Abstract
Psychotherapies for children and adolescents have been tested in hundreds of randomized controlled trials across five decades, and many of these youth therapies have now been classified as “empirically-supported treatments” (ESTs). A burgeoning movement is underway to implement these ESTs in clinical practice settings, but questions arise as to the readiness of the treatments for practice, and whether they will improve outcomes for clinically-referred youths. Our data show ESTs to be more effective than usual care, on average, but only modestly so, and there are troubling exceptions. One reason may be that the design of most ESTs (e.g., single-disorder focus, linear session sequence) does not fit the characteristics of referred youths or clinical practice very well. Indeed, youth psychotherapy research has not focused much on the clients or contexts of actual clinical care. An alternative empirical approach, the deployment-focused model, proposes developing and testing interventions with the clients, clinicians, and contexts for which they are ultimately intended. Recent application of the model highlights its potential for stimulating robust treatments that are effective in clinical practice.
Keywords: empirically supported treatments, youth psychotherapy, children, adolescents, implementation
Efforts to help children and adolescents (herein collectively, “youth”) are as old as parenthood. However, specific strategies for helping have evolved dramatically over time, influenced by ancient religious teachings (e.g., “spare the rod and spoil the child”), classical philosophy (e.g., using discourse to explore and restructure thoughts and behavior), medicine, and other healing traditions. The approach called youth psychotherapy is often dated to Sigmund Freud’s consultation with the father of a very anxious “Little Hans” and Freud’s psychoanalysis of his own daughter. Youth psychotherapy was later shaped by psychology’s grand theories, humanism, behaviorism (e.g., Jones, 1924), cognitive and cognitive-behavioral methods (e.g., Meichenbaum & Goodman, 1971), and diverse alternative approaches. By the turn of this century, Kazdin (2000) identified 551 different named therapies used with children and adolescents.
Empirical Tests of Youth Psychotherapy
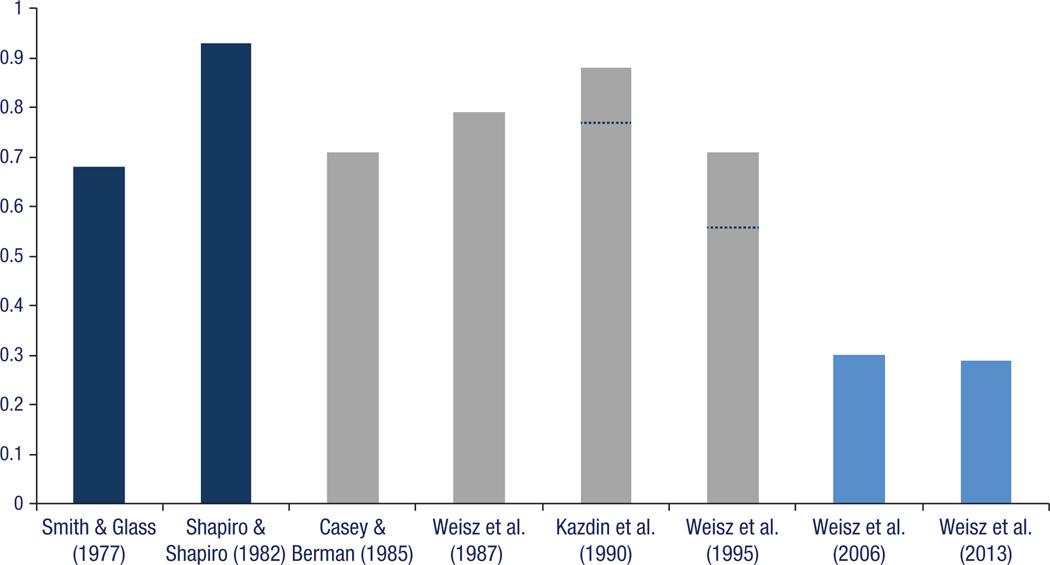
Youth treatments began to be tested empirically in the mid-1900s. Initial quasi-experimental studies of vaguely-described treatments were followed by increasingly rigorous randomized controlled trials (RCTs) testing better-documented, manual-guided psychotherapies. With this shift, concerns that youth psychotherapy had no effect (Eysenck, 1966; Levitt, 1963) gave way to evidence showing therapy outperforming various control groups. Eventually, meta-analyses (e.g., Weisz et al., 1995, 2006) showed respectable mean effects across hundreds of RCTs, effects within the range found for adult psychotherapy (see Figure 1). Task forces have now applied scientific criteria to the accumulating RCTs, to identify evidence-based or empirically supported treatments (ESTs) for youth (e.g., Silverman & Hinshaw, 2008). The criteria for EST status differ somewhat across various task forces and review groups, but most require multiple supportive RCTs, ideally conducted by independent research teams. Identifying ESTs is now a growth industry: The National Registry of Evidence-Based Programs and Practices (http://www.nrepp.samhsa.gov/ViewAll.aspx; accessed 10/05/2013) lists 306 “evidence-based” interventions, 192 for children and adolescents. A national movement is now underway to implement these interventions in everyday treatment settings.
Figure 1.
Mean effect sizes found in two broad-based meta-analyses of adult psychotherapy effects (the two bars at the left: Smith & Glass, 1977; Shapiro & Shapiro, 1982), four broad-based meta-analyses of youth psychotherapy effects (the four middle bars: Casey & Berman, 1985; Weisz et al., 1987; Kazdin et al., 1990; Weisz et al., 1995), and two meta-analyses of RCTs comparing evidence-based youth psychotherapies to usual clinical care (the two bars at the right: Weisz et al. 2006a and 2013b). The full bar for Kazdin et al. (1990) shows the mean effect size for treatment vs. inert control group comparisons; the dashed line shows the mean for treatment vs. active control group comparisons. The full bar for Weisz et al. (1995) shows the mean effect size when unweighted least squares analyses were conducted; the dashed line shows the mean for weighted least squares analyses. [Reprinted with permission, John R. Weisz].
As we enter the implementation era, two critical questions arise for clinical science: (a) Do the ESTs actually improve youth outcomes more than current practices do? [If not, then the case for implementing ESTs may not be so clear.] and (b) Are the ESTs designed in ways that fit the clinical care contexts where implementation will occur? [If not, the ESTs may be difficult to implement properly where they are most needed—i.e., where clinically-referred young people are actually treated.] These two questions pivot on a core issue for our field: Is clinical science in its current form producing interventions that are robust enough to succeed in the real-world contexts where most youth mental health care takes place. My students, colleagues, and I address these questions in much of our work.
Empirically-Supported Treatments (ESTs) versus Usual Care
Our RCTs and meta-analyses have shown that classifying a treatment “EST” is no guarantee that it will outperform the status quo. In fact, benefit tends to drop markedly when treatments leave the secure base of their university or laboratory settings and are tested against usual clinical care. Our meta-analyses of RCTs pitting ESTs against usual care (Weisz et al., 2006, 2013) show highly variable outcomes, numerous studies in which ESTs do not outperform (or even underperform) usual care, and markedly lower mean effect sizes than studies using mainly waitlist and experimenter-constructed control groups (see Figure 1). In fact, the mean effect sizes in our EST vs. usual care meta-analyses reflect a probability of only .58 (vs. chance at .50) that a randomly selected youth treated with an EST would be better off after treatment than a randomly selected youth treated with usual care. Importantly, our most recent meta-analysis (Weisz et al., 2013) showed that ESTs did not significantly outperform usual care among studies using (a) clinically referred youths, or (b) youths impaired enough to meet criteria for a formal diagnosis. These two groups are arguably prime targets for EST implementation.
These findings may be a logical consequence of the research that has produced the youth ESTs; that research is not very representative of real-world clinical practice (Weisz, Jensen-Doss, & Hawley, 2005). Although the studies are generally high in internal validity (good news), most of them are low in external validity (bad news, if effective implementation in clinical care is one’s goal). In a recent examination of 461 youth RCTs, spanning the 1960s through the most recent decade, we found that only 2.1% of all the groups were described by authors as involving clinically referred clients, treated by practitioners, in practice settings (Weisz, Ng, & Bearman, in press).
This body of relatively unrepresentative research has produced primarily (a) treatments for single disorders, or homogenous clusters, even though most clinically referred youths have comorbidity, multiple co-occurring problems, and diverse treatment needs; (b) linear treatments—with therapist manuals presenting session contents in a prescribed order (e.g., psychoeducation first, then relaxation training, etc.)—even though everyday treatment is packed with unexpected events and shifts in treatment needs; and (c) treatments that work well when implemented by researchers’ own students or employees, and under conditions designed by researchers, even though real-world implementation definitely won’t be done that way. As we have seen, these ESTs, which do not seem to fit the everyday clinical care context well, also fail to show either consistent or substantial effects in that context when compared to usual care (Weisz et al., 2006, 2013).
The problem with ESTs that do not fit well or perform well in practice settings is not just a concern for clinical science but a challenge for our colleagues in the clinical practice community, as well. The risk is that practitioners may not have access to those EBTs that will most benefit their practice and most enhance outcomes for the girls and boys they treat. Clearly, clinical scientists and clinical practitioners have a shared interest in the development of treatments that fit well and perform well within the ecosystem of real-world clinical care.
Building More Robust Treatments
To build robust treatments that are potent in everyday clinical care, we have proposed a deployment-focused model (Weisz, 2004; Weisz & Gray, 2008). The model calls for interventions to be developed and tested with the kinds of clients and therapists, and in the kinds of settings, for which the interventions are ultimately intended, and routinely tested against usual care. Such research can and should meet the same rigorous methodological standards as traditional RCTS, but it can arguably generate more externally valid evidence on intervention effects, moderation, mediation, and mechanisms of change, than research in clinically unrepresentative contexts. The deployment-focused model reflects this notion: ESTs that have been built for, adapted to, and tested within clinical care contexts should be more effective in those contexts than ESTs that have not followed that process.
Our application of the model over the years has taught us a lot about the conditions within which ESTs must be robust to succeed (Weisz, Ugueto, Cheron, & Herren, 2013). Our most recent effort, in collaboration with wise colleagues in the Research Network on Youth Mental Health, led to creation of a transdiagnostic protocol designed to address youth comorbidity (anxiety, depression, and misconduct) and ongoing shifts in treatment needs (Chorpita & Weisz, 2009). An RCT showed this treatment approach to be markedly more effective than usual care, and more effective than traditional single-disorder treatments (Weisz et al., 2012). We expect to continue applying the deployment-focused model and experimenting with treatment innovations; in the process, we hope to engage an ever-larger cohort of clinical scientists building vigorous, practice-ready treatments and a rigorous evidence base on their impact.
Acknowledgments
Some of the research reported here was supported by grants from the National Institute of Mental Health (MH57347, MH068806, MH085963), the Norlien Foundation, the MacArthur Foundation, and the Annie E. Casey Foundation. I am grateful to so many wise colleagues, postdoctoral fellows, and graduate students, for their many contributions to this work, to Lea Petrovic for her valuable help with this manuscript, and to the children, families, clinicians, clinic administrators, and government program and policy leaders who have participated in and supported our research and enriched our thinking. I receive royalties for some of the published works cited in this paper. Address correspondence to John R. Weisz, Department of Psychology, Harvard University, William James Hall, 33 Kirkland Street, Cambridge, MA 02138.
References
- Chorpita BF, Weisz JR. MATCH-ADTC: Modular approach to therapy for children with anxiety, depression, trauma, or conduct problems. Satellite Beach, FL: PracticeWise; 2009. [Google Scholar]
- Eysenck HJ. The effects of psychotherapy: An evaluation. Journal of Consulting Psychology. 1952;16:319–324. doi: 10.1037/h0063633. [DOI] [PubMed] [Google Scholar]
- Jones MC. The elimination of children’s fears. Journal of Experimental Psychology. 1924;7:382–390. [Google Scholar]
- Levitt EE. Psychotherapy with children: A further evaluation. Behaviour Research and Therapy. 1963;60:326–329. doi: 10.1016/0005-7967(63)90007-x. [DOI] [PubMed] [Google Scholar]
- Kazdin AE. Psychotherapy for Children and Adolescents: Directions for Research and Practice. New York, NY: Oxford University Press; 2000. [Google Scholar]
- Meichenbaum D, Goodman S. Training impulsive children to talk to themselves: A means of developing self-control. Journal of Abnormal Psychology. 1971;77:115–126. doi: 10.1037/h0030773. [DOI] [PubMed] [Google Scholar]
- Silverman WK, Hinshaw SP. The second special issue on evidence-based psychosocial treatments for children and adolescents: A 10-year update. Journal of Child and Adolescent Clinical Psychology. 2008;37:1–7. doi: 10.1080/15374410701818293. [DOI] [PubMed] [Google Scholar]
- Weisz JR. Psychotherapy for children and adolescents: Evidence-based treatments and case examples. New York: Cambridge University Press; 2004. [Google Scholar]
- Weisz JR, Chorpita BF, Palinkas L, Schoenwald SK, Miranda J, Bearman SK the Research Network on Youth Mental Health. Testing standard and modular designs for psychotherapy treating depression, anxiety, and conduct problems in youth: A randomized effectiveness trial. Archives of General Psychiatry. 2012;69:274–282. doi: 10.1001/archgenpsychiatry.2011.147. [DOI] [PubMed] [Google Scholar]
- Weisz JR, Gray JS. Evidence-based psychotherapies for children and adolescents: Data from the present and a model for the future. Child and Adolescent Mental Health. 2008;13:54–65. doi: 10.1111/j.1475-3588.2007.00475.x. [DOI] [PubMed] [Google Scholar]
- Weisz JR, Jensen-Doss AJ, Hawley KM. Youth psychotherapy outcome research: A review and critique of the evidence base. Annual Review of Psychology. 2005;56:337–363. doi: 10.1146/annurev.psych.55.090902.141449. [DOI] [PubMed] [Google Scholar]
- Weisz JR, Jensen-Doss A, Hawley KM. Evidence-based youth psychotherapies versus usual clinical care: A meta-analysis of direct comparisons. American Psychologist. 2006;61:671–689. doi: 10.1037/0003-066X.61.7.671. [DOI] [PubMed] [Google Scholar]
- Weisz JR, Kuppens S, Eckshtain D, Ugueto AM, Hawley KM, Jensen-Doss A. Do evidence-based youth psychotherapies outperform usual clinical care? A multilevel meta-analysis. JAMA Psychiatry. 2013 doi: 10.1001/jamapsychiatry.2013.1176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weisz JR, McCarty CA, Valeri SM. Effects of psychotherapy for depression in children and adolescents: A meta-analysis. Psychological Bulletin. 2006;132:132–149. doi: 10.1037/0033-2909.132.1.132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weisz JR, Ng MN, Bearman SK. Odd couple? Re-envisioning the relation between science and practice in the dissemination-implementation era. Clinical Psychological Science. (in press). [Google Scholar]
- Weisz JR, Southam-Gerow MA, Gordis EB, Connor-Smith JK, Chu BC, Langer DA, Weiss B. Cognitive-behavioral therapy versus usual clinical care for youth depression: An initial test of transportability to community clinics and clinicians. Journal of Consulting and Clinical Psychology. 2009;77:383–396. doi: 10.1037/a0013877. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weisz JR, Uqueto AM, Cheron DM, Herren J. Evidence-based youth psychotherapy in the mental health ecosystem. Journal of Clinical Child and Adolescent Psychology. 2013;42:274–286. doi: 10.1080/15374416.2013.764824. [DOI] [PubMed] [Google Scholar]
- Weisz JR, Weiss B, Han SS, Granger DA, Morton T. Effects of psychotherapy with children and adolescents revisited: A meta-analysis of treatment outcome studies. Psychological Bulletin. 1995;117:450–468. doi: 10.1037/0033-2909.117.3.450. [DOI] [PubMed] [Google Scholar]