Abstract
Parental coping with new CF diagnoses often includes religion; however, little is known about how the use of religion changes over time. Longitudinal grounded theory method, in which parents were interviewed twice the 2 years after their child’s diagnosis, was used. Parents constructed the meaning that parenting a child with CF is their vocation, in accordance with “God’s plan.” A shift from isolation to an outward focus and reentry into the community was clear. The use of faith evolved over time and continues to be a source of support and hope for parents. Clinical implications of parental religion are discussed.
Keywords: Cystic fibrosis, Parents, Coping, Religion, Diagnosis
Introduction
After receiving the potentially devastating news that their child has been diagnosed with a life-shortening disease such as cystic fibrosis (CF), parents may use a variety of strategies to cope. Given the importance of religion in the United States, many parents use religious beliefs to cope with their child’s disease and make meaning of their experience (Newport 2008). This meaning-making may have an effect not only on parental distress but also in the way they respond to the challenge of managing their child’s disease. Despite this, while the psychological impact of CF has been well-documented, relatively few studies in CF include a religious or spiritual dimension (Bluebond-Langner 1996; Glasscoe and Quittner 2003; Glasscoe et al. 2007; Glasscoe and Smith 2008). Religion is “the feelings, thoughts, experiences, and behaviors that arise from a search for the sacred…and the means and methods of that search are validated and supported by an identifiable group of others” (Hill and Pargament 2003). Religion is a multidimensional construct differing from spirituality, which does not require that the means and methods arising from one’s search for the sacred be validated by others. One dimension of religion is called “religious coping,” which is defined as, “the search for significance, in ways related to the sacred, in times of stress” (Pargament 1997). Religious coping is one form of coping previously reported by parents of children with chronic diseases, including CF (Abbott et al. 2001; Tarakeshwar and Pargament 2001; Grossoehme et al. 2008, 2009). Pargament, who initially described religious coping, names three broad goals that people use in their search for significance: to control/problem-solve, to seek comfort/intimacy, and to make meaning (Pargament 1997). Coping by making meaning becomes more important in situations where problem-solving is not an option, as in a genetic disease (Park 2005). Religion then provides causal explanations for stressors, and the reappraisals it offers of stressors have health associations (Pargament 1997; Park 2005).
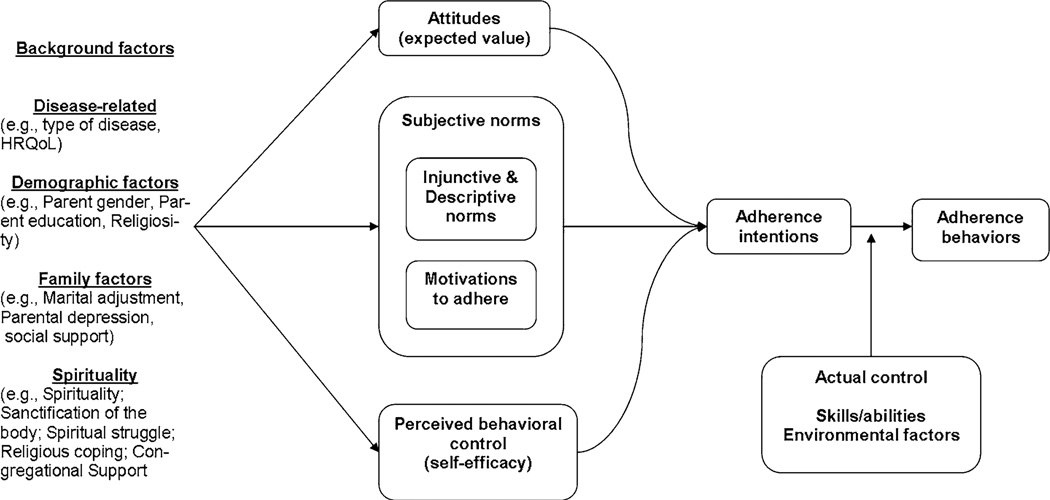
CF is a life-shortening, autosomal recessive, chronic disease with a mediate life expectancy of 37 years (in 2008) (Cystic Fibrosis Foundation Patient Registry 2011). The incidence in the United States is 1 in 4,000 and affects primarily Caucausians. Although frequently considered a pulmonary disease, CF is also associated with diabetes, pancreatic malabsorption, cirrhosis of the liver, infertility in males, and sinusitis and nasal polyps. The at-home treatment regimen is burdensome, including chest physiotherapy 2–4 times daily, inhaled antibiotics or corticosteroids, nutritional enzymes, insulin (if diabetic), and a high-calorie diet (Wilfond and Taussig 1999). Parental response to the demands of caring for a child with CF, including adherence to treatment, is partly determined by the way this family crisis is experienced. Scholars have recognized the association between parents’ use of religious coping and their child’s health outcomes (Tarakeshwar and Pargament 2001). Prominent models of human behavior, such as the theory of reasoned action (TRA) (Fishbein and Ajzen 2010), suggest ways that religious coping may be linked to adherence behavior. The TRA (Fig. 1) suggests that people’s intentions reasonably follow from their attitudes about the behavior’s value, their motivations to perform the behavior, their self-efficacy in completing the behavior, and environmental factors. Within the TRA, religious coping is a “background factor” affecting attitudes and motivations (Ajzen and Fishbein 1980). We posit that parental religious coping is a potentially important variable in adherence behavior, and therefore potentially important to health outcomes for children with chronic health conditions such as CF.
Figure 1.
Theory of reasoned action
Studies in religion/spirituality and health have been hampered by cross-sectional, rather than longitudinal designs, thus failing to account for religious development over time (Koenig et al. 2001). Pargament has shown that religion may either facilitate psychological growth or block it (Pargament 2008). Fowler’s developmental theory of faith posits that beliefs evolve due to experience (Fowler 1981). The present study attempts to address this handicap by presenting a longitudinal qualitative study modeling parents’ use of religion in the 2 years following their child’s CF diagnosis. When there are no a priori models offering hypotheses to test, the grounded theory method is frequently used in health care (over 3,000 articles in PubMed, although only 10 are in CF samples) (Pendleton et al. 2002). This method provides a structured means of obtaining, analyzing, and interpreting qualitative data leading to the development of an emergent theoretical model that is capable of later testing (Glaser and Strauss 1967; Charmaz 2006).
Methods
Participants
This study was approved by the hospital’s institutional review board. The study was conducted at an academic pediatric hospital with an accredited CF Center. The CF Center serves the population in portions of four states. Approximately 10–12 children are diagnosed annually at this Center, primarily through newborn screening. Purposive sampling was used to obtain the names of parents of children diagnosed with CF between June 1, 2007, and February 28, 2009 (15 diagnosed children with 21 parents with custody of them). Parents of children diagnosed with CFTR-metabolic syndrome were excluded. Non-participation is accounted for as follows: one parent was incarcerated; one did not have a functional telephone and did not bring their child to clinic during the recruitment period; two parents of one child did not keep interview appointments twice and were dropped from the study; and two children were diagnosed while data were being collected and analyzed and before data saturation occurred and were not contacted to participate. Given the reasons for non-participation, there did not appear to be a pro-religious bias among those who agreed to participate. The length of the recruitment period was determined by achieving “saturation” as described below. All but one child was diagnosed by newborn screening (the other child was diagnosed following an ultrasound of the sinuses). The study and parents’ eligibility was explained to the parents during their child’s regularly scheduled clinic visit at least 3 months after their child was diagnosed with CF. Opportunity to “opt out” of any further participation in this study was given; those who did not opt out were contacted by telephone within the next 2 weeks to answer any questions about the study, and to schedule an interview and obtain informed consent if either or both parents desired. Fifteen parents agreed to participate (71%); participation by both parents occurred in three cases, following the model of previous studies which included both parents (Mahoney et al. 1999; Myers 2006; Yoshimoto et al. 2006). Parents were interviewed separately if both participated. Demographics of participants in both the first and second interviews are presented in Table 1.
Table 1.
Demographic characteristics of parent sample
| Year 1 | Year 2 | |
|---|---|---|
| Number of parent participants | 15 | 12 |
| Parent gender (% female) | 9 (66) | 7 (58) |
| Median child age at diagnosis (range) | 0.25 mos (0.25–55mos) | 0.25 mos (0.25–55 mos) |
| Religious affiliation | ||
| Roman Catholic | 5 | 4 |
| Baptist | 6 | 3 |
| Non-denominational Christian | 4 | 5 |
Procedure
One year after their initial interview, parents were re-contacted by telephone, reminding them of the second interview and inviting them to schedule one. Parents were again offered the choice of telephone or in-person interviews; all chose telephone interviews. Given the potentially sensitive nature of interviews regarding religious beliefs, interviews that are not in-person have been considered to yield better data and lack the perceived need for participants to offer socially correct or expected responses (Midanik et al. 2001; Jaya et al. 2008). Interviews were audio recorded, transcribed, and checked for accuracy. If both parents of a child participated in an interview, interviews were conducted individually to alleviate any potential spousal influence. The semi-structured interview guide was developed based upon the findings from the first year’s findings, consistent with the grounded theory method in which questions evolve based on emerging information. The interview guide focused on prompts to invite deeper reflection on the meaning of faith statements commonly made during the first interviews, while encouraging an open-ended discussion on how participants used religion over the course of the first 2 years. Recruitment, data collection and data analysis in grounded theory methodology continues until a sufficient quantity and quality of data are achieved. The criterion generally used is “saturation”—the point at which no new information was being gained (Morse 1995). Charmaz advocates adopting Christian and Denzin’s criterion of “interpretive sufficiency” (Charmaz 2005). We were guided by Charmaz’ proposal in evaluating the interpretive sufficiency of our data and defining the end-point to the recruitment period.
Analysis
The second year interview transcripts were analyzed one sentence or segment of sentences at a time, and the concept was named using the parent’s own words (Charmaz 2006). Coding of data was completed by at least two authors to counteract potential single-coder biases. This initial coding, using the constant comparative method, resulted in 737 coded segments. Focused coding proceeded by grouping data segments judged to be similar to one another into categories. Categorization was done initially by the first three authors individually, resulting in 32 categories, after which results were compared and the relationship between the categories clarified and conflicts resolved by consensus. Following Saldana’s longitudinal qualitative analytic method, the major categories from the second year interviews were compared to those from the first year interviews (Saldana 2003). The change over time, if any, of the categories was noted, and a central theme with five explanatory categories was developed. This central theme summarized parents’ use of religion during the first 2 years after their child was diagnosed with CF. The central theme and explanatory categories were then presented by e-mail or in-person to the parent participants as a form of member-checking to assure the trustworthiness of the analysis.
Results
Demographics
Twelve of the fifteen parents from the first study participated in second interviews (75%; N = 7 female); demographics are presented in Table 1. The average interview length was 32 min. All reported being Christian (N = 4 Roman Catholic, N = 3 Baptist; N = 5 nondenominational). Their 7 children (5 were female) had a median age at diagnosis of 70 days (range = 1–1,653 days). All parents were Caucasian. These demographics are typical of this CF Center. Three of the original fifteen parents did not participate in second interviews: one moved and no contact information was available; and two parents agreed to the second interview but did not schedule one. During member-checking, three parents provided feedback on the emergent model, which led to the substitution of “faith” for “religion.” Religion had negative connotations to them of denominational divisiveness; faith suggested an equality of means to reach the same Deity.
Central Theme: Parenting a Child with CF is a Vocation
Two years after their child’s CF diagnosis, parents continue to cope by making religious meaning of their experience. However, the meaning evolved over time. After the first year, the meaning was, “We can handle this devastating diagnosis” and articulated a belief in an active, benevolent, interventionist God who worked in their child’s best interest. Over the subsequent year, they constructed the meaning that parenting a child with CF is a vocation to which they have been called by God. Parents were far more outspoken after the second year that “God has a plan for us” or “This [CF] was put on us for a reason.” One father expressed perceiving God’s Plan as calling them to a vocation of parenting a child with CF: “We were chosen as a family to have CF…” A mother accepted her parental vocation by saying, “…if it takes me to have a baby with CF instead of a family that maybe doesn’t want to take the time to do the treatments, or just doesn’t have time in their life or has too much on her plate or whatever, I would rather do it.” Several parents commented on the purpose of their vocation as CF parents as being, “…to open our eyes to different problems, not only CF but different problems with little kids and people in general…” This represents a shift in how parents view themselves, evolving from believing that God is active, though somewhat mysteriously, in their lives, to believing that they have been selected for the special vocation of parenting a child with CF.
Explanatory Categories
Learning How God Works in this World
By the end of the second year, parents had begun to describe an educational aspect to their vocation. They spoke of learning through experience how God works in this world. A father said, “I can’t change God’s plan, I just need to learn what I need to learn” and another parent said, “I have to let God teach me what He needs to teach me…part of that is realizing that there is a purpose to it (CF)…” Some parents described their learning about God’s plan as, “an evolving revelation as we go on.”
Articulating a Role for Genetics
The constructed meaning in the second year included an explanation for genetics. Four parents endorsed genetics’ role, and three of them held their understanding of genetics and God in tension. One mother said, “I’m a die-hard biology major…I know about prayer, and I know that God has given me strength and knowledge, but I also have a very firm grasp on the science behind CF…I just don’t feel that God can take CF away…” Another mother, while verbalizing that “genetics are genetics and that’s what it is” went on to say that “I also don’t think that I ended up with a child with CF for no reason…”
Religious Beliefs Have Adherence Implications
Religion’s implications for adherence/treatment continued to be a theme: “I think you kind of do what you can here, by doing treatments and medications and doing what works.” A mother said, “God created women (who) have these motherly instincts…I think God is always in our hearts telling us what to do. Even if it was the decision was to have the feeding tube but I knew it was the right thing, I would have felt a tugging on my heart that says, ‘Okay, you need to let the doctors do what they need to do.’ But I just knew [she wouldn’t need it].” Adherence affects parents’ psychologically: “If I go to bed at the end of the day and say, I did all those treatments and everything she needed in regards to that, as well as being the mom to a 2-year-old and what a 2-year-old needs, then I’m okay. If I were to go to bed and think I didn’t give her a breathing treatment–that would be a different story.”
Decreasing Isolation and Increasing Outward Focus
Parents described a shift from the first to the second years’ experience in terms of feeling less isolated, and more outwardly focused. Parents’ prayers shifted from the inward question “Why?” to the outward question, “What? One father’s described his prayers evolving from, “Woe is me” to “What do you want me to do now?,” and “How can I give back more than I’m doing?” Parents described ending their self-imposed isolation due to infection control concerns and the amount of time needed for home treatments. One mother said, “It was a pretty devastating blow…probably for the next year we kept him in a bubble. I was so afraid about anyone even breathing on him. We just isolated him from people and it was miserable for us…we would take turns going to church…(now) I don’t know if I do let my guard down or I said God won’t let you get sick there…and so we just go very early and wipe down the pews and books and he has every right to be part of that community just as everybody else there does.”
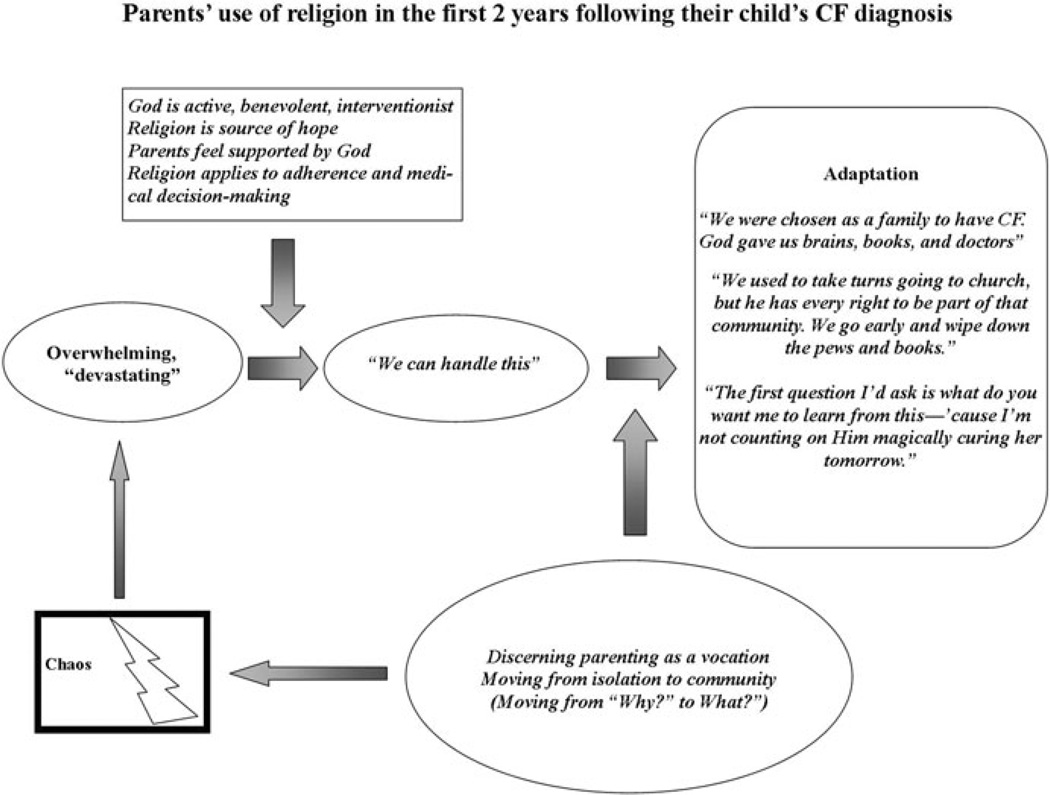
Discussion
We present results of a longitudinal study of parents’ use of faith to cope with having a child with CF (see Fig. 2). Their use of faith is important because parents used faith in medical decision-making as well as in coping. Parents used faith to cope by constructing meaning, which evolved over 2 years from a sense of survival expressed by the quote, “We can handle this” to developing a new identity: parenting a child with CF is their vocational calling. This meaning reflected increased parental self-confidence and self-competence: a movement from feeling a victim’s fear and anger, to feeling a sense of pride at being chosen and able to care for a special child. This implied a need to learn how God was active in their lives and to complete recommended treatments. By the end of the second year, parents experienced God acting internally, providing what they needed to face challenges, rather than God acting outwardly to cure their child’s CF. They also believed that God’s plan included “giving back” to others and learning to assert their child’s right to be in community rather than in a protective bubble. Their statements demonstrate how their faith played a role in adapting to living with a child’s chronic illness.
Figure 2.
Model of parental use of religion
Although rarely expressed during the first interviews, parents uniformly connected their experience of having a child with CF to “God’s plan.” Attributing disease to God’s will or plan is common. Allen previously described this use of religious language as a means of preserving a sense of order in the world despite appearances to the contrary (Allen 1992). Mickelson and colleagues described attributions to fate/God’s will, and found that was the only attribution related to less distress among parents of children born with Down’s Syndrome, as well as the only predictor of decreased depression (Mickelson et al. 1999). Even if providers disagree with the parents’ attribution, it may be potentially harming to contradict or attempt to change their perspective.
Parental understanding of God’s plan as being progressively revealed allows new experiences to be readily integrated into their orienting system. This is consistent with work by Cadge and colleagues, studying written prayers in a hospital chapel, in which they noted that the desired outcome expressed in the prayers was frequently worded vaguely permitting multiple interpretations. They suggested a potential psychological benefit to this openness to God’s work; however, it proceeded, rather than insisting that there could only be one outcome in a situation (Cadge et al. 2008).
Emerging in the second round of interviews was the relationship between the genetic cause of CF and God’s plan. The parents who verbalized the genetic basis of CF described it as the means by which God’s plan for their child unfolded. This is a significant point with two implications. First, this attribution may explain the apparent lack of parental guilt for passing on genes with the mutations causing CF to their child: since the disease is part of God’s Plan for their child, they may be responsible for gene transmission but not culpable for the disease. Second, we suggest that attributing CF to God’s plan allowed these parents to move from isolated inwardness to more outwardly directed re-integration into community. Through “normalizing” the diagnosis as being part of God’s plan, they did not develop a sense of chronic guilt or shame but developed means of making their way back into important groups of people outside their homes.
The developers of the grounded theory method initially advocated delaying the literature review of a topic until after data analysis was completed. This attempted to minimize the influence of sources other than the participants’ own words (Charmaz 2006). We discuss our findings in terms of two topics of previous research: health care behaviors as modeled in the theory of reasoned action and the emotional impact of a having a child diagnosed with CF.
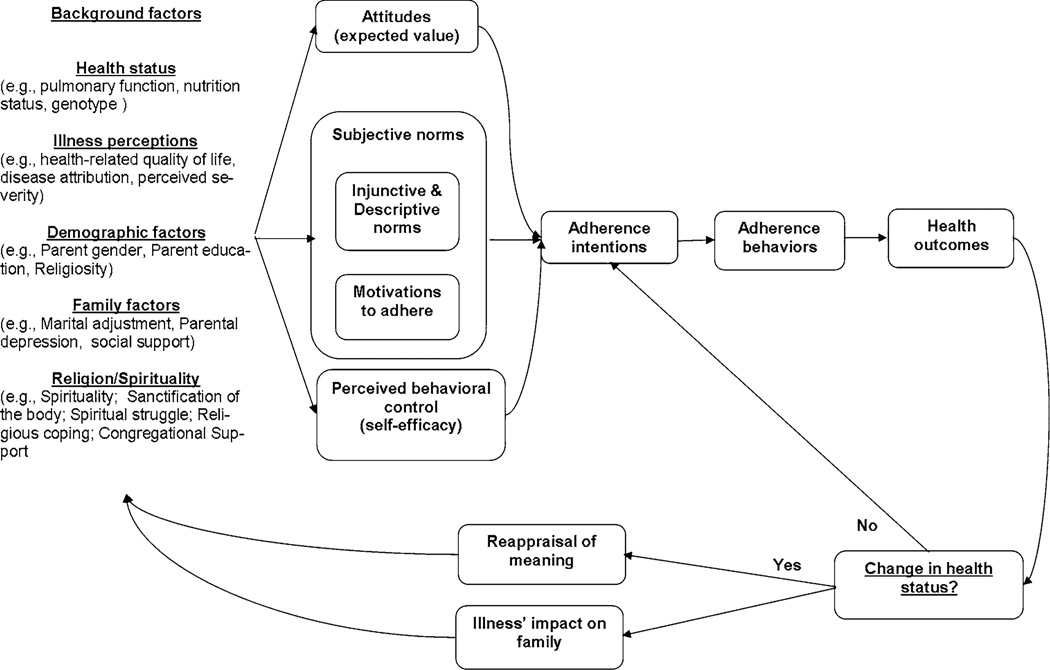
Extension of Theory of Reasoned Action
Religious beliefs and coping mechanisms are among many “background factors” in the TRA. While the TRA is typically shown as a linear model, this may fail to capture the dynamic and recursive nature of the relationship between religious beliefs and behavior and the influence of changing disease acuity. Park and Folkman presented a processive model in which religious coping is conceptualized as a meaning-making framework for coping with stressors such as illness (Park 2005). This model is especially helpful in understanding behaviors in cases where coping as “problem-solving” is unlikely to be helpful, such as in bereavement, trauma, and stressors which will not “go away,” such as a child’s CF disease. Parks suggests that coping with such stressors is principally the construction of meaning. Pargament has argued that the stability of religious beliefs for many adults is such that persons are more likely to construct a new meaning for a novel event rather than change their beliefs (Pargament 1997). Park’s model is a continuous cycle of assessing a stressor and any discrepancy between one’s current assessment and previous assessments of the stressor. When the current situation is appraised to be discrepant with one’s previous situation (e.g., realizing that the rule “children should outlive their parents” is threatened by a child’s CF diagnosis), the distress generated leads to changes in coping styles. The changing use of religion over the two s in this study suggests that the TRA should be extended to show that changes in how religion is used to make meaning may lead to changes in any or all of the three determinants of adherence behaviors (utility, injunctive norms, and self-efficacy). Such changes may lead to changed adherence behavior which in turn may lead to a change in health status (decreased pulmonary function, or the slowing of such a decrease). A change in health status leads to reappraising the level of the stressor presented by a child’s CF and the cycle repeats. We depict this recursive process in Fig. 3.
Figure 3.
Extended theory of reasoned action
Emotional Impact of Having a Child Diagnosed with CF
There are a limited number of in-depth studies concerning the impact of CF on parents. One well-known study was conducted between 1985 and 1986 by Bluebond-Langner. Her work described the time between a child’s diagnosis and their first anniversary clinic visit in terms of coping by developing a routine for CF-treatment tasks and compartmentalizing information about CF and its consequences. Thereafter, parents begin to avoid reminders of CF; redefine “normal”; reassess their priorities and reconceptualize the future (Bluebond- Langner 1996). As in the present study, Bluebond-Langner describes similar feelings to the “devastating” language and fear expressed in the present study during the first year after diagnosis and increased self-confidence thereafter (Bluebond-Langner 1996).
Bluebond-Langner’s study did not include discussion of religion or spirituality. This affects the comparisons which can be drawn between the two studies, since the present study reports on parental coping by constructing meaning through religious beliefs. Parents’ identity and to some extent their adherence and medical decision-making behaviors are based on religious beliefs. Given the 25 years that have elapsed since the field work for that study was completed, CF parents today face a different reality with CF. The average life expectancy in the United States in the mid-1980s was about 27 years; in 2008 it was 37 years (Cystic Fibrosis Foundation Patient Registry 2011). Current airway clearance techniques now include alternatives unavailable to the parents in her study, which alters the parental burden, and therefore potentially the means of coping required to meet its challenges. One point of contact between the two studies is the redefinition of a normal life sometime after the first year post-diagnosis. One parent’s description of changes in their worship behavior exemplifies this: the mother asserted that her child, “…has every right to be part of that community as everybody else there does.” The same family integrated infection control practices and worship with their early arrival at the church to “wipe down the pews and books.” The movement from decreasing isolation and increasing outward focus in the present study is consistent with the adjustment described by Bluebond-Langner.
While our study did not intend to explore parental mood, parents did describe feeling “devastated” and isolation during the first year. This may be related to the increased vulnerability to depression of parents whose children were diagnosed with CF during their first nine months of life compared to parents of healthy infants (Glasscoe et al. 2007). The parents’ description of the isolating nature of CF was in terms of their infection control concerns that isolation may exacerbate dysphoria and contribute toward one’s vulnerability to depression by stretching a parent’s coping skills beyond what they are normally able to handle. Their use of the word “devastating” may be a means of giving voice to the hopelessness characteristic of depression.
Clinical Implications
The clinical implications are three-fold. First, some parents’ faith provides motivation to adhere to recommended treatments and therapies as well as guide their medical decisions. This guidance and motivation are frequently hidden from view, as in the case of a mother who resisted discussing a g-tube for weight gain because she and her husband felt God would answer their prayers for their child to gain weight and obviate the need for a g-tube. Such tacit beliefs may be a driving force unknown to physicians and yet working at cross-purposes to theirs. The inclusion of a chaplain in the treatment team may be helpful in early resolution of potentially conflictive encounters. Second, parents’ religious attributions of disease are common and do not suggest a lack of acceptance of a diagnosis or lack of understanding about the genetic causes of disease. In fact, such attributions may well confer a psychological health benefit that genetic attributions may not. Third, parents’ religious faith continues to be a source of support and hope and deserves to be a focus of clinical attention. Religious or spiritual assessment may be help identify parents whose beliefs are challenged by their child’s diagnosis or no longer providing them support and for whom suggestions or referrals for additional supportive services may be provided.
Limitations and Future Research
This study has limitations. The sample size is small; this Center serves a 4-state region with little religious diversity. Nonetheless, important conclusions can still be drawn. We present a longitudinal study of how parental use of religion evolved. Parental faith continues to play a positive motivating and guiding role in their child’s health care. Parents’ began attributing their child’s CF to God’s plan, understanding genetics in that light. Grounded theories are not generalizable; the findings are applicable to this study sample and will be used to generate hypotheses for future testing. Future research should test whether attributing CF to “God’s Plan” has positive or negative implications for parental decision-making or adherence to recommended therapies. Longitudinal studies of parental use of religion over the entire trajectory of a chronic disease are needed to fully understand its role in child health. Future studies should also include greater religious/spiritual diversity.
Acknowledgments
The authors acknowledge with thanks the comments and suggestions of [names of two persons withheld to preserve blinded review] that provided helpful feedback on an early version of this manuscript.
Contributor Information
Daniel H. Grossoehme, Email: Daniel.grossoehme@cchmc.org, Division of Pulmonary Medicine, Cincinnati Children’s Hospital Medical Center, 3333 Burnet Avenue, MLC2021, Cincinnati, OH 45229, USA; Department of Pastoral Care, Cincinnati Children’s Hospital Medical Center, Cincinnati, OH, USA.
Judith R. Ragsdale, Department of Pastoral Care, Cincinnati Children’s Hospital Medical Center, Cincinnati, OH, USA
Amy Snow, Department of Pastoral Care, Cincinnati Children’s Hospital Medical Center, Cincinnati, OH, USA.
Michael Seid, Division of Pulmonary Medicine, Cincinnati Children’s Hospital Medical Center, 3333 Burnet Avenue, MLC2021, Cincinnati, OH 45229, USA; James M. Anderson Center for Health Systems Excellence, Cincinnati Children’s Hospital Medical Center, Cincinnati, OH, USA.
References
- Abbott J, Dodd M, et al. Ways of coping with cystic fibrosis: Implications for treatment adherence. Disability and Rehabilitation. 2001;23(8):315–324. doi: 10.1080/09638280010004171. [DOI] [PubMed] [Google Scholar]
- Ajzen I, Fishbein M. Understanding attitudes and predicting social behavior. NJ, Prentice-Hall: Englewood Cliffs; 1980. [Google Scholar]
- Allen JT. God-talk and myth: Turning chaso into comfort. Journal of Pastoral Care. 1992;46(4):340–348. [Google Scholar]
- Bluebond-Langner M. In the shadow of illness. Princeton, NJ: Princeton University Press; 1996. [Google Scholar]
- Cadge W, Freese J, et al. The provision of hospital chaplaincy in the United States: A national overview. Southern Medical Journal. 2008;101(6):626–630. doi: 10.1097/SMJ.0b013e3181706856. [DOI] [PubMed] [Google Scholar]
- Charmaz K. Grounded theory in the 21st century. In: Denzin NK, Lincoln YS, editors. The SAGE handbook of qualitative research. Thousand Oaks, CA: Sage Publications; 2005. pp. 507–535. [Google Scholar]
- Charmaz K. Constructing grounded theory. Thousand Oaks, CA: SAGE Publications; 2006. [Google Scholar]
- Cystic Fibrosis Foundation Patient Registry. 2009 Annual Data Report. Bethesda, MD: Cystic Fibrosis Foundation; 2011. [Google Scholar]
- Fishbein M, Ajzen I. Predicting and changing behavior. New York, NY: Taylor & Francis; 2010. [Google Scholar]
- Fowler JW. Stages of faith. New York: HarperCollins; 1981. [Google Scholar]
- Glaser BG, Strauss AL. The discovery of grounded theory: Strategies for qualitative research. Chicago: Aldine Publications; 1967. [Google Scholar]
- Glasscoe C, Lancaster GA, et al. Parental depression following the early diagnosis of cystic fibrosis: A matched, prospective study. Journal of Pediatrics. 2007;150(2):185–191. doi: 10.1016/j.jpeds.2006.11.022. [DOI] [PubMed] [Google Scholar]
- Glasscoe C, Smith JA. Through a mother’s lens: A qualitative analysis reveals how temporal experience shifts when a boy born preterm has cystic fibrosis. Clinical Child Psychology and Psychiatry. 2008;13:609–626. doi: 10.1177/1359104508096772. [DOI] [PubMed] [Google Scholar]
- Glasscoe CA, Quittner AL. Psychological interventions for cystic fibrosis. Cochrane Database of Systematic Reviews. 2003;(3):CD003148. doi: 10.1002/14651858.CD003148. [DOI] [PubMed] [Google Scholar]
- Grossoehme DH, Cotton S, et al. Religious/spiritual coping by parents of adolescents with sickle cell disease: A pilot study. Spirituality, health and human flourishing: Meaning? Measurement? Implications? Durham, North Carolina: 2008. [Google Scholar]
- Grossoehme DH, Ragsdale JR, et al. Parents’ use of religion in the first year following their child’s diagnosis with cystic fibrosis. Pediatric Pulmonology. 2009;44(S32):427. doi: 10.1080/08854726.2010.480833. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hill PC, Pargament KI. Advances in the conceptualization and measurement of religion and spirituality. Implications for physical and mental health research. American Psychologist. 2003;58(1):64–74. doi: 10.1037/0003-066x.58.1.64. [DOI] [PubMed] [Google Scholar]
- Jaya J, Hindin MJ, et al. Differences in young people’s reports of sexual behaviors according to interview methodology: A randomized trial in India. American Journal of Public Health. 2008;98(1):169–174. doi: 10.2105/AJPH.2006.099937. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Koenig HG, McCullough ME, editors. Handbook of religion and health. New York, NY: Oxford University Press; 2001. [Google Scholar]
- Mahoney A, Pargament KI, et al. Marriage and the spiritual realm: The role of proximal and distal religious constructs in marital functioning. Journal of Family Psychology. 1999;13(3):321–338. [Google Scholar]
- Mickelson KD, Wrobel M, et al. “Why my child?”: Parental attributions for children’s special needs. Journal of Applied Social Psychology. 1999;29(6):1263–1292. [Google Scholar]
- Midanik LT, Greenfield TK, et al. Reports of alcohol-related harm: Telephone versus face-to-face interviews. Journal of Studies on Alcohol. 2001;62(1):74–78. doi: 10.15288/jsa.2001.62.74. [DOI] [PubMed] [Google Scholar]
- Morse JM. The significance of saturation. Qualitative Health Research. 1995;5:147–149. [Google Scholar]
- Myers SM. Religious homogamy and marital quality: Historical and generational patterns, 1980–1997. Journal of Marriage and Family. 2006;68(2):292–304. [Google Scholar]
- Newport F. Majority of Americans believe in God. Washington, DC: Gallup, Inc.; 2008. (Speaker). (on-line video recording, retrieved 7 March 2011, http://www.gallup.com/video/109111/Majority-Americans-Believe-God.aspx) [Google Scholar]
- Pargament KI. Psychology of religious coping. New York: Guildford Press; 1997. [Google Scholar]
- Pargament KI. Religious struggles: A fork in the road to growth or decline. Durham, North Carolina: Spirituality, Health, and Human Flourishing: Meaning? Measurement? Implications?; 2008. [Google Scholar]
- Park CL. Religion as a meaning-making framework in coping with life stress. Journal of Social Issues. 2005;61(4):707–729. [Google Scholar]
- Pendleton SM, Cavalli KS, et al. Religious/spiritual coping in childhood cystic fibrosis: A qualitative study. Pediatrics. 2002;109(1):E8. doi: 10.1542/peds.109.1.e8. [DOI] [PubMed] [Google Scholar]
- Saldana J. Longitudinal qualitative research. Walnut Creek, CA: AltaMira Press; 2003. [Google Scholar]
- Tarakeshwar N, Pargament KI. Religious coping in families with autism. Focus on Autism and other Developmental Delays. 2001;16:247–260. [Google Scholar]
- Wilfond BS, Taussig LM. Cystic fibrosis: General overview. In: Taussig LM, Landau LI, editors. Pediatric respiratory medicine. St. Louis: Mosby; 1999. pp. 982–990. [Google Scholar]
- Yoshimoto SM, Ghorbani S, et al. Religious coping and problem-solving by couples faced with prostate cancer. European Journal of Cancer Care. 2006;15(5):481–488. doi: 10.1111/j.1365-2354.2006.00700.x. [DOI] [PubMed] [Google Scholar]