72.7 vs. 68.2%, p = 0.04) and older (mean age 85.0 ± 6.2 vs. 83.4 ± 5.7 years, p < 0.001) than those who participated. The baseline sample comprised 1,001 participants (fig. 1).
Fig. 1.
Flowchart of participants. * χ2 test.
Data Collection
The baseline data were collected between August 2008 and December 2010 and the participants were followed up for 3 years or until they died, whichever was shorter. Dates of NHA and death were available for all participants in the study period. Health workers in the municipality services who participated in standardized training programs prior to the assessments collected the data.
The participants were assessed with a number of tools, including the Mini-Mental State Examination [23], in which the scores add up to give a sum score between 0 and 30 and lower scores indicate poorer cognitive functioning. In the Clock Drawing Test, a ‘perfect’ clock was given a score of 5, visuospatial errors from minor to severe were given a score from 4 to 1, and an inability to make any reasonable representation of a clock was given a 0 score [24]. The Informant Questionnaire on Cognitive Decline in the Elderly assesses observed change in cognition over the last decade reported by the next of kin [25]. On a scale ranging from 0 to 5, a score <3 indicates improvement, a score >3 indicates deterioration and a score of 3 indicates no change. The Clinical Dementia Rating scale (CDR) assesses the level of dementia [26]. The CDR includes six items and is scored by the assessor considering all available information. Based on an algorithm giving precedence to memory, a CDR score is generated with scores 0, 0.5, 1, 2 and 3, indicating no, possible, mild, moderate and severe dementia, respectively. NPSs were assessed with the Neuropsychiatric Inventory ten-item version (NPI-10) [27]. It collects information on symptoms in ten domains and the ratings are based on symptoms occurring over the previous month reported by the next of kin. The item scores are calculated by multiplying the frequency score by the severity score. The Physical Self-Maintenance Scale (PSMS) was used to evaluate functional impairment [28]. This scale evaluates six different areas with a total score ranging from 6 (best) to 30 (worst). Medical comorbidity was assessed using the General Medical Health Rating (GMHR) scale [29], which produced a score in one of four categories: very good, good, fair or poor.
Two physicians with wide experience in old age psychiatry independently provided diagnoses of dementia according to the ICD-10 [30] and of mild cognitive impairment according to the Winblad criteria using all available information [31]. Where they disagreed, a third clinical expert was consulted and consensus was reached.
Statistical Analyses
Data were analyzed using IBM SPSS statistics Windows version 22 (IBM Corp., Armonk, N.Y., USA).
In cases with <50% missing items on a scale, missing values were imputed. In cases with >50% missing items on a scale, the scale was kept as missing. Because of statistically significant differences on some demographic variables between those with and those without missing variables (GMHR), the same imputation algorithm was performed within each stratum, which was defined by significant demographic variables.
In order to identify sub-syndromes of the NPI, a principal component analysis was conducted. The results of this analysis showed that all items loaded into distinct factors apart from the NPI item agitation, which loaded on hyperactivity and psychosis (slightly stronger on the latter). Due to clinical experience, the item agitation was analyzed as part of the hyperactivity factor. This produced three different sub-syndromes of NPS: psychosis (delusions and hallucinations), affective (depression, anxiety and apathy) and hyperactivity (agitation, disinhibition, euphoria, irritability and aberrant motor behavior). This conforms to earlier research even if some studies suggested that apathy should be analyzed as an individual factor [7].
Bivariate logistic regression was used to estimate the odds ratio (OR) for NHA and death. To ensure the independence of variables included in the model, the correlation between the variables was controlled and none of the correlation coefficients were >0.5. Each explanatory variable was tested separately in a bivariate Cox proportional hazard regression model. Any association between a covariate and the outcomes (p < 0.2) was included in a multivariate Cox proportional hazard regression model.
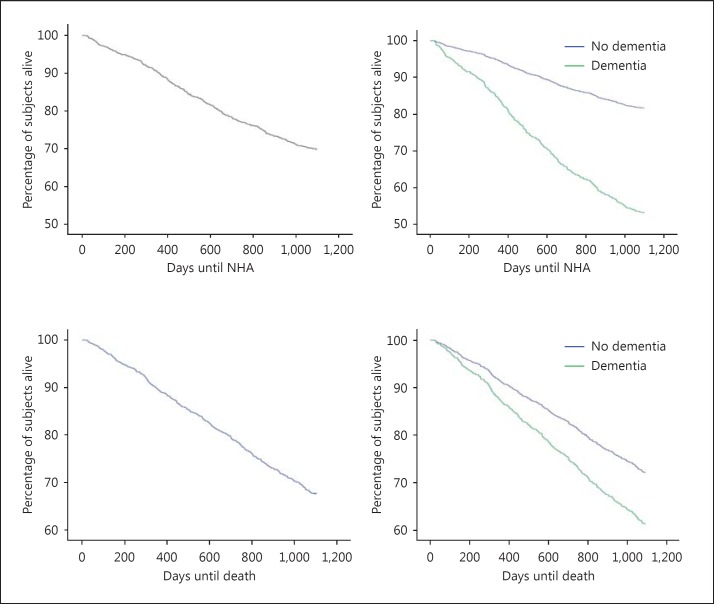
To ensure that the effects of the explanatory variables were independent of time from baseline, we performed two different tests. For the continuous explanatory variables (age, GMHR, PSMS, NPI and NPI sub-syndromes), we estimated the Cox model and saved the partial residuals. Then we tested the correlation between the partial residuals and the time variable. If these correlations were <0.2, the explanatory variable was judged to be independent of time. All the tested continuous variables were independent of time. For dichotomous variables (sex, living alone, dementia and any use of psychotropic drugs), we plotted the survival curves with a Kaplan-Meier plot for each variable split on the two possible scores (fig. 2) and checked for crossing lines. Variables with non-crossing lines were assumed to be independent of time [32]. This was the case for all dichotomous variables. All significance tests were two-tailed and the level of significance was set at <0.05.
Fig. 2.
Time until NHA and death of the whole sample and of participants with and without dementia.
Ethical Considerations
Prior to participating in the study, all participants and their next of kin were given written and oral information about the project and gave informed consent to participate in the study. The closest family proxy gave informed written consent on behalf of his/her next of kin for those who lacked the capacity to consent. The Regional Committee for Medical and Health Research Ethics; Committee A, Eastern Norway (S-08111b), the Norwegian Social Science Data Services (NSD) (07-2008SI) and the Directorate for Health and Social Affairs (08/2984) approved the project.
Results
The study included 1,001 participants. Table 1 presents the characteristics of the sample at baseline. Of the baseline sample, 30.7, 27.8 and 41.5% were diagnosed as having no cognitive impairment, minimal cognitive impairment and dementia, respectively. As shown in figure 1, 302 participants (30.2%) experienced NHA. Of these, 194 participants (64.2%) had dementia at baseline. During the study period, 324 participants (32.4%) died. Of these, 161 participants (49.7%) had dementia at baseline.
Table 1.
Participant characteristics regarding demographics and function levels at baseline (n = 1,001)
| Characteristics | n1 | Baseline scores |
|---|---|---|
| Age, years (mean ± SD) | 1,001 | 83.4 ± 5.7 |
| Women, n (%) | 1,001 | 682 (68.2) |
| Living alone, n (%) | 984 | 665 (66.5) |
| Good/very good physical health (GMHR), n (%) | 999 | 547 (54.7) |
| Dementia, n (%) | 1,001 | 415 (41.5) |
| PSMS severity (mean ± SD) | 996 | 9.2 ± 3.6 |
| Sum NPI (mean ± SD) | 958 | 5.06 ± 9.5 |
| NPI sub-syndrome hyperactivity (mean ± SD) | 966 | 1.66 ± 4.6 |
| NPI sub-syndrome psychosis (mean ± SD) | 975 | 0.53 ± 2.0 |
| NPI sub-syndrome affective (mean ± SD) | 972 | 2.88 ± 5.3 |
SD = Standard deviation.
Number of participants with complete data.
Participants with dementia had an almost four times higher crude risk of NHA (OR 3.88, 95% confidence interval [CI] 2.92-5.16) compared to participants without dementia. The crude risk of dying was higher among those who experienced NHA compared to those who continued to stay at home (OR 3.04, 95% CI 2.29-4.04). The mean time to NHA and death was 510.6 ± 289.5 and 553.7 ± 303.0 days, respectively.
Kaplan-Meier plots showed that the relationship between the survival functions of days until NHA and death were constant over time, thus meeting the proportional hazards assumption (fig. 2).
The independent variables associated with NHA and mortality risk (p ≤ 0.2) were all included in two Cox regression models. Tables 2 and 3 display the bivariate and the multivariate Cox regression results. In the multivariate analysis, the baseline variables associated with NHA were dementia, the NPI sub-syndrome psychosis, poorer functional impairment and age (table 2). Baseline variables associated with death were female sex, age, worse general medical health and greater functional impairment (table 3).
Table 2.
Cox proportional hazards model of the time until NHA, including all characteristics as potential influencing factors – bivariate and multivariate associations
| Characteristics | n1 | Bivariate analysis, HR (95% CI) | Multivariate analysis, HR (95% CI), n = 976 |
|---|---|---|---|
| Age | 1,001 | 1.07 (1.04 – 1.09) | 1.05 (1.03 – 1.07) |
| Female sex | 1,001 | 1.27 (1.00 – 1.61) | not significant |
| Living alone | 984 | 1.14 (0.90 – 1.44) | not included |
| GMHR | 999 | 1.36 (1.19 – 1.55) | not significant |
| Dementia | 1,001 | 3.12 (2.47 – 3.95) | 2.06 (1.58 – 2.68) |
| PSMS | 996 | 1.14 (1.11 – 1.17) | 1.09 (1.06 – 1.12) |
| Sum NPI | 958 | 1.03 (1.02 – 1.04) | not included |
| NPI sub-syndrome hyperactivity | 966 | 1.04 (1.02 – 1.06) | not significant |
| NPI sub-syndrome psychosis | 975 | 1.15 (1.12 – 1.20) | 1.11 (1.07 – 1.15) |
| NPI sub-syndrome affective | 972 | 1.05 (1.03 – 1.07) | not significant |
HR derived using Cox proportional hazards regression model with 3-year risk of NHA as the dependent variable.
Number of participants with complete data.
Table 3.
Cox proportional hazards model of the time until death, including all characteristics as potential influencing factors – bivariate and multivariate associations
| Characteristics | n1 | Bivariate analysis, HR (95% CI) | Multivariate analysis, HR (95% CI), n = 976 |
|---|---|---|---|
| Age | 1,001 | 1.04 (1.02 – 1.06) | 1.03 (1.01 – 1.05) |
| Female sex | 1,001 | 1.78 (1.43 – 2.22) | 1.66 (1.33 – 2.08) |
| Living alone | 984 | 1.37 (1.10 – 1.72) | not significant |
| GMHR | 999 | 1.56 (1.38 – 1.77) | 1.35 (1.18 – 1.55) |
| Dementia | 1,001 | 1.50 (1.21 – 1.87) | not significant |
| PSMS | 996 | 1.12 (1.09 – 1.15) | 1.08 (1.05 – 1.11) |
| Sum NPI | 995 | 1.01 (1.00 – 1.02) | not included |
| NPI sub-syndrome hyperactivity | 966 | 1.02 (1.00 – 1.04) | not significant |
| NPI sub-syndrome psychosis | 975 | 1.07 (1.02 – 1.08) | not significant |
| NPI sub-syndrome affective | 972 | 1.02 (1.00 – 1.04) | not significant |
HR derived using Cox proportional hazards regression model with 3-year risk of death as the dependent variable.
Number of participants with complete data.
Discussion
This study aimed to identify variables associated with NHA and mortality risk among older people receiving domiciliary care. Functional impairment and age were predictors for both NHA and death. Dementia and the NPI sub-syndrome psychosis were predictors for NHA but not death, while female sex and worse general medical health were predictors for death but not for NHA. Having dementia more than doubled the risk of NHA within the study period. These findings confirm earlier studies reporting that dementia, NPS and activities of daily living function were important predictors for NHA [1,2,4,6,11,13,14].
A Swedish population-based study showed that dementia, functional impairment and hip fracture predicted NHA among home-dwelling older people >75 years of age [2]. The present study confirms that dementia, functional impairment and old age are predictors for NHA.
An American population-based study reported that clinically significant delusion (hazard ratio [HR] 5.74), agitation (HR 4.70), and depression (HR 3.06) were associated with a higher risk of NHA [17]. The present study found that the NPI sub-syndrome psychosis increased the risk of NHA (HR 1.11), whereas the NPI sub-syndromes hyperactivity and affective did not increase the risk of NHA. Knowledge about delusions and hallucinations and how to meet and cope with such symptoms in the family seems to be particularly important if NHA is to be postponed or avoided.
In the present study, functional impairment was almost an equally strong predictor for NHA as a predictor for death (HR 1.08 vs. 1.09). For each decade of aging, the risk of NHA increased by 50% while the risk of death increased by 30%. According to Gerstorf et al. [33], depression and hallucinations (HR 1.56 HR 2.59, respectively) were associated with a higher mortality risk. The population-based study by Eaker et al. [11] found that people with dementia are at greater risk of NHA than of dying compared to people without dementia. Dementia is reported to increase the risk of death, independent of comorbid conditions [11]. Such reports are contrary to the findings of the present study, possibly a result of the fact that the other studies were population-based, while this study had a selected sample of older people.
The type of dementia, degree of functional impairment, caregiver's age and perceived burden are reported to be predictors for NHA [4,17], while behavioral disturbance, depressive mood and functional impairment are associated with caregiver burden [4,12,19]. Support to the caregiver and education on how to meet and cope with behavioral disturbance, depressive mood and sub-syndrome psychosis will probably enable the family to adapt to late life changes better and make everyday life more manageable. Domiciliary care needs to address the consequences of dementia and relieve the burden of the caregiver in order to postpone NHA. Designing interventions to target and treat NPS and decrease the burden of NPS on the caregiver can be important avenues to decreasing negative clinical outcomes.
This study has considerable strengths. The data come from a clinical sample, generating a representative sample of community-dwelling people ≥70 years who receive some kind of domiciliary care. Functional impairment and need for assistance in this sample highly correlate with nationwide data [34], even if the attrition of invited participants was rather large. The participants were assessed using standardized instruments, leading to a precise measurement of many variables thought to be associated with NHA. The participants constitute a vulnerable group compared to older people who do not receive domiciliary care, which provides important information about predictors for NHA and death.
The limitations of this study include the fact that numerous assessors with different experience in using assessment tools were engaged in order to assess the participants. However, all the assessors completed comprehensive and standardized training prior to the data collection, and all of the assessors were familiar with observing and cooperating with older people and their families in their homes. It must be acknowledged that this study was carried out in Norway in the context of a public and universal health care system, which also includes coverage for long-term care institutions. Thus, the generalizability to other health care systems is not evident.
Conclusion
The present study confirms that dementia and psychosis are predictors for NHA. Functional impairment and age predict NHA and death, whereas general medical health and female sex predict death.
Individual characteristics that predict NHA and death outline a need in domiciliary care to address how these individual characteristics affect the psychosocial environment of older people. Supportive and tailored domiciliary services, which involve the caregiver and other family members, might relieve caregiver burden, increase quality of life and postpone NHA. Hence, psychosocial interventions, education of the patient-caregiver dyad and tailored daycare programs might be relevant avenues to implement.
Disclosure Statement
All authors declare no conflict of interest.
Acknowledgements
We are grateful to the participating families and staff in the domiciliary care services for their help in data collection. The project was made possible by funding from the Norwegian Directorate of Health and by grant 187980 from the Research Council of Norway. Coordinator Lisbeth D. Høgset and statistician Jurate Salyte-Benth also contributed assistance and counseling that improved the study and the content of this paper.
References
- 1.Luck T, Luppa M, Weber S, Matschinger H, Glaesmer H, Konig HH, Angermeyer MC, Riedel-Heller SG. Time until institutionalization in incident dementia cases – results of the Leipzig Longitudinal Study of the Aged (LEILA 75+) Neuroepidemiology. 2008;31:100–108. doi: 10.1159/000146251. [DOI] [PubMed] [Google Scholar]
- 2.Agüero-Torres H, von Strauss E, Viitanen M, Winblad B, Fratiglioni L. Institutionalization in the elderly: the role of chronic diseases and dementia. Cross-sectional and longitudinal data from a population-based study. J Clin Epidemiol. 2001;54:795–801. doi: 10.1016/s0895-4356(00)00371-1. [DOI] [PubMed] [Google Scholar]
- 3.Luppa M, Luck T, Brähler E, König HH, Riedel-Heller SG. Prediction of institutionalisation in dementia. A systematic review. Dement Geriatr Cogn Disord. 2008;26:65–78. doi: 10.1159/000144027. [DOI] [PubMed] [Google Scholar]
- 4.Hebert R, Dubois MF, Wolfson C, Chambers L, Cohen C. Factors associated with long-term institutionalization of older people with dementia: data from the Canadian Study of Health and Aging. J Gerontol A Biol Sci Med Sci. 2001;56:M693–M699. doi: 10.1093/gerona/56.11.m693. [DOI] [PubMed] [Google Scholar]
- 5.Dramé M, Lang PO, Jolly D, Narbey D, Mahmoudi R, Lanièce I, Somme D, Gauvain JB, Heitz D, Voisin T, de Wazières B, Gonthier R, Ankri J, Saint-Jean O, Jeandel C, Couturier P, Blanchard F, Novella JL. Nursing home admission in elderly subjects with dementia: predictive factors and future challenges. J Am Med Dir Assoc. 2012;13:83.e17–83.e20. doi: 10.1016/j.jamda.2011.03.002. [DOI] [PubMed] [Google Scholar]
- 6.Afram B, Stephan A, Verbeek H, Bleijlevens MH, Suhonen R, Sutcliffe C, Raamat K, Cabrera E, Soto ME, Hallberg IR, Meyer G, Hamers JP, RightTimePlaceCare Consortium Reasons for institutionalization of people with dementia: informal caregiver reports from 8 European countries. J Am Med Dir Assoc. 2014;15:108–116. doi: 10.1016/j.jamda.2013.09.012. [DOI] [PubMed] [Google Scholar]
- 7.Aalten P, Verhey FR, Boziki M, Bullock R, Byrne EJ, Camus V, Caputo M, Collins D, De Deyn PP, Elina K, Frisoni G, Girtler N, Holmes C, Hurt C, Marriott A, Mecocci P, Nobili F, Ousset PJ, Reynish E, Salmon E, Tsolaki M, Vellas B, Robert PH. Neuropsychiatric syndromes in dementia. Results from the European Alzheimer Disease Consortium: part I. Dement Geriatr Cogn Disord. 2007;24:457–463. doi: 10.1159/000110738. [DOI] [PubMed] [Google Scholar]
- 8.Craig D, Mirakhur A, Hart DJ, McIlroy SP, Passmore AP. A cross-sectional study of neuropsychiatric symptoms in 435 patients with Alzheimer's disease. Am J Geriatr Psychiatry. 2005;13:460–468. doi: 10.1176/appi.ajgp.13.6.460. [DOI] [PubMed] [Google Scholar]
- 9.Okura T, Plassman BL, Steffens DC, Llewellyn DJ, Potter GG, Langa KM. Prevalence of neuropsychiatric symptoms and their association with functional limitations in older adults in the United States: the aging, demographics, and memory study. J Am Geriatr Soc. 2010;58:330–337. doi: 10.1111/j.1532-5415.2009.02680.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Fauth EB, Schwartz S, Tschanz JT, Ostbye T, Corcoran C, Norton MC. Baseline disability in activities of daily living predicts dementia risk even after controlling for baseline global cognitive ability and depressive symptoms. Int J Geriatr Psychiatry. 2013;28:597–606. doi: 10.1002/gps.3865. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Eaker ED, Vierkant RA, Mickel SF. Predictors of nursing home admission and/or death in incident Alzheimer's disease and other dementia cases compared to controls: a population-based study. J Clin Epidemiol. 2002;55:462–468. doi: 10.1016/s0895-4356(01)00498-x. [DOI] [PubMed] [Google Scholar]
- 12.Gaugler JE, Yu F, Krichbaum K, Wyman JF. Predictors of nursing home admission for persons with dementia. Med Care. 2009;47:191–198. doi: 10.1097/MLR.0b013e31818457ce. [DOI] [PubMed] [Google Scholar]
- 13.Bharucha AJ, Pandav R, Shen CY, Dodge HH, Ganguli M. Predictors of nursing facility admission: a 12-year epidemiological study in the United States. J Am Geriatr Soc. 2004;52:434–439. doi: 10.1111/j.1532-5415.2004.52118.x. [DOI] [PubMed] [Google Scholar]
- 14.St John PD, Montgomery PR, Kristjansson B, McDowell I. Cognitive scores, even within the normal range, predict death and institutionalization. Age Ageing. 2002;31:373–378. doi: 10.1093/ageing/31.5.373. [DOI] [PubMed] [Google Scholar]
- 15.Lavretsky H, Zheng L, Weiner MW, Mungas D, Reed B, Kramer JH, Jagust W, Chui H, Mack WJ. Association of depressed mood and mortality in older adults with and without cognitive impairment in a prospective naturalistic study. Am J Psychiatry. 2010;167:589–597. doi: 10.1176/appi.ajp.2009.09020280. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Dorenlot P, Harboun M, Bige V, Henrard JC, Ankri J. Major depression as a risk factor for early institutionalization of dementia patients living in the community. Int J Geriatr Psychiatry. 2005;20:471–478. doi: 10.1002/gps.1238. [DOI] [PubMed] [Google Scholar]
- 17.Okura T, Plassman BL, Steffens DC, Llewellyn DJ, Potter GG, Langa KM. Neuropsychiatric symptoms and the risk of institutionalization and death: the Aging, Demographics, and Memory Study. J Am Geriatr Soc. 2011;59:473–481. doi: 10.1111/j.1532-5415.2011.03314.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Benoit M, Robert PH, Staccini P, Brocker P, Guerin O, Lechowski L, Vellas B, REAL.FR Group One-year longitudinal evaluation of neuropsychiatric symptoms in Alzheimer's disease. The REAL.FR Study. J Nutr Health Aging. 2005;9:95–99. [PubMed] [Google Scholar]
- 19.Banerjee S, Murray J, Foley B, Atkins L, Schneider J, Mann A. Predictors of institutionalisation in people with dementia. J Neurol Neurosurg Psychiatry. 2003;74:1315–1316. doi: 10.1136/jnnp.74.9.1315. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Gaugler JE, Kane RL, Kane RA, Clay T, Newcomer R. Caregiving and institutionalization of cognitively impaired older people: utilizing dynamic predictors of change. Gerontologist. 2003;43:219–229. doi: 10.1093/geront/43.2.219. [DOI] [PubMed] [Google Scholar]
- 21.Yaffe K, Fox P, Newcomer R, Sands L, Lindquist K, Dane K, Covinsky KE. Patient and caregiver characteristics and nursing home placement in patients with dementia. JAMA. 2002;287:2090–2097. doi: 10.1001/jama.287.16.2090. [DOI] [PubMed] [Google Scholar]
- 22.Brevik I, Nygård L. Mønstre og mangel på mønster i innretningen av de kommunale omsorgstjenestene (in Norwegian). Oslo, NIBR, 2013, Contract No 2013, p 104.
- 23.Folstein MF, Folstein SE, McHugh PR. ‘Mini-mental state’. A practical method for grading the cognitive state of patients for the clinician. J Psychiatr Res. 1975;12:189–198. doi: 10.1016/0022-3956(75)90026-6. [DOI] [PubMed] [Google Scholar]
- 24.Shulman KI. Clock-drawing: is it the ideal cognitive screening test? Int J Geriatr Psychiatry. 2000;15:548–561. doi: 10.1002/1099-1166(200006)15:6<548::aid-gps242>3.0.co;2-u. [DOI] [PubMed] [Google Scholar]
- 25.Jorm AF. The Informant Questionnaire on Cognitive Decline in the Elderly (IQCODE): a review. Int Psychogeriatr. 2004;16:275–293. doi: 10.1017/s1041610204000390. [DOI] [PubMed] [Google Scholar]
- 26.Hughes CP, Berg L, Danziger WL, Coben LA, Martin RL. A new clinical scale for the staging of dementia. Br J Psychiatry. 1982;140:566–572. doi: 10.1192/bjp.140.6.566. [DOI] [PubMed] [Google Scholar]
- 27.Cummings JL, Mega M, Gray K, Rosenberg-Thompson S, Carusi DA, Gornbein J. The Neuropsychiatric Inventory: comprehensive assessment of psychopathology in dementia. Neurology. 1994;44:2308–2314. doi: 10.1212/wnl.44.12.2308. [DOI] [PubMed] [Google Scholar]
- 28.Lawton MP, Brody EM. Assessment of older people: self-maintaining and instrumental activities of daily living. Gerontologist. 1969;9:179–186. [PubMed] [Google Scholar]
- 29.Lyketsos CG, Galik E, Steele C, Steinberg M, Rosenblatt A, Warren A, Sheppard JM, Baker A, Brandt J. The General Medical Health Rating: a bedside global rating of medical comorbidity in patients with dementia. J Am Geriatr Soc. 1999;47:487–491. doi: 10.1111/j.1532-5415.1999.tb07245.x. [DOI] [PubMed] [Google Scholar]
- 30.World Health Organization International Statistical Classification of Diseases and Related Health Problems 10th Revision. World Health Organisation, 2013 (accessed April 10, 2013]. Available from http://apps.who.int/classifications/icd10/browse/2010/en.
- 31.Winblad B, Palmer K, Kivipelto M, Jelic V, Fratiglioni L, Wahlund LO, Nordberg A, Backman L, Albert M, Almkvist O, Arai H, Basun H, Blennow K, de Leon M, DeCarli C, Erkinjuntti T, Giacobini E, Graff C, Hardy J, Jack C, Jorm A, Ritchie K, van Duijn C, Visser P, Petersen RC. Mild cognitive impairment – beyond controversies, towards a consensus: report of the International Working Group on Mild Cognitive Impairment. J Intern Med. 2004;256:240–246. doi: 10.1111/j.1365-2796.2004.01380.x. [DOI] [PubMed] [Google Scholar]
- 32.Therneau TM, Grambsch PM. Modeling survival data: extending the Cox model. New York: Springer; 2000. [Google Scholar]
- 33.Gerstorf D, Ram N, Lindenberger U, Smith J. Age and time-to-death trajectories of change in indicators of cognitive, sensory, physical, health, social, and self-related functions. Dev Psychol. 2013;49:1805–1821. doi: 10.1037/a0031340. [DOI] [PubMed] [Google Scholar]
- 34.Selbaek G, Høgset LD. IPLOS and assessment of the need for services among home-dwelling elderly with cognitive impairment (in Norwegian). Sykehuset Innlandet HF, AFS, 2010. Unnumbered report.