Abstract
Background:
Prone position is commonly used to provide surgical access to a variety of surgeries. In view of the advantages of induction of anesthesia in the prone position, we conducted a randomized study to evaluate and compare ProSeal laryngeal mask airway (LMA) and i-gel in the prone position.
Materials and Methods:
Totally, 40 patients of either sex as per American Society of Anesthesiologists physical status I or II, between 16 and 60 years of age, scheduled to undergo surgery in prone position were included in the study. After the patients positioned themselves prone on the operating table, anesthesia was induced by the standard technique. LMA ProSeal was used as an airway conduit in group 1 while i-gel was used in group 2. At the end of surgery, the airway device was removed in the same position.
Results:
Insertion of airway device was successful in first attempt in 16, and 17 cases in ProSeal laryngeal mask airway (PLMA) and i-gel groups, respectively. A second attempt was required to secure the airway in 4 and 3 patients in PLMA and i-gel groups, respectively. The mean insertion time was 21.8 ± 2.70 s for group 1 and 13.1 ± 2.24 s for group 2, the difference being statistically significant (P < 0.05). The mean seal pressure in group 1 was 36 ± 6.22 cm H2 O and in group 2 was 25.4 ± 3.21 cm H2 O. The difference was statistically significant (P < 0.05). 13 patients in group 1 had fiberoptic bronchoscopy (FOB) grade 1 while it was 6 for group 2. The remaining patients in both groups had FOB grade 2.
Conclusion:
Insertion of supraglottic airways and conduct of anesthesia with them is feasible in the prone position. The PLMA has a better seal while insertion is easier with i-gel.
Keywords: Anesthesia, i-gel, prone position, ProSeal laryngeal mask airway, supraglottic airway device
INTRODUCTION
The prone position is commonly used to provide surgical access to a variety of surgeries. Conventionally, anesthesia is induced in the supine position and after tracheal intubation using nonkinking reinforced endotracheal tube; they are turned over to the prone position. An alternative to this technique can be induction of anesthesia in the prone position. Endotracheal intubation is difficult in the prone position. Hence, supraglottic devices may be preferred for securing the airway in the prone position. The laryngeal mask airway classic (cLMA) has been used in the prone position by various authors in emergencies and elective surgeries.[1,2,3,4]
The ProSeal laryngeal mask airway (PLMA) offers several advantages over cLMA.[5] The i-gel airway (Intersurgical Ltd., U.K.) is a cuffless, single use supraglottic airway device with a drain tube and provides good vertical and lateral stability on insertion.[6,7]
In view of the advantages of induction of anesthesia in prone position and feasibility of airway management with supraglottic devices, we conducted a randomized study to determine the feasibility of insertion of PLMA and i-gel in prone position and to evaluate and compare PLMA and i-gel in prone position with respect to ease of insertion, airway seal pressure and fiberoptic grading.
MATERIALS AND METHODS
The present study was conducted in a prospective and randomized manner. Totally, 40 patients of either sex as per American Society of Anesthesiologists physical status class I or II, between 16 and 60 years of age, scheduled to undergo surgery in prone position were included in the study. Edentulous patients, patients with known difficult airway, diseases of the spine, body mass index (BMI) >35 kg/m2, mouth opening <2.5 cm, risk of aspiration, history of upper gastro-intestinal surgery, bleeding or clotting abnormalities, esophageal trauma or evidence of upper gastro-intestinal bleed were excluded from the study.
All the patients were visited a day prior to surgery, and an informed written consent was obtained. They were premedicated with tablet alprazolam 0.25 mg and tablet ranitidine 150 mg at bedtime the day prior to surgery and 2 h preoperatively. Patients were randomly allocated to one of the two groups using computer generated sequence of random numbers as follows:
Group 1 - (n = 20): In these patients, PLMA was used as an airway conduit.
Group 2 - (n = 20): In these patients, i-gel was used as an airway conduit.
After securing venous access, the patients were asked to lie in the prone position with the head resting on a soft ring and rotated to their left side. Routine monitoring such as heart rate, noninvasive blood pressure, electrocardiogram and oxygen saturation were set up. The operating table was tilted laterally to have the patient's left side up by 15°, to improve the access to face for mask ventilation and insertion of the airway device. Pillows were placed under the thorax and pelvis to allow adequate movement of anterior abdominal wall during ventilation. Patients were asked to position their arms comfortably. All prospective pressure points were adequately protected using cotton padding. A trolley was positioned on the side of operating table so that the patient could be rapidly made supine, should airway management fail.
Preoxygenation with 100% oxygen was done for 3 min. Induction of anesthesia was achieved with standardized general anesthetic technique comprising of glycopyrrolate 0.2 mg, fentanyl 1 μg/kg and propofol 2.5 mg/kg. Increments of propofol were given till there was a loss of response to verbal commands. When there was no response to jaw thrust, the appropriate size PLMA or i-gel was inserted depending on the group assigned using the introducer technique for PLMA and digital technique for i-gel. The size of the airway device was selected as per weight criteria.[7,8] After insertion, the airway device was connected to the anesthesia breathing system. PLMA cuff was inflated to a pressure of 60 cm of H2O. Correct placement of the device was confirmed by manual ventilation and obtaining square wave capnograph on the monitor. In the event of complete or partial airway obstruction or a significant leak, it was decided to remove the airway device and attempt reinsertion. If correct placement of the airway device was not achieved in two attempts, it would have been considered as failure. In such a situation, it the patient would have been turned supine on the trolley and the airway would have been secured with an endotracheal tube. Muscle relaxation with vecuronium was provided after confirming proper placement of the airway device. Positive pressure ventilation was instituted with 66% N2O in O2 and isoflurane, with a tidal volume of 8 ml/kg, respiratory rate of 12/min and I:E ratio of 1:2. The surgery then commenced.
Data recorded were ease of insertion, time of device placement, oropharyngeal seal pressure, gastric tube placement and fiberoptic grading.
Ease of insertion was graded on a three-point scale: Easy, difficult or failure. An easy insertion was defined as the insertion without resistance in a single maneuver. A difficult insertion was one where more than one attempt was required to seat the device. In case it was not possible to insert the device in two attempts, it would have been labeled as failure. The time interval between picking-up the PLMA or i-gel and obtaining an effective airway was noted as time required for device placement. Oropharyngeal seal pressure was determined by switching off the ventilator at a fixed gas flow of 3 L/min, with the expiratory valve completely closed and recording the airway pressure (maximum allowed 40 cm of water) at which equilibrium was reached.[9] A well lubricated gastric tube of size 14 FG was passed through the drain tube of PLMA and a size 12 FG through i-gel. Its correct placement was confirmed by injection of air and simultaneous epigastric auscultation. A flexible fibreoptic scope was introduced into the airway tube to grade the laryngeal view. Fibreoptic view was graded as recommended by Lardner et al.[9]
Trachea in line with distal lumen and clear view of the glottis.
Glottis and posterior epiglottis visualized.
Glottis and anterior epiglottis visualized with <50% of glottis obscured.
Glottis and anterior epiglottis visualized with >50% of glottis obscured.
Glottis not seen.
Any other problem encountered was recorded. After completion of the surgical procedure, neuromuscular blockade was reversed. The airway device was removed in the same position when the patient was able to open the mouth on command. The patient was then turned supine on to the trolley.
At the end of the study, the data were compiled and analyzed statistically. Two-tailed unpaired t-test for age, weight, height, BMI, insertion time and seal pressure and Chi-square tests for sex distribution, Mallampatti grade, size of device used, number of attempts, ease of insertion and fiberoptic bronchoscopy (FOB) grade were applied.
Observations
The mean ages of the patients in groups 1 and 2 were 28.7 ± 11.15 and 24.2 ± 5.73, respectively. The mean weight of patients was 62.8 ± 11.30 kg in PLMA group and 63.25 ± 9.78 kg in i-gel group. The mean height of the patients was 1.62 ± 0.13 m in PLMA group and 1.61 ± 0.09 m in i-gel group. The mean BMI was 24.06 ± 3.38 kg/m2 in PLMA group and 22.99 ± 3.44 kg/m2 in i-gel group. The demographic profile [Table 1] of the patients in the two groups was comparable (P > 0.05).
Table 1.
Showing demographic profile
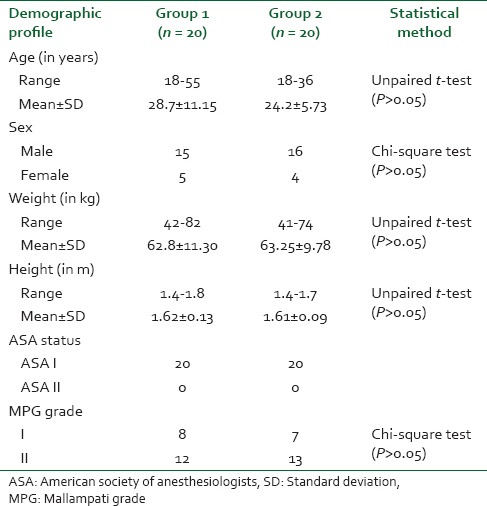
Eight patients in PLMA group had a MPG 1, while 7 patients in i-gel group had an MPG 1. Remaining patients in both groups had a MPG 2. The difference was not statistically significant. Size 3 airway device was inserted in 5 patients in PLMA group and 4 patients in i-gel group. A size 4 device was inserted in the remaining patients in both groups. The difference was not statistically significant (P > 0.05).
It was possible to insert the airway device in first attempt in 16 (80%) and 17 (85%) cases in PLMA and i-gel groups respectively. A second attempt was required to secure the airway in 4 and 3 patients in PLMA and i-gel groups, respectively [Table 2]. The difference was not statistically significant (P > 0.05). The mean insertion time was 21.8 ± 2.70 s for group 1 with minimum time of 16 s and maximum time of 26 s and 13.1 ± 2.24 s for group 2 with minimum time of 10 s and maximum time of 17 s. The difference was statistically significant [Table 2].
Table 2.
Showing various parameters
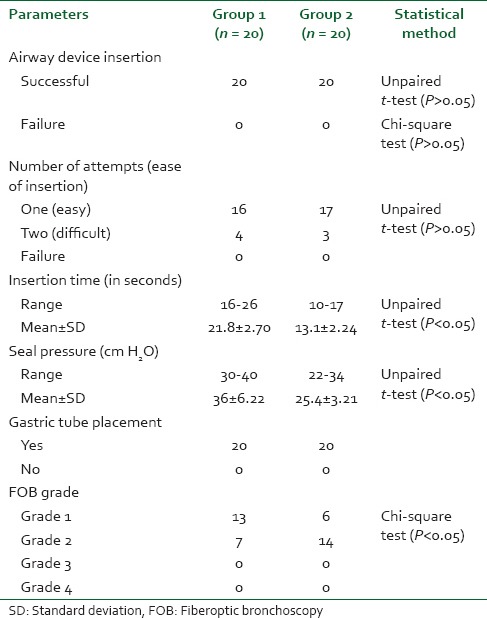
The mean seal pressure in group 1 was 36 ± 6.22 cm H2O and in group 2 was 25.4 ± 3.21 cm H2O. The difference was statistically significant (P < 0.05). The lowest seal pressures in groups 1 and 2 were 30 and 22 cm H2O, respectively, and the highest in groups 1 and 2 were 40 and 34 cm H2O, respectively. 13 patients in PLMA group had a FOB grade 1 while it was 6 for the i-gel group. The remaining patients in both groups had a FOB grade 2. The difference was significant (P < 0.05). Gastric tube placement was possible in all the patients in both groups [Table 2].
There were no episodes of hypoxia, hypercapnia, displacement, regurgitation, gastric insufflations or airway reflex activation.
DISCUSSION
With induction of anesthesia in prone position, there is less chance of peripheral nerve damage as patients can take comfortable position themselves before induction of anesthesia, and less medical and paramedical personnel are required to position the patients. Induction in the prone position may also be advantageous in patients who are unable to lie in the supine position due to painful lesions on the back.[1,10]
In our study, we found that it was possible to insert the airway device in first attempt in 16 (80%) and 17 (85%) cases in PLMA and i-gel groups, respectively. A second attempt was required to secure the airway in 4 and 3 patients in PLMA and i-gel groups respectively. The difference between groups was not statistically significant (P > 0.05). There were no failures, and no patient had to be turned supine during induction or maintenance of anesthesia. The difficulty in the insertion of airway device in first attempt was due to inadequate anesthesia and was managed successfully with additional increments of propofol as was seen by Ng et al. in their prospective audit of 73 patients who underwent prone position surgeries with cLMA as airway device, encountered difficulty in insertion in nine cases (12%).[2] Raphael et al. managed a case of accidental extubation in the prone position, with cLMA, which was inserted without any difficulty.[11] LMA has been used as airway rescue in intubated neonate after accidental extubation in the prone position.[12] Dingeman et al. also secured airway in a case of accidental extubation with cLMA, which was easily inserted.[3] Kumar et al. in a study of 100 patients anesthetized in the prone position, had difficulty inserting cLMA in two cases, in whom it was inserted in second attempt. In one case, there was folding of LMA cuff on itself making it difficult to be pushed inside. In the other case, patient started closing the mouth just when the LMA had passed half-way inside the oral cavity. Those problems were attributed to inadequate depth of anesthesia and responded to deepening of anesthesia.[1] Stevens and Mehta in a retrospective chart review of 103 patients who underwent prone surgical procedures with cLMA found that 94.7% of patients had LMAs that were inserted successfully in the first attempt, and in the remaining cases, it was possible in the second attempt.[4]
Brimacombe et al. in their retrospective audit in which PLMA was inserted in 245 healthy adults in prone position, reported that insertion of the PLMA was successful at the first attempt in 237 patients using the digital technique and at the second attempt with bougie-guided method. No patient required rotation back to the supine position for airway management. The etiology of failure was difficulty in advancing the cuff into the pharynx on seven occasions and ineffective ventilation related to malpositioning on one occasion.[13] Agrawal et al. reported a case in which an intubating LMA was used to secure airway in the prone position in the first attempt without any difficulty.[14] Singh et al. in a comparison of the clinical performance of i-gel with PLMA in 60 elective surgeries in supine position, found that the ease of insertion was more with i-gel (29/30) than with PLMA (23/30) (P < 0.05). The success rate of first attempt of insertion were 30/30 (100%) for i-gel and 28/30 (93.3%) for PLMA, which was not statistically significant.[15] We noted a success rate of 80% with PLMA group and 85% with i-gel group. Shin et al. in 2010 investigated the usefulness of the i-gel compared to the cLMA and PLMA in 167 patients who underwent surgery in the supine position. The success rates for first attempt of insertion were similar among the three groups (P = 0.670).[16]
The mean insertion time was 21.8 ± 2.70 s for group 1 with minimum time of 16 s and maximum time of 26 s and 13.1 ± 2.24 s for group 2 with minimum time of 10 s and maximum time of 17 s. The difference was statistically significant (P < 0.05). The longer insertion time with PLMA may be due to the introducer tool technique or its bulkier structure in relation to the i-gel. López et al. reported a mean insertion time of 21 ± 15 s with LMA Supreme in the prone position.[17] There is no study to the best of our knowledge that mentions the insertion time for PLMA or i-gel in supine or prone position.
Gastric tube placement was possible in all the patients in both groups. Brimacombe et al. also reported successful insertion of the gastric tube in 245 patients who underwent surgeries in the prone position with PLMA as airway conduit.[13] Gastric tube insertion was possible in all the 40 cases in the study by López et al. where LMA Supreme was used in the prone position.[17] Singh et al. reported in their study of 60 patients in supine position surgeries that gastric tube insertion was easier through i-gel (30/30) than through PLMA (26/30), though it was possible to insert it in the remaining cases with some manipulation.[15]
The mean seal pressure in group 1 was 36 ± 6.22 cm H2O and in group 2 was 25.4 ± 3.21 cm H2O. The difference was statistically significant (P < 0.05). The lowest seal pressures in groups 1 and 2 were 30 and 22 cm H2O, respectively, and the highest in groups 1, and 2 were 40 and 34 cm H2O, respectively. Brimacombe et al. reported mean seal pressure of 32 ± 12 cm H2O with PLMA in the prone position in a retrospective audit of 245 patients.[13] López et al. in their study obtained mean seal pressure of 27 ± 5 cm H2O with LMA supreme in 40 patients.[17] Singh et al. in a comparison study of PLMA and i-gel in supine position in 60 cases, found the average airway sealing pressure with i-gel as 25.27 cm H2O and that with LMA ProSeal as 29.6 cm H2O, which was statistically significant (P < 0.05).[15] Shin et al. compared i-gel with PLMA and cLMA in 167 patients in supine position and reported that the airway leak pressures of the i-gel group (27.1 ± 6.4 cm H2O) and PLMA group (29.8 ± 5.7 cm H2O) were significantly higher than that of the cLMA group (24.7 ± 6.2 cm H2O).[16]
The superior seal of PLMA compared to i-gel in our study is thus substantiated by the studies in the supine position.
Both the groups had a good fiberoptic grade of 1 and 2, where 13 patients in PLMA group had a FOB grade 1 (65%), while it was 6 for the i-gel group (30%). The remaining patients in both groups had a FOB grade 2. The difference was significant (P < 0.05). None of the patients had a grade where glottis was not visible. There are no studies that mention the fiberoptic grade of supraglottic devices in the prone position.
After the induction of anesthesia in the prone position, the jaw and tongue fall anteriorly, and the lungs of all patients were easy to ventilate manually via a facemask. There was no instance of desaturation or hemodynamic instability during the surgery and no patient had to be turned supine during induction or maintenance of anesthesia. Ng et al., Dingeman et al., Brimacombe et al. and Valero et al. also reported the same phenomenon in their reports.[2,3,13,18] Neuromuscular blocking agent was given only after confirming proper placement of the device to avoid desaturation due to difficult ventilation. All the studies related to the use of supraglottic devices in elective surgeries in the prone position also mentioned the same practice.[1,4,13,18,19,20,21]
To conclude, we would like to state that there is no study to the best of our knowledge regarding the use of i-gel in the prone position. The routine use of supraglottic devices in elective prone position surgeries has to be validated by larger randomized controlled studies. However as this has given confidence to us for airway rescue in a neonate we are hopeful that this study of ours will be of great use in similar situations or in case where airway control is necessary in prone position.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Kumar V, Lalitha K, Lone T. Use of classic laryngeal mask airway inserted in prone position for controlled ventilation: A feasibility study. Indian J Anesth. 2008;52:813–7. [Google Scholar]
- 2.Ng A, Raitt DG, Smith G. Induction of anesthesia and insertion of a laryngeal mask airway in the prone position for minor surgery. Anesth Analg. 2002;94:1194–8. doi: 10.1097/00000539-200205000-00026. [DOI] [PubMed] [Google Scholar]
- 3.Dingeman RS, Goumnerova LC, Goobie SM. The use of a laryngeal mask airway for emergent airway management in a prone child. Anesth Analg. 2005;100:670–1. doi: 10.1213/01.ANE.0000146512.48688.FA. [DOI] [PubMed] [Google Scholar]
- 4.Stevens WC, Mehta PD. Use of the Laryngeal Mask Airway in patients positioned prone for short surgical cases in an ambulatory surgery unit in the United States. J Clin Anesth. 2008;20:487–8. doi: 10.1016/j.jclinane.2008.05.009. [DOI] [PubMed] [Google Scholar]
- 5.Brain AI, Verghese C, Strube PJ. The LMA ‘ProSeal’ — A laryngeal mask with an oesophageal vent. Br J Anesth. 2000;84:650–4. doi: 10.1093/bja/84.5.650. [DOI] [PubMed] [Google Scholar]
- 6.Levitan RM, Kinkle WC. Initial anatomic investigations of the I-gel airway: A novel supraglottic airway without inflatable cuff. Anesthesia. 2005;60:1022–6. doi: 10.1111/j.1365-2044.2005.04258.x. [DOI] [PubMed] [Google Scholar]
- 7.Gabbott DA, Beringer R. The iGEL supraglottic airway: A potential role for resuscitation? Resuscitation. 2007;73:161–2. doi: 10.1016/j.resuscitation.2006.10.026. [DOI] [PubMed] [Google Scholar]
- 8.Cook TM, Nolan JP, Verghese C, Strube PJ, Lees M, Millar JM, et al. Randomized crossover comparison of the proseal with the classic laryngeal mask airway in unparalysed anesthetized patients. Br J Anesth. 2002;88:527–33. doi: 10.1093/bja/88.4.527. [DOI] [PubMed] [Google Scholar]
- 9.Lardner DR, Cox RG, Ewen A, Dickinson D. Comparison of laryngeal mask airway (LMA) - Proseal and the LMA-Classic in ventilated children receiving neuromuscular blockade. Can J Anesth. 2008;55:29–35. doi: 10.1007/BF03017594. [DOI] [PubMed] [Google Scholar]
- 10.Saini S, Bansal T. Anesthetic management of a patient in prone position-advantage of proseal laryngeal mask airway along with review of literature. Cumhuriyet Med J. 2013;35:98–101. [Google Scholar]
- 11.Raphael J, Rosenthal-Ganon T, Gozal Y. Emergency airway management with a laryngeal mask airway in a patient placed in the prone position. J Clin Anesth. 2004;16:560–1. doi: 10.1016/j.jclinane.2004.03.004. [DOI] [PubMed] [Google Scholar]
- 12.Taxak S, Gopinath A. Laryngeal mask airway classic as a rescue device after accidental extubation in a neonate in prone position. Indian J Anesth. 2011;55:542. doi: 10.4103/0019-5049.89902. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Brimacombe JR, Wenzel V, Keller C. The proseal laryngeal mask airway in prone patients: A retrospective audit of 245 patients. Anesth Intensive Care. 2007;35:222–5. doi: 10.1177/0310057X0703500211. [DOI] [PubMed] [Google Scholar]
- 14.Agrawal S, Sharma JP, Jindal P, Sharma UC, Rajan M. Airway management in prone position with an intubating Laryngeal Mask Airway. J Clin Anesth. 2007;19:293–5. doi: 10.1016/j.jclinane.2006.09.009. [DOI] [PubMed] [Google Scholar]
- 15.Singh I, Gupta M, Tandon M. Comparison of Clinical Performance of I-Gel with LMA-Proseal in Elective Surgeries. Indian J Anesth. 2009;53:302–5. [PMC free article] [PubMed] [Google Scholar]
- 16.Shin WJ, Cheong YS, Yang HS, Nishiyama T. The supraglottic airway I-gel in comparison with ProSeal laryngeal mask airway and classic laryngeal mask airway in anesthetized patients. Eur J Anesthesiol. 2010;27:598–601. doi: 10.1097/EJA.0b013e3283340a81. [DOI] [PubMed] [Google Scholar]
- 17.López AM, Valero R, Brimacombe J. Insertion and use of the LMA Supreme in the prone position. Anesthesia. 2010;65:154–7. doi: 10.1111/j.1365-2044.2009.06185.x. [DOI] [PubMed] [Google Scholar]
- 18.Valero R, Serrano S, Adalia R, Tercero J, Blasi A, Sánchez-Etayo G, et al. Anesthetic management of a patient in prone position with a drill bit penetrating the spinal canal at C1-C2, using a laryngeal mask. Anesth Analg. 2004;98:1447–50. doi: 10.1213/01.ane.0000111102.52964.7f. [DOI] [PubMed] [Google Scholar]
- 19.Weksler N, Klein M, Rozentsveig V, Weksler D, Sidelnik C, Lottan M, et al. Laryngeal mask in prone position: Pure exhibitionism or a valid technique. Minerva Anestesiol. 2007;73:33–7. [PubMed] [Google Scholar]
- 20.Taxak S, Gopinath A. Insertion of the i-gel airway in prone position. Minerva Anestesiol. 2010;76:381. [PubMed] [Google Scholar]
- 21.Sharma V, Verghese C, McKenna PJ. Prospective audit on the use of the LMA-Supreme for airway management of adult patients undergoing elective orthopaedic surgery in prone position. Br J Anesth. 2010;105:228–32. doi: 10.1093/bja/aeq118. [DOI] [PubMed] [Google Scholar]


