Abstract
Aim.
To determine the influence of sociodemographic factors on patients´ satisfaction with health care system.
Methods.
In a cross-sectional study, 1,995 patients from 12 municipalities of Zenica-Doboj Canton were interviewed after a visit to the practice. Individual interviews were conducted and the questionnaire was made on the basis of EUROPEP (European Task Force on Patient Evaluations of General Practice Care) standardized questionnaire.
Results:
Out of the total number patients, 47.1% were females, 47.9% were from urban population and median of age was 42.0 years (IQR = 30.0 to 53.0 years). The rural population was more likely to buy drugs for medical treatment (p < 0.001) and parenteral injections in primary care practice (p < 0.001). Patients with lower level of education were more likely: to be ordered for physical examination (p = 0.001), to buy drugs for medical treatment (p = 0.001), to buy parenteral injections in primary care practice (p < 0.001); to pay unofficially to someone from medical staff (p < 0.001); to feel that they could be better treated (p = 0.032) and they had longer waiting for health service in primary care practice (p < 0.001). Older population had better assessment of secondary (p = 0.040) and tertiary health care practices (p = 0.034); needed more time is needed to reach health facilities (p = 0.016), longer waiting for health service in primary care practice (p < 0.001); more likely to have health problems in the past 12 months but they did not request medical treatment (p = 0.008); more likely to be ordered for physical examination (p < 0.001); more likely to buy drugs for medical treatment (p = 0.004); more likely to buy parenteral injections in primary care practice (p < 0.001).
Conclusion:
The following variables: gender, age, overall perception of health status and financial status appear to be predictors of patients´ satisfaction.
Keywords: patients´, satisfaction, sociodemographic characteristics, health system assessment
1. INTRODUCTION
Measuring healthcare quality and improving patients´ satisfaction have become increasingly prevalent, especially among healthcare providers and purchasers of healthcare (1). Surveys of patients are increasingly used internationally as an indicator of the performance of health systems (2). Systematic gathering of information on patients’ needs and experiences, using methodologically-sound instruments such as validated questionnaires, should therefore be an integral part of routine care (3). Results of regular application of such instruments can be used in health systems for quality improvement and clinical governance, as well as to compare the quality of services between care providers (4). In recent years, many health systems have focussed their attention to patients needs, satisfaction and its determinants in order to meet these challenges, to become more effective and to provide patient-centred clinical environment. However, the relationship between patient satisfaction and health care utilization, expenditures, and outcomes remains ill defined (5). A key way to measure whether care is patient-centered is by surveying people who have had contact with the health care system (6). The factors with the clearest relationship to satisfaction include the accessibility of medical care, the organizational structure of clinics, treatment length, perceived competence of physicians, clarity and retention of physicians’ communication to patients, physicians’ affiliative behavior, physicians’ control and patients’ expectations (7). According to the B&H Constitution Law Health Care System is regulated on the entity level. Republic of Srpska has centralized system, Federation of B&H has decentralized system and care is organized on canton’s level. FB&H has ten cantons, every canton has independent Ministry of health responsible for organization of health care system on primary level (Health centres with General Practitioners of Family Medicine offices), on secondary level (polyclinics and cantonal hospitals) and on tertiary level (general hospitals, special hospitals and university hospitals – university clinical centres) (8). The one of the principal reform of health system in FB&H is focused on strengthening of primary health care and rationalization of hospital care. There are no reliable data dealing with the satisfaction of patients within health care system in FB&H, and we aimed our study to determine patients’ satisfaction with the health care on primary care level in one canton in Federation of Bosnia and Herzegovina, in order to identify the sociodemographic factors influencing it.
2. METHOD
A cross-sectional study was conducted and included all 12 municipalities of Zenica-Doboj Canton.
Subjects
A stratified sample of 146 primary health care practices was recruited. We aimed at a sample of at least 1,806 patients (12 per practice) to provide a reliable comparison among urban and rural population (α = 0.05, P = 0.80 and minimal expected difference in satisfaction = 5%). The achieved number of patients was 1,995 (14 per practice). The study were included patients with recent experience in general practice, aged 18 years or older.
Procedures
Individual interviews were conducted in one randomly selected day of the week, except Monday and Friday.
Instruments and variables
The questionnaire was made on the basis of EUROPEP standardized questionnaire, related to the patient satisfaction with a health care (9,10,11). This questionnaire consists of 44 questions, including demographic data and evaluations of different aspects of care (the quality of physical examination and medical treatment conducted by physician; professional conduct of hospital staff at admission and during the hospital stay; conduct of health care professionals in dealing with the patient and satisfaction with primary, secondary and tertiary health care practices). A patient satisfaction was rated on a 5 point scale, response categories being poor, fair, good, very good, and excellent.
Statistical analysis
Statistical analysis was performed using the IBM SPSS version 21.0 for Windows system (SPSSInc., Chicago, Illinois, USA). Data are presented as mean ± standard deviation or as median with interquartile range (IQR, 25th to 75th percentiles) dependent on normality of variables distribution. The Kolmogorov–Smirnov statistic with a Lilliefors significance level was used for testing normality of distribution. In the case of categorical variables, counts and percentages were reported. A logistic regression was applied and each item is recoded for statistical analysis as a dichotomous variable. A five point scale of patient´s satisfaction was distributed in two categories: unsatisfied (poor or fair) and satisfied (good, very good and excellent) patients. A p-value <0.05 was considered as significant.
3. RESULTS
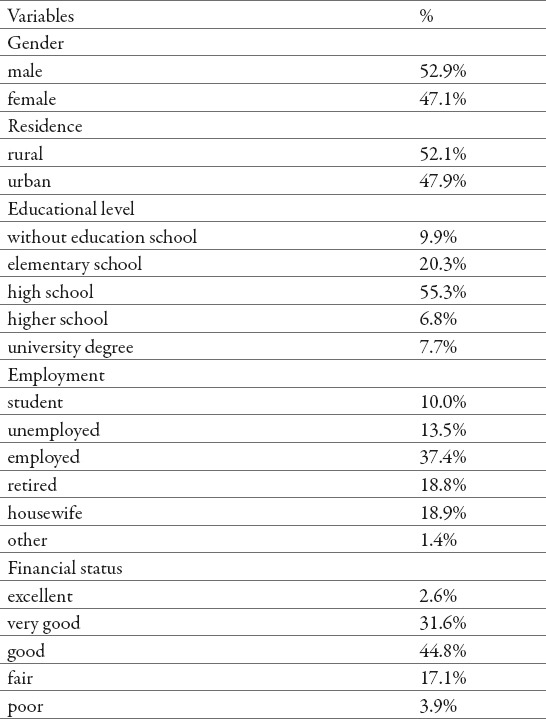
Out of total number (n=1 995), 47.1% were females; 47.9% was urban population and median of age was 42 years (IQR = 30 to 53 years). More than half of patients (69.8%) had finished high school or higher education. One third of patients or 34.2% was rated their own financial status as very good or excellent, 44.8% as good and 21.0% as poor or fair (Table 1).
Table 1.
Socio-demographic characteristics of patients
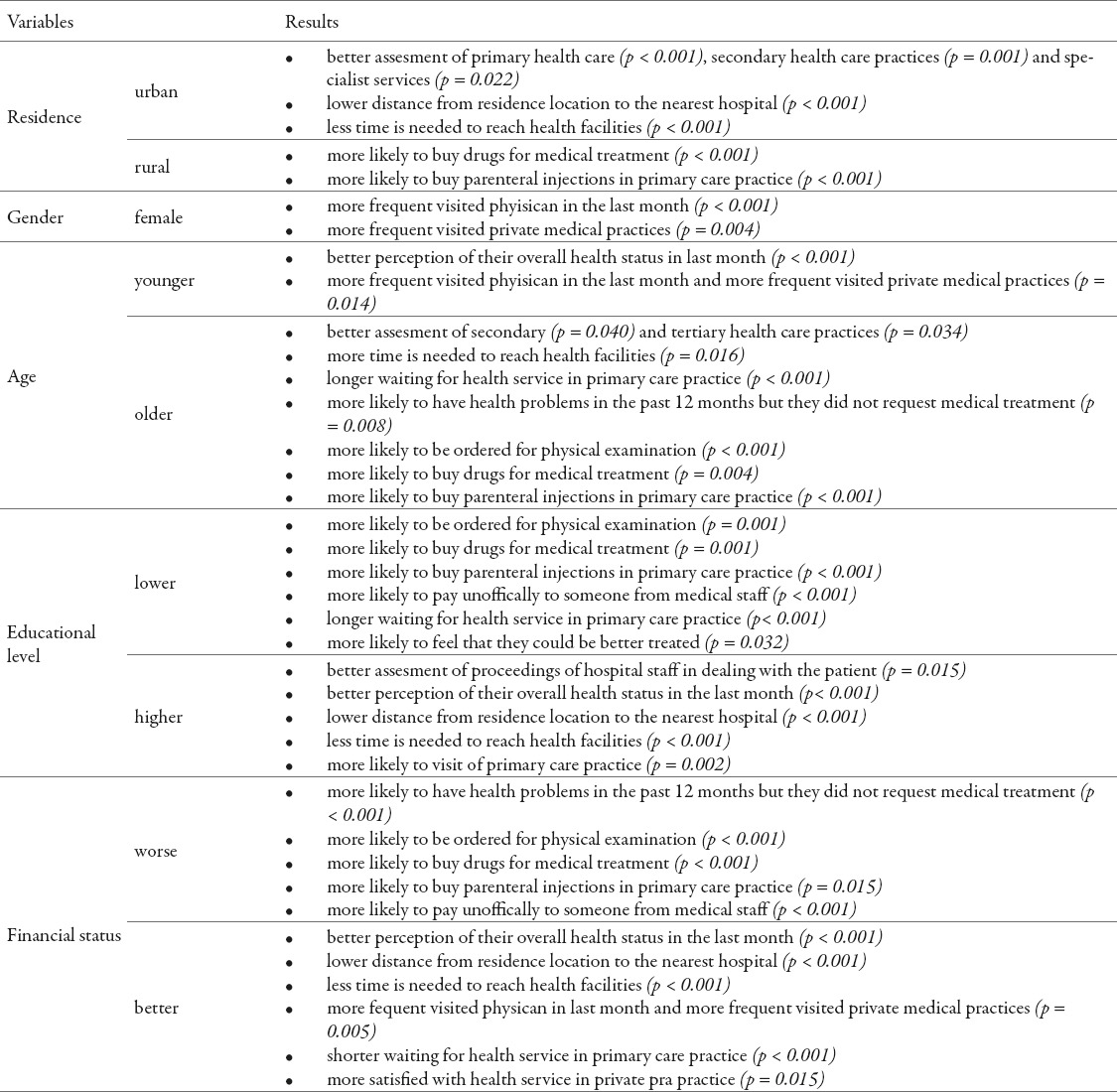
The influence of patient-based factors on reported satisfaction with health care system presented in table 2.
Table 2.
Cluster of socio-demographic variables in assesment of patients´satisfaction
The logistic regression model was statistically significant in assessment of patients´ satisfaction with physical examination and medical treatment by physician for urban (χ2 = 68.505; df = 5; p < 0.001; R2CS = 0.074) and rural population (χ2 = 50.354; df = 5; p < 0.001; R2CS = 0.051). Of the five predictor variables only three were statistically significant for urban population: gender (p = 0.024), age (p < 0.001) and overall perception of health status (p < 0.001); for rural population: age (p < 0.001), overall perception of health status (p < 0.001) and financial status (p < 0.001). Advanced age and overall perception of health status was correlated with an increased likelihood of patients’ satisfaction, females had 1.39 times higher odds to manifest satisfaction with physical examination and medical treatment than males in urban population. In rural population, for a one-unit increase in overall perception of health status and financial status there is an increase of 48.3% and 37.7% in the odds of being fulfilled with physical examination and medical treatment, respectively (Figure 1).
Figure 1.
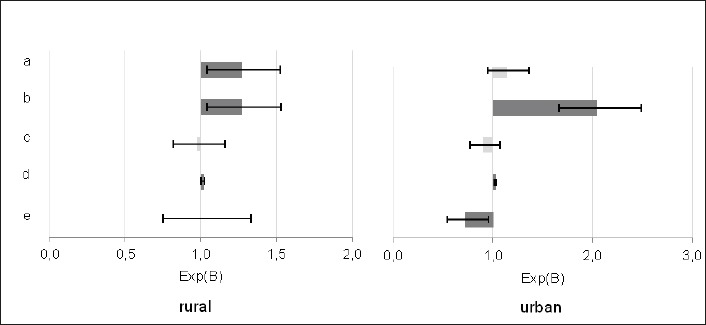
A logistic regression was performed to ascertain the effects of financial status (a), overall perception of health status (b), educational level (c), age (d) and male gender (e) on patients´ satisfaction with physical examination and medical treatment by physican. The logistic regression model was statistically significant in both rural (p < 0.001; R2CS = 0.051) and urban population (p < 0.001; R2CS = 0.074).
The logistic regression model was not statistically significant in assessment of patients´ satisfaction with professional conduct of hospital staff at admission for urban (p = 0.078) and rural population (p = 0.079) and with professional conduct of hospital staff during hospital stay for urban population (p = 0.206). The logistic regression model is not statistically significant in assessment of patients´ satisfaction with professional conduct of hospital staff during hospital stay for rural population (χ2 = 16.506; df = 5; p = 0.006; R2CS = 0.046), for a one-unit increase in overall perception of health status (p = 0.020) there is about 42.5% in the odds of being fulfilled with professional conduct of hospital staff during hospital stay. The logistic regression model was statistically significant in assessment of patients´ satisfaction with professional conduct of hospital staff in dealing with the patient for urban (χ2 = 31.580; df = 5; p < 0.001; R2CS = 0.035) and rural population (χ2 = 32.432; df = 5; p < 0.001; R2CS = 0,033). In urban population, advanced age was correlated with an increased likelihood of patients´ satisfaction with professional conduct of hospital staff in dealing with the patient (p = 0.003) and for a one-unit increase in overall perception of health status there is about 66.2% increase in the odds of being fulfilled (p < 0.001). In rural population, for a one-unit increase in overall perception of health status (p = 0.004) and financial status (p = 0.002) there is 34.9% or 39.5% increase in the odds of being fulfilled with professional conduct of hospital staff in dealing with the patient, respectively (Figure 2).
Figure 2.
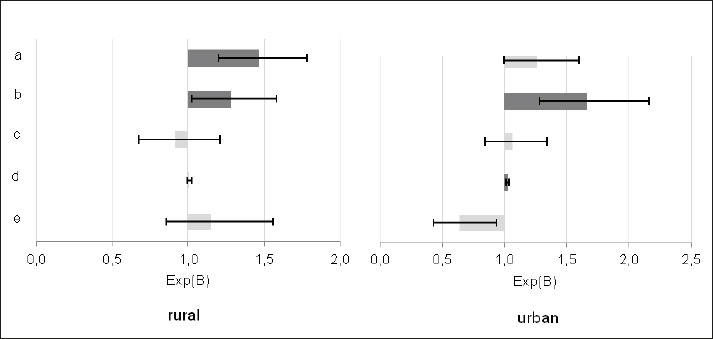
A logistic regression was performed to ascertain the effects of financial status (a), overall perception of health status (b), educationa level (c), age (d) and male gender (e) on patient´s satisfaction with proceedings of hospital staff in dealing with the patient. The logistic regression model was statistically significant in rural (p<0.001; R2CS=0.033) and urban population (p<0.001; R2CS=0.035).
The logistic regression model was statistically significant in patients´ satisfaction with primary health care for urban (χ2 = 23.205; df = 5; p < 0.001; R2CS = 0.026) and rural population (χ2 = 40.980; df = 5; p < 0.001; R2CS = 0.041). In urban population, advanced age was associated with an increased likelihood of patients´ satisfaction with primary health care (p <0.001) and for a one-unit increase in overall perception of health status (p = 0.003) and financial status (p = 0.049), there is about 31.3% or 19.4% in the odds of being fulfilled, respectively. In rural population, for a one-unit increase in overall perception of health status (p = 0.047) and financial status (p < 0.001) there is about 17.7% or 56.7% in the odds of being fulfilled with primary health care, respectively. The logistic regression model was statistically significant in patients´ satisfaction with secondary health care for urban (χ2 = 32.769; df = 5; p < 0.001; R2CS = 0.126) and rural population (χ2 = 54.033; df = 5; p < 0.001; R2CS = 0.119). In urban population, advanced age were correlated with an increased likelihood of patients’ satisfaction with secondary health care (p <0.001) and for a one-unit increase in overall perception of health status (p < 0.001), there is 2.33 times higher odds of being fulfilled. Females had 1.95 times higher odds to manifest satisfaction with secondary health care than males in urban population (p = 0.027). In rural population, advanced age was correlated with an increased likelihood of patients satisfaction with secondary health care (p <0.001) and for a one-unit increase in overall perception of health status (p < 0.001) we expect to see 2.2 times higher odds of being satisfied. The logistic regression model was statistically significant in patient satisfaction with tertiary health care for urban (χ2 = 43.625; df = 5; p < 0.001; R2CS = 0.053) and rural population (χ2 = 21.829; df = 5; p = 0.001; R2CS = 0,028). In urban population, advanced age was associated with an increased likelihood of patients satisfaction with tertiary health care (p <0.001) and for a one-unit increase in overall perception of health status (p < 0.001) and financial status (p = 0.011) there is 59.0% or 29.5% in the odds of being fulfilled with tertiary health care, respectively. In rural population, for a one-unit increase in overall perception of health status (p = 0.002) and financial status (p = 0.036) there is 34.5% or 21.9% in the odds of being fulfilled with tertiary health care, respectively.
4. DISCUSSION
In this paper we presented the results of the survey conducted in Zenica-Doboj Canton in Federation of B&H about patients’ satisfaction with health care system. The study of Marjanovic et al., argued that health professionals re-training and the application of principles of family medicine contribute to patients’ satisfaction and consequently improved primary health care. Theirs results indicate that every sixth patient (16.4%) in general medicine waits for admission in doctor’s office more than an hour or 45.9% of patients wait longer than half an hour, while in family medicine, the number of patients waiting over an hour is 0.6%, and that 5.8% of patients wait more than half an hour (12). In our study, every fourth patient (24.2%) waits for admission in primary health care more than 15 minutes, for 47.8% the waiting time is between 16-30 minutes and for 19.0% patients the waiting time is in range of 31 to 60 minutes. Only one eleventh of patients waits (8.9%) more than 60 minutes. In the study of Sing et al., the average waiting time was 2 hours and 40 minutes, which is in accordance with the waiting time of thirty minutes in primary health care in developed countries (13). Prolonged waiting time was associated with lower patient satisfaction (p < 0.05). In opposite, amount of time spent in physician’s office is the strongest predictor of patient satisfaction (14). In our study, more than half of patients or 59.4% were satisfied (categories very good or good) with physical examination and medical treatment. In the study of Bleich et al., were explored what determines people’s satisfaction with the health-care system besides of their patients’ experience proper. Factors as patient expectations, health status, type of care, and immunization coverage were marked as significant predictors of health system satisfaction; although all of them put together explained only 17.5% of the observed variation, while broader societal factors might largely account for the unexplained portion of satisfaction with the health-care system (15). Previously studies concluded that older patients are more satisfied with health care (16,17), which is in correlation with our results. In our study, the number of variables as gender, age, overall perception of health status and patients’ financial status were predictors significant of patients’ satisfaction, both in urban and in rural population. Our results cannot be representative for the planning of public health policy but can certainly point out to weaknesses of health system and contribute its reform in Federation of Bosnia and Herzegovina-B&H.
5. CONCLUSION
The patients’ gender, age, overall perception of health status and patients’ financial status appear to be the significant predictors of patients´ satisfaction. These results were obtained in survey in one canton level and it would be recommended to continue with research in remaining nine cantons of the FB&H, using the same methodology. We believe that the results obtained in such manner and compared will provide a new insight and facilitate the health system reform. A comparison with results in the region and worldwide should be interesting, too.
Footnotes
CONFLICT OF INTEREST: NONE DECLARED.
REFERENCES
- 1.Soufi G, et al. Patient satisfaction in an acute medicine department in Morocco. BMC Health Services Research. 2010;10:149. doi: 10.1186/1472-6963-10-149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Salisbury c, Montgomery AA. Patients’ experience and satisfaction in primary care: secondary analysis using multilevel modelling. BMJ. 2010;341:c5004. doi: 10.1136/bmj.c5004. doi: 10.1136/bmj.c5004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Strasbourg: Council of Europe; 1997. Council of Europe. Recommendation number R(97)17 of the Committee to Member States on the development and implementation of quality improvement systems (QIS) in health care. [Google Scholar]
- 4.Grol R, et al. Patients in Europe evaluate general practice care: an international comparison. British Journal of General Practice. 2000;50:882–887. [PMC free article] [PubMed] [Google Scholar]
- 5.Fenton JJ, Jerant AF, Bertakis KD, Franks P. The Cost of Satisfaction. A National Study of Patient Satisfaction, Health Care Utilization, Expenditures, and Mortality. Arch Intern Med. 2012;172(5):405–411. doi: 10.1001/archinternmed.2011.1662. [DOI] [PubMed] [Google Scholar]
- 6.Browne K, Roseman D, Shaller D, Edgman-Levitan S. Analysis & commentary Measuring Patient Experience As A Strategy For Improving Primary Care. Health Aff. 2010;29(5):921–925. doi: 10.1377/hlthaff.2010.0238. [DOI] [PubMed] [Google Scholar]
- 7.Lochman JE. Factors related to patients’ satisfaction with their medical care. Journal of Community Health. 1983;9(2):91–109. doi: 10.1007/BF01349873. [DOI] [PubMed] [Google Scholar]
- 8.Masic I, Novo A, Pilav A, Jokic I, Toromanovic S. Health care system in Federation of Bosnia and Herzegovina. Mater Sociomed. 2006;18(4):212–218. [Google Scholar]
- 9.Vedsted P, Sokolowski I, Heje HN. Data quality and confirmatory factor analysis of the Danish EUROPEP questionnaire on patient evaluation of general practice. ScandJ Prim Health Care. 2008;26:174–180. doi: 10.1080/02813430802294803. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Bjertnaes OA, Lyngstad I, Malterud K, Garratt A. The Norwegian EUROPEP questionnaire for patient evaluation of general practice: data quality, reliability and construct validity. Fam Pract. 2011;28:342–349. doi: 10.1093/fampra/cmq098. [DOI] [PubMed] [Google Scholar]
- 11.Brandao AL, Giovanella L, Campos CE. Evaluation of primary care from the perspective of users: adaptation of the EUROPEP instrument for major Brazilian urban centers. Cien Saude Colet. 2013;18:103–114. doi: 10.1590/s1413-81232013000100012. [DOI] [PubMed] [Google Scholar]
- 12.Marjanovic M, Omanic A. Satisfaction of the health services users in general practice and family medicine policlinics - A cros-sectional study. Medical journal. 2012;18(4):284–287. [Google Scholar]
- 13.Sing H, Haqq ED, Mustapha N. Patients perceptions and satisfactions with health care proffesionals at primary health care facilities in Trinidad and Tobago. Bull World Health Organ. 1999;77:356–360. [PMC free article] [PubMed] [Google Scholar]
- 14.Anderson RT, Camacho FT, Balkrishnan R. Willing to wait?: The influence of patient wait time on satisfaction with primary care. BMC Health Services Research. 2007;7:31. doi: 10.1186/1472-6963-7-31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Bleich SN, Ozaltin E, Murray CK. How does satisfaction with the health-care system relate to patient experience? Bull World Health Organ. 2009 Apr;87(4):271–278. doi: 10.2471/BLT.07.050401. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Hargraves JL, et al. Adjusting for patient characteristics when analyzing reports from patients about hospital care. Med Care. 2001;39:635–641. doi: 10.1097/00005650-200106000-00011. [DOI] [PubMed] [Google Scholar]
- 17.Jaipaul CK, Rosenthal GE. Are older patients more satisfied with hospital care than younger patients? J Gen Intern Med. 2003;18:23–30. doi: 10.1046/j.1525-1497.2003.20114.x. [DOI] [PMC free article] [PubMed] [Google Scholar]


