Abstract
Objective
Dental caries is the most common preventable chronic disease among preschool children. The pediatric primary care setting provides an alternative site to deliver preventive oral health. This study estimates the cost-effectiveness of a medical office-based preventive oral health program in North Carolina (“Into the Mouths of Babes,” IMB).
Design
Observational study using Medicaid claims (2000–2006).
Setting
Medical staff delivered IMB services in medical offices. Dentists provided dental services in offices or hospitals.
Participants
209,285 Medicaid enrolled children at age 6 months.
Intervention
IMB visits included screening, parental counseling, topical fluoride application, and referral to dentists if needed. The cost-effectiveness analysis used the Medicaid program perspective and a propensity-score matched sample with regression analysis to compare children with ≥4 versus 0 IMB visits.
Main Outcome Measures
Dental treatments and Medicaid payments for children up to age 6 enabled assessment of the likelihood that IMB was cost-saving and, if not, the additional payments per hospital episode avoided.
Results
IMB is 32% likely to be cost-saving with discounting of benefits and payments. On average, IMB visits cost $11 more than reduced dental treatment payments per person. The program almost breaks even if future benefits from prevention are not discounted and would be cost-saving with certainty if IMB services could be provided at $34 instead of $55 per visit. The program is cost-effective with 95% certainty if Medicaid is willing to pay $2331 per hospital episode avoided.
Conclusions
IMB improves dental health for additional payments that can be weighed against unmeasured hospitalization costs.
INTRODUCTION
Various studies document high and growing rates of dental caries among children younger than five years of age1, 2 as well as related negative health consequences.3, 4 Most children with dental caries are in low-income families and use dental care infrequently despite eligibility for services through public insurance.5 The limited dentist supply and dentists’ low rate of participation in Medicaid further preclude access, motivating many communities to examine alternate approaches to this pressing public health problem.6
The pediatric primary care setting provides an alternative site to deliver preventive oral health interventions for preschool-aged children before they develop poor oral health.7, 8 Although very young children are unlikely to visit dentist offices, they frequently make well-child visits to primary care physicians.9 Preventive oral health care programs in medical offices include screening and risk assessment, parental counseling, topical fluoride application, and referral to dentists for further assessment or treatment if needed.8 Topical fluoride varnish is viewed as a cost-effective component of oral health care for low-income children, with recommendations for use every 3 to 6 months in high-risk children younger than 6 years of age.10–12 Studies show that intervention in preschool-aged children with fluoride varnish improves dental health and defrays costs but is not cost-saving.13, 14
Evidence on the effectiveness of oral health care in medical settings is limited.15 A program called Into the Mouths of Babes (IMB) was initiated in North Carolina (NC) in 2000 in which physicians are reimbursed by Medicaid to conduct dental screenings of children 3 years of age or younger, apply fluoride varnish, and counsel parents. IMB improved access to oral health care for children up to 3 years of age in NC.16 Depending on age, 18 to 39 percent of children had fluoride applications compared to a national estimate that only 2.5 percent of children under age four had fluoride treatments from dentists in 2006.17 Furthermore, children receiving four or more preventive IMB visits in medical offices had a 17 percent reduction in dental caries-related treatments up to 6 years of age compared with children not receiving IMB visits; the fact that physicians made referrals to dentists for treatment of the disease meant that children with IMB visits received treatment from referrals but also had improved dental health.18–20
By 2010, Medicaid programs in 42 states approved reimbursement of medical providers for preventive oral health services,21 and advocacy groups called for expansion of reimbursement for physicians to apply topical fluoride varnish.22 Furthermore, the Affordable Care Act (Title V, Section 5304) requires demonstrations of new models of dental care including training of primary care physicians. Although fluoride varnish application in schools or dental clinics is cost-saving,23 the cost-effectiveness of preventive dental care in early childhood is largely unknown.24, 25 This study assesses the cost-effectiveness of IMB services from the perspective of the North Carolina Medicaid program.
METHODS
Study Design
Participation by medical offices in the IMB program increased over time. By 2006, each NC county had at least one pediatric practice, family medicine practice or community clinic participating in IMB. Each month an estimated 40% of Medicaid enrollees under 3 years eligible for a visit that month received an IMB visit.16
During the study period (2000–2006), Medicaid paid for up to 6 IMB visits per child through 35 months of age. Services could be provided at any visit, though the recommended periodicity of well-child visits at 6, 9, 12, 15, 18 and 24 months are an ideal time for delivering IMB services. Many children did not see providers participating in the program or receive the full complement of 6 visits, though some children received at least four IMB visits. This observational population-based cohort study estimates the cost-effectiveness of the IMB program, measured as receipt of four or more IMB visits before age 3 versus no IMB visits. We exclude children who received 1–3 IMB visits to avoid underestimating the cost-effectiveness.
Data and Measures
The study included children enrolled in NC Medicaid at 6 months of age and deemed to be continuously enrolled for at least an additional 12 months during 2000–2006. We followed children until they were 72 months of age or no longer enrolled in NC Medicaid. The study was approved by an Institutional Review Board at UNC-CH.
A longitudinal analysis file of monthly observations per child was constructed using Medicaid claims. Because most gaps in Medicaid enrollment for these children were due to administrative factors, we calculated continuous enrollment from the first to last date of enrollment. Children with conditions unrelated to dental caries (e.g., surgery for cleft palette or mouth injury) were excluded. Medicaid reimbursement codes identified IMB visits (W8002, W8003, D0150, D0120, D1203, and D1330) and caries-related treatments (procedure codes beginning with D2-D9) including restorations, extractions, stainless steel crowns, and nerve-related treatments (pulpotomies/ pulpectomies). Through January 2007, the IMB program paid $61 for the first IMB visit and $53 for subsequent visits; based on the visit distribution, we used $54.81 as the average IMB visit payment by Medicaid during the study period.
Economic Evaluation Issues
Our cost-effectiveness analysis is conducted from the Medicaid program’s perspective; analysis issues are discussed below.
Effects
Although poor access to dental care affects quality of life, conventional measures of quality-adjusted life years may not be sensitive for assessing the impact of preventive oral health care. The main measure of effect was hospital episodes averted by IMB, assuming that it is worth paying something to avoid treatment under general anesthesia as well as associated pain, psychological implications and other difficult -to-quantify effects.
Costs
We measured costs from the payer perspective using Medicaid payments in 2006 dollars as follows:
| [Eq. 1] |
The payments for IMB recipients consist of IMB visits plus all other services related to dental care, whereas only the latter component applies for children not receiving IMB visits. We measured 3 categories of dental service payments:
Payments for hospital episodes for caries-related dental treatment (CRT), including emergency room visits with caries as a main diagnosis, physician services including anesthesiology, operating room expenses, overnight stays, and dentist services;
Dentist office visit payments for CRT; and
Dentist office visit payments for preventive services without CRT (including visits for planning treatments).
Medicaid payments were estimated by multiplying the monthly probability of any dental services by location (hospital-based, office-based with CRT, and office-based without CRT) by estimates of the Medicaid payments for each event type.
| [Eq. 2] |
If payments for IMB plus dental services for children receiving 4 or more IMB visits were less than payments for dental services for children not receiving IMB, then the program was cost-saving to Medicaid. Otherwise, the incremental cost effectiveness ratio (ICER) provides the payments per hospital episode averted:
| [Eq. 3] |
The denominator was multiplied by negative one so that the outcome becomes hospital episodes averted. All quantities in the ICER, except for the IMB visit payments, were derived as predicted values from regression analyses summed over all children and months of age.
Length of Follow-up and Discounting
We estimated payments for all services from 6 to 72 months of age. Because all IMB visits occur prior to 3 years of age, we used a discount rate of 3 percent per year beyond age 3 for Medicaid payments and hospital episodes averted.
Accounting for Uncertainty in Estimates
The analysis has uncertainty in the estimates of the monthly probability of each event (hospital episodes, office visits with CRT, and office visits without CRT). We generated 1000 bootstrap replications of the estimates and use a cost-effectiveness acceptability curve (CEAC) to depict the probably that IMB is cost-effective at different levels of willingness to pay for a hospital episode averted. The bootstrap sampled all observations for a child, so the confidence intervals are adjusted for repeat observations by child.
Statistical Analysis
The lack of program randomization in study design means that treatment selection could bias program impact estimates. If providers choose treatment based on caries risk status of the child, then the population impact of IMB in reducing dental treatment costs can be over- or underestimated. For example, if children receiving IMB services were inherently less likely to have severe dental caries, the resulting estimates would underestimate the true effect of the IMB program on dental disease and treatment. We conducted the analyses using the propensity-score matched sample. Using the aggregated experience of each child up to 36 months of age, we used logistic regression to estimate the likelihood of having ≥4 IMB visits controlling for child characteristics (gender, age, race, Hispanic ethnicity, and special needs, as defined by the NC Medicaid program) and county characteristics (defined below). Controlling for the special needs indicator was important because these children might be more likely to see primary care physicians more often. To control for systematic differences between children in the treatment and comparison groups, we matched IMB to control observations using predictions from this propensity score regression and single nearest-neighbor matching without replacement.26, 27
We used multinomial logistic regression to estimate the likelihood of the service category each month (hospital episode, dental office visit with CRT, dental office visit with no CRT, or no dental services). To estimate monthly Medicaid payments for each dental service category, we used linear regression models, estimated only for children receiving that service.
Each regression controlled for the following observed characteristics:
IMB indicator of four or more visits (and interactions with child age to allow treatment effects to vary by age);
child characteristics: gender, age, race, Hispanic ethnicity, special needs, and number of well-child visits up to age 3 (squared values of age and well-child visits allowed for non-linear effects);
county characteristics: the number of general and pediatric dentists who treat children per 10,000 population, pediatricians and family physicians per 10,000 population, the county’s Medicaid-eligible population less than age 18, urban status of the child’s county of residence,28 and percent of the county population with access to fluoridated public drinking water;29 and
linear time trend to control for unmeasured state-level changes in socioeconomic conditions and provider supply.
Using predicted estimates of the likelihood of dental service use and Medicaid payments, we averaged the estimates over all children in each age-month and then aggregated the experience over 6 to 72 months of age to estimate cumulative costs and effects. Although within each child’s experience, the months are not independent (e.g., a child who has a hospitalization one month for dental disease is not likely to have a hospitalization in the next month for dental disease), this approach predicts the experience for Medicaid-eligible children of each age, so that the aggregation over the 6 to 72 month experience provided cumulative population estimates. All analyses were conducted in Stata/IC 12 (Statacorp, College Station, TX).
RESULTS
Table 1 provides descriptive statistics for the full sample of 209,285 children by IMB visit category (0 versus ≥4). All children entered the analysis at 6 months of age and were followed while enrolled in Medicaid for approximately 42 months on average. Some characteristics differ by IMB visit categories; in particular, children having ≥4 visits had more well-child visits on average before 3 years of age (5.5 versus 3.3). Monthly dental treatment rates are very low, with fewer than 2 percent of children receiving any dental treatment in a given month. The last column of Table 1 contains statistics for the propensity-matched sample of children with 0 IMB visits; these statistics correspond very closely to the statistics for children with ≥4 IMB visits, showing that propensity score matching produced an appropriate comparison group..
Table 1.
Child-Level Descriptive Statistics (Full Sample and Propensity Score Matched Sample)
| All (n=209,285) |
≥4 IMB (n=12,984) |
0 IMB (n=196,301) |
Propensity Score 0 IMB (n=12,339) |
|
|---|---|---|---|---|
| Child-level variables | ||||
| Follow-up (months enrolled in Medicaid) | 42.36 | 40.52 | 42.48 | 40.5 |
| Monthly Rates of Dental Treatment | ||||
| Hospital Episode for Caries-related Treatment (CRT) | 0.0014 | 0.0011 | 0.0014 | 0.0015 |
| Dental Office Visit for CRT | 0.0082 | 0.0068 | 0.0083 | 0.0075 |
| Dental Office Visit without CRT | 0.0188 | 0.0198 | 0.0187 | 0.0213 |
| Male | 0.508 | 0.52 | 0.51 | 0.52 |
| Race | ||||
| White | 0.4 | 0.36 | 0.41 | 0.38 |
| Black | 0.37 | 0.38 | 0.37 | 0.37 |
| Other | 0.23 | 0.26 | 0.22 | 0.25 |
| Hispanic | 0.135 | 0.163 | 0.133 | 0.16 |
| Well child visits (6–36 months) | 3.41 | 5.49 | 3.26 | 5.47 |
| Special needs (NC program identification) | 0.036 | 0.031 | 0.036 | 0.030 |
| County-level variables (mean values in 2005) | ||||
| Medicaid eligibles/10,000 population | 731.2 | 816.3 | 724.9 | 806.8 |
| Dentists/10,000 population | 4.3 | 3.4 | 4.3 | 3.4 |
| Physicians/10,000 population | 4.6 | 4.0 | 4.6 | 4.1 |
| County population with fluoridated drinking water | ||||
| 0–24% | 0.04 | 0.04 | 0.05 | 0.04 |
| 25–49% | 0.02 | 0.04 | 0.02 | 0.04 |
| 50–74% | 0.10 | 0.07 | 0.10 | 0.08 |
| 75–100% | 0.85 | 0.86 | 0.85 | 0.85 |
| Urban status/metro adjacency of child’s county | ||||
| 1 Metro areas of 1 million pop or more | 0.16 | 0.07 | 0.17 | 0.07 |
| 2 Metro areas of 250,000 to 1 million pop | 0.45 | 0.25 | 0.47 | 0.27 |
| 3 Metro areas of fewer than 250,000 pop | 0.08 | 0.14 | 0.07 | 0.13 |
| 4 Urban pop of 20,000+, adjacent | 0.18 | 0.34 | 0.16 | 0.33 |
| 5 Urban pop of 20,000+, not adjacent | 0.01 | 0.05 | 0.01 | 0.03 |
| 6 Urban pop of 2500–19999, adjacent | 0.10 | 0.10 | 0.09 | 0.11 |
| 7 Urban pop of 2500–19999, not adjacent | 0.02 | 0.03 | 0.02 | 0.03 |
| 8 Completely rural or <2,500 urban pop, adjacent | 0.02 | 0.02 | 0.01 | 0.03 |
| 9 Completely rural or <2,500 urban pop, not adjacent | 0.02 | 0.04 | 0.02 | 0.04 |
Note: IMB is the preventive dentistry program “Into the Mouths of Babes.” The propensity score final analysis file included 12,339 children in each group for a total of 1,036,301 child-months observations.
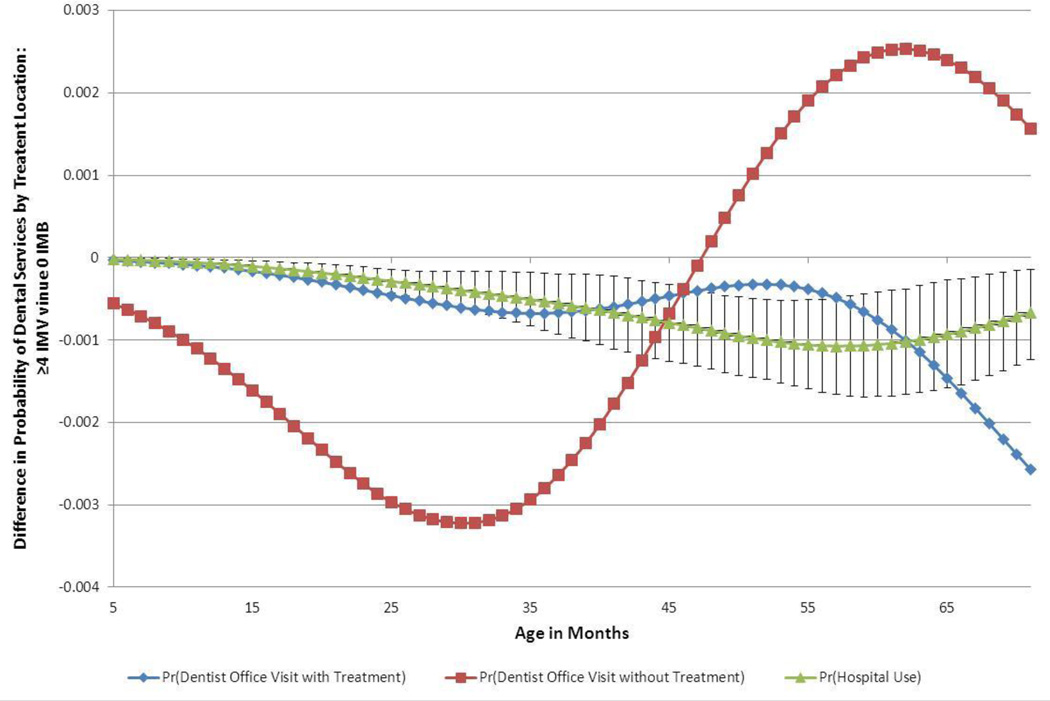
Figure 1 provides rates of dental service use predicted from the service regressions. (Results from all regressions are available on request.) Compared to children with 0 IMB, children receiving ≥4 IMB visits have a lower likelihood of having dental CRT in a hospital or dentist office at each month of age. IMB results in a statistically significant reduction in the likelihood of having a hospital episode related to dental caries, as shown by the 95% confidence interval bars in Figure 1. Children receiving ≥4 IMB visits before age 3 are more likely to have a non-treatment visit (including preventive visits as well as visits to identify but not treat dental caries) beyond 48 months of age than are children with 0 IMB visits, though the effect is not statistically significant at p<0.05.
Figure 1.
The Effect of ≥4 IMB Visits on the Probability of Dental Services: By Treatment Location with 95% CI for Pr(Hospital Use)
Table 2 provides estimated mean Medicaid payments for the 3 dental service categories conditional upon receiving caries-related treatments. Children with ≥4 IMB visits had lower Medicaid payments for hospital or dentist office treatments, suggesting fewer treatments within a treatment episode.
Table 2.
Regression Predictions of Mean Values Per Child over 6 to 72 Months of Age for Medicaid Payments# Matched Sample)
| ≥4 IMB | 0 IMB | |
|---|---|---|
| Mean Medicaid Payments (95% CI): | ||
| Hospital Episode for Dental Caries-related Treatment | $2,936 ($2035, $3247) |
$3,051 ($2150, $3362) |
| Dental Office Visit with Caries-related Treatment | $334 ($271, $423) |
$362 ($299, $452) |
| Dental Office Visit without Caries-related Treatment | $84 ($73, $96) |
$84 ($73, $96) |
Note: IMB is the preventive dentistry program “Into the Mouths of Babes”
Preparation of payment data involved: (1) exclusion of records with payments in the lowest five percentiles within each category that were likely not reflective of true costs; and (2) reclassification of 3,301 child-month observations with 12 or more dental treatments as dental hospitalizations despite having a primary diagnosis other than dental caries.
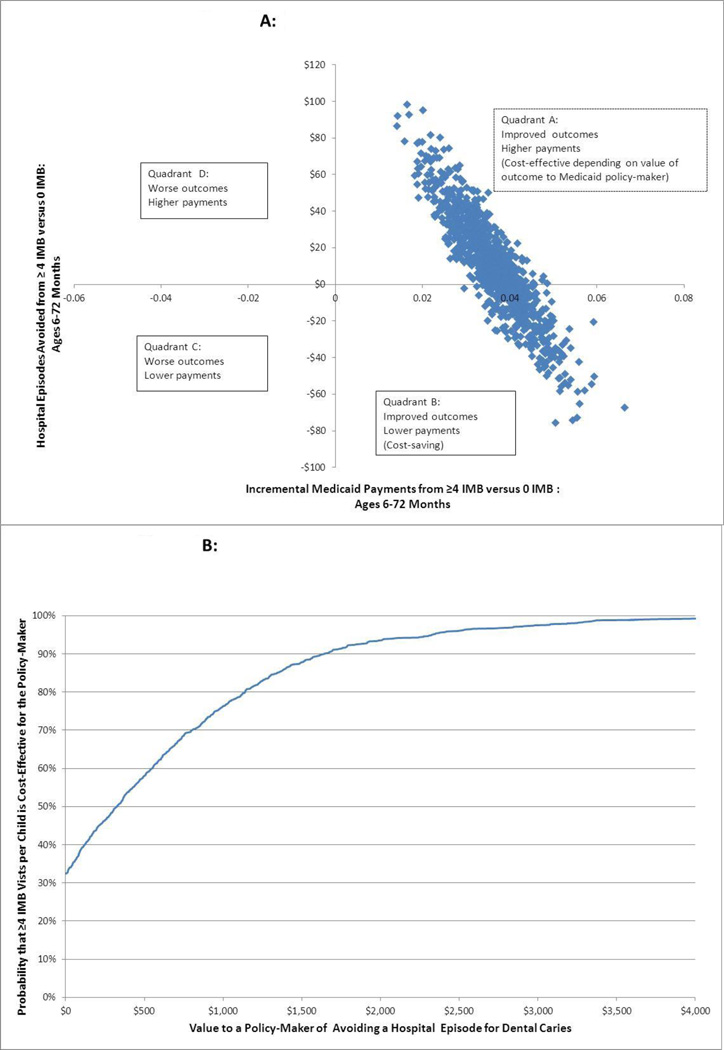
Table 3 provides estimates of the impact of ≥4 IMB visits on the key components of the ICER representing cumulative payments from 6 to 72 months old for the propensity score matched sample with discounting. The cumulative reduction in Medicaid payments for dental services is $231. Having ≥4 IMB visits was not cost-saving on average because the average IMB payment for this group was $242, or $11 more than the average reduction in dental payments. The bootstrap estimates in the cost-effectiveness plane (Figure 2A) show that having ≥4 IMB visits unambiguously averted hospital episodes and had a 32 percent chance of being cost-saving.
Table 3.
Cumulative Differences (≥4 IMB minus 0 IMB) in Payments and Hospital Episodes Averted (Aggregated over 6 to 72 Months of Age), Propensity Score Matched Sample with Discounting
| Discounted# | |
|---|---|
| Incremental Dental Payments | −$231 |
| IMB Visit Payments @ $54.81 per IMB Visit | $242 |
| Incremental Hospital Episodes Averted | 0.0360 |
| Probability Cost-Saving @ $54.81 per IMB Visit | 32.0% |
| If IMB Visit Payment is $54.81: Willingness to Pay Needed per Hospital Episode Averted for 95% Probability that IMB is Cost-Effective | $2,331 |
| Max IMB Visit Payment for 100% Cost-Saving | $33.67 |
Dental payments discounted at 3% per year from age 3 onward. IMB visit payments, which all occur before age 3 and are not discounted, are calculated based on the mean number of visits (4.42) times $54.81 per visit.
Figure 2.
2A: Incremental Cost-Effectiveness Plane (Bootstrap Estimates from Propensity Score Sample with Discounting)
2B: Cost Effectiveness Acceptability Curve (Cost per Hospital Episode Avoided for Dental caries) Propensity Score Sample with Discounting
The CEAC in Figure 2B depicts the cost per hospital episode averted for the other 68 percent of the estimates in which IMB improved health (i.e., averted poor outcomes) but at some additional cost.30 Depending on a Medicaid policymaker’s value of averting hospital episodes (e.g., the value of avoiding the unmeasured costs such as pain and suffering as well as lost time at school or parental employment when a child is hospitalized), IMB may still be cost-effective. If Medicaid feels that avoiding a hospital episode for CRT is worth at least $2,331, the probability that providing ≥4 IMB visits to each Medicaid-enrolled child is cost-effective is 95 percent.
A lower visit payment could increase the likelihood that IMB is cost-saving as long as lowering the payment does not affect medical provider provision of services that contribute to IMB effectiveness. The last row of Table 3 shows that the estimated maximum amount that NC Medicaid could pay for an IMB visit to have virtual certainty that the program is cost-saving is $33.67.
We conducted sensitivity analyses for discounting and the full sample. Discounting usually decreases the cost-effectiveness of preventive programs because expenditures for preventive services occur in the short run, and savings in terms from reduced treatments for disease come later and are more heavily discounted. Providing estimates for the full sample is important because if selection is not a problem, then the full sample estimates are generalizable to the population. Without discounting, the likelihood that having ≥4 IMB visits is cost-saving increased to 47.9 percent, so the program is close to break-even. The estimated maximum payment per IMB visit that could achieve cost-saving with virtual certainty ranged from $30.93 (full sample with discounting) to $34.84 (propensity score matched sample without discounting).
DISCUSSION
This analysis shows that the provision of repeat oral health visits in medical offices reduces hospitalizations and office visits for dental CRT, but the implications for Medicaid payments are more nuanced. Assuming payment of $54.81 for an IMB visit, the probability that the program reduced total Medicaid program expenditures (i.e., was cost-saving) for hospital episodes was 32 percent. Dental caries involves costs beyond service payments,31 and the analysis did not adjust for the pain, suffering and indirect costs such as lost parental work time associated with CRT. Considering the value of avoiding unmeasured costs associated with hospitalizing a child, the IMB program is 95% likely to be cost-effective if Medicaid is willing to pay at least $2,331 to avert a hospital episode.
Currently, some states pay less for preventive oral health care in medical offices than the NC program, though the service package may be less comprehensive and/or physician participation may not be as high. The effectiveness of the various components of the IMB visit in NC cannot be separated. If the effectiveness is attributable primarily to fluoride varnish, then a lower payment for varnish alone (e.g., $15 as is paid in some states) could lead unambiguously to cost-savings. If screening, counseling and referral are important components that affected outcomes, then reimbursement for these services may be required to achieve similar outcomes. If the components that were effective could be provided at $34 per IMB visit, then the program would be cost-saving with virtual certainty based on this study.
Several factors limit the results. The use of observational data means the results may be affected by patient selection and may not be generalizable to the entire population. Children receiving ≥4 IMB visits had more well-child visits before age 3 than children not receiving any IMB visits; while well-child visits provide a good opportunity for IMB services, the propensity score matched sample may be healthier on average or more focused on good health practices than the rest of the full sample that did not receive IMB visits. If these children have worse dental health, then the potential reduction in treatments and payments from IMB could be greater for this group. The full sample results were close to the propensity score sample results, but selection based on unobserved factors could still bias the results. Furthermore, the study only assessed dental treatments rather than dental health. The IMB program probably decreased rates of dental caries and increased the rate of treatment for those experiencing dental disease.
In total, the IMB program improved dental health outcomes for Medicaid-enrolled children with a 32% chance of cost-saving. The benefits may be worth the extra Medicaid payments from a societal perspective that encompasses all the costs of dental caries. Identification of the most effective components of the IMB service package and the costs of those components could determine the most appropriate rate for the IMB services. If payment is set to achieve the medical provider and family participation rates experienced in NC, then preventive oral health services in medical offices can be cost-effective (depending on the valuation by the policy-maker) and possibly cost-saving.
ACKNOWLEDGMENTS
This study was supported by grant numbers R01 DE013949 and R03 DE017350 from the National Institute of Dental and Craniofacial Research (NIDCR). The content is solely the responsibility of the authors and does not necessarily represent the official views of the NIDCR or the National Institutes of Health (NIH). Sally C. Stearns is independent of any commercial funder, has full access to all the data in the study, and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Contributor Information
R. Gary Rozier, Email: gary_rozier@unc.edu.
Ashley M. Kranz, Email: akranz@unc.edu.
Bhavna T. Pahel, Email: bpahel@dentistry.unc.edu.
Rocio B. Quiñonez, Email: quinoner@dentistry.unc.edu.
References
- 1.Dye BA, Arevalo O, Vargas CM. Trends in paediatric dental caries by poverty status in the United States, 1988–1994 and 1999–2004. International Journal of Paediatric Dentistry. 2010;20(2):132–143. doi: 10.1111/j.1365-263X.2009.01029.x. [DOI] [PubMed] [Google Scholar]
- 2.Edelstein B, Chinn C. Update on disparities in oral health and access to dental care for America's children. Acad Pediatr. 2009 Nov-Dec;9(6):415–419. doi: 10.1016/j.acap.2009.09.010. [DOI] [PubMed] [Google Scholar]
- 3.Pahel BT, Rozier RG, Slade GD. Parental perceptions of children's oral health: The Early Childhood Oral Health Impact Scale (ECOHIS) Health and Quality of Life Outcomes. 2007;5 doi: 10.1186/1477-7525-5-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Vargas C, Monajemy N, Khurana P, Tinanoff N. Oral health status of preschool children attending Head Start in Maryland, 2000. Pediatr Dent. 2002 May-Jun;24(3):257–263. [PubMed] [Google Scholar]
- 5.Edelstein BL, Chinn CH. Update on disparities in oral health and access to dental care for America's children. Acad Pediatr. 2009 Nov-Dec;9(6):415–419. doi: 10.1016/j.acap.2009.09.010. [DOI] [PubMed] [Google Scholar]
- 6.Felland L, Lauer J, Cunningham P. Community Efforts to Expand Dental Services for Low-Income People. [Accessed 5/18/2011];Issue Brief: Findings for HSC. [ http://hschange.org/CONTENT/1000/. [PubMed] [Google Scholar]
- 7.American Academy of Pediatric Dentistry. Clinical guidelines on periodicity of examination, preventive dental services, anticipatory guidance, and oral treatment for children. Reference manual. 2007–2008 Available from: http://www.aapd.org/media/Policies_Guidelines/G_Periodicity.pdf. [PubMed] [Google Scholar]
- 8.American Academy of Pediatrics. Policy statement. Oral health risk assessment timing and establishment of the dental home. Pediatrics. 2003;111:1113–1116. doi: 10.1542/peds.111.5.1113. [DOI] [PubMed] [Google Scholar]
- 9.Yu SM, Bellamy HA, Kogan MD, Dunbar JL, Schwalberg RH, Schuster MA. Factors that influence receipt of recommended preventive pediatric health and dental care. Pediatrics. 2002 Dec;110(6):8. doi: 10.1542/peds.110.6.e73. [DOI] [PubMed] [Google Scholar]
- 10.Marinho VC, Higgins JP, Logan S, Sheiham A. Fluoride varnishes for preventing dental caries in children and adolescents. Cochrane Database Syst Rev. 2002;(3) doi: 10.1002/14651858.CD002279. CD002279. DOI: 002210.001002/14651858.CD14002279. [DOI] [PubMed] [Google Scholar]
- 11.Azarpazhooh A, Main PA. Fluoride varnish in the prevention of dental caries in children and adolescents: A systematic review. Journal of the Canadian Dental Association. 2008;74(1):73J–79J. [PubMed] [Google Scholar]
- 12.American Dental Association MAahwaoprpjrrfp. Report of the Council on Scientific Affairs. Evidence-based Clinical Recommendations:Professionally Applied Topical Fluoride. [Accessed May 25, 2011]; http://www.ada.org/sections/scienceAndResearch/pdfs/report_fluoride_exec.pdf. [Google Scholar]
- 13.Quinonez RB, Stearns SC, Talekar BS, Rozier RG, Downs SM. Simulating cost-effectiveness of fluoride varnish during well-child visits for medicaid-enrolled children. Archives of Pediatrics & Adolescent Medicine. 2006;160(2):164–170. doi: 10.1001/archpedi.160.2.164. [DOI] [PubMed] [Google Scholar]
- 14.Wennhall I, Norlund A, Matsson L, Twetman S. Cost-analysis of an oral health outreach program for preschool children in a low socioeconomic multicultural area in Sweden. Swedish Dental Journal. 2010;34(1):1–7. [PubMed] [Google Scholar]
- 15.Bader JD, Rozier RG, Lohr KN, Frame PS. Physicians' roles in preventing dental caries in preschool children: a summary of the evidence for the U.S. Preventive Services Task Force. Am J Prev Med. 2004 May;26(4):315–325. doi: 10.1016/j.amepre.2003.12.001. [DOI] [PubMed] [Google Scholar]
- 16.Rozier RG, Stearns SC, Pahel BT, Quinonez RB, Park J. How A North Carolina Program Boosted Preventive Oral Health Services For Low-Income Children. Health Affairs. 2010;29(12):2278–2285. doi: 10.1377/hlthaff.2009.0768. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.National Institute of Dental and Craniofacial Research and Centers for Disease Control and Prevention. Dental, Oral and Craniofacial Data Resource Center, Data Query System. [Accessed 2010 Jun 25]; http://drc.hhs.gov/.
- 18.Pahel BT, Rozier RG, Stearns SC, Quinonez RB. Effectiveness of Preventive Dental Treatments by Physicians for Young Medicaid Enrollees. Pediatrics. 2011;127(3):E682–E689. doi: 10.1542/peds.2010-1457. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Pierce KM, Rozier RG, Vann WF., Jr Accuracy of pediatric primary care providers' screening and referral for early childhood caries. Pediatrics. 2002 May;109(5):E82–E82. doi: 10.1542/peds.109.5.e82. [DOI] [PubMed] [Google Scholar]
- 20.Beil H, Rozier R. Primary health care providers' advice for a dental checkup and dental use in children. Pediatrics. 2010;126(2):e435–e441. doi: 10.1542/peds.2009-2311. [DOI] [PubMed] [Google Scholar]
- 21.American Academy of Pediatrics. Department of Community CaSA, editor. AAP programs promote dental services in physician's offices. 2010;32:24. [Google Scholar]
- 22.The Pew Center on the States. Reimbursing physicians for fluoride varnish: A cost-effective solution to improving access. [Accessed May 25, 2011]; http://www.pewcenteronthestates.org/uploadedFiles/wwwpewcenteronthestatesorg/Initiatives/Promotional_Items/Dental/Reimbursing_Physicians%20Factsheet.pdf?n=871. [Google Scholar]
- 23.Skold UM, Petersson LG, Birkhed D, Norlund A. Cost-analysis of school-based fluoride varnish and fluoride rinsing programs. Acta Odontologica Scandinavica. 2008;66(5):286–292. doi: 10.1080/00016350802293978. [DOI] [PubMed] [Google Scholar]
- 24.Lee JY, Bouwens TJ, Savage MF, Vann WF. Examining the cost-effectiveness of early dental visits. Pediatric Dentistry. 2006;28(2):102–105. [PubMed] [Google Scholar]
- 25.Kallestal C, Norlund A, Soder B, et al. Economic evaluation of dental caries prevention: a systematic review. Acta Odontologica Scandinavica. 2003 Dec;61(6):341–346. doi: 10.1080/00016350310007815. [DOI] [PubMed] [Google Scholar]
- 26.Rosenbaum PR, Rubin DB. The central role of the propensity score in observational studies for causal effects. Biometrika. 1983;70(1):41–55. 1983. [Google Scholar]
- 27.Guo S, Fraser M. Propensity score analysis: statistical methods and applications. Thousand Oaks, CA: 2010. [Google Scholar]
- 28.Economic Research Service. Measuring rurality: Rural-urban continuum: United States Department of Agriculture. [Accessed November 2006];2005 Available at: http://www.ers.usda.gov/briefing/rurality.
- 29.North Carolina Oral Health Section. County-level water fluoridation data. Raleigh, NC: NC Department of Health and Human Services; 2007. [Google Scholar]
- 30.Fenwick E, O'Brien BJ, Briggs A. Cost-effectiveness acceptability curves - facts, fallacies and frequently asked questions. Health Economics. 2004 May;13(5):405–415. doi: 10.1002/hec.903. [DOI] [PubMed] [Google Scholar]
- 31.Casamassimo PS, Thikkurissy S, Edelstein BL, Maiorini E. Beyond the dmft The human and economic cost of early childhood caries. Journal of the American Dental Association. 2009 Jun;140(6):650–657. doi: 10.14219/jada.archive.2009.0250. [DOI] [PubMed] [Google Scholar]