Abstract
Smartphones are now ubiquitous and can be harnessed to offer psychiatry a wealth of real-time data regarding patient behavior, self-reported symptoms, and even physiology. The data collected from smartphones meet the three criteria of big data: velocity, volume, and variety. Although these data have tremendous potential, transforming them into clinically valid and useful information requires using new tools and methods as a part of assessment in psychiatry. In this paper, we introduce and explore numerous analytical methods and tools from the computational and statistical sciences that appear readily applicable to psychiatric data collected using smartphones. By matching smartphone data with appropriate statistical methods, psychiatry can better realize the potential of mobile mental health and empower both patients and providers with novel clinical tools.
Keywords: Smartphones, Mobile, Big data, Technology, Statistical methods
Introduction
Progress in medical science has always been driven by highquality data. Although patient retrospective recollection is a valuable and commonly used source of information in psychiatry, data accumulated over time has been shown to have higher accuracy across numerous psychiatric diseases [1]. Recently, mobile monitoring and mobile interventions, such as smartphone applications, are beginning to offer psychiatry a nearly constant longitudinal stream of patient data. Data collected from smartphone applications gives investigators the opportunity to not only help assess cross-sectional symptoms but also inform the patient and the clinician how symptoms vary in time, space, and across social contexts. However, in order to realize the potential of such new data, psychiatry has much to gain from matching these new complex data streams with commensurate analytical tools and statistical methods from biostatistics, data science, and the computational sciences more broadly.
Current research on smartphone applications for monitoring psychiatric diseases has shown feasibility across diverse ranges of disorders including depression [2], bipolar disorder [3], schizophrenia [4••], anxiety disorders [5], and substance abuse disorders [6••]. The numerous sensors embedded in smartphones offer a wealth of data relevant to psychiatric illnesses [7] such as GPS to monitor spatial location, accelerometers to record movement and gross motor activity, call and messaging logs to document social engagement with others, and voice and tone records to estimate mood. Smartphone sensor data is only expected to increase in quality and variety in the next few years [8]. Recent research suggests that mental health patients’ rates of smartphone ownership is near the national average and that they have a strong interest in using their phones to monitor mental health [9, 10••]. Therefore, the question of how psychiatry might be able to best leverage the full potential of this data is now timely.
The limitations of analytical tools and methods currently applied to mobile mental health may be an impediment to utilizing its full potential. A recent systematic review of smartphone applications for mental health, featuring studies with pre- to posttest design or comparison to a control group, noted that no firm conclusions could be drawn because of a lack of evidence [11]. There is increasing recognition that new methods beyond pre- to posttest design are needed, and even randomized controlled trials may not be appropriate methodologies to study the efficacy of smartphone interventions [12]. It is equally important to take a step back and consider what data is collected, what data is missed, and how the collected data are analyzed. As an example, many smartphone applications for mental health function as journals for recording patient symptoms [13, 2]. But smartphones are able to collect far more complex data, sometimes referred to as “big data.” Although there is no universally accepted definition for what constitutes big data, we adopt the commonly used “3V” definition [14]: the data is of high velocity (arrives non-stop), of high volume (there is plenty of it), and of high variety (combination of different types of data).
Simple survey apps available on the commercial market-places already operate in the realm of big data as surveys may arrive frequently, from thousands of subjects, and may contain a combination of data beyond survey responses alone, such as time of survey completion and time to answer each survey question (e.g., how long the subject spent answering a question regarding suicidality). However, utilizing such data requires developing new statistical tools in order to transform these data streams into clinically valid and meaningful measures. The challenge for psychiatry thus lies not in the recognition of the importance of big data [15], or ability to collect it, but how to analyze these data in meaningful ways. While many areas in medicine stand to gain from these types of data, it appears that their payoff could be especially large in psychiatry. The combination of big data and appropriate data analytic tools therefore not only enables psychiatry to draw from these new developments but also places the field at the forefront of this nascent and rapidly developing field.
Data Velocity: a Focus on Real-Time Data
Patient information and data used by clinical psychiatrists today are often gathered during office visits. Once the patient walks out of the office, the psychiatrist has likely gathered the majority of the information she will use. But smartphone data can be collected and analyzed non-stop, at all times of the day, regardless of whether the patient is in the office or not. The clinical potential of such high-velocity data can be seen in suicide, where there is increasing appreciation of the temporal dynamics of patient risk [16]. The ability to monitor high-risk patients using high-frequency measurements, and the potential to detect certain behavioral signatures and use them as markers of elevated risk, could be clinically very meaningful. While most current studies of mobile devices employ a small and limited number of data collection waves per day, smartphones have the capability to provide essentially continuous data streams on patient behavior. However, new methods for understanding and utilizing this high-velocity data are necessary to realize its potential for patient care.
Working with high-velocity data is actually not new in psychiatry, and researchers have already embraced methodologies to tackle these challenges in fMRI studies of PTSD patients. These recent studies [17, 18] utilized an analytical method called a hidden Markov model [19]. This modeling framework assumes that subjects’ actual mental state at any given time can be described as one of a limited number of discrete states in a model, with states transitioning to other states over time and each state giving rise to its own distinct set of behaviors. Psychiatrists already work with these mental states on a daily basis. While a patient may not be able to correctly recognize their depressed state, psychiatrists diagnose and deduce such information from interaction and examination with patients. Likewise, the hidden Markov models assume that state itself is latent, or hidden, and cannot be directly observed. However, just like a psychiatrist can still characterize the state of a bipolar patient (e.g., manic vs. depressed) even though the patient may never use such labels, this model also can infer a patient’s mental state based on observed data. A recent study used instantaneous information from smartphones to rapidly recognize distinct mental states in patients with bipolar disorder [20]. The hidden Markov model can use such state information to provide clinically useful predictions of patient moods and behaviors, and was designed to predict transitions between different internal states. A schematic of this type of model is shown in Fig. 1. Using data gathered on smartphones to estimate the patient’s current state and the hidden Markov model to predict future states, psychiatry may soon be able to better predict manic episodes or schizophrenic relapses and enable more timely interventions and treatments. Utilizing this analytical method, the constant stream of a bewildering amount of patient smartphone data can be turned into a clinically informative monitoring and diagnostic tool.
Fig. 1.
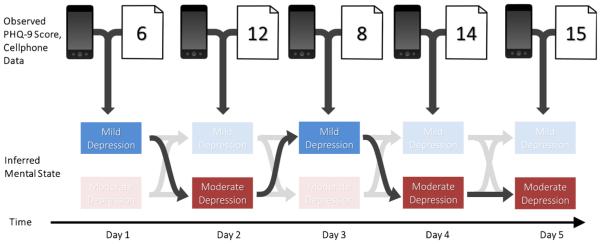
A schematic combining a hidden Markov model with smartphone data in a bipolar patient. In this example, the patient occupies one of a limited number of states at any given time, and the observed scores are generated from a distribution that is distinct to that given state. For example, one of the states could correspond to the patient being depressed and neither leaving the house, calling friends, nor being active, whereas another state could correspond to the patient being manic, with the patient very active and calling many friends. Here, for simplicity, we use only two states: “mild depression” and “moderate depression.” Although the states are not observed directly in this framework, hidden Markov models can learn the transition patterns and frequencies between states from observed data
A whole family of statistical learning methods has been designed for explanatory interpretation and robust prediction of complex longitudinal data, with hidden Markov models serving here as one of many possible examples. Some of these methods have traditionally been referred to as either data mining or machine learning methods, but the best under any banner are increasingly culled and curated for non-specialist use, including provision of software to implement them [21, 22••]. These methods appear to be ideal for analyzing and modeling real-time patient data obtained from smartphones. Consequently, expanding and tuning these methods to the specific needs of mental health appears to be a very promising future direction for research. This transformation of real-time data into accessible models, combined with clinical experience and judgment, offers psychiatry the opportunity to utilize smartphone data as a practical clinical tool.
Data Volume: Focus on Active Data
Psychiatrists are already used to working with high volumes of data when conducting clinical interviews and chart reviews, and seek collateral. Smartphones offer psychiatrists a high volume of new types of data: the term “active data” refers to data whose generation requires a patient’s active involvement, such as taking surveys or contributing audio samples, whereas “passive data” refers to data that are generated without the patient’s involvement, such as GPS and accelerometer data or communication logs from voice calls and text messages, 24 h per day. In the mobile phone sensing literature in computer science, these two modes of data collection are known as participatory sensing [23] and opportunistic sensing [24] respectively.
There is already an evolving literature on the utility of active data in the form of conducting clinical surveys on smartphones. While such data is often assumed to be similar to more traditional paper/pencil-based surveys collected in the clinical setting, implementing surveys on a smartphone offers many exciting opportunities for psychiatry. For example, most surveys consist of multiple test items, each designed to detect a possible manifestation of psychiatric illness. However, traditional diagnosis itself is performed based on a single composite measure of that test, such as a total score, which implicitly assumes that all survey items have both the same weight and meaning. Realistically, however, psychiatric evaluation items themselves very likely differ in what they measure and how well they measure it. A smartphone-based survey can leverage item response theory (IRT) [25] to look beyond survey totals and instead consider the ability of each question to discriminate mental features for individual patients. Psychiatrists regularly do this, for example, when administering the Patient Health Questionnaire 9-item (PHQ-9) and weighing question 9, regarding suicidality, higher than other questions when conducting a safety assessment. Furthermore, patients’ answer ratings may vary based on their current context, cultural background, individual characteristics, engagement in treatment, and survey fatigue. IRT offers a methodology to study subject outcomes over time as a function of question items as well as subject covariates [26]. The item response theory has been used in psychiatry to study the effect of individual survey questions for different population groups [27], or their effect over time [28], but not both, which is easily accomplished with smartphones. This lack of variety-rich studies means that potentially useful insights about patients are going to waste, and survey questions are not as formally validated as they could be. As smartphone technology allows for more frequent and personalized survey assessments, psychiatrists will have the opportunity to interpret their surveys and understand their patients more effectively.
Data Variety: Focus on Passive Data
Finally, the variety of smartphone data offers psychiatry perhaps its largest opportunity as well as its greatest challenge. The availability of data on patient location, activity level, and social engagement provided by smartphones, among other streams of data, is unparalleled. While there is little literature on the use of passive smartphone data in psychiatry, there is rapidly evolving interest in this area as well as some promising preliminary results [29]. Discerning clinically relevant or meaningful information from such a disparate set of data again requires appropriate statistical methods.
One of the first goals toward this end is to categorize complex smartphone data into an interpretable social or environmental context. For example, the class of statistical learning methods known as decision trees offers a simple yet high-performance approach for dividing data into classes by using a series of unambiguous and interpretable rules [30]. An example of decision trees is shown in Fig. 2. Researchers have successfully used decision trees on smartphone data to discover whether people were walking, standing, or driving [31]. Context classification algorithms like decision trees belong to a family of well-validated tools used to predict outcomes from complex data [22], including mental health [22]. While using smartphones to learn such contexts would be immensely useful, it is still a challenge in practice [24].
Fig. 2.
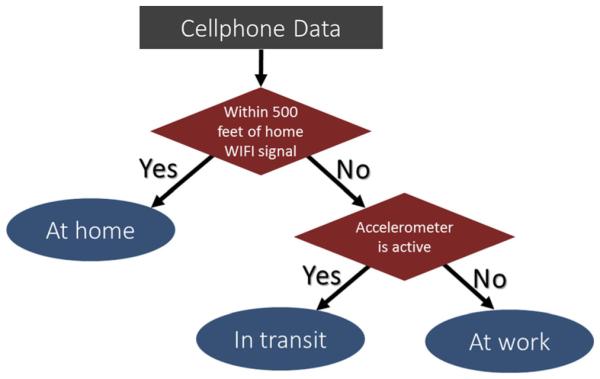
A diagram of a simple decision tree. Whereas workflows are common in workplaces made by conscientious decision-makers, decision trees are developed automatically by statistical learning algorithms that divide data efficiently into meaningful contexts. In this diagram, cell phone data is divided in order to discover the user’s location. Applying this kind of method to uncover valid clinical information is a standing challenge
Pattern recognition is commonly used for some highly complex psychiatric data like neuroimaging [32, 33], so its applicability to the real-time, real-world lifestyle information gathered by smartphones is a tantalizing hypothesis. For example, one recent study employed decision trees to smartphone data to extract context in the service of understanding depression [34], with mixed results. Some studies have sought to identify manic episodes in bipolar disorder patients by utilizing a variety of smartphone sensors [2, 20], but clinical results remain elusive. It may be possible to unify information from different clinicians and seemingly incommensurable surveys to make sharper inference about patients’ well-being [35]. For example, one study compared the sensitivity and specificity of smartphone assessment to classical inperson clinician assessments [13]. However, while we know the clinical phenotype of mental illnesses, smartphone data allow for personalized assessment for which there are perhaps no gold standards to compare them to. The digital signatures of mental illness that smartphones can detect are likely dynamic and have variable targets, and new real-time signatures will be discovered only by creating new methods for this data. Despite these challenges, learning the behavioral context from smartphone data has seen encouraging success, and it is likely to improve with larger studies and advances in statistical methodology designed for psychiatric use [8, 36].
Another variety of data, always important to psychiatry but difficult to collect prior to smartphones and other digital technologies, is information on social engagement. In many ways, psychiatric diseases may be considered social diseases, but there is a paucity of data on the role of social interactions and social networks in psychiatry. One recent study utilized 32 years in three waves of survey data from the Framingham Heart Study to explore how social networks can predict depressive behavior, postulating that depression may spread from one person to another [37]. However, this study did not investigate social-network-based markers of depression. Social networks have been used in the past few years to study the relationship between social contagion and a range of outcomes such as obesity, smoking, and happiness [38]. Although isolating causal mechanisms in these types of observational studies is challenging [39], it has been demonstrated that some of the results on social contagion are robust to certain types of confounding [40]. Social networks can also improve understanding of mental illness in controlled prospective settings such as the likelihood of suicide in prisoners [39]. Furthermore, social behavior is owed to brain behavior, and some neuroscientists have argued that studying social disorders requires shifting research focus from brain structures to features of neural networks [40]. Thus, in a range of circumstances, data on social engagement can be included in clinical assessment to improve causal understanding and prediction of mental attitudes and behavior.
Transforming data such as number of conversation partners, time spent associating with a given friend, or reciprocity of call patterns into clinically useful metrics requires use of models and tools from network science in physics and social network analysis in statistics. Among many other applications, networks have been embraced to explore genetics [41], structure of neural networks [42, 43], and properties of social networks mediated by cell phone calls [44••, 45, 46]. Similar methods can now be used to explore the social network data generated by smartphones [47••]. Early research efforts incorporating social networks have already resulted in important findings for suicide. One group demonstrated the role of networks in understanding the diffusive nature of suicidal ideation in a friendship network of adolescents after a peer suicide attempt [48]. With the influx of social data from smartphones increasing, the importance of network tools cannot be overstated.
Case Study
To illustrate how smartphone-based surveys coupled with appropriate statistical tools can be turned into clinically meaningful information, we present a case study from our recent work. Thirteen patients with major depressive disorder used a simple smartphone application to answer three randomly sampled questions from the PHQ-9 survey, three times per day, for the duration of 1 month [49]. The data encompassed a total of 90 such “micro-surveys” with three questions in each for every patient, resulting in potentially 270 measurements per patient in 1 month. The data arrived three times daily, which is overwhelming when compared to a traditional in-office PHQ-9 survey that might be administered perhaps monthly at clinical appointments and often only every 3 months. In this case, we did a statistical adjustment for psychometric surveys that were only partially filled in and, from the information available, obtained daily estimated PHQ-9 scores for each patient. In the same way as one might monitor daily weight using a weight scale or daily body temperature using a thermometer, we were able to monitor the patients’ overall psychiatric health on a day-by-day basis. Furthermore, comparing patient’s current responses to previous responses, we could formally estimate how unexpected any given response was. Investigation of these types of score departures could help a psychiatrist make more informed clinical decisions in the near future.
Mobile mood monitoring offers clinicians with real-time data on a patient’s depression but can also be used to predict worsening or improvement of the condition. If related subject information is available at the time the survey is gathered, it can be used to infer what real-time context or time of day is associated with score changes. An example of daily scores over time is shown in Fig. 3. The dark blue curve shows the daily PHQ-9 score adjusting for missingness by imputing likely scores from previous responses. Given previous responses, it is possible to estimate how extreme a subject’s daily score is when compared to previous responses, information that in the future could be used to construct a person-specific risk score or risk profile. The light blue curve and colored bands show each day’s expected PHQ-9 score, as well as confidence bands with a significance rate that can be pre- specified by the clinician. This approach has substantial clinical potential, as significant scores could one day be used to prompt timely responses, such as trigger computerized therapy sessions, send notification to the patient’s mental health team, or even activate the emergency medical system such as calling 911.
Fig. 3.
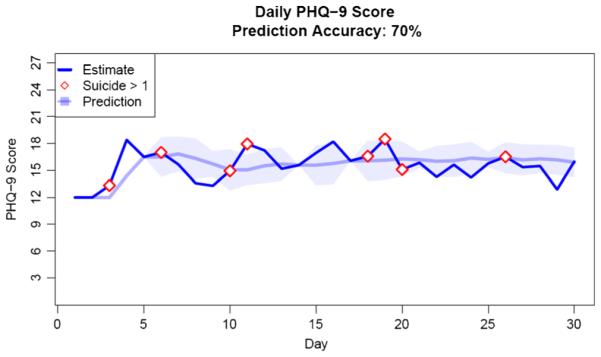
An example of estimated daily PHQ-9 scores over 1 month as reported in [52]. The dark blue curve shows estimates adjusting for missingness owing to the study design as well as patient unresponsiveness. The light blue curve and confidence bands characterize the predicted score and bounds of scores of what would be more extreme than predicted by previous scores. This significance rate can be set to a meaningful threshold by the clinician
Conclusion
Psychiatric diseases are some of the most complex medical conditions. Smartphones now offer the technology to gather rich behavioral data on patients and deliver information about how symptoms vary in time, space, and across social dimensions. Unlike prior sensor-based research that required expensive customized hardware, smartphones are now ubiquitous and immediately usable devices that patients want to use to improve their mental health. To maximize clinical impact, it is imperative that this complex data be matched with appropriate analytical and modeling methods in order for the field to realize the full potential of smartphones in mental health. Real-time data promises rapid assessment and safety monitoring, although its high volume requires specific analytical tools to realize its potential. Active data in the form of surveys can bring clinical assessments outside of the healthcare setting into real life as lived and experienced by patients, but will require the use of new tools to maximize its utility. Finally, passive data from smartphone users’ sensors and activity logs offer a tremendous variety of information that opens new paradigms for understanding mental illness, but will similarly require adaption of existing methods. Just as neurobiological data complements psychiatry but does not replace clinical expertise, smartphone data can better inform clinical decisions in psychiatry. Real-time, active, passive, social, and behavioral data from smartphones therefore augments existing tools, yet is not a substitute for clinical evaluation. While data privacy and security issues still remain important barriers [50], through a partnership with smartphone technology and the data sciences, psychiatry has the potential to embark on a new journey of transformational research, discovery, and, ultimately, patient health.
Acknowledgments
PS is supported by NIH-95T32ES0071429-32 (PI Coull) and JPO by NIH-1DP2MH1039099-01 (PI Onnela).
Footnotes
Compliance with Ethics Guidelines
Conflict of Interest John Torous, Patrick Staples, and Jukka-Pekka Onnela declare that they have no conflict of interest.
Human and Animal Rights and Informed Consent This article does not contain any studies with human or animal subjects performed by any of the authors.
References
Papers of particular interest, published recently, have been highlighted as:
•• Of major importance
- 1.Takayanagi Y, Spira AP, Roth KB, Gallo JJ, Eaton WW, Mojtabai R. Accuracy of reports of lifetime mental and physical disorders: results from the Baltimore epidemiological catchment area study. JAMA Psychiatr. 2014;71(3):273–80. doi: 10.1001/jamapsychiatry.2013.3579. http://eutils.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&id=24402003&retmode=ref&cmd=prlinks. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.BinDhim NF, Shaman AM, Trevena L, Basyouni MH, Pont LG, Alhawassi TM. Depression screening via a smartphone app: crosscountry user characteristics and feasibility. J Am Med Inform Assoc. 2015;22:29–34. doi: 10.1136/amiajnl-2014-002840. doi:10.1136/amiajnl-2014-002840. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Faurholt-Jepsen M, Frost M, Vinberg M, Christensen EM, Bardram JE, Kessing LV. Smartphone data as objective measures of bipolar disorder symptoms. Psychiatry Res. 2014;217:124–7. doi: 10.1016/j.psychres.2014.03.009. http://eutils.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&id=24679993&retmode=ref&cmd=prlinks. [DOI] [PubMed] [Google Scholar]
- 4••.Ben-Zeev D, Brenner CJ, Begale M, Duffecy J, Mohr DC, Mueser KT. Feasibility, acceptability, and preliminary efficacy of a smartphone intervention for schizophrenia. Schizophr Bull. 2014:1–10. doi: 10.1093/schbul/sbu033. doi:10.1093/schbul/sbu033. This is a significant paper as it demonstrates high levels of patient engagement with a smartphone apps and the immediate clinical applicability of current smartphone technology. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Pramana G, Parmanto B, Kendall PC, Silk JS. The SmartCAT: an m-health platform for ecological momentary intervention in child anxiety treatment. Telemed J E Health. 2013;20:419–27. doi: 10.1089/tmj.2013.0214. doi:10.1089/tmj.2013.0214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6••.Gustafson DH, McTavish FM, Chih M-Y, et al. A smartphone application to support recovery from alcoholism: a randomized clinical trial. JAMA Psychiatr. 2014;71:566–72. doi: 10.1001/jamapsychiatry.2013.4642. doi:10.1001/jamapsychiatry.2013.4642. This is a significant paper as it is one of the largest and most methodologically rigorous studies demonstrating the clinical applicability of smartphones and their ability to collect high volume, variety and velocity data related to clinical care. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Glenn T, Monteith S. New measures of mental state and behavior based on data collected from sensors, smartphones, and the Internet. Curr Psychiatry Rep. 2014 doi: 10.1007/s11920-014-0523-3. doi:10.1007/s11920-014-0523-3. [DOI] [PubMed] [Google Scholar]
- 8.Miller G. The smartphone psychology manifesto. Perspect Psychol Sci. 2012;7(3):221–37. doi: 10.1177/1745691612441215. doi:10.1177/1745691612441215. [DOI] [PubMed] [Google Scholar]
- 9.Torous J, Friedman R, Keshvan M. Smartphone ownership and interest in mobile applications to monitor symptoms of mental health conditions. J Med Internet Res. 2014:16. doi: 10.2196/mhealth.2994. doi:10.2196/mhealth.2994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10••.Torous J, Chan SR, Tan SY, et al. Patient smartphone ownership and interest in mobile apps to monitor symptoms of mental health conditions: a survey in four geographically distinct psychiatric clinics corresponding author. JMIR Ment Heal. 2014;1:1–7. doi: 10.2196/mental.4004. doi:10.2196/mental.4004. This paper provides the largest dataset, stratified by age and clinic setting, regarding mental health patients’ interest in smartphone monitoring. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Donker T, Petrie K, Proudfoot J, Clarke J, Birch MR, Christensen H. Smartphones for smarter delivery of mental health programs: a systematic review. J Med Internet Res. 2013:15. doi: 10.2196/jmir.2791. doi:10.2196/jmir.2791. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Boudreaux ED, Waring ME, Hayes RB, Sadasivam RS, Mullen S, Pagoto S. Evaluating and selecting mobile health apps: strategies for healthcare providers and healthcare organizations. Transl Behav Med. 2014;4:363–71. doi: 10.1007/s13142-014-0293-9. doi:10.1007/s13142-014-0293-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Bush NE, Skopp N, Smolenski D, Crumpton R, Fairall J. Behavioral screening measures delivered with a smartphone app: psychometric properties and user preference. J Nerv Ment Dis. 2013;201:991–5. doi: 10.1097/NMD.0000000000000039. doi:10.1097/NMD.0000000000000039. [DOI] [PubMed] [Google Scholar]
- 14.Press G. 12 big data definitions: what’s yours? Forbes. 2014 http://www.forbes.com/sites/gilpress/2014/09/03/12-big-data-definitions-whats-yours/. Accessed 3 Jan 2015.
- 15.Markowetz A, Błaszkiewicz K, Montag C, Switala C, Schlaepfer TE. Psycho-informatics: big data shaping modern psychometrics. Med Hypotheses. 2014;82:405–11. doi: 10.1016/j.mehy.2013.11.030. doi:10.1016/j.mehy.2013.11.030. [DOI] [PubMed] [Google Scholar]
- 16.Selby EA, Yen S, Spirito A. Time varying prediction of thoughts of death and suicidal ideation in adolescents: weekly ratings over 6-month follow-up. J Clin Child Adolesc Psychol. 2013;42:481–95. doi: 10.1080/15374416.2012.736356. doi:10.1080/15374416.2012.736356. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Ou J, Xie L, Jin C, et al. Characterizing and differentiating brain state dynamics via hidden Markov models. Brain Topogr. 2014 doi: 10.1007/s10548-014-0406-2. doi:10.1007/s10548-014-0406-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Ip EH, Zhang Q, Rejeski WJ, Harris TB, Kritchevsky S. Partially ordered mixed hidden Markov model for the disablement process of older adults. J Am Stat Assoc. 2013;108(2015):370–80. doi: 10.1080/01621459.2013.770307. doi:10.1080/01621459.2013.770307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Elliot RJ, Aggoun L, Moore JB. Hidden Markov models. 2008 [Google Scholar]
- 20.Grunerbl A, Muaremi A, Osmani V, et al. Smart-phone based recognition of states and state changes in bipolar disorder patients. IEEE J Biomed Health Inform. 2014 doi: 10.1109/JBHI.2014.2343154. doi:10.1109/JBHI.2014.2343154. [DOI] [PubMed] [Google Scholar]
- 21.Hastie T, Tibshirani R, Friedman J. The elements of statistical learning. Elements. 2009;1:337–87. doi:10.1007/b94608. [Google Scholar]
- 22••.James G, Witten D, Hastie T, Tibshirani R. An introduction to statistical learning. Springer; New York: 2013. This book summarizes a wide variety of the best and most basic methods available to predict and interpret data, written for non-specialists with a focus on application. [Google Scholar]
- 23.Burke J a, Estrin D, Hansen M, et al. Participatory sensing. WSW’06 at SenSys’06. 2006 [Google Scholar]
- 24.Lane ND, Miluzzo E, Lu H, Peebles D, Choudhury T, Campbell AT. A survey of mobile phone sensing. IEEE Commun Mag. 2010;48:140–50. (September) doi:10.1109/MCOM.2010.5560598. [Google Scholar]
- 25.De Boeck P, Wilson M. Explanatory item response models. 2004:382. doi:10.1007/978-1-4757-3990-9. [Google Scholar]
- 26.Liu LC, Hedeker D. A mixed-effects regression model for longitudinal multivariate ordinal data. Biometrics. 2006;62:261–8. doi: 10.1111/j.1541-0420.2005.00408.x. (March) doi:10.1111/j.1541-0420.2005.00408.x. [DOI] [PubMed] [Google Scholar]
- 27.Liu LC, Hedeker D, Mermelstein RJ. Modeling nicotine dependence: an application of a longitudinal IRT model for the analysis of adolescent nicotine dependence syndrome scale. Nicotine Tob Res. 2012;15:326–33. doi: 10.1093/ntr/nts125. doi:10.1093/ntr/nts125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Iani L, Lauriola M, Costantini M. A confirmatory bifactor analysis of the hospital anxiety and depression scale in an Italian community sample. Health Qual Life Outcomes. 2014;12(1):84. doi: 10.1186/1477-7525-12-84. doi:10.1186/1477-7525-12-84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Klasnja P, Pratt W. Healthcare in the pocket: mapping the space of mobile-phone health interventions. J Biomed Inform. 2012;45(1):184–98. doi: 10.1016/j.jbi.2011.08.017. doi:10.1016/j.jbi.2011.08.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Kotsiantis SB. Decision trees: a recent overview. Artif Intell Rev. 2013;39:261–83. (June 2011) doi:10.1007/s10462-011-9272-4. [Google Scholar]
- 31.Mun M, Reddy S, Shilton K, Yau N. PEIR, the personal environmental impact report, as a platform for participatory sensing systems research. MobiSys. 2009:55–68. doi:10.1145/1555816.1555823. [Google Scholar]
- 32.Wu M-J, Wu HE, Mwangi B, et al. Prediction of pediatric unipolar depression using multiple neuromorphometric measurements: a pattern classification approach. J Psychiatr Res. 2015 doi: 10.1016/j.jpsychires.2015.01.015. doi:10.1016/j.jpsychires.2015.01.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Patel MJ, Andreescu C, Price JC, Edelman KL, Reynolds CF, Aizenstein HJ. Machine learning approaches for integrating clinical and imaging features in late-life depression classification and response prediction. Int J Geriatr Psychiatry. 2015 doi: 10.1002/gps.4262. doi:10.1002/gps.4262. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Burns MN, Begale M, Duffecy J, et al. Harnessing context sensing to develop a mobile intervention for depression. J Med Internet Res. 2011;13(3):e55. doi: 10.2196/jmir.1838. http://eutils.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&id=21840837&retmode=ref&cmd=prlinks. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Curran PJ, McGinley JS, Bauer DJ, et al. A moderated nonlinear factor model for the development of commensurate measures in integrative data analysis. Multivar Behav Res. 2014;49:214–31. doi: 10.1080/00273171.2014.889594. (February 2015) doi:10.1080/00273171.2014.889594. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Perera C, Zaslavsky A, Christen P, Georgakopoulos D. Context aware computing for the Internet of things: a survey. IEEE Commun Surv Tutorials. 2014;16(1):414–54. doi:10.1109/SURV.2013.042313.00197. [Google Scholar]
- 37.Rosenquist JN, Fowler JH, Christakis NA. Social network determinants of depression. Mol Psychiatry. 2011;16(3):273–81. doi: 10.1038/mp.2010.13. doi:10.1038/mp.2010.48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Christakis NA, Fowler JH. Social contagion theory: examining dynamic social networks and human behavior. Stat Med. 2013;32:556–77. doi: 10.1002/sim.5408. (November 2011) doi:10.1002/sim.5408. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Rivlin A, Hawton K, Marzano L, Fazel S. Psychosocial characteristics and social networks of suicidal prisoners: towards a model of suicidal behaviour in detention. PLoS One. 2013:8. doi: 10.1371/journal.pone.0068944. doi:10.1371/journal.pone.0068944. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Kennedy DP, Adolphs R. The social brain in psychiatric and neurological disorders. Trends Cogn Sci. 2012;16(11):559–72. doi: 10.1016/j.tics.2012.09.006. doi:10.1016/j.tics.2012.09.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Barabási A-L, Gulbahce N, Loscalzo J. Network medicine: a network-based approach to human disease. Nat Rev Genet. 2011;12:56–68. doi: 10.1038/nrg2918. doi:10.1038/nrg2918. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Bullmore E, Sporns O. The economy of brain network organization. Nat Rev Neurosci. 2012 doi: 10.1038/nrn3214. doi:10.1038/nrn3214. [DOI] [PubMed] [Google Scholar]
- 43.Rubinov M, Bullmore E. Schizophrenia and abnormal brain network hubs. Dialogues Clin Neurosci. 2013;15:339–49. doi: 10.31887/DCNS.2013.15.3/mrubinov. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44••.Onnela J-P, Saramäki J, Hyvönen J, et al. Structure and tie strengths in mobile communication networks. Proc Natl Acad Sci U S A. 2007;104:7332–6. doi: 10.1073/pnas.0610245104. doi:10.1073/pnas.0610245104. This was the first paper to demonstrate the construction of social networks from mobile phone communication data, also known as call detail records (CDRs), which is a form of high-volume passive data collected by telecom operators for billing purposes worldwide. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Onnela J-P, Saramäki J, Hyvönen J, et al. Analysis of a large-scale network of one-to-one human communication. New Journal of Physics. 2007;9(9):179–179. doi:10.1088/1367-2630/9/6/179. [Google Scholar]
- 46.Onnela J-P, Arbesman S, Gonzalez M, et al. Geographic constraints on social network groups. PLoS ONE. 2011;6(4):e16939. doi: 10.1371/journal.pone.0016939. doi:10.1371/journal.pone.0016939. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47••.Eagle N, Pentland A. Reality mining: sensing complex social systems. Pers Ubiquit Comput. 2006;10:255–68. doi:10.1007/s00779-005-0046-3. This is a significant paper as it was one of the first to propose mobile phone sensing in computer science in the academic research community. [Google Scholar]
- 48.Baller RD, Richardson KK. The “dark side” of the strength of weak ties: the diffusion of suicidal thoughts. J Health Soc Behav. 2009;50:261–76. doi: 10.1177/002214650905000302. doi:10.1177/002214650905000302. [DOI] [PubMed] [Google Scholar]
- 49.Torous J, Staples P, Shanahan M, Charlie L, Pamela P, Keshavan M, et al. Utilizing a personal mobile phone custom app to assess the Patient Health Questionnaire-9 depressive symptoms in patients with major depressive disorder. JMIR Ment Heal. 2015;2(1):e8. doi: 10.2196/mental.3889. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Powell AC, Landman AB, Bates DW. In search of a few good apps. JAMA. 2014;311(18):1851–2. doi: 10.1001/jama.2014.2564. [DOI] [PubMed] [Google Scholar]


