Abstract
Background
Several studies showed that the waist circumference of US adults has increased over the past 25 y. However, because of the high correlation between waist circumference and body mass index (BMI; in kg/m2) (r ~ 0.9), it is uncertain if these trends in waist circumference exceed those expected on the basis of BMI changes over this time period.
Objective
We assessed whether the recent trend in waist circumference was independent of changes in BMI, age, and race-ethnicity.
Design
We analyzed data from the 1999–2000 through 2011–2012 cycles of the NHANES.
Results
The mean waist circumference increased by ~2 cm (in men) and ~4 cm (in women) in adults in the United States over this 12-y period. In men, this increase was very close to what would be expected because of the 0.7 increase in mean BMI over this period. However, in women, most of the secular increase in waist circumference appeared to be independent of changes in BMI (mean: 0.6), age, and race-ethnicity over the 12-y period. We estimated that, independent of changes in these covariates, the mean waist circumference increased by 0.2 cm in men and 2.4 cm in women from 1999–2000 through 2011–2012; only the latter estimate was statistically significant.
Conclusions
Our results indicate that, in women but not men, the recent secular trend in waist circumference is greater than what would be expected on the basis of changes in BMI. Possible reasons for this secular increase, along with sex differences, are uncertain.
Keywords: BMI, abdominal obesity, secular trends, waist circumference, panel design, adults, NHANES, obesity
INTRODUCTION
The prevalence of obesity, which is defined as BMI (in kg/m2) ≥30 in adults in the United States increased from ~15–35% between 1960–1964 and 2011–2012 (1, 2). However, recent data indicated that this secular trend has either slowed or plateaued (1, 3, 4). Although it is widely accepted that BMI is an imprecise indicator of body fatness, several studies showed that BMI is as strongly correlated with various metabolic complications as are more-accurate estimates of body fatness (5–7).
However, BMI cannot assess the distribution of body fatness, and the adverse consequences of obesity may be most strongly associated with the amount of visceral fat (8). Therefore, waist circumference has been considered to be a valuable measurement (9), and many, but not all (10), studies showed that waist circumference is either a better predictor of adverse health outcomes than is BMI or that it provides independent information on disease risk (11–14). National guidelines recommend the measurement of waist circumference in adults, particularly those with BMI between 25 and 35 (15). However, the very strong correlation (r ~ 0.9) between BMI and waist circumference complicates the assessment of the adverse consequences of body fat distribution.
The waist circumference of adults in the United States and in several other countries has increased over the past 2 decades (16–22), and some investigators concluded that these increases were at least partly independent of changes in BMI (17, 20, 21, 23). These increases in abdominal obesity have been attributed to various factors, including changes in energy intake and physical activity, increased stress, differences in race-ethnicity, and endocrine disruptors (19, 20, 24). However, it is not clear if these characteristics specifically influence abdominal rather than generalized obesity. It is also possible that most of the increase in waist circumference can be attributed to 1) secular trends in BMI over this period and 2) the strong association between BMI and waist circumference. A recent article presented mean waist circumferences and the prevalence of abdominal obesity in the NHANES from 1999–2000 through 2011–2012 (22), and the current study extends these results. Our objective was to assess whether these secular trends were independent of changes that occurred in BMI.
METHODS
We used data from the NHANES from 1998 to 1994 (NHANES III) and the seven 2-y cycles conducted from 1999–2000 through 2011–2012 (25). The NHANES used a multistage, stratified, cluster design to select a representative sample of the US civilian, noninstitutionalized population. The surveys received human subject research approval, participants provided informed consent, and procedures for the surveys were conducted in accordance with the ethical standards of the CDC. Analyses included men and nonpregnant women who were ≥20 y of age at interview and had measurements of height, weight, and waist circumference. Race and ethnicity were self-reported, and in this study, subjects were classified as non-Hispanic (NH) white, NH black, Mexican American, or other (which included Hispanics from other countries).
During the NHANES physical examination, weight, height, and waist circumference were measured in a standardized fashion (26). BMI was calculated as weight divided by the square of height. Waist circumference was measured to the nearest 1 mm just above the iliac crest by using a steel tape. Obesity was defined as BMI ≥30.0, and abdominal obesity was defined as waist circumference >102 cm (in men) or >88 cm (in women) (15).
All analyses accounted for the sample weights and sample design by using the survey package in R software (versions 3.0 and 3.1) (27, 28). For estimates shown in Figure 1 and Supplemental Table 1, obesity prevalences were age standardized to projected estimates of the 2000 US Census by using the direct method with age groups 20–39, 40–59, and ≥60 y; proportions of subjects in these age groups were 0.3966, 0.3718, and 0.2316 (29). With the exception of Supplemental Table 1, other analyses were restricted to the 7 examination cycles conducted from 1999–2000 through 2011–2012.
FIGURE 1.
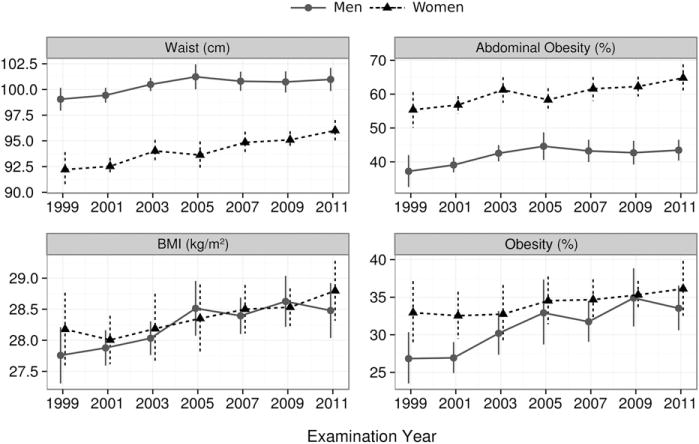
Mean, age-standardized levels (95% CIs) of waist circumference, BMI, abdominal obesity, and obesity in adults from 1999–2000 through 2011–2012. The x axis label shows the beginning of each 2-y examination cycle. Abdominal obesity was defined as waist circumference >102 cm in men and >88 cm in women.
Sex-specific regression models were used to summarize the relation of waist circumference to BMI, which was slightly nonlinear, with each 1-unit increase in BMI associated with smaller waist differences at higher BMI. We accounted for this nonlinearity by modeling BMI (and age) with restricted cubic splines with 4 knots (located at the 5th, 35th, 65th, and 95th percentiles) (30) in all regression analyses. To summarize secular trends in waist circumference, we focused on a 7-level categorical variable for the study period with 1999–2000 serving as the reference category; waist circumference was predicted by using the study period, race-ethnicity, age, and interaction between age (linear term) and race-ethnicity.
To examine whether changes in waist circumference were independent of BMI, we included BMI in a second regression model that also included cross-product terms between BMI (linear term), age (linear), and race-ethnicity. We focused the difference between study-period effects in the 2 models (with and without BMI adjustment) for waist circumference (Figure 2). Similar models, but with a linear term for study year, were constructed to assess the significance of change in waist circumference from 1999–2000 through 2011–2012. These BMI-adjusted models also examined whether trends in waist circumference varied by sex (in the overall sample), race-ethnicity, or age by including various interaction terms with the year (such as year × sex) (Figure 3).
FIGURE 2.
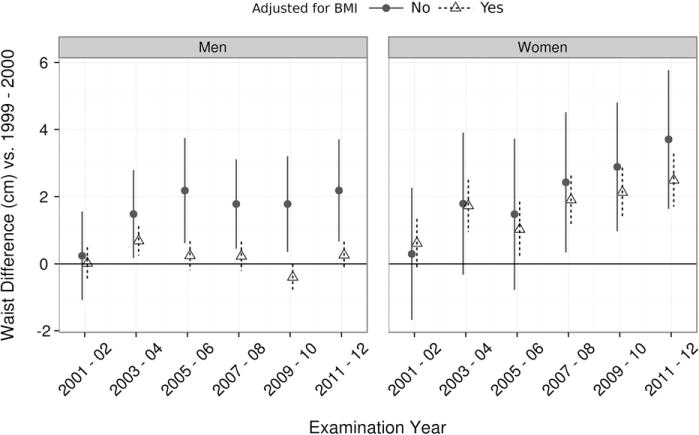
Linear regression coefficients (95% CIs) showing the difference in mean waist circumference between 1999–2000 and each subsequent study. Differences were estimated by using a logistic regression model that included the study cycle as a 7-level categorical variable with 1999–2000 as the reference category. Black circles and solid lines denote estimates from models that included race and age, whereas open triangles are estimates from models that included BMI as an additional predictor. Age and BMI were modeled by using restricted cubic splines with 4 knots, and 2-factor (linear) interactions between age, BMI, and race-ethnicity were included in the BMI-adjusted model.
FIGURE 3.
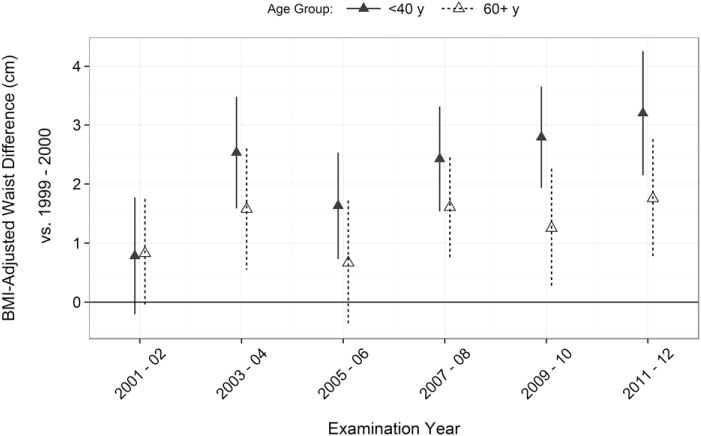
Linear regression coefficients (95% CIs) showing the difference in mean waist circumference (after BMI adjustment) between 1999–2000 and each subsequent study in 20- to 39-y-old women (solid triangle and lines) and women who were ≥60 y of age (open triangles and dotted lines). All estimates were based on models that contained race, age, and BMI as predictors. As assessed by an age × year interaction term, the secular increase in BMI-adjusted waist circumference over the 12-y period decreased with age (P < 0.001) in women.
To assess secular trends in abdominal obesity, we used Poisson regression (31–33) to estimate the RR for each 2-y cycle relative to 1999–2000 (Figure 4). In contrast to logistic regression, Poison regression can directly estimate RRs (31). We followed a similar process to that used to examine differences in waist circumference across cycles, and we estimated RRs in 2 models, one not adjusted for BMI and one that contained BMI. These regression analyses were performed with the svyglm function of the survey package (28), and although confidence intervals (CIs) estimated by Poisson regression can be conservative (31), we estimated SEs by using a quasi-Poisson model that estimated the variance of abdominal obesity from data (34). We found that these SE estimates were almost identical to those obtained by jackknife replicate reweighting.
FIGURE 4.
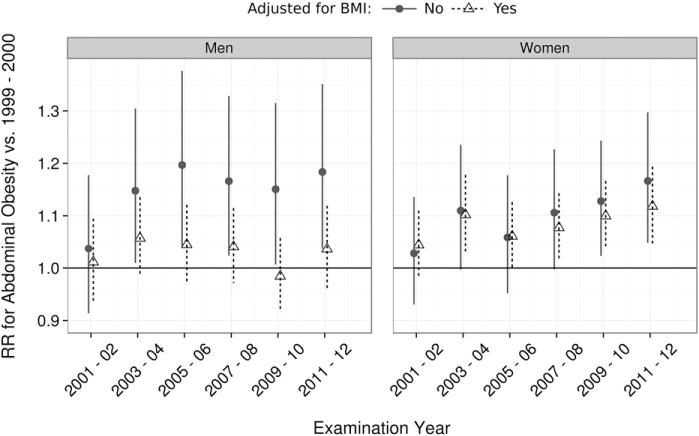
RRs (95% CIs) for abdominal obesity (waist circumference >102 cm in men and >88 cm in women) relative to 1999–2000 as calculated by using quasi-Poisson regression. Black circles and solid lines represent estimates without adjustment for BMI, and open triangles represent estimates from models that also included BMI as a predictor. These models contained the same predictor variables and interactions as in Figure 2.
There were 1339 subjects (3.3%) who had measured BMI but were missing data for waist circumference. Initial analyses indicated that the probability of missingness was related to sex (higher in women) and race (higher in blacks) and was positively associated with both BMI (missing for ~6% of subjects who had BMI ≥40) and age. To assess the potential impact of these missing measurements, we used the Amelia package (35) in the R program to generate multiple (m = 20) imputations in which missing waist data were estimated from BMI, dual-energy X-ray absorptiometry percentage of body fat, skinfold thicknesses, and other characteristics. The uncertainty of imputations were incorporated into the results by analyzing each imputation set and combining the 20 results (36). We compared imputed estimates to results obtained by excluding missing values.
RESULTS
Figure 1 and Supplemental Table 1 show mean, age-adjusted waist circumferences and BMI along with the prevalence of obesity in each study from 1999–2000 through 2011–2012. (To allow for an examination of trends over a longer period, Supplemental Table 1 also shows means of these characteristics in 1988–1994.) Between 1999–2000 and 2011–2012, mean waist circumference increased by ~2 cm (men) and ~4 cm (women), and mean BMI increased by 0.6–0.7. Over this time period, the prevalence of obesity increased by 7 percentage points in men and 3 percentage points in women.
Table 1 shows the relation of waist circumference to BMI and age in the entire sample. BMI and waist circumference were strongly correlated with the magnitudes of the associations being slightly stronger in men than women (Pearson’s r ~ 0.93 compared with 0.91), but differences across race-ethnic groups were small and inconsistent. Magnitudes of correlations tended to decrease slightly with age but were ≥0.89 in each sex-age group.
TABLE 1.
Relation of waist circumference to age and BMI1
| Race-ethnicity and age by sex | n | Correlation of waist compared with age2 | Correlation of waist compared with BMI2 |
|---|---|---|---|
| Men | |||
| NH whites | 7834 | 0.28 | 0.92 |
| NH blacks | 3347 | 0.24 | 0.94 |
| Mexican Americans | 3086 | 0.22 | 0.93 |
| Women | |||
| NH whites | 7595 | 0.19 | 0.91 |
| NH blacks | 5275 | 0.14 | 0.91 |
| Mexican Americans | 5526 | 0.20 | 0.91 |
| Age (y) | |||
| Men | |||
| 20–39 | 5546 | 0.21 | 0.94 |
| 40–59 | 5275 | 0.08 | 0.93 |
| 60–90 | 5526 | −0.08 | 0.92 |
| Women | |||
| 20–39 | 5305 | 0.12 | 0.93 |
| 40–59 | 5427 | 0.10 | 0.92 |
| 60–90 | 5559 | −0.13 | 0.89 |
Correlations were based on data for adults ≥20 y of age who were examined from NHANES 1999–2000 through 2011–2012. Note that the relation of waist circumference to both age and BMI was nonlinear. Correlations were assessed in linear regression models; all correlation coefficients were significant at the 0.0001 level. NH, non-Hispanic.
All values are weighted Pearson’s correlation coefficients.
Additional analyses indicated that the relation of BMI to waist circumference was linear up to BMI ~40, but that additional BMI increases were associated with smaller increases in waist circumference. On the basis of observed associations in 1999–2000, we estimated that mean BMI increases from 1999–2000 through 2011–2012 would be expected to be associated with a 1.8-cm (men) or 1.3-cm (women) increase in waist circumference over this time period for a NH white 45-y-old (data not shown). In men, this expected increase was close to the observed 2-cm increase, but in women, the expected increase was substantially smaller than the 4-cm increase that was observed.
Figure 2 shows mean (95% CI) differences in waist circumference from 1999 to 2000 (the referent category in the regression model) through each subsequent study after controlling for race and age (gray points). In men, the mean waist circumference increased until 2005–2006 but was subsequently stable, whereas the mean increase in women was generally monotonic. However, the inclusion of BMI as an additional predictor of waist circumference (triangles and dashed CIs) greatly reduced the differences in men and resulted in BMI-adjusted waist-circumference changes that ranged from −0.4 (in 2009–2010) to 0.7 cm (2003–2004) relative to those in 1999–2000. However, in women, BMI-independent increases of 0.6 (2001–2002) to 2.5 cm (2011–2012) were observed. We also obtained very similar results in analyses that were based on multiple imputation of missing waist-circumference data; all BMI-adjusted waist circumference differences differed <0.05 cm between nonimputed and imputed data.
As assessed by the areas between the x = 0 line and lines connecting either unadjusted or adjusted estimates in Figure 2, we estimated that controlling for BMI accounted for 89% of the increase in mean waist circumference in men during this period. (The AUC obtained by integration was 17 cm × year for the model that did not control for BMI, whereas the BMI-adjusted area was 2.) In women, the comparable percentage reduction was 21%. Additional regression models that incorporated a single term rather than a categorical variable for study year indicated that the linear trend in waist circumference over the period was significant in women (β = 0.20/y, P < 0.001), but not men (β = −0.01/y, P = 0.40). As assessed by a sex × year interaction term in a model that contained both men and women, the male-female difference in BMI-adjusted waist circumference change over the 12-y period was significant at the 0.0001 level. Note that we found very similar results when waist circumference was adjusted for weight rather than BMI; controlling for weight almost eliminated the secular trend in waist circumference in men but accounted for only ~25% of the trend in women (data not shown).
Additional analyses in women indicated that secular increases in BMI-adjusted waist circumference decreased with age (P-age × year interaction term < 0.001). Figure 3 shows mean (95% CI) increases in BMI-adjusted waist circumference over the 12-y period in women who were 20–39 y of age (solid triangles and CIs) and those who were ≥60 y of age (open triangles and dashed CIs). Although there was no difference between the 2 age groups in 2001–2002 (mean waist circumference increases of 0.8 cm), subsequent levels differed substantially. For example, the mean, BMI-adjusted increase in waist circumference in 2011–2012 was ~75% larger in younger women (3.2 cm) than older women (1.8 cm). In contrast to this interaction with age, there was no evidence that secular changes in waist circumference differed in NH white, NH black, and Mexican American women (P-interaction term = 0.70).
We examined whether secular increases in the prevalence of abdominal obesity on the basis of waist-circumference cutoffs >102 cm (in men) and >88 cm (in women) could be attributed to changes in BMI (Figure 4). In Figure 4, circles (solid lines) represent RRs (corresponding CIs) in each 2-y period compared with 1999–2000 after controlling for race-ethnicity and age, and open triangles (and dotted lines) represent RRs after further controlling for BMI.
Over the 12-y study period, the prevalence of abdominal obesity increased from ~36% to 44% in men and 55% to 66% in women. After controlling for race and age, RRs from 2003–2004 through 2011–2012 (compared with in 1999–2000) varied from 1.15 to 1.20 in men and 1.06 to 1.17 in women. Additional control for BMI indicated that almost all of the increase in abdominal obesity in men was attributable to BMI across studies, with BMI-adjusted RRs ranging from 1.0 to 1.06. In women, adjustment for BMI had little effect on RR estimates from 2001–2002 through 2005–06, but RRs in the more-recent cycles were reduced by 20–30%. This sex difference, as assessed by a sex × year interaction term in the model, was significant at the 0.0001 level.
DISCUSSION
Our results indicated that, although waist circumference has increased by ~2 cm (in men) and ~4 cm (women) cm in adults in the US since 1999–2000, the increase in men was close to what would be expected because of the 0.7 increase in mean BMI over the 12-y period. However, in women, most of the secular increase in waist circumference was independent of changes in BMI, age, and race-ethnicity. After we controlled for race, age, and BMI from 1999–2000 through 2011–2012, the independent, secular increases in waist circumference were 0.2 cm (in men) and 2.4 cm (in women); only the latter result was significant. Note that, although our analyses focused on BMI, we also found that adjustment for weight accounted for almost all of the secular increase in waist circumference in men. This finding may have been because there was very little change in the height of adults in the United States from 1999–2000 through 2011–2012.
Several studies have reported secular increases in waist circumference in both men and women in the United States (16–20) and other countries (37–42). Because of the strong correlation between BMI and waist circumference (r ~ 0.9), it was somewhat surprising that most of the secular increase in waist circumference in women in the current study was independent of changes in BMI. However, there is some evidence that the correlation between longitudinal changes in BMI and those in waist circumference are weaker than are cross-sectional correlations. For example, over a 5-y period, the correlation between weight change and waist circumference change was r ~ 0.70 in Australian adults (38). This longitudinal study also showed that, although the annual rate of weight gain was greater between 1999 and 2004 than between 2004 and 2011, the rate of waist circumference increase was slightly larger in the second period (38).
Relatively few of these investigators have attempted to determine whether secular trends in waist circumference are independent of BMI, and a recent study of waist-circumference trends in NHANES (22) did not consider the effects of changes in BMI. However, some investigators concluded that waist-circumference changes that have occurred between 1959–1962 (23) or 1988–1994 (17, 20) and more-recent NHANES cycles were, at least in part, independent of BMI. It was also concluded that there have been larger increases in waist circumference than BMI in adults in other countries (21). We showed that trends in waist circumference from 1999–2000 through 2011–2012 were largely independent of those in BMI in women but not men. Furthermore, we showed that the largest secular increases in women occurred in 20- to 39-y-olds (P-age × year interaction < 0.001). The differing time periods and statistical methods across studies likely accounted for these differing conclusions.
For example, it may be problematic to combine waist-circumference data from the recent NHANES cycles with data from National Health and Examination Survey (NHES) I (1959–1962) (23) because measurement protocols differed. Although more-recent NHANES studies measured waist circumference just above the ilium (26), the location in the NHES-I was midway between the iliac crest and lower edge of the rib cage (43). The measurement at the superior border of the iliac crest was shown to be up to 1.7 cm greater in men and up to 5.6 cm greater in women than the midway measurements (44, 45). This effect could have been further increased in regression models because the much-earlier data from the NHES-I would have had high leverage (influence) on estimates. It should also be noted that, although Walls et al. (20) emphasized 0.72-cm (in men) and 0.79-cm (in women) increase in BMI-adjusted waist circumference between 1988–94 and 2005–2006, there was no mention that adjustment for BMI accounted for most of the ~5-cm (age-adjusted) increase in waist circumference over this period.
Several possible explanations were proposed for the observed trends in waist circumference (20, 23), including changes in energy take, distribution of race-ethnicity, and prevalence of endocrine disruptors, physical activity, polycystic ovary syndrome (46), use of antiobesity treatments (47, 48), certain depressive symptoms (49), use of antidepressants (50), sleep deprivation, and weight cycling. Furthermore, Björntorp (24) proposed that abdominal obesity is associated with a wide range of stress reactions, including various psychosocial and depressive traits. However, to account for the trends in waist circumference observed in the current study, it would have been necessary for a characteristic to 1) have a preferential influence on abdominal, rather than generalized, obesity, 2) have a greater effect in women, particularly those <40 y of age, than men, and 3) have a sufficiently high prevalence so that it would result in population-level changes. It is uncertain if any of the postulated factors could meet these conditions. An additional complication in identifying the explanatory factor was that the relation of this characteristic to abdominal obesity is likely to be much weaker than is the association between BMI and waist circumference.
There were several limitations of the current study that should be considered in the interpretation of our results. Of eligible persons included in the analyses, 1339 (3.3%) were missing data for waist circumference, and we showed that the probability of missingness was related to BMI and other characteristics. However, analyses based on multiple imputation yielded results that were almost identical to those observed by simply excluding missing data. In addition, because we wanted to examine recent trends in waist circumference, our results may not be applicable to trends over longer periods. Because the more-recent NHANES cycles measured waist circumference just above the iliac, our results also apply only to this location, which has been characterized as being technically difficult to measure (51). This measurement difficulty may, at least in part, account for why Bozeman et al. (52) showed that simple sex-specific equations could predict waist circumference very accurately, but prediction errors were much greater in women than men (3.9 compared with 0.3 cm) when the equations were applied to an external sample.
In conclusion, our results indicate that, in men, both BMI and waist circumference responded similarly over time to various environmental and lifestyle characteristics that have resulted in both characteristics having increased since 1999–2000. However, in women, mean waist circumference and the prevalence of abdominal obesity have increased substantially more than would be expected on the basis of changes in BMI. Our results suggest that it is possible that the adverse effects of secular trends in obesity, particularly in women, may be underestimated by using only BMI.
Supplementary Material
Acknowledgments
We thank Brian K Kit, National Center for Health Statistics, CDC, Hyattsville, MD, for assistance.
Footnotes
From the Divisions of Nutrition, Physical Activity, and Obesity (DSF) and Adult and Community Health (ESF), CDC, Atlanta, GA.
The findings and conclusions in this report are those of the authors and do not necessarily represent the position of the CDC.
The authors reported no funding received for this study.
Supplemental Table 1 is available from the “Supplemental data” link in the online posting of the article and from the same link in the online table of contents at http://ajcn.nutrition.org.
The authors’ responsibilities were as follows—DSF: analyzed data, wrote the manuscript, and had primary responsibility for the content of manuscript; and ESF: analyzed data and wrote parts of the manuscript. Neither author had a conflict of interest.
References
- 1.Ogden CL, Carroll MD, Kit BK, Flegal KM. Prevalence of childhood and adult obesity in the United States, 2011–2012. JAMA. 2014;311:806–14. doi: 10.1001/jama.2014.732. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.National Center for Health Statistics (NCHS) Health, United States, 2011: with special feature on socioeconomic status and health. Hyattsville (MD): National Center for Health Statistics; 2012. [PubMed] [Google Scholar]
- 3.Flegal KM, Carroll MD, Kit BK, Ogden CL. Prevalence of obesity and trends in the distribution of body mass index among US adults, 1999–2010. JAMA. 2012;307:491–7. doi: 10.1001/jama.2012.39. [DOI] [PubMed] [Google Scholar]
- 4.Flegal KM, Carroll MD, Ogden CL, Curtin LR. Prevalence and trends in obesity among US adults, 1999–2008. JAMA. 2010;303:235–41. doi: 10.1001/jama.2009.2014. [DOI] [PubMed] [Google Scholar]
- 5.Sun Q, Van Dam RM, Spiegelman D, Heymsfield SB, Willett WC, Hu FB, van Dam RM. Comparison of dual-energy x-ray absorptiometric and anthropometric measures of adiposity in relation to adiposity-related biologic factors. Am J Epidemiol. 2010;172:1442–54. doi: 10.1093/aje/kwq306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Hariri AA, Oliver NS, Johnston DG, Stevenson JC, Godsland IF. Adiposity measurements by BMI, skinfolds and dual energy X-ray absorptiometry in relation to risk markers for cardiovascular disease and diabetes in adult males. Dis Markers. 2013;35:753–64. doi: 10.1155/2013/763907. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Steinberger J, Jacobs DR, Raatz S, Moran A, Hong CP, Sinaiko AR. Comparison of body fatness measurements by BMI and skinfolds vs dual energy X-ray absorptiometry and their relation to cardiovascular risk factors in adolescents. Int J Obes (Lond) 2005;29:1346–52. doi: 10.1038/sj.ijo.0803026. [DOI] [PubMed] [Google Scholar]
- 8.Després JP, Lemieux I, Bergeron J, Pibarot P, Mathieu P, Larose E, Rodes-Cabau J, Bertrand OF, Poirier P. Abdominal obesity and the metabolic syndrome: contribution to global cardiometabolic risk. Arterioscler Thromb Vasc Biol. 2008;28:1039–49. doi: 10.1161/ATVBAHA.107.159228. [DOI] [PubMed] [Google Scholar]
- 9.Klein S, Allison DB, Heymsfield SB, Kelley DE, Leibel RL, Nonas C, Kahn R. Waist Circumference and Cardiometabolic Risk: a Consensus Statement from Shaping America’s Health: Association for Weight Management and Obesity Prevention; NAASO, the Obesity Society; the American Society for Nutrition; and the American Diabetes Associat. Obesity (Silver Spring) 2007;15:1061–7. doi: 10.1038/oby.2007.632. [DOI] [PubMed] [Google Scholar]
- 10.Wormser D, Kaptoge S, Di Angelantonio E, Wood AM, Pennells L, Thompson A, Sarwar N, Kizer JR, Lawlor DA, Nordestgaard BG, et al. Separate and combined associations of body-mass index and abdominal adiposity with cardiovascular disease: collaborative analysis of 58 prospective studies. Lancet. 2011;377:1085–95. doi: 10.1016/S0140-6736(11)60105-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Nyamdorj R, Qiao Q, Lam TH, Tuomilehto J, Ho SY, Pitkäniemi J, Nakagami T, Mohan V, Janus ED, Ferreira SRG. BMI compared with central obesity indicators in relation to diabetes and hypertension in Asians. Obesity (Silver Spring) 2008;16:1622–35. doi: 10.1038/oby.2008.73. [DOI] [PubMed] [Google Scholar]
- 12.de Hollander EL, Bemelmans WJ, Boshuizen HC, Friedrich N, Wallaschofski H, Guallar-Castillón P, Walter S, Zillikens MC, Rosengren A, Lissner L, et al. The association between waist circumference and risk of mortality considering body mass index in 65- to 74-year-olds: a meta-analysis of 29 cohorts involving more than 58 000 elderly persons. Int J Epidemiol. 2012;41:805–17. doi: 10.1093/ije/dys008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kodama S, Horikawa C, Fujihara K, Heianza Y, Hirasawa R, Yachi Y, Sugawara A, Tanaka S, Shimano H, Iida KT, et al. Comparisons of the strength of associations with future type 2 diabetes risk among anthropometric obesity indicators, including waist-to-height ratio: a meta-analysis. Am J Epidemiol. 2012;176:959–69. doi: 10.1093/aje/kws172. [DOI] [PubMed] [Google Scholar]
- 14.Carmienke S, Freitag MH, Pischon T, Schlattmann P, Fankhaenel T, Goebel H, Gensichen J. General and abdominal obesity parameters and their combination in relation to mortality: a systematic review and meta-regression analysis. Eur J Clin Nutr. 2013;67:573–85. doi: 10.1038/ejcn.2013.61. [DOI] [PubMed] [Google Scholar]
- 15.National Heart Lung and Blood Institute, National Institutes of Health (NIH) National Heart, Lung, and Blood Institute N. Clinical guidelines on the identification, evaluation, and treatment of overweight and obesity in adults: executive summary. Expert Panel on the Identification, Evaluation, and Treatment of Overweight in Adults. Am J Clin Nutr. 1998;68(4):899–917. doi: 10.1093/ajcn/68.4.899. [DOI] [PubMed] [Google Scholar]
- 16.Li C, Ford ES, McGuire LC, Mokdad AH. Increasing trends in waist circumference and abdominal obesity among US adults. Obesity (Silver Spring) 2007;15:216–24. doi: 10.1038/oby.2007.505. [DOI] [PubMed] [Google Scholar]
- 17.Ford ES, Mokdad AH, Giles WH. Trends in waist circumference among U.S. adults. Obes Res. 2003;11:1223–31. doi: 10.1038/oby.2003.168. [DOI] [PubMed] [Google Scholar]
- 18.Ford ES, Li C, Zhao G, Tsai J. Trends in obesity and abdominal obesity among adults in the United States from 1999–2008. Int J Obes (Lond) 2011;35:736–43. doi: 10.1038/ijo.2010.186. [DOI] [PubMed] [Google Scholar]
- 19.Okosun IS, Chandra KMD, Boev A, Boltri JM, Choi ST, Parish DC, Dever GEA. Abdominal adiposity in U.S. adults: prevalence and trends, 1960–2000. Prev Med. 2004;39:197–206. doi: 10.1016/j.ypmed.2004.01.023. [DOI] [PubMed] [Google Scholar]
- 20.Walls HL, Stevenson CE, Mannan HR, Abdullah A, Reid CM, McNeil JJ, Peeters A. Comparing trends in BMI and waist circumference. Obesity (Silver Spring) 2011;19:216–9. doi: 10.1038/oby.2010.149. [DOI] [PubMed] [Google Scholar]
- 21.Visscher TL, Heitmann BL, Rissanen A, Lahti-Koski M, Lissner L. A break in the obesity epidemic? Explained by biases or misinterpretation of the data? Int J Obes (Lond) doi: 10.1038/ijo.2014.98. Epud ahead of print 2014 Jun 9. [DOI] [PubMed] [Google Scholar]
- 22.Ford ES, Maynard LM, Li C. Trends in mean waist circumference and abdominal obesity among US adults, 1999–2012. JAMA. 2014;312:1151–3. doi: 10.1001/jama.2014.8362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Elobeid MA, Desmond RA, Thomas O, Keith SW, Allison DB. Waist circumference values are increasing beyond those expected from BMI increases. Obesity (Silver Spring) 2007;15:2380–3. doi: 10.1038/oby.2007.282. [DOI] [PubMed] [Google Scholar]
- 24.Björntorp P. Do stress reactions cause abdominal obesity and comorbidities? Obes Rev. 2001;2:73–86. doi: 10.1046/j.1467-789x.2001.00027.x. [DOI] [PubMed] [Google Scholar]
- 25.Centers for Disease Control and Prevention (CDC) National Center for Health Statistics: National Health and Nutrition Examination Survey data. 2012 [cited 2014 Feb 3]. Available from: http://www.cdc.gov/nchs/nhanes/nhanes_questionnaires.htm.
- 26.National Center for Health Statistics (NCHS) Anthropometry procedures manual. National Health and Nutrition Examination Survey (NHANES); 2011. [cited 2014 Feb 3]. Available from: http://www.cdc.gov/nchs/data/nhanes/nhanes_11_12/Anthropometry_Procedures_Manual.pdf. [Google Scholar]
- 27.R Core Team. R: a language and environment for statistical computing Vienna (Austria): R Foundation for Statistical Computing. 2014 [cited 2014 Dec 29]. Available from: http://www.r-project.org/
- 28.Lumley T. Analysis of complex survey samples. Hoboken (NJ): John Wiley & Sons; 2010. [Google Scholar]
- 29.National Center for Health Statistics (NCHS) How to generate age-adjusted prevalence rates and means in SUDAAN. [cited 2014 May 8]. Available from: http://www.cdc.gov/nchs/tutorials/NHANES/NHANESAnalyses/AgeStandardization/Task1a.htm.
- 30.Harrell FE. Regression modeling strategies: with applications to linear models, logistic regression, and survival analysis. New York: Springer; 2001. [Google Scholar]
- 31.Zou G. A modified Poisson regression approach to prospective studies with binary data. Am J Epidemiol. 2004;159:702–6. doi: 10.1093/aje/kwh090. [DOI] [PubMed] [Google Scholar]
- 32.Yelland LN, Salter AB, Ryan P. Performance of the modified Poisson regression approach for estimating relative risks from clustered prospective data. Am J Epidemiol. 2011;174:984–92. doi: 10.1093/aje/kwr183. [DOI] [PubMed] [Google Scholar]
- 33.Lumley T, Kronmal R. UW Biostatistics Working Paper Series: relative risk regression in medical research: models, contrasts, estimators, and algorithms. 2006 [cited 2014 Dec 29]. Available from: http://biostats.bepress.com/uwbiostat/paper293.
- 34.Zeileis A, Kleiber C, Jackman S. Regression models for count data in R. 2008 [cited 7 Aug 2014]. Available from: http://cran.r-project.org/web/packages/pscl/vignettes/countreg.pdf.
- 35.Honaker J, King G, Blackwell M. AMELIA II. a program for missing data. J Stat Softw [Internet]. [cited 38 Jul 2013] 2011;45:1–47. Available from: http://cran.r-project.org/package=Amelia. [Google Scholar]
- 36.Little RJA, Rubin DB. Statistical analysis with missing data. 2nd. Hoboken (NJ): John Wiley & Sons; 2002. [Google Scholar]
- 37.Howel D. Trends in the prevalence of abdominal obesity and overweight in English adults (1993–2008) Obesity (Silver Spring) 2012;20:1750–2. doi: 10.1038/oby.2011.127. [DOI] [PubMed] [Google Scholar]
- 38.Peeters A, Magliano DJ, Backholer K, Zimmet P, Shaw JE. Changes in the rates of weight and waist circumference gain in Australian adults over time: a longitudinal cohort study. BMJ Open. 2014;4:e003667. doi: 10.1136/bmjopen-2013-003667. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Xi B, Liang Y, He T, Reilly KH, Hu Y, Wang Q, Yan Y, Mi J. Secular trends in the prevalence of general and abdominal obesity among Chinese adults, 1993–2009. Obes Rev. 2012;13:287–96. doi: 10.1111/j.1467-789X.2011.00944.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Wardle J, Boniface D. Changes in the distributions of body mass index and waist circumference in English adults, 1993/1994 to 2002/2003. Int J Obes (Lond) 2008;32:527–32. doi: 10.1038/sj.ijo.0803740. [DOI] [PubMed] [Google Scholar]
- 41.Lahti-Koski M, Harald K, Männistö S, Laatikainen T, Jousilahti P. Fifteen-year changes in body mass index and waist circumference in Finnish adults. Eur J Cardiovasc Prev Rehabil. 2007;14:398–404. doi: 10.1097/HJR.0b013e32800fef1f. [DOI] [PubMed] [Google Scholar]
- 42.Visscher TLS, Seidell JC. Time trends (1993–1997) and seasonal variation in body mass index and waist circumference in the Netherlands. Int J Obes Relat Metab Disord. 2004;28:1309–16. doi: 10.1038/sj.ijo.0802761. [DOI] [PubMed] [Google Scholar]
- 43.National Center for Health Statistics (NCHS) National Health Examination Survey 1959–62. Public use data tape documentation; physical measurements I, tape number 1003. [cited 26 Mar 2014]. Available from: http://www.cdc.gov/nchs/data/nhanes/nhes123/1003.pdf.
- 44.Ma W-Y, Yang C-Y, Shih S-R, Hsieh H-J, Hung CS, Chiu F-C, Lin M-S, Liu P-H, Hua C-H, Hsein Y-C, et al. Measurement of waist circumference: midabdominal or iliac crest? Diabetes Care. 2013;36:1660–6. doi: 10.2337/dc12-1452. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Bosy-Westphal A, Booke C-A, Blöcker T, Kossel E, Goele K, Later W, Hitze B, Heller M, Gluer C-C, Müller MJ. Measurement site for waist circumference affects its accuracy as an index of visceral and abdominal subcutaneous fat in a Caucasian population. J Nutr. 2010;140:954–61. doi: 10.3945/jn.109.118737. [DOI] [PubMed] [Google Scholar]
- 46.Carmina E, Bucchieri S, Esposito A, Del Puente A, Mansueto P, Orio F, Di Fede G, Rini G. Abdominal fat quantity and distribution in women with polycystic ovary syndrome and extent of its relation to insulin resistance. J Clin Endocrinol Metab. 2007;92:2500–5. doi: 10.1210/jc.2006-2725. [DOI] [PubMed] [Google Scholar]
- 47.Aydin N, Topsever P, Kaya A, Karasakal M, Duman C, Dağar A. Orlistat, sibutramine, or combination therapy: which performs better on waist circumference in relation with body mass index in obese patients? Tohoku J Exp Med. 2004;202:173–80. doi: 10.1620/tjem.202.173. [DOI] [PubMed] [Google Scholar]
- 48.Gokcel A, Gumurdulu Y, Karakose H, Melek Ertorer E, Tanaci N, Bascil Tutuncu N, Guvener N. Evaluation of the safety and efficacy of sibutramine, orlistat and metformin in the treatment of obesity. Diabetes Obes Metab. 2002;4:49–55. doi: 10.1046/j.1463-1326.2002.00181.x. [DOI] [PubMed] [Google Scholar]
- 49.Dunbar JA, Reddy P, Davis-Lameloise N, Philpot B, Laatikainen T, Kilkkinen A, Bunker SJ, Best JD, Vartiainen E, Kai Lo S, et al. Depression: an important comorbidity with metabolic syndrome in a general population. Diabetes Care. 2008;31:2368–73. doi: 10.2337/dc08-0175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Ma Y, Balasubramanian R, Pagoto SL, Schneider KL, Hébert JR, Phillips LS, Goveas JS, Culver AL, Olendzki BC, Beck J, et al. Relations of depressive symptoms and antidepressant use to body mass index and selected biomarkers for diabetes and cardiovascular disease. Am J Public Health. 2013;103:e34–43. doi: 10.2105/AJPH.2013.301394. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Wang J, Thornton JC, Bari S, Williamson B, Gallagher D, Heymsfield SB, Horlick M, Kotler D, Laferrere B, Mayer L, et al. Comparisons of waist circumferences measured at 4 sites. Am J Clin Nutr. 2003;77:379–84. doi: 10.1093/ajcn/77.2.379. [DOI] [PubMed] [Google Scholar]
- 52.Bozeman SR, Hoaglin DC, Burton TM, Pashos CL, Ben-Joseph RH, Hollenbeak CS. Predicting waist circumference from body mass index. BMC Med Res Methodol. 2012;12:115. doi: 10.1186/1471-2288-12-115. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


