Abstract
Objective
To examine the relationship between job type, weight status and lifestyle factors that are potential contributors to obesity including, diet, physical activity and perceived stress among employees enrolled in the Working on Wellness (WOW) project.
Methods
Randomly selected employees at 24 worksites completed a baseline survey (n=1700); some also an in-person survey and anthropometric measures (n=1568). Employees were classified by US Labor standards as: white collar (n=1297), blue collar (n=303), or service worker (n=92), 8 unknown. Associations were analyzed using Chi-Square, GLM procedures, and adjusted for demographics using Logistic Regression.
Results
In unadjusted models, BMI of service workers was higher than white collar workers; F&V intake was higher for service and blue collar than white collar; white collar workers reported highest stress levels in job and life. However, in models adjusted for demographics, the only significant difference was to physical activity (i.e., MET/min per week), with blue collar workers reporting higher levels of physical activity than service workers, who reported higher levels than the white collar workers.
Conclusions
Future research should further examine the relationship between health and job status to corroborate the results of the current study and to consider designing future worksite health promotion interventions that are tailored by job category.
Keywords: Occupation, worksite, weight status, diet, physical activity, stress
Introduction
Obesity continues to be a significant public health issue in the United States with about one-third (33.8%) of adults categorized as obese in 2007–2008.1 The number of obese adults has doubled from 1980 through 2008; with substantial increases in obesity for all groups across age, sex, race, ethnicity, socioeconomic status, and education levels, and geographic regions.2, 3 This trend has profound implications for public health costs, resulting in significant medical, emotional, social and monetary health burden, individually, nationally and even globally.4 Additionally, obesity can cause or exacerbate type 2 diabetes mellitus, dyslipidemia, hypertension, cardiovascular disease, certain cancers, osteoarthritis, respiratory complications, reproductive issues, and depression and can also decrease longevity.5–12
A public health threat of this magnitude requires intervention efforts on many levels. Interventions that address behavior change in the context of societal and environmental influences are feasible and have produced favorable outcomes, while highlighting the need to gain more insight into the impact of environment on obesity.13–16 To further this aim, the National Institutes of Health (in 2005) formulated a Strategic Plan for obesity research. The research goal of this plan was to prevent and treat obesity by lifestyle modification through behavioral and environmental methods, including interventions based at the worksite.17 The Centers for Disease Control Task Force on Community Preventive Services has also recommended combining nutrition and physical activity intervention strategies for controlling obesity in worksite settings.18
More than half (58.6%) of American adults are employed.19 Thus, the worksite offers an important opportunity as a venue for obesity prevention, as it provides access to working-age Americans who spend a significant amount of their time at work.20,21 Worksites have several inherent advantages for health promotion efforts including obesity prevention, such as: existing pre-defined communication channels and social networks,19 plus the potential for multi-level intervention through influence on worksite environment and policies as well as individual behavior. 20,21 Though the worksite is a promising setting for obesity prevention, obesity risk may not be homogeneous within worksites. Some researchers have found that certain work-related factors such as job stress, overnight and sedentary work may contribute to weight gain and abdominal fat accumulation.22, 23 However, little else is found in the literature regarding this issue. According to Caban et al. more investigation is urgently needed to examine the relationship between obesity, occupation and weight loss intervention programs targeting workers employed in occupational groups with high or increasing rates of obesity.24 This view is reinforced by Schulte P et al.,23 who state that little research has examined the effects of occupational status and work conditions (including organizational factors) on BMI.
Objective
The purpose of this study is to examine the relationship between job type (blue collar vs. white collar vs. service workers), weight status and lifestyle factors that are potential contributors to obesity including, diet, physical activity and perceived stress among employees enrolled in the Working on Wellness (WOW) project. WOW is a group-randomized trial in 24 worksites in southern New England studying the cost-effectiveness of a multilevel weight gain prevention intervention. The analysis by job type will provide important data to guide the development of future worksite wellness programs to improve employee health.
Methods
Design
The present analysis is from the baseline data collected for the WOW group-randomized trial. To participate in WOW, worksites needed to: be located within 60 miles of Providence, RI and have 150 or more permanent employees located within one facility having an onsite cafeteria and/or food vending services. Prior to randomization, worksites were matched into pairs according to size of employee population and type of business (e.g., health/medical services; manufacturing, research and development, etc.). A total of 24 worksites participated in the WOW study.
We established an “evaluation cohort” of approximately 70 employees per worksite to assess employee baseline and follow-up characteristics and the effect of treatment. We utilized a voluntary “opt-out” employee consent procedure combined with random selection to establish the ‘cohort’ at each site. These procedures were chosen to enable recruitment of a more representative sample at each worksite than would be achieved by simply asking for volunteers. All employees at a site were notified via a personalized form letter delivered to them at the worksite that they had 10 days to notify us via calling a toll-free number or placing their form in a drop-box placed at worksite of their decision to opt-out from inclusion in the cohort. Any employees who did not “opt out” were eligible to be randomly selected for screening into the evaluation cohort. We utilized a random integer generator process25 to randomly select a representative sample for the evaluation cohort from remaining employees after the opt-out deadline. We contacted members of the selected sample to tell them more about WOW’s evaluation component, and if they agreed, to determine their eligibility to participate in the evaluation cohort.
Evaluation cohort participants were eligible if they were aged 18 or older, not pregnant, able to speak and read English, as well as walk for exercise. Brown University Institutional Review Board approved the study. Informed consent was obtained for all employee participants prior to study enrollment. Employees were offered the choice of completing the baseline survey on the telephone or online. Participants who completed a baseline survey were subsequently scheduled for a meeting at the worksite to undergo anthropometric measures and to complete an additional self-administered questionnaire. The goal was to have an average of 70 employees per company enroll in the evaluation cohort and complete all baseline measurements. Employees were contacted for follow-up measures 12 months and 24 months after baseline.
After the baseline measurement period, worksites were then randomly assigned to receive either a 24-month weight gain prevention or a generic wellness comparison intervention. Worksites randomly assigned to the intervention arm received educational and environmental interventions related to weight management, nutrition and physical activity and worksites in the comparison arm received interventions related to stress management, injury prevention, financial wellness, food safety and back care. All employees were invited to participate in intervention activities (not just the employees in the evaluation cohort) and evaluation cohort participants were not required to participate. Only the baseline data collected for this study were used in the current analysis.
Measures used for the present study
Body Mass Index (BMI)
Weight was measured on a calibrated portable electronic scale (model BWB-800 Tanita) to the nearest 0.1 pound. Height was measured with a portable stadiometer (model 214 Seca) to the nearest eighth-inch increment. Both weight and height were measured twice, with a third measure taken if the difference was equal to or greater than one-half pound or one-quarter inch, respectively. Final weight and height values were calculated as the averages of the values, which were used to calculate BMI [weight (lb)/height (in) squared x 703]. A weight status variable was created using BMI based on CDC definitions as follows: underweight {<18.5), normal (18.5 – 24.9), overweight (25.0 – 29.9) or obese (≥ 30.0).25 BMI values calculated at > 40 were excluded from analyses.
Nutrition and Physical Activity
Dietary intake measures included validated National Cancer Institute (NCI) questionnaires to measure fruit and vegetable (F&V) (NCI By-Meal Screener) as well as fat consumption (NCI Fat Screener). The F&V screener is comprised of 14 items that assess consumption of fruits and vegetables other than salad and potatoes during past month by time of day, frequency, and amount.27, 28 The fat screener uses 17 variables regarding frequency of foods eaten by month, during past 12 months, to assess percent energy from fat.29, 30 The validated International Physical Activity Questionnaire short form was used to assess self-reported physical activity.31 Participants were asked to respond to questions about frequency in the past seven days and duration in minutes of participation in leisure, home and yard, occupation, transportation and exercise-related physical activities across four levels of intensity: sitting, low, moderate intensity and vigorous-intensity. Physical activity is calculated as a product of intensity, (measured by metabolic equivalents), duration (minutes of participation) and frequency (number of events per week) summed across the four types of intensities and expressed as metabolic equivalent-minutes per week (MET-min/continuous).
Perceived Stress and Demographics
Perceived stress level of the participant’s job and life were measured by asking participants to rate job and life stress (one question for each type) on a 10-point Likert scale from 0 (not at all stressful) to 10 (extremely stressful) using a question adapted from the Blue Cross Blue Shield of RI Personal Health Assessment. Demographic questions included gender, age, marital status, level of education obtained, annual household income, race and ethnicity.
Occupation/job-type
Respondents were asked to classify their job into one of the following categories: science/technical, manual, professional/managerial, machine operator, clerical/office/sales, service worker, other. These responses were then later categorized as: white collar, blue collar or service worker according to the Bureau of Labor Statistics.32 Examples of each category are: service worker (i.e. health and nurses’ aides, orderlies, cooks and kitchen workers); blue collar (i.e. machine operators, packers, assemblers, construction workers); and white collar (i.e. engineers, sales, registered nurses, office managers).
Analyses
Initial Chi Square tests were used to compare job category with demographic characteristics (age, education, race, gender, ethnicity, employment status, household income, and marital status). Continuous variables (age, BMI), were also assessed using ANOVA models. To further identify possible confounding relationships, ANOVA models were constructed with the outcome variables (BMI, F&V intake, percent energy from fat, physical activity, and stress in life and in the work place) as the dependent variable, and job category as the independent variable. The potential confounding variables were identified for each outcome as demographic characteristics associated with both the outcome and the job category variable. Site was included in each model to adjust for any organizational level differences. Outcome measures were assessed by job category initially using simple ANOVA models. Subsequently, we constructed adjusted linear models including all potential confounders as identified above. All analyses were performed using SAS version 9.2 (SAS Institute, Cary, NC).
Results
The 24 worksites enrolled in WOW included eight that provided health/medical services; eight manufacturing (jewelry, textile manufacture, ship building), five research and development, and three call centers and production/assembly worksites. Overall an average of 12% of employees opted out from participation in the evaluation cohort (1211 out of 9895 total employees). A total of 1,700 employees completed the baseline survey, of whom 1,568 (92%) additionally completed the baseline in-person self-administered questionnaire and anthropometric measures (see Table 1). The baseline sample population (Table 2) included mostly women (59.5%), full time employees (90%), non-Hispanic (94%) and of white race (85%). Two-thirds were married or had a domestic partner, almost half (49%) were college graduates or had post-college education, more than one-fourth (27.6%) had household income of $100,001 or more, and about 40% have income $50,001 – $100,000. Mean age of the cohort was 45 years and mean BMI was 28.4 with 72% overweight/obese. More than three-fourths (76.3%) were categorized as white-collar workers, with 17.8% and 5.5% categorized as blue collar and service workers, respectively (Table 1).
Table 1.
Worksites in the WOW study and number (and percentage) of employees in random evaluation cohort
| Worksite Pair # | Worksite Assignment | Worksite Type | Total # of Employees | # Opted Out | % Opted Out | Randomly Selected Sample | # Baseline Phone Surveys | % total Employee Pop. | # Baseline In-Person Surveys | % total Employee Pop. |
|---|---|---|---|---|---|---|---|---|---|---|
| 1 | Intervention | Manufacturing | 430 | 11 | 3% | 178 | 43 | 10% | 34 | 8% |
| Comparison | Manufacturing | 356 | 77 | 22% | 238 | 40 | 11% | 38 | 11% | |
| 2 | Intervention | Manufacturing | 148 | 65 | 44 | 88 | 53 | 36% | 52 | 35% |
| Comparison | Manufacturing | 127 | 31 | 24% | 96 | 47 | 37% | 44 | 35% | |
| 3 | Intervention | Research & design/mfg | 291 | 50 | 17% | 213 | 97 | 33% | 96 | 33% |
| Comparison | Call center/mfg | 329 | 93 | 28% | 226 | 103 | 31% | 100 | 30% | |
| 4 | Intervention | Shipbuilding | 244 | 17 | 7% | 183 | 77 | 32% | 76 | 31% |
| Comparison | Manufacturing | 249 | 81 | 33% | 166 | 68 | 27% | 63 | 25% | |
| 5 | Intervention | Research & design/mfg | 487 | 41 | 8% | 261 | 98 | 20% | 91 | 19% |
| Comparison | Research & design/mfg | 515 | 55 | 11% | 285 | 66 | 13% | 65 | 13% | |
| 6 | Intervention | Medical/health care | 295 | 17 | 6% | 267 | 57 | 19% | 47 | 16% |
| Comparison | Research & design/mfg | 361 | 35 | 10% | 248 | 91 | 25% | 88 | 24% | |
| 7 | Intervention | Medical/health care | 728 | 72 | 10% | 317 | 106 | 15% | 86 | 12% |
| Comparison | Medical/health care | 1309 | 71 | 5% | 436 | 105 | 8% | 88 | 7% | |
| 8 | Intervention | Medical/health care | 333 | 36 | 11% | 236 | 88 | 26% | 79 | 24% |
| Comparison | Research & design/mfg | 433 | 27 | 6% | 250 | 86 | 20% | 86 | 20% | |
| 9 | Intervention | Manufacturing | 381 | 157 | 41% | 223 | 66 | 17% | 62 | 16% |
| Comparison | Manufacturing | 177 | 94 | 53% | 177 | 65 | 37% | 65 | 37% | |
| 10 | Intervention | Medical/health care | 1300 | 71 | 5% | 425 | 91 | 7% | 79 | 6% |
| Comparison | Medical/health care | 515 | 59 | 11% | 230 | 77 | 15% | 74 | 14% | |
| 11 | Intervention | Call center | 332 | 17 | 5% | 136 | 48 | 14% | 45 | 14% |
| Comparison | Call center | 135 | 20 | 15% | 133 | 52 | 39% | 46 | 34% | |
| 12 | Intervention | Medical/health care | 195 | 5 | 3% | 184 | 25 | 13% | 24 | 12% |
| Comparison | Medical/health care | 225 | 9 | 4% | 154 | 41 | 18% | 38 | 17% | |
| TOTALS | 9895 | 1211 | 12% | 5350 | 1690 | 17% | 1566 | 16% | ||
Note: Of the 5350 randomly chosen employees, 1638 (25.8%) were unable to be reached for registration surveys within the allotted time, 1196 (22.4%) refused and 288 (5.4%) were ineligible due to age, pregnancy, language, no longer at company, employment status, and health reasons. Of the 2216 who completed registration, 247 (11.2%) were unable to be reached for baseline surveys within the allotted time, 251 (11.3%) refused and 28 (1.3%) were ineligible due to language, no longer at company, or employment status. After subtracting those who were ineligible, 30.3% of the randomly selected sample completed all baseline measures. We reached our goal of an average of 70 employees per site.
Table 2.
Demographic characteristics: overall and by job category
| Variable | Category | All % (n) | White Collar % (n) | Blue Collar % (n) | Service Worker % (n) | p-value |
|---|---|---|---|---|---|---|
| Age Category | 18–34 | 20.5 (344) | 20.3 (269) | 18 (48) | 31.4 (27) | 0.0941 |
| 35–51 | 46.9 (788) | 46.6 (619) | 49.4 (132) | 43 (37) | ||
| 52+ | 32.7 (549) | 33.1 (440) | 32.6 (87) | 25.6 (22) | ||
| Gender | Male | 40.5 (681) | 37.6 (499) | 59.2 (158) | 27.9 (24) | <0.0001* |
| Female | 59.5 (1000) | 62.4 (829) | 40.8 (109) | 72.1 (62) | ||
| Employment Status | Full-time | 89.8 (1510) | 88.4 (1174) | 98.9 (264) | 83.7 (72) | <0.0001* |
| Part-time and Per Diem | 10.5 (171) | 11.6 (154) | 1.1 (3) | 16.3 (14) | ||
| Hispanic | Yes | 5.5 (92) | 2.9 (38) | 18.4 (49) | 5.9 (5) | <0.0001* |
| No | 94.5 (1580) | 97.1 (1283) | 81.6 (217) | 94.1 (80) | ||
| Race | White | 89.9 (1440) | 91.2 (1181) | 86.2 (193) | 80.5 (66) | <0.0001* |
| Black | 4.6 (74) | 3.7 (48) | 5.8 (13) | 15.9 (13) | ||
| Asian | 2.7 (43) | 2.6 (34) | 4 (9) | 0 (0) | ||
| Hawaiian | 0.2 (3) | 0.2 (2) | 0.4 (1) | 0 (0) | ||
| Native American | 1 (9) | 0.3 (4) | 1.3 (3) | 2.4 (2) | ||
| More than one race | 2 (32) | 2 (26) | 2.2 (5) | 1.2 (1) | ||
| Education Status | ≤HS | 20.7 (347) | 10 (132) | 65.9 (174) | 47.7 (41) | <0.0001* |
| Some post secondary educ | 30.2 (505) | 29.9 (395) | 26.9 (71) | 45.3 (39) | ||
| College grad/post grad | 49.1 (821) | 60.2 (796) | 7.2 (19) | 7 (6) | ||
| Income Status | ≤$50,000 | 28.5 (442) | 20.7 (252) | 56.9 (141) | 57.6 (49) | <0.0001* |
| $50,001–$100,000 | 41.4 (642) | 42.2 (514) | 38.7 (96) | 37.6 (32) | ||
| $100,001+ | 30.1 (466) | 37.1 (451) | 4.4 (11) | 4.7 (4) | ||
| Marital Status | Married/living w/domestic partner | 66.0 (1104) | 68 (900) | 58.7 (155) | 57 (49) | 0.0253* |
| Separated/divorced | 13.0 (217) | 12.2 (161) | 17 (45) | 12.8 (11) | ||
| Widowed | 1.8 (30) | 1.6 (21) | 2.7 (7) | 2.3 (2) | ||
| Never married | 19.3 (322) | 18.2 (241) | 21.6 (57) | 27.9 (24) | ||
| BMI | Underweight | 13 | 0.9 (11) | 0.8 (2) | 0 (0) | 0.0024* |
| Normal | 421 | 29.4 (363) | 19.5 (48) | 13 (10) | ||
| Overweight | 573 | 36 (444) | 39.8 (98) | 40.3 (31) | ||
| Obese | 550 | 33.7 (416) | 39.8 (98) | 46.8 (36) |
| Variable | Overall Mean (Std. Dev) (n) | White Collar Mean (Std. Dev) (n) | Blue Collar Mean (Std. Dev) (n) | Service Worker Mean (Std. Dev) (n) | P-value |
|---|---|---|---|---|---|
| Age (mean years) | 44.18 (12.21) (1681) | 45.27 (11.57)(1328) | 45.26 (11.07)(267) | 42.02 (14.00)(86) | 0.042* |
| BMI No Outliers (mean) | 29.60 (5.84)(1540) | 28.32 (5.77)(1219) | 29.75 (5.78)(244) | 30.73 (5.98)(77) | <0.0001* |
We found significant differences in gender, employment status, ethnicity, race, education, income and marital status by job categories (Table 1). Service workers were more likely to be young (18–34), female, part-time workers, never-married, and were also more likely to be obese or overweight when BMI was calculated with no outliers. Blue-collar workers were more likely to be male, Hispanic, full-time employed, but at lowest education and income level. White-collar workers mostly reported White race and highest educational and income level.
Associations among job category and weight status, diet, physical activity (PA) and stress are shown in Table 3. Discussion of each outcome measure and its relationship to job category follows.
Table 3.
Association of outcome variables with job category (blue collar, white collar, service worker) in unadjusted and adjusted ANOVA models.
| Job category (worker type) | |||||||
|---|---|---|---|---|---|---|---|
| Measure | White Collar (N=1328) | Blue Collar (N=267) | Service (N=86) | P-value | |||
| Unadjusted | |||||||
| mean | 95% CI | mean | 95% CI | mean | 95% CI | ||
| BMI (mean) | 28.8 | 28.40–29.19 | 29.6 | 28.71–30.47 | 30.2 | 28.75–31.68 | 0.0689 |
| F&V servings (no fries no juice) | 1.5 | 1.39–1.54 | 1.3 | 1.13–1.46 | 1.3 | 1.03–1.59 | 0.1569 |
| F&V servings (no fries with juice) | 3.0 | 2.82–3.12 | 3.4 | 3.04–3.72 | 3.1 | 2.55–3.68 | 0.1047 |
| Fat intake (% energy) | 31.1 | 30.82– 31.30 | 31.4 | 30.91– 31.99 | 31.2 | 30.27–32.05 | 0.4569 |
| PA activity - MET/min per week | 2,784 | 2,526–3,043 | 4812 | 4,238–5386 | 3687 | 2,745–4,629 | <0.0001*** |
| Stress level - life (mean of scale 0 – 10) | 6.0 | 5.90–6.19 | 5.5 | 5.14–5.78 | 5.3 | 4.75–5.78 | 0.0002** |
| Stress level - job (mean of scale 0 – 10) | 6.2 | 6.07–6.35 | 5.4 | 5.10–5.72 | 5.3 | 4.77–5.80 | <0.0001*** |
| Adjusted | |||||||
| mean | 95% CI | mean | 95% CI | mean | 95% CI | ||
| BMI (mean) | 29.5 | 27.94–31.07 | 29.5 | 27.65–31.26 | 30.0 | 27.85–32.18 | 0.8166 |
| F&V servings (no fries no juice) | 1.6 | 1.30–1.86 | 1.7 | 1.40–2.04 | 1.7 | 1.34–2.11 | 0.3585 |
| F&V servings (no fries with juice) | 4.9 | 4.17–5.59 | 5.4 | 4.63–6.17 | 5.2 | 4.26–6.04 | 0.0716 |
| Fat intake (% energy) | 31.0 | 29.98–32.01 | 30.7 | 29.53–31.84 | 30.4 | 29.07–31.78 | 0.4379 |
| PA activity - MET/min per week | 3,024 | 1,889–4,160 | 5,091 | 3,802–6,381 | 3,577 | 2,084–5,071 | <0.0001*** |
| Stress level - life (mean of scale 0 – 10) | 5.7 | 5.04–6.39 | 5.4 | 4.71–6.16 | 5.4 | 4.52–6.20 | 0.2499 |
| Stress level - job (mean of scale 0 – 10) | 5.4 | 4.66–6.11 | 5.2 | 4.38–5.95 | 5.0 | 4.09–5.87 | 0.2886 |
p<0.05
p<0.01
p<0.001
BMI adjusted for site, age, race, education, and income;
F&V Intake adjusted for site, age, gender, race, ethnicity, income and education;
Stress level adjusted for site, age, gender, ethnicity, race, income, education, and marital status;
Fat Intake adjusted for site, race, education, income, and marital status;
Physical Activity adjusted for site, race, education, income, and marital status
Body Mass Index and weight status
BMI was found in the initial models which did not include outliers to be highest among service workers (31 kg/m2), compared with blue (29.6 kg/m2) and white collar (28.3 kg/m2) workers; however, these difference were no longer significant after including outliers in the unadjusted model and the model with adjustment for demographics.
Fruit and vegetable intake
F&V intake (excluding fries and juice), was not different between workers of different job categories in either crude or adjusted models.
Fat intake
Fat intake (% energy from fat) was not significantly different between workers of different job categories in either crude or adjusted models.
Physical Activity
Service and blue-collar workers had the highest levels of physical activity (met-min/week), followed by white-collar workers, p<.0001, which remained after adjustment for demographics.
Perceived Stress
White collar workers reported significantly higher life and job stress compared to service and blue collar workers, who reported similar levels of stress in both categories. After adjustment for demographics, these associations persisted, but were no longer significant.
Discussion
Categorizing this study’s employee population by occupational category and then comparing measures of various health-related factors (obesity, PA, dietary intake of fat, F&V intake, stress) among them revealed some interesting associations. Each job category had lifestyle factors with potential for increased health risk; despite the fact that the occupational categories varied in size, the employees within each occupational category were distinct enough to warrant investigation. In unadjusted models, BMI of service workers was higher than white collar workers; F&V intake was higher for service and blue collar than white collar; white collar workers reported highest stress levels in job and life. However, in models adjusted for demographics, there was just a significant difference in reported physical activity (i.e., MET/min per week) by job category, with blue collar workers reporting higher levels of physical activity than service workers, who reported higher levels than the white collar workers. However, even though some of the differences we found by job category were attenuated with demographic adjustments, the data still highlights the fact that lifestyle interventions might need to be targeted to different groups by employment status.
Our findings lend support to several other studies. However, these studies did not adjust for demographic differences, as was done in the present study, and thus should be interpreted with that in mind. Prior to adjusting for demographic differences between job categories, we had found statistically significant differences in levels of physical activity and job and life stress. For example, with respect to obesity, similar to our results when we examined BMI with no outliers in the unadjusted sample, Ogden et al., found that the highest prevalence of obesity was present among service and manual/blue collar workers in a national sample; this study did not adjust for demographic differences.35 Similarly in a study with a large, nationally representative sample of US workers, Caban et al found that obesity rates rose in all worker groups by an average of almost 10% between the survey years 1986 and 2002, but that specific occupations (motor vehicle operators and service workers) had greater increases in and a higher prevalence of obesity.24 Niknian M et al compared health risk factors between female white and blue-collar workers and found blue collar workers to be at higher risk for certain controllable risk factors, including BMI.36 Furthermore, it has been shown that admission rates for obesity among hospital employees (many who were categorized as service workers) were 46% higher compared to the general population.37 Conversely, in a large study involving Hawaiian hotel employees, the highest prevalence of obesity and mean BMI was found among those in managerial and facility maintenance positions; this study did not adjust for demographic differences.38 Future studies should further examine occupations with high and lower prevalence of obesity to help further elucidate the relationship between occupation and body weight.24
Because long-term employment relationships are common and people tend to remain in the same occupation,39 targeting interventions to address risk disparities by job type could potentially improve the effectiveness of employee health promotion. Results from the current study and existing research in this area suggest that perhaps blue and service collar workers could benefit from interventions to control their weight, while worksite interventions aimed at white-collar workers may consider an emphasis on increasing PA levels and reducing stress.
Future longitudinal studies are needed to look at the effects of different interventions on changes in health-related and lifestyle outcomes by job status and whether interventions targeted by occupation are more effective than generic interventions. A few studies have found that health promotion interventions targeting blue-collar workers or manufacturing worksites were effective in smoking cessation,40 reducing fat intake,33, 41 and/or increasing F&V intake32 and strengthening and flexibility exercise,33 but more research is needed. Primary and secondary prevention of obesity in occupational settings must take into account the many societal and occupational factors that influence energy imbalance via multifaceted interventions (e.g., accountability of healthy food choices and food quantity, exercise programs).24
The current study extends the evidence regarding the association between job category and lifestyle characteristics, but nonetheless is not without limitations. While the current study attempted to evaluate a randomly selected, representative cohort of employees at all worksites, workers were able to opt out of the cohort or refuse participation and some employees chosen for the evaluation cohort were never reached for the baseline measurement; therefore, we recognize that the evaluation cohort may be not be truly representative of all workers at these sites. In addition, only English-speaking employees are included in the cohort, which limits generalizability of the findings. The analyses are cross-sectional, so cannot be interpreted in terms of cause and effect. Another limitation was the use of self-report versus objective measures of PA and diet; however, we do include the objective measure of BMI. Also, stress is measured using questions with excellent face validity, but that have not been otherwise previously tested. This ten-level ordinal measure is entered as a continuous variable in linear models, so interpretation should keep these limitations in mind.
Conclusions/Implications
The results of the current study demonstrate that obesity and health-related lifestyle behaviors may differ by job-category (or by demographic characteristics that cluster within job category), which may indicate the need for targeted interventions at worksites. More longitudinal and intervention studies are needed to investigate the potential relationships between job type, weight status, and lifestyle behaviors among employees, particularly with larger populations of service workers for comparative purposes. Furthermore, future research should determine whether targeted or tailored interventions to specific worker characteristics are more effective. These studies should include objective measures such as BMI and accelerometer data for measuring PA as well as other health outcomes such as blood pressure, blood cholesterol, etc. in addition to self-report lifestyle measures.
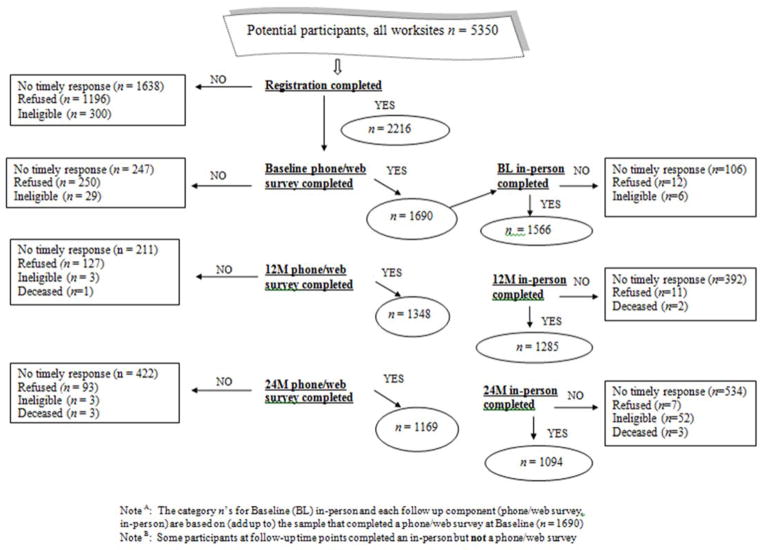
Figure 1. Cohort recruitment and retention diagram.
Note A: The category n’s for Baseline (BL) in-person and each follow up component (phone/web survey, in-person) are based on (add up to) the sample that completed a phone/web survey at Baseline (n = 1690)
Note B: Some participants at follow-up time points completed an in-person but not a phone/web survey
Acknowledgments
Research for this paper was made possible by funding from National Institutes of Diabetes and Digestive and Kidney Diseases, Grant No. 5R18DK071946. We would like to acknowledge the efforts of the following individuals for their help with the WOW study or with the preparation of this manuscript: Reese Middler, Robin Scheer, Nicole Ferreira, Suzanne Brodney-Folse, Janette Baird, Rajiv Kumar, Brad Weinstein, Mark Wooding, Don Wilson, Jamie M. Enos, Agatha Barnes, David Upegui, Laura Dionne, and Julie Zhao.
Abbreviations
- WOW
Working on Wellness
- BMI
Body Mass Index
- PA
Physical Activity
- F&V
Fruit and vegetable
Footnotes
Financial Disclosure
There is no conflict of interest by any author.
Bibliography
- 1.Flegal KM, Carroll MD, Kit BK, Ogden CL. Prevalence of obesity and trends in the distribution of body mass index among US adults, 1999–2010. JAMA: the journal of the American Medical Association. 2012;307(5):491–7. doi: 10.1001/jama.2012.39. Epub 2012/01/19. [DOI] [PubMed] [Google Scholar]
- 2.Ogden CL, Carroll MD, Kit BK, Flegal KM. Prevalence of obesity in the United States, 2009–2010. NCHS data brief. 2012;(82):1–8. Epub 2012/05/24. [PubMed] [Google Scholar]
- 3.Centers for Disease Control and Prevention, National Center for Chronic Disease Prevention and Health Promotion. Obesity, Halting the Epidemic by Making Health Easier – at a Glance 2011. 2013 Sep 29; Available from: http://www.cdc.gov/chronicdisease/resources/publications/aag/pdf/2011/obesity_aag_web_508.pdf.
- 4.World Health Organization. Report of a WHO Consultation on obesity, June 3–5, 1997. Geneva: World Health Organization; 1997. Obesity: preventing and managing the global epidemic; p. 894. [PubMed] [Google Scholar]
- 5.Lewis CE, Jacobs DR, Jr, McCreath H, Kiefe CI, Schreiner PJ, Smith DE, Williams OD. Weight gain continues in the 1990s: 10-year trends in weight and overweight from the CARDIA study. Coronary Artery Risk Development in Young Adults. Am J Epidemiol. 2000;151(12):1172–81. doi: 10.1093/oxfordjournals.aje.a010167. [DOI] [PubMed] [Google Scholar]
- 6.Kopelman PG. Obesity as a medical problem. Nature. 2000;404(6778):635–43. doi: 10.1038/35007508. [DOI] [PubMed] [Google Scholar]
- 7.U.S. Department of Health and Human Services PHS, Office of the Surgeon General. The Surgeon General’s call to action to prevent and decrease overweight and obesity 2001. 2008 May 31; Available from: http://www.surgeongeneral.gov/topics/obesity/calltoaction/CalltoAction.pdf. [PubMed]
- 8.Fried VPK, MacKay AP, Xia H. (NCHS) NCfHS, editor. Chartbook on Trends in the Health of Americans. 2003. [Google Scholar]
- 9.National Heart, Lung, and Blood Institute (NHLBI) What are the health risks of overweight and obesity? 2014 Nov 14; Available from http://www.nhlbi.nih.gov/health/health-topics/topics/obe/risks.
- 10.Malnick SD, Knobler H. The medical complications of obesity. Q J Med. 2006;99(9):565–579. doi: 10.1093/qjmed/hcl085. [DOI] [PubMed] [Google Scholar]
- 11.Flegal KM, Kit BK, Orpana H, Graubard BI. Association of all-cause mortality with overweight and obesity using standard body mass index categories: A systematic review and meta-analysis. JAMA. 2003;309(1):71–82. doi: 10.1001/jama.2012.113905. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Flegal KM, Graubard BI, Williamson DF, Gail M. Cause-specific excess deaths associated with underweight, overweight, and obesity. JAMA. 2013;298(17):2028–2037. doi: 10.1001/jama.298.17.2028. [DOI] [PubMed] [Google Scholar]
- 13.Economos CD, Hyatt RR, Goldberg JP, Must A, Naumova EN, Collins JJ, Nelson ME. A community intervention reduces BMI z-score in children: Shape Up Somerville first year results. Obesity (Silver Spring) 2007;15(5):1325–36. doi: 10.1038/oby.2007.155. [DOI] [PubMed] [Google Scholar]
- 14.Papas MA, Alberg AJ, Ewing R, Helzlsouer KJ, Gary TL, Klassen AC. The built environment and obesity. Epidemiologic reviews. 2007;29:129–43. doi: 10.1093/epirev/mxm009. [DOI] [PubMed] [Google Scholar]
- 15.Swinburn B, Gill T, Kumanyika S. Obesity prevention: a proposed framework for translating evidence into action. Obes Rev. 2005;6(1):23–33. doi: 10.1111/j.1467-789X.2005.00184.x. [DOI] [PubMed] [Google Scholar]
- 16.Stokols D. Establishing and maintaining healthy environments. Toward a social ecology of health promotion. Am Psychol. 1992;47(1):6–22. doi: 10.1037//0003-066x.47.1.6. [DOI] [PubMed] [Google Scholar]
- 17.Spiegel AM, Alving BM. Executive summary of the Strategic Plan for National Institutes of Health Obesity Research. The American journal of clinical nutrition. 2005;82(1 Suppl):211S–4S. doi: 10.1093/ajcn/82.1.221S. [DOI] [PubMed] [Google Scholar]
- 18.Katz DL, O’Connell M, Yeh MC, Nawaz H, Njike V, Anderson LM, Cory S, Dietz W Task Force on Community Preventive S. Public health strategies for preventing and controlling overweight and obesity in school and worksite settings: a report on recommendations of the Task Force on Community Preventive Services. MMWR Recommendations and reports: Morbidity and mortality weekly report Recommendations and reports/Centers for Disease Control. 2005;54(RR-10):1–12. [PubMed] [Google Scholar]
- 19.U.S. Department of Labor, Bureau of Labor Statistics. The Employment Situation Summary. 2013. [Google Scholar]
- 20.Bureau of Labor Statistics, U.S. Department of Labor. The Employment Situation - August 2013. 2013. [Google Scholar]
- 21.Lusk SL, Raymond DM., 3rd Impacting Health through the Worksite. Wierenga M, editor. Nursing Clinics of North America: Lifestyle Modification. 2002:247–56. doi: 10.1016/s0029-6465(01)00004-4. [DOI] [PubMed]
- 22.Nakamura K, Shimai S, Kikuchi S, Tominaga K, Takahashi H, Tanaka M, Nakano S, Motohashi Y, Nakadaira H, Yamamoto M. Shift work and risk factors for coronary heart disease in Japanese blue-collar workers: serum lipids and anthropometric characteristics. Occupational medicine. 1997;47(3):142–6. doi: 10.1093/occmed/47.3.142. [DOI] [PubMed] [Google Scholar]
- 23.Schulte PA, Wagner GR, Ostry A, Blanciforti LA, Cutlip RG, Krajnak KM, Luster M, Munson AE, O’Callaghan JP, Parks CG, Simeonova PP, Miller DB. Work, obesity, and occupational safety and health. American journal of public health. 2007;97(3):428–36. doi: 10.2105/AJPH.2006.086900. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Caban AJ, Lee DJ, Fleming LE, Gomez-Marin O, LeBlanc W, Pitman T. Obesity in US workers: The National Health Interview Survey, 1986 to 2002. American journal of public health. 2005;95(9):1614–22. doi: 10.2105/AJPH.2004.050112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Random Integer Generator. 2013 [cited 2013 September 20, 2013]. Available from: http://www.random.org/integers/
- 26.Centers for Disease Control and Prevention. Healthy Weight - it’s not a diet, it’s a lifestyle! 2013 Sep 20; Available from: http://www.cdc.gov/healthyweight/assessing/bmi/adult_bmi/index.html.
- 27.Thompson FE, Subar AF, Smith AF, Midthune D, Radimer KL, Kahle LL, Kipnis V. Fruit and vegetable assessment: performance of 2 new short instruments and a food frequency questionnaire. Journal of the American Dietetic Association. 2002;102(12):1764–72. doi: 10.1016/s0002-8223(02)90379-2. [DOI] [PubMed] [Google Scholar]
- 28.National Cancer Instititue. Fruit & Vegetable Screeners in the Eating at America’s Table Study (EATS): Overview. 2013 Sep 20; Available from: http://appliedresearch.cancer.gov/diet/screeners/fruitveg/
- 29.Thompson FE, Midthune D, Subar AF, Kipnis V, Kahle LL, Schatzkin A. Development and evaluation of a short instrument to estimate usual dietary intake of percentage energy from fat. Journal of the American Dietetic Association. 2007;107(5):760–7. doi: 10.1016/j.jada.2007.02.006. [DOI] [PubMed] [Google Scholar]
- 30.Thompson FE, Midthune D, Williams GC, Yaroch AL, Hurley TG, Resnicow K, Hebert JR, Toobert DJ, Greene GW, Peterson K, Nebeling L. Evaluation of a short dietary assessment instrument for percentage energy from fat in an intervention study. The Journal of nutrition. 2008;138(1):193S–9S. doi: 10.1093/jn/138.1.193S. [DOI] [PubMed] [Google Scholar]
- 31.Craig CL, Marshall AL, Sjostrom M, Bauman AE, Booth ML, Ainsworth BE, Pratt M, Ekelund U, Yngve A, Sallis JF, Oja P. International physical activity questionnaire: 12-country reliability and validity.[see comment] Medicine & Science in Sports & Exercise. 2003;35(8):1381–95. doi: 10.1249/01.MSS.0000078924.61453.FB. [DOI] [PubMed] [Google Scholar]
- 32.US Department of Labor. Bureau of Labor Statistics, Appendix A. The Standard Occupational Classification System August 1998. 2013 Oct 2; Available from: http://www.bls.gov/oes/2003/may/appendix_a.pdf.
- 33.Campbell MK, Tessaro I, DeVellis B, Benedict S, Kelsey K, Belton L, Sanhueza A. Effects of a tailored health promotion program for female blue-collar workers: health works for women. Preventive medicine. 2002;34(3):313–23. doi: 10.1006/pmed.2001.0988. [DOI] [PubMed] [Google Scholar]
- 34.Emmons KM, Marcus BH, Linnan L, Rossi JS, Abrams DB. Mechanisms in multiple risk factor interventions: smoking, physical activity, and dietary fat intake among manufacturing workers. Working Well Research Group. Preventive medicine. 1994;23(4):481–9. doi: 10.1006/pmed.1994.1066. [DOI] [PubMed] [Google Scholar]
- 35.Ogden CL, Lamb MM, Carroll MD, Flegal KM. Obesity and socioeconomic status in children and adolescents: United States, 2005–2008. NCHS data brief. 2010;(51):1–8. Epub 2011/01/08. [PubMed] [Google Scholar]
- 36.Niknian M, Linnan LA, Lasater TM, Carleton RA. Use of population-based data to assess risk factor profiles of blue and white collar workers. Journal of occupational medicine. 1991;33(1):29–36. doi: 10.1097/00043764-199101000-00010. [DOI] [PubMed] [Google Scholar]
- 37.Truven Health Analytics. Health Leaders FactFile Hospital Employee Health Risk May 2013. 2013 Sep 24; Available from: http://www.healthleadersmedia.com/content/291731.pdf.
- 38.Williams AE, Vogt TM, Stevens VJ, Albright CA, Nigg CR, Meenan RT, Finucane ML. Work, weight, and wellness: The 3W program: A worksite obesity prevention and intervention trial. Obesity. 2007;15:16s–26s. doi: 10.1038/Oby.2007.384. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Farber HS. Chapter 37 Mobility and stability: The dynamics of job change in labor markets. In: Ashenfelter O, Card D, editors. Handbook of Labor Economics. Part B. 3A. 1999. pp. 2439–2483. [Google Scholar]
- 40.Sorensen G, Stoddard A, Ockene JK, Hunt MK, Youngstrom R. Worker participation in an integrated health promotion/health protection program: results from the WellWorks project. Health Educ Q. 1996;23(2):191–203. doi: 10.1177/109019819602300205. [DOI] [PubMed] [Google Scholar]
- 41.Lassen AD, Thorsen AV, Sommer HM, Fagt S, Trolle E, Biltoft-Jensen A, Tetens I. Improving the diet of employees at blue-collar worksites: results from the ‘Food at Work’ intervention study. Public health nutrition. 2011;14(6):965–74. doi: 10.1017/S1368980010003447. [DOI] [PubMed] [Google Scholar]