Abstract
Background
Previous studies examining gender-based disparities in Emergency Department (ED) pain-care have been limited to a single pain-condition, a single study-site, and lack rigorous control for confounders.
Objective
A multicenter evaluation of the effect of gender on abdominal pain (AP) and fracture (FP) pain-care outcomes.
Research Design
Retrospective cohort-review of ED visits at 5 US hospitals in January, April, July and October 2009.
Subjects
6,931 patients with a final ED diagnosis of FP (n=1682) or AP (n=5249).
Measures
The primary-predictor was gender. The primary outcome was time to analgesic-administration. Secondary outcomes included time to medication-order, and the likelihood the receiving an analgesic and change in pain scores 360 minutes after triage: Multivariable models, clustered by study site, were conducted to adjust for race, age, comorbidities, initial pain-score, ED crowding and triage acuity.
Results
On adjusted analyses, compared with men, women with AP waited longer for analgesic administration [AP Women: 112 (65–187) min, Men: 96 (52–167) min, p<0.001] and ordering Women: [84 (41–160) min, Men: 71 (32–137) min, p<0.001], whereas women with FP did not (Administration: p=0.360; Order: p=0.133). Compared with men, women with AP were less likely to receive analgesics in the first 90 minutes (OR: 0.766, 95% CI: 0.670 – 0.875, p<0.001), whereas women with FP were not (p=0.357).
Discussion
In this multicenter study, we found that women experienced delays in analgesic administration for AP, but not for FP. Future research and interventions to decrease gender-disparities in pain-care should take type of pain into account.
Keywords: Gender, Pain Care, Health Policy
INTRODUCTION
Differences in pain treatment such as oligoanalgesia, delays in pain assessment and delays in treatment have been found across several settings.1 These differences have been attributed to patient characteristics (such as age, 2–4 gender, 5 race 6), institution,7 physician characteristics (gender and clinical experience8), triage acuity,9 and Emergency Department (ED) crowding. 2, 4, 10–15
In 2014, in response to concerns that women experience more severe acute and chronic pain, a commission formed by the Society of Academic Emergency Medicine investigated gender-based differences in pain treatment.16 The commission noted a paucity of studies on gender differences in the assessment and treatment of acute pain in the ED.16 Previous studies have yielded conflicting evidence about the existence of gender based differences in pain care,5, 8, 17–19 but these studies have been limited to a single type of pain (e.g. abdominal or back pain), a single study site, or were vulnerable to confounders such as ED crowding. Additionally, few studies have examined disparities in the quality of pain treatment in the early hours of the ED visit. Time to pain treatment is an important metric as early analgesia administration has been shown to have an impact ED outcomes such as length of stay20 and early pain relief, 21 may improve diagnostic accuracy 21, and may prevent development of chronic pain.22–24 To our knowledge, no multicenter study has examined gender-based disparities in early acute pain care process metrics, and how these early treatment disparities may affect patient pain outcomes.
The objective of this study was to identify gender-based differences in pain treatment processes and patient outcomes. Specifically, this study seeks to assess whether gender-differences in delays to analgesics, doses of analgesics, and likelihood of analgesic administration exist, and whether these differences change over time. This study will also examine whether gender differences exist in early ED pain relief (based on a 10-point verbal pain score).
METHODS
Design and Setting
This was a secondary analysis of data from a multicenter cohort of 7,082 patient visits collected by Hwang et al. for a study on age-related disparities in emergency department pain care 3. The cohort includes all adult (18+) patients with fracture or abdominal pain presenting to five geographically distinct hospital emergency departments in the months of January, April, July and October 2009 (Jan 1 to 31, 2009; April 1 to 30, 2009; July 1 to 31, 2009, and October 1 to 31, 2009). Four of the EDs were academic centers; one was a community hospital. Four of the sites were considered urban, one suburban. Two sites were located in the Northeast region of the United States, one in the Mid-Atlantic, one in the Rocky Mountain Region, and one on the West Coast. We excluded visits that did not have time data available or whose time data did not follow a plausible timeline (e.g. patients who were recorded to receive an analgesic after ED discharge). This study received institutional board approval with a waiver of informed consent at all five sites. For more information about cohort selection by pain condition, please see original study methods.3
Variables
The primary patient predictor was gender, which was characterized into men and women. Covariates included in analyses were patient and site related factors that could affect the quality of pain care received in the ED (based on literature review or construct validity). These covariates included race/ethnicity,6 age,3 gender,16 Charlson Comorbidity Index, triage acuity, the first recorded pain score, the number of medications patients were taking prior to the ED visit, and ED occupancy rate (a validated measure of ED crowding 25; defined as ED census divided by the number of ED treatment bays). Adjusted analyses were clustered by site and also controlled for the type of fracture (long, short, facial bone) and type of abdominal pain (nonspecific abdominal pain, appendicitis, biliary, bowel obstruction, cancer, colitis, constipation, flank pain, hernia, musculoskeletal, obstetrics/gynecology, pancreatic, urological).
Early Pain Care Process Metrics
To evaluate pain care during the early period of the ED visit, we examined analgesic administration within the first 360 minutes of the ED visit. This period was broken into 90-minute intervals and included whether an analgesic was provided, whether an opioid was provided, and the cumulative equianalgesic dose of opioids administered at each interval. Additional treatment processes examined were time to first analgesic order and time to analgesic administration.
Change in Pain Score
All five sites used a 10-point verbal rating scale to assess patients’ pain. This study examined the change in pain score reported by patients within the first 360 minutes of their ED visit. This was calculated by subtracting the first recorded pain score in the ED (normally recorded during triage) from the pain score at the 360th minute of the ED visit (defined as the last pain score recorded within the first 360 minutes of the ED visit). Although this outcome measure is novel to this study, the calculation methodology has been employed previously to calculate total ED pain score change by subtracting the first recorded pain score from the last recorded pain score before discharge.3
Data Collection
The five sites in the primary study all had ED electronic medical records (EMRs) (four used ED Pulsecheck, PICIS Inc, Wakefield, MA; one used Epic ASAP – Epic Systems Corp, Verona, WI). The EMRs used at each of the five sites time stamp data when entered; thus time of pain care processes including pain assessments, medication orders and administration, disposition and discharge are all logged. These time data, together with patient characteristics and pain process data, were abstracted by research personnel trained at each of the five sites according to methods established and described by investigators of prior ED pain studies.2, 4, 10 The abstractors were blinded to the study hypothesis, and were trained using the twelve recommended criteria for medical record review studies.26 Each abstractor received at least a four-hour training session, shadowed the chart review process of the investigator, did chart abstractions that were compared with those of the investigators, and were deemed qualified to abstract independently when test abstractions were completed with 95% agreement.
Medications
For our analysis, we considered opioids, acetaminophen, topical anesthetics and non-steroidal anti-inflammatory drugs (NSAID) as analgesics. Opioids included codeine, fentanyl, hydrocodone, hydromorphone, morphine, methadone as well as combination drugs and opioids such as Percocet (acetaminophen and oxycodone). NSAIDS included ibuprofen, aspirin, indomethacin, naproxen, and ketorolac. Topical anesthetics consisted mainly of topical lidocaine. For patients with abdominal pain, proton pump inhibitors, antacids, H1 receptor antagonists, anti-gas and phenazopyridine were also considered treatments for abdominal pain.
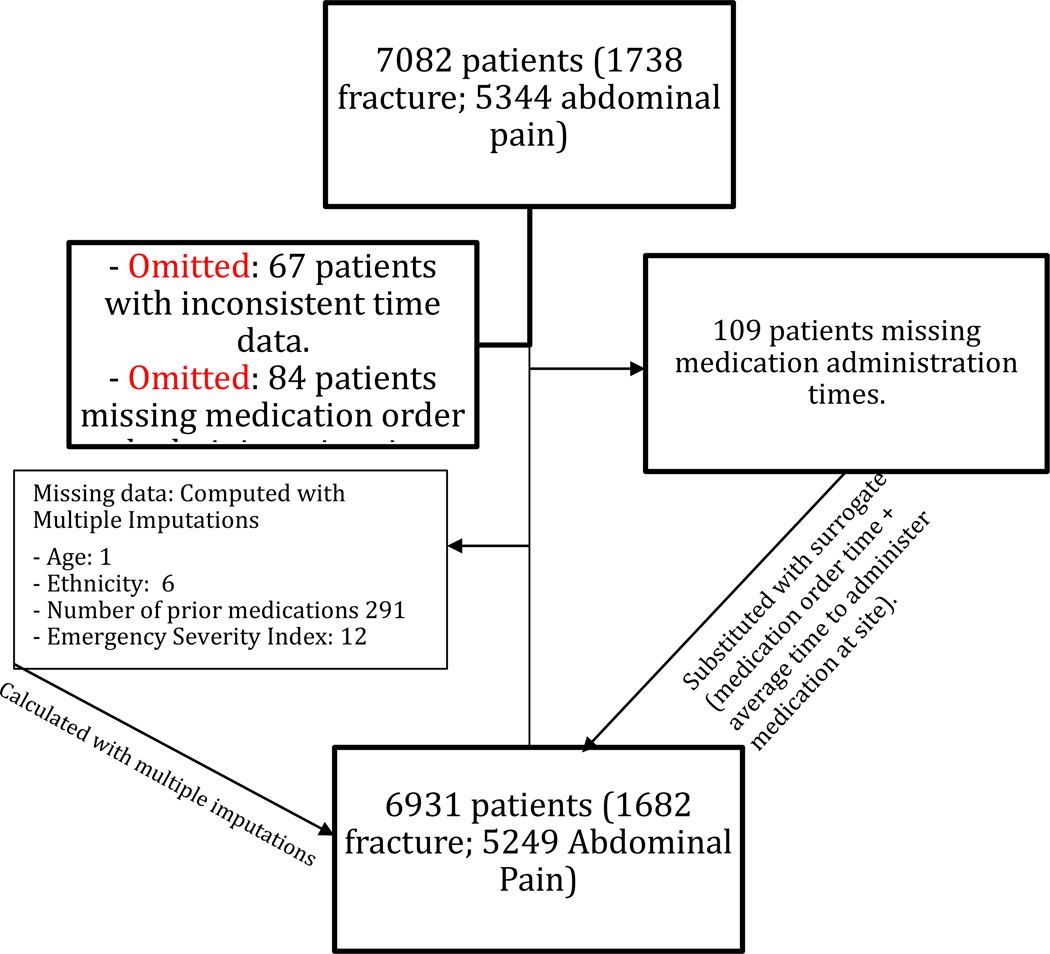
Time Data
Time stamp data from the study were reviewed manually for accuracy and consistency. Patients missing crucial time data (for example, the time of medication administration and order) were excluded from analysis. Additionally, any patients with time points that did not adhere to a plausible timeline (e.g. recorded as receiving pain medication several days after ED discharge) were removed from the final analysis (see Figure 1). For the remaining patients, all pain care processes, medication administration times, and pain scores within the first 90 minutes, 180 minutes, 270 minutes and 360 minutes from triage were manually filtered and compiled together for further analysis. Analgesic administration in the first 90 minutes has been used as a threshold for evaluation of difference in pain care processes in prior studies 20, because the literature suggests that up to an one-hour threshold is a permissible delay in managing severe pain27, 28 and because 90 minutes is the median time to analgesics reported in many EDs.29, 30 Sensitivity analyses were conducted using 90-minute intervals up to 360 minutes.
Data Analysis
All data were collected in Microsoft Excel (Microsoft Corp., Redmond, WA, USA), and analyzed using SPSS 20.0.0 (SPSS Inc., Chicago, IL, USA). Descriptive analyses were completed for the cohort by gender categories and subcategorized by type of pain (fracture vs. abdominal). Any covariate that could impact the outcome measure based on construct validity or existing evidence in literature, was included in adjusted analysis. Adjusted analyses were completed using generalized estimating equations (GEE) clustered by study site, using linear models for continuous outcomes, logistic models for categorical outcomes, and gamma with log link function for time-based outcomes. Values reported represent those of adjusted analyses.
RESULTS
Cohort Characteristics
A total of 7,082 visits met inclusion criteria (5,344 abdominal pain; 1738 fracture pain). Of these visits, 6,931 (98%) (5,249 abdominal pain; 1,682 fracture pain) had pain care time data and were retained for analyses. The characteristics of this study cohort are listed in Table 1. There were significant differences by gender in ethnicity, number of prior medications, Charlson Comorbidity Index, and final ED diagnoses of abdominal or fracture pain (see Table 1).
Analgesic Administration
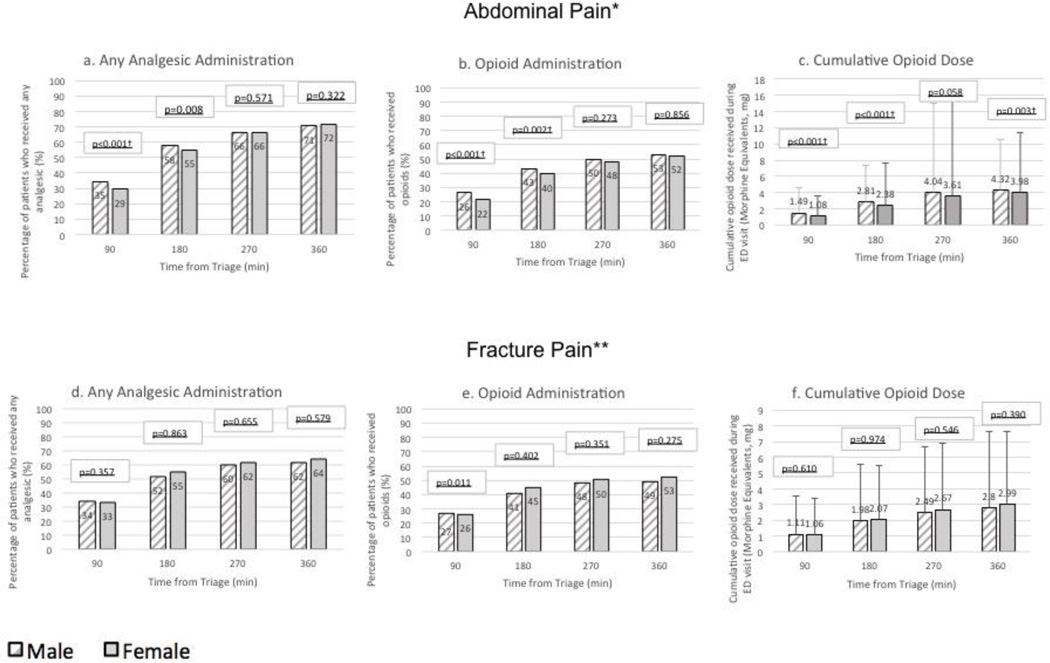
Analgesic administration varied by gender and pain condition. On adjusted analyses of abdominal pain patients, women experienced longer delays to both analgesia ordering and administration (see table 2). Consistent with the delay in administration, women were less likely to receive to receive an analgesic up to 180 minutes into the ED visit (OR: 0.906, 95% CI: 0.842 to 0.974, p=0.008), but differences were non-significant by 270 minutes (OR:0.969, 95% CI: 0.867 to 1.082) (see Figure 2a). Women were less likely to receive opioids until 180 minutes (OR: 0.872, 95% CI: 0.798 to 0.951, p = 0.002), but by 270 minutes, there were no statistically significant differences in opioid administration (OR:0.944, 95% CI: 0.850 to 1.047) (see Figure 2b). Women received lower morphine equivalents in the first 90 minutes. This difference in total opioid dose persisted until at least 360 minutes into the ED visit (see Figure 2c).
In contrast, gender-based differences in pain care processes were not identified in patients with fracture pain. There were no significant differences in the time to first analgesic order (p = 0.133), and administration (p=0.360) (see Table 2). There were no significant gender-based differences in the likelihood of analgesic administration (OR: 1.009, 95 CI: 0.699 to 1.455, p=0.357 at 90 min) or dose of opioids in fracture patients (see Figure 2 f).
Pain scores
When comparing patients with abdominal pain by gender, no significant differences were found in final 360 minute pain score (p=0.210) or the change in pain score after 360 minutes (p=0.210). Likewise, for fracture pain, no significant differences were found between genders in the final 360 minute pain score (p=0.636) or the change in pain score at 360 minutes (p=0.569)(Table 3).
DISCUSSION
The results of this multicenter observational study suggest that women experienced delays to pain care (rather than a reduction in the overall likelihood of receiving analgesics), and that these differences are condition-specific. When patients with abdominal pain were analyzed, women were found to have greater delays to both analgesic order and administration. On the other hand, when patients with fractures were analyzed, no significant differences were found between genders in the time to analgesic administration and ordering.
The differences in pain care between fracture and abdominal pain align with the clinical manifestations of these conditions. Abdominal pain is less overt, can be due to multiple etiologies and, in women, may require additional diagnostic work-up such as imaging, pregnancy tests and pelvic exams. Additionally, the delay in abdominal pain medication may be worsened due to a residual belief among some providers that analgesics may decrease diagnostic accuracy of the abdominal exams.31 Although no reason exists to delay analgesic administration while awaiting diagnostic workup, it is conceivable that providers may prioritize completion of the extensive work-up over proper pain management. In contrast, the work-up and treatment of fractures is similar in both genders; the absence of additional diagnostic evaluation may account for the absence of differences between genders in time to analgesics.
Our results complement recent studies that have found no gender-based difference in the overall likelihood of analgesic administration in the ED. Banz et al. found no difference in the overall likelihood of analgesic reception in a cohort of women arriving to the ED with any type of pain.18 However, our study is novel in that it examines the first 90 minutes of the ED visit, when disparities do exist, before becoming non-significant as the ED visit progresses. This difference in early analgesic administration can likely be explained by the longer delays in analgesic administration to women found by this study. Few studies have specifically examined gender-based analgesia delays. However, our results are consistent with a small study by Chen, E. H., et al., in which women in a prospective cohort of 75 patients waited 16 minutes longer for analgesics compared with men.5 Our study also found that women receive lower doses at all times during the first 360 minutes of an ED visit, but this difference may be due to differences in weight-based dosing between genders.
Our study is novel in that it compares and contrasts management of two different types of ED pain conditions at several intervals during an ED visit. These data suggest that different provider-level management regimes for different pain conditions may drive gender disparities in pain care. This study also suggests that gender-based disparities may be hidden if processes are examined of the ED visit as a whole; in our study, pain care disparities differences emerged when the ED visit was examined at each time interval. In an acute care setting such as the ED, early processes may deserve special investigation, as early pain management is an essential function of ED care.16
This study has several clinical implications. First, delay to analgesia due to long diagnostic workup may be mitigated by operational policies that streamline analgesic administration. Ideally, these interventions should target both medication ordering and administration. For example, nurse-initiated analgesic administration has been shown to reduce time to analgesics by as much as 50%.32 Second, recognizing that abdominal pain in women requires a more comprehensive diagnostic work-up, steps may be taken to ensure early initiation of workup. For example, training nursing staff to order imaging at triage has been shown to reduce delays to care by up to 20 minutes.33 Third, delays to abdominal pain medications may be caused by persisting clinician concern that early analgesia sacrifices the accuracy of diagnostic tests (despite evidence to the contrary34). Until recently, for example, a primary surgical textbook advocated holding analgesics until the physical exam was complete.35 Efforts to improve clinician awareness about the safety and necessity of early analgesics may therefore be a critical target to reduce delays to analgesics.36
This study is subject to several limitations. First, as it is a retrospective review, this study cannot conclusively determine why gender disparities in early pain treatment exist. However, one reason may be that the more extensive diagnostic workup required for abdominal pain in women may contribute to the differences. Second, though this study accounts for several confounders, including ED crowding, triage acuity, comorbidities and age, it could not control for provider gender. Third, this study cannot account for verbal medication orders (e.g. one provider getting the analgesic supplies ready, while another places the order in the chart). Finally, the lag time to logging processes of care in the EMR may be influenced by site-level practice variation. For example, at some ERs, nurses may enter medication orders by the bedside wheras at others they may do it at a central unit. We clustered our analyses by study site to reduce the effects of site-level practice variation on our results. Additionally, although the lag time between medication administration and charting of medication administration may vary by site, medication ordering is time-stamped instantaneously. Because medications cannot be administered before the order is placed in an EMR, we believe delays to medication ordering (regardless of the reason) “count” as delays in care.
In conclusion, this is the first multicenter study to evaluate gender-based differences in ED pain care. We found women with abdominal pain experienced delays to both medication administration and medication ordering, but not women with fractures. Although gender-based disparities were identified within the first 90 minutes of the ED visit, these differences disappeared by 360 minutes into the ED visit. Despite appearing to wait longer for analgesics, women were, overall, not less likely to receive an analgesic. Future interventions and research into gender-based disparities in pain care should take into account the type of pain condition being treated and address time to analgesic rather than likelihood of receiving analgesic.
Figure 1.
Missing Data Flowchart
Figure 2.
Gender differences in analgesic administration for the first 360 minutes of an ED, at 90 minute intervals, separated by type of presenting pain.
*Abdominal pain p values adjusted (using General Estimating Equations) for race, age, crowding, Charlson Comorbidity Index, triage acuity, the first recorded pain score, the number of medications patients were taking prior to the ED visit, and the type of abdominal pain
** Fracture p values adjusted (using General Estimating Equations) for race, age, crowding, Charlson Comorbidity Index, triage acuity, the first recorded pain score, the number of medications patients were taking prior to the ED visit, and the type of Fracture.
Table 1.
Patient characteristics by gender category (n=6931)
| Characteristics | Men n = 2804 |
Women n = 4127 |
P value |
|---|---|---|---|
| Age mean (SD) | 43.90 (16.94) | 44.68 (19.10) | 0.076 |
| Race/ethnicity, n (%) | <0.001 | ||
| White | 1265 (45.1) | 1717 (41.6) | |
| Black | 501 (17.9) | 987 (23.9) | |
| Hispanic | 640 (22.8) | 999 (24.2) | |
| ESI, mean (SD) | 3.06 (0.574) | 3.04 (0.52) | 0.160 |
| Number of current medications, mean (SD) | 2.01 (3.21) | 2.58 (3.70) | <0.001 |
| Charlson Comorbditiy Index, mean (SD) | 0.72 (1.57) | 0.63 (1.37) | 0.016 |
| Emergency Department Occupancy Rate at triage, mean (SD) | 1.32 (0.64) | 1.33 (0.64) | 0.906 |
| Abdominal Pain final diagnosis, n (%) | 1970 (70.3) | 3280 (79.5) | <0.001 |
ESI = Emergency Severity Index (1= acute, 5=non-acute)
Table 2.
Delays in analgesic administration of pain patients by gender
| Abdominal Pain | Fracture Pain | |||||
|---|---|---|---|---|---|---|
| Process Measure |
Men | Women | P value* | Men | Women | P Value** |
| Time to first analgesic, min, median (25%– 75%) |
96 (52 – 167) |
112 (65– 187) |
<0.001 | 82 (41– 147) |
90 (44 – 151) |
0.360 |
| Time to first analgesic order, min, median (25 – 75%) |
71 (32– 137) |
84 (41 – 160) |
<0.001 *** | 65 ( 27 – 127) |
68 (26 – 126) |
0.133 **** |
Adjusted for race, age, gender, Charlson Comorbidity Index, triage acuity, the first recorded pain score, the number of medications patients were taking prior to the ED visit, and the type of abdominal pain. General Estimating Equations (GEE) were used for multivariable analysis.
Adjusted for race, age, gender, Charlson Comorbidity Index, triage acuity, the first recorded pain score, the number of medications patients were taking prior to the ED visit, and the type of Fracture. GEE were used for multivariable analysis.
Adjusted for race, age, gender, Charlson Comorbidity Index, triage acuity, the first recorded pain score, the number of medications patients were taking prior to the ED visit, time to first medication order, and the type of abdominal pain. GEE were used for multivariable analysis.
Adjusted for race, age, gender, Charlson Comorbidity Index, triage acuity, the first recorded pain score, the number of medications patients were taking prior to the ED visit, time to first medication order, and the type of Fracture. GEE were used for multivariable analysis.
Table 3.
Pain score changes by gender.
| Abdominal Pain | Fracture Pain | |||||
|---|---|---|---|---|---|---|
| Measure | Men | Women | P value* | Men | Women | P Value** |
| First pain score, Mean (SD) |
7.45 (2.60) |
7.58 (3.30) |
0.945 | 6.73 (2.69) |
6.91 (2.67) |
0.02 |
| Pain score at 360 minutes after triage, Mean (SD) |
4.35 (3.39) |
4.64 (3.33) |
0.210 | 5.38 (2.98) |
5.37 (3.10) |
0.636 |
| Reduction in pain score in the first 360 minutes of ED visit, Mean (SD) |
2.93 (3.45) |
2.77 (3.42) |
0.210 | 1.30 (2.66) |
1.45 (2.72) |
0.569 |
Adjusted for race, age, gender, Charlson Comorbidity Index, triage acuity, the first recorded pain score, the number of medications patients were taking prior to the ED visit, and the type of abdominal pain. GEE were used for multivariable analysis.
Adjusted for race, age, gender, Charlson Comorbidity Index, triage acuity, the first recorded pain score, the number of medications patients were taking prior to the ED visit, and the type of Fracture. GEE were used for multivariable analysis.
Acknowledgments
Funding Sources: UH was supported by a K23 award from the National Institute on Aging (K23 AG031218)
Contributor Information
Ammar Siddiqui, Postal Address: 50 east 98th street Apt 4B New York NY 10029, USA, Ammar.Siddiqui@mssm.edu, Telephone Number: 603-729-6180, Fax Number: 646-537-9497, Institution: Emergency Department, Icahn School of Medicine at Mount Sinai, New York, NY 10029, USA.
Laura Belland, Laura.Belland@mssm.edu, Telephone Number: 513-315-1274, Fax Number: 646-537-9497, Correspondence Address: 217 E 84th St, Apt 1A, New York, NY 10028, Institution: Emergency Department, Icahn School of Medicine at Mount Sinai, New York, NY 10029, USA.
Laura Rivera-Reyes, laura.rivera@mountsinai.org, Telephone Number: 212-241-8062, Institution: Emergency Department, Icahn School of Medicine at Mount Sinai, New York, NY 10029, USA.
Daniel Handel, handel@musc.edu, Telephone Number: 8 43-792-2383, Correspondence Address: 169 Ashley Avenue, 248 NT, MSC 332, Institution: Medical University of South Carolina, Charleston, SC 29425, USA.
Kabir Yadav, Kabiryadav@gmail.com, Telephone Number: (310) 222-3503, Fax Number: (310) 212-6101, Institution: Department of Emergency Medicine, University of California Lost Angeles, Los Angeles, CA 90095, USA.
Kennon Heard, Kennon.heard@ucdenver.edu, Telephone Number: 720-848-6777, Institution: University of Colorado School of Medicine Department of Emergency Medicine, Aurora CO 80045.
Amanda Eisenberg, eisenberg.m.amanda@gmail.com, Telephone Number: 732-616-7256, Institution: Mount Sinai Beth Israel, New York, NY, 10128, USA.
Ula Hwang, ula.hwang@mountsinai.org, Telephone Number: 212-241-8062, Fax Number: 646-537-9497, Correspondence Address: 19 East 98th Street Floor 3rd Room 316A, New York, NY 10029, Institution: Emergency Department, Icahn School of Medicine at Mount Sinai, New York, NY 10029, USA.
REFERENCES
- 1.Weimer MB, Macey TA, Nicolaidis C, et al. Sex differences in the medical care of VA patients with chronic non-cancer pain. Pain medicine. 2013;14:1839–1847. doi: 10.1111/pme.12177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Bernstein SL, Aronsky D, Duseja R, et al. The Effect of Emergency Department Crowding on Clinically Oriented Outcomes. Academic Emergency Medicine. 2009;16:1–10. doi: 10.1111/j.1553-2712.2008.00295.x. [DOI] [PubMed] [Google Scholar]
- 3.Hwang U, Belland LK, Handel DA, et al. Is all pain is treated equally? A multicenter evaluation of acute pain care by age. Pain. 2014;155:2568–2574. doi: 10.1016/j.pain.2014.09.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Hwang U, Richardson L, Livote E, et al. Emergency Department Crowding and Decreased Quality of Pain Care. Academic Emergency Medicine. 2008;15:1248–1255. doi: 10.1111/j.1553-2712.2008.00267.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Chen EH, Shofer FS, Dean AJ, et al. Gender disparity in analgesic treatment of emergency department patients with acute abdominal pain. Academic emergency medicine : official journal of the Society for Academic Emergency Medicine. 2008;15:414–418. doi: 10.1111/j.1553-2712.2008.00100.x. [DOI] [PubMed] [Google Scholar]
- 6.Mills AM, Shofer FS, Boulis AK, et al. Racial disparity in analgesic treatment for ED patients with abdominal or back pain. The American journal of emergency medicine. 2011;29:752–756. doi: 10.1016/j.ajem.2010.02.023. [DOI] [PubMed] [Google Scholar]
- 7.Vinson DR, Hurtado TI, Vandenberg JT, et al. Variations among emergency departments in the treatment of benign headache. Ann Emerg Med. 2003;41:90–97. doi: 10.1067/mem.2003.24. [DOI] [PubMed] [Google Scholar]
- 8.Safdar B, Heins A, Homel P, et al. Impact of physician and patient gender on pain management in the emergency department--a multicenter study. Pain medicine. 2009;10:364–372. doi: 10.1111/j.1526-4637.2008.00524.x. [DOI] [PubMed] [Google Scholar]
- 9.Arya R, Wei G, Mccoy JV, et al. Decreasing Length of Stay in the Emergency Department With a Split Emergency Severity Index 3 Patient Flow Model. Academic Emergency Medicine. 2013;20:1171–1179. doi: 10.1111/acem.12249. [DOI] [PubMed] [Google Scholar]
- 10.Hwang U, Richardson LD, Sonuyi TO, et al. The effect of emergency department crowding on the management of pain in older adults with hip fracture. J Am Geriatr Soc. 2006;54:270–275. doi: 10.1111/j.1532-5415.2005.00587.x. [DOI] [PubMed] [Google Scholar]
- 11.Kulstad EB, Sikka R, Sweis RT, et al. ED overcrowding is associated with an increased frequency of medication errors. American Journal of Emergency Medicine. 2010;28:304–309. doi: 10.1016/j.ajem.2008.12.014. [DOI] [PubMed] [Google Scholar]
- 12.Mills AM, Shofer FS, Chen EH, et al. The Association between Emergency Department Crowding and Analgesia Administration in Acute Abdominal Pain Patients. Academic Emergency Medicine. 2009;16:603–608. doi: 10.1111/j.1553-2712.2009.00441.x. [DOI] [PubMed] [Google Scholar]
- 13.Mullins PM, Pines JM. National ED crowding and hospital quality: results from the 2013 Hospital Compare data. American Journal of Emergency Medicine. 2014;32:634–639. doi: 10.1016/j.ajem.2014.02.008. [DOI] [PubMed] [Google Scholar]
- 14.Pines JM, Shofer FS, Isserman JA, et al. The Effect of Emergency Department Crowding on Analgesia in Patients with Back Pain in Two Hospitals. Academic Emergency Medicine. 2010;17:276–283. doi: 10.1111/j.1553-2712.2009.00676.x. [DOI] [PubMed] [Google Scholar]
- 15.Sills MR, Fairclough DL, Ranade D, et al. Emergency Department Crowding Is Associated with Decreased Quality of Analgesia Delivery for Children with Pain Related to Acute, Isolated, Long-bone Fractures. Academic Emergency Medicine. 2011;18:1330–1338. doi: 10.1111/j.1553-2712.2011.01136.x. [DOI] [PubMed] [Google Scholar]
- 16.Musey PI, Jr, Linnstaedt SD, Platts-Mills TF, et al. Gender Differences in Acute and Chronic Pain in the Emergency Department: Results of the 2014 Academic Emergency Medicine Consensus Conference Pain Section. Academic emergency medicine : official journal of the Society for Academic Emergency Medicine. 2014 doi: 10.1111/acem.12529. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Bijur PE, Latimer CT, Gallagher EJ. Validation of a verbally administered numerical rating scale of acute pain for use in the emergency department. Academic emergency medicine : official journal of the Society for Academic Emergency Medicine. 2003;10:390–392. doi: 10.1111/j.1553-2712.2003.tb01355.x. [DOI] [PubMed] [Google Scholar]
- 18.Banz VM, Christen B, Paul K, et al. Gender, age and ethnic aspects of analgesia in acute abdominal pain: is analgesia even across the groups? Internal medicine journal. 2012;42:281–288. doi: 10.1111/j.1445-5994.2010.02255.x. [DOI] [PubMed] [Google Scholar]
- 19.Uri O, Elias S, Behrbalk E, et al. No gender-related bias in acute musculoskeletal pain management in the emergency department. Emergency medicine journal : EMJ. 2013 doi: 10.1136/emermed-2013-202716. [DOI] [PubMed] [Google Scholar]
- 20.Sokoloff C, Daoust R, Paquet J, et al. Is adequate pain relief and time to analgesia associated with emergency department length of stay? A retrospective study. BMJ open. 2014;4:e004288. doi: 10.1136/bmjopen-2013-004288. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Attard AR, Corlett MJ, Kidner NJ, et al. Safety of early pain relief for acute abdominal pain. Bmj. 1992;305:554–556. doi: 10.1136/bmj.305.6853.554. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Carroll I, Hah J, Mackey S, et al. Perioperative interventions to reduce chronic postsurgical pain. Journal of reconstructive microsurgery. 2013;29:213–222. doi: 10.1055/s-0032-1329921. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Baker K. Chronic pain syndromes in the emergency department: identifying guidelines for management. Emergency medicine Australasia : EMA. 2005;17:57–64. doi: 10.1111/j.1742-6723.2005.00690.x. [DOI] [PubMed] [Google Scholar]
- 24.Plunkett A, Turabi A, Wilkinson I. Battlefield analgesia: a brief review of current trends and concepts in the treatment of pain in US military casualties from the conflicts in Iraq and Afghanistan. Pain management. 2012;2:231–238. doi: 10.2217/pmt.12.18. [DOI] [PubMed] [Google Scholar]
- 25.McCarthy ML, Aronsky D, Jones ID, et al. The emergency department occupancy rate: a simple measure of emergency department crowding? Annals of emergency medicine. 2008;51:15–24. doi: 10.1016/j.annemergmed.2007.09.003. 24 e11-12. [DOI] [PubMed] [Google Scholar]
- 26.Worster A, Bledsoe RD, Cleve P, et al. Reassessing the methods of medical record review studies in emergency medicine research. Annals of emergency medicine. 2005;45:448–451. doi: 10.1016/j.annemergmed.2004.11.021. [DOI] [PubMed] [Google Scholar]
- 27.JCoAH, editor. Organizations. 2001. Pain: current understanding of assessment, management, and treatments. [Google Scholar]
- 28.Carns P. In: Health Care Guideline: Assessment and Management of Acute Pain. 6th Edition Improvement IfCS, editor. 2008. [Google Scholar]
- 29.Boyd RJ, Stuart P. The efficacy of structured assessment and analgesia provision in the paediatric emergency department. Emergency medicine journal : EMJ. 2005;22:30–32. doi: 10.1136/emj.2002.003574. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Todd KH, Ducharme J, Choiniere M, et al. Pain in the emergency department: results of the pain and emergency medicine initiative (PEMI) multicenter study. The journal of pain : official journal of the American Pain Society. 2007;8:460–466. doi: 10.1016/j.jpain.2006.12.005. [DOI] [PubMed] [Google Scholar]
- 31.Vermeulen B, Morabia A, Unger PF, et al. Acute appendicitis: influence of early pain relief on the accuracy of clinical and US findings in the decision to operate--a randomized trial. Radiology. 1999;210:639–643. doi: 10.1148/radiology.210.3.r99fe54639. [DOI] [PubMed] [Google Scholar]
- 32.Kelly AM, Brumby C, Barnes C. Nurse-initiated, titrated intravenous opioid analgesia reduces time to analgesia for selected painful conditions. Cjem. 2005;7:149–154. doi: 10.1017/s148180350001318x. [DOI] [PubMed] [Google Scholar]
- 33.Lindley-Jones M, Finlayson BJ. Triage nurse requested x rays--are they worthwhile? Journal of accident & emergency medicine. 2000;17:103–107. doi: 10.1136/emj.17.2.103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Thomas SH, Silen W, Cheema F, et al. Effects of morphine analgesia on diagnostic accuracy in Emergency Department patients with abdominal pain: a prospective, randomized trial. Journal of the American College of Surgeons. 2003;196:18–31. doi: 10.1016/s1072-7515(02)01480-1. [DOI] [PubMed] [Google Scholar]
- 35.Williams LF. Copes Early Diagnosis of the Acute Abdomen, 16th Edition - Silen, W. New Engl J Med. 1983;309:996–997. [Google Scholar]
- 36.Shojania KG, Duncan BW, McDonald KM, et al. Making health care safer: a critical analysis of patient safety practices. Evidence report/technology assessment. 2001:i–x. 1–668. [PMC free article] [PubMed] [Google Scholar]