Abstract
Background:
Agonist maintenance therapy with methadone is amongst the preferred remedies for treating opioid dependence and is increasingly supported by the regional governments in this part of the world. In this study we have investigated the clinical manifestations and factors affecting the outcome of therapy in patients with methadone poisoning in a Middle-Eastern (Iranian) referral tertiary care University hospital.
Methods:
In this prospective and descriptive-analytic study which was done in a tertiary care and referral University hospital in Iran (2012-2013) all of the admitted patients with a clear and reliable history of methadone poisoning (n=433) were included and demographic data, Clinical status on admission including Glasgow Coma Scale (GCS) score, time elapsed from ingestion to hospital admission, average dose of naloxone used, any history of psychiatric disorder, type of toxic exposure, co ingestion of other medication, hospitalization time and the outcome were recorded and statistically analyzed.
Results:
The average length of hospital stay was 33 ± 26 hours. 80.1% of patients had ingested methadone alone, and 90.3% survived. Complications were pulmonary edema (7%), aspiration pneumonia (1.4%), generalized tonic colonic seizure (0.9%), and renal failure (0.5%). GCS, systolic blood pressure and respiratory rate were lower in fatal cases and GCS had prognostic value for the outcome of therapy in methadone intoxicated patients. Patients with higher GCS on admission had better outcome [OR =0.47 (95% CI: 0.38-0.580); P value< 0.0001].
Conclusion:
Admission time GCS score maybe considered as an important predictor for the outcome of therapy in methadone poisoning.
Keywords: Methadone, Overdose, Opiate Substitution Therapy
1. INTRODUCTION
Abuse of opium and its natural and synthetic derivatives is still a sizeable health care problem in the Middle East region (1) which is rooted in many socioeconomic factors (2). Agonist maintenance therapy with methadone is amongst the preferred remedies for treating opioid dependence (3, 4) and is increasingly supported by the regional governments in this part of the world (5, 6). On the other hand, widespread uses of methadone in the community based addiction treatment facilities in Middle Eastern countries raised many cases of intentional and unintentional methadone toxicity (7) in which the role of genetic predisposition is not ignorable (8). Methadone poisoning may occur from overdose due to abuse of narcotic substance; accidentally by children or elderly; or intentionally for suicidal purposes (9). This may be due to the large number of addicted patients under methadone maintenance therapy (MMT) protocol and also methadone availability to other family members. Moreover, pharmaceutical companies usually prepare methadone for the purpose of MMT as a solution with a sweet fruit taste and this may attract young children as well (10).
Classical manifestations of poisoning are central nervous system (CNS) depression, miosis and respiratory depression which may last for several days due to the long lasting effects of methadone (11). Nearly 25% of death cases with methadone poisoning have been reported in the first 14 days starting on methadone maintenance treatment with opioids (12).
Notably methadone maintenance therapy facilities do not use the same guideline in Iran and some other countries in the Middle East region, and methadone with its long lasting effects is more or less available in some community pharmacies for many of people. Moreover, our physicians’ education about the general clinical features of methadone toxicity in this region is limited. Hence, in this study we have investigated the clinical manifestations and factors affecting the outcome of therapy in patients with methadone poisoning in a Middle-Eastern (Iranian) referral tertiary care University hospital.
2. PATIENTS AND METHODS
This cross-sectional study was done in the department of toxicological emergencies of Noor and Ali-Asghar [PBUH] University hospital affiliated to the Isfahan University of Medical Sciences, Isfahan from September 2012 to September 2013. This center which is the major referral medical center for toxicological emergencies for the central part of Iran, is facilitated, staffed and designed for the management of poisoned patients and approximately 400 poisoned patients are admitted to it monthly.
The study protocol was approved by the institutional board of human studies at Isfahan University of Medical Sciences (Registration number: IUMS 391261). In addition, before the inclusion of patients to this study, the whole study were explained to each of them separately and they had the option to fill in a written consent form and entering the study. If the patient was not able or had not the capacity for decision making, informed consent for inclusion to this study were taken from the patients’ first degree family.
All patients with a clear and reliable history of methadone poisoning whom were hospitalized in the poisoning emergencies ward and poisoning intensive care unit during the above mentioned period were investigated. Patients who had been discharged by their own consent were excluded from the study. Demographic data (age, gender, route of poisoning,), Clinical status on admission including vital signs and Glasgow Coma Scale (GCS) score, time elapsed from ingestion to hospital admission, average dose of naloxone used, any history of psychiatric disorder, type of toxic exposure (under MMT program, accidental, intentional), co ingestion of other medication, hospitalization time and the outcome (survived with or without complication and death) were recorded.
Data was analyzed by SPSS 20 (SPSS, Chicago, IL, USA). ANOVA, Chi-square, or Fisher Exact Test were used. P value less than 0.05 was considered to be statistically significant. Binary backward step logistic regression was used for predicting factors in outcome (Survived or death). The results were presented as mean (SE) or number (%) where appropriate.
3. RESULTS
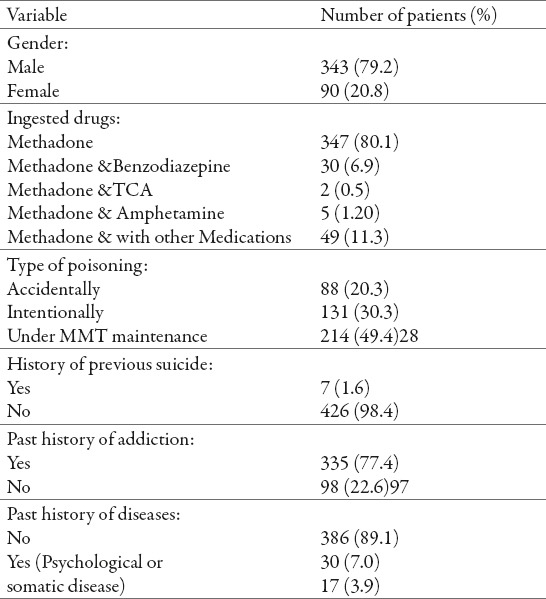
During the defined period of the study 433 patients (79.2 % men) with methadone poisoning were completely investigated. 347 patients (80.1%) had ingested only methadone and 86 patients (19.7%) had ingested other medications with methadone. Demographic and general characteristics of the study patients are presented in Table 1.
Table 1.
Demographic and general characteristics of the study patients (n=433). MMT: methadone maintenance treatment. TCA: tricyclic antidepressant
The average interval between methadone ingestion by the study patients and the first medical care was 6.6 ± 1.1 hours (range: 1-125 hours). Treatments offered to the patients included gastric evacuation which was performed for 33 patients (7.6%), activated charcoal administration for 42 patients (9.7%). Naloxone was prescribed for 253 patients. Average dose of naloxone used during the hospitalization period of the study patients was 1.3 ± 0.15 mg.
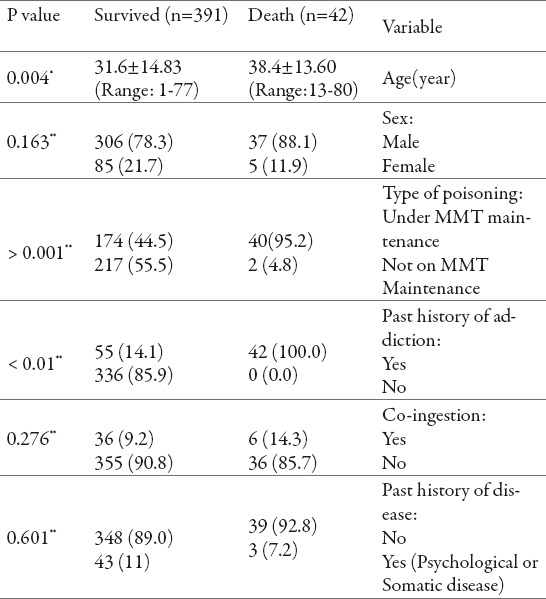
A total of 387 patients were survived and 46 patients died. Complications observed in some patients including pulmonary edema in 30 patients; aspiration pneumonia in six, and renal failure was observed in two cases. Four patients had brief generalized tonic colonic seizure. With respect to outcome there were significant differences in age, gender, type of poisoning, past history of diseases and co ingestion (Table 2). Most of died patients had been under MMT treatment.
Table 2.
Comparison of different characteristics of the study patients with respect to outcomes. The results are presented as mean ± SD or N (%). SD: standard deviation. *independent t-test, **Fisher exact test
The Glasgow coma scale (GCS) score, systolic blood pressure and respiratory rate was lower in fatal cases (Table 3).
Table 3.
Clinical manifestations of patients with methadone poisoning with respect to outcomes *independent t-test, **Fisher exact test
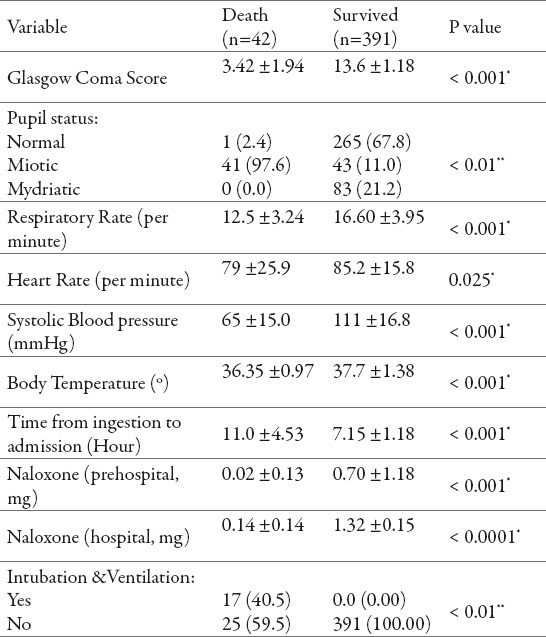
Among all different studied variables, GCS score had prognostic value for the outcome of therapy in methadone intoxicated patients. Patients with higher GCS score on admission had better outcome [OR 0.47 (95% CI: 0.38-0.580); P value< 0.0001]. The average length of hospital stay was 32.99 ± 25.98 hours.
4. DISCUSSION
The general purpose of this study was to determine epidemiological and clinical characteristics of the Iranian patients poisoned with methadone. According to the results obtained from this study, 60% of the methadone poisoned patients were in the young age group which is compatible with previous studies (3, 13). Most of the poisoning cases were addicts’ patients. According to our finding from patients’ history, the most important factor in poisoning with methadone was the easiness of its availability in community pharmacies, MMT facilities or street markets. Family members of the abuser would also be predisposed for accidental or intentional overdose as well. Hence, access limitation to methadone and prevention of its sale, can be considered an appropriate approach to prevent and reduce methadone poisoning.
Pharmaceutical dosage form of methadone and the easiness of consumption are other factors we should be considered effective on the toxico-epidemiology of this drug. Available Methadone formulations in Iran are syrup and tablet. In a recent study, the difference between the characteristics of methadone poisoning in syrup and tablet formulation is discussed. In this study the average dose of ingested methadone in syrup and tablet dosage form was reported 153±3 and 88±3 respectively. Authors concluded that higher doses of methadone in the syrup form may exert a similar severity of poisoning and outcomes compared to lesser doses of that in the tablet form. Similarities in outcomes, despite differences in exposure history, may reflect relatively prompt transfer to hospital and adequate provision of clinical care, including supportive care and naloxone (14). They have also recommend for the use of child-resistant containers for dispensing syrup, reduction in methadone concentration, adding a coloring agent, special flavor, and education of patients on the safe storage of methadone in their home in order to reduce the occurrence of accidental poisonings (14). In present study we have not separated patients in terms of the dosage form of methadone they have consumed. Questionable reliability of these kinds of data in these patients which were mostly addict was the most important reason.
Our results supports our previous study in which previous suicidal attempts, age, gender and a history of psychiatric disorders have predictive value for the outcome in methadone acute poisoning (9). In our present study most of the deceased patients had been under MMT program. Some of them were under MMT treatment before poisoning and some of them had stopped MMT for a while and restarted methadone use again by themselves with the last ingested dose. Some previous studies indicated the incidence of methadone poisoning symptoms in the same situation (15, 16). Mixed-drug poisoning was an important cause of death in our patients.
Moreover, methadone poisoning can also occur either intentionally or accidentally. In our study, 30.3% of the patients had intentionally used the drug and this means that addicts under MMT program also need to be evaluated by a psychiatric consultant as well.
According to our results, the pupils’ size, level of consciousness, heart rate and respiratory rate of the poisoned patients on hospital admission were statistically different between patients with respect to outcome (Table 3). This is consistent with some previous studies which have shown that miosis is an important symptom of methadone poisoning (17, 18). However in Caplehorn’s study, the most common initial symptom of methadone poisoning has been reported to be euphoria, slurred speech and ataxia (19). The difference in the admission clinical symptoms could be attributed to the difference in the severity of poisoning cases on admission and the amount of methadone ingested.
The systolic blood pressure of our poisoned patients was also lower in patients who died compared to the survived ones. In the study by Afshari et al., methadone poisoning also caused a considerable drop in the systolic blood pressure (20). Our results also showed that critical symptoms (table 3) of the patients at the time of admission to our center showed that respiratory rate of the patients was significantly different from that of the nonfatal patients, which may be due to intentional ingestion and severity of toxicity.
Factors affecting the outcome of therapy in methadone poisoning is previously reviewed elsewhere (21). According to the results of this study, 25.8% of the intentionally poisoned patients and 12.3% of the unintentionally poisoned ones had a history of psychiatric disease and this difference was statistically significant (p=0.001). In another study it was shown that there is a significant relationship between addiction, mental disorder and suicide and that most of the addict patients committing suicide had a mental disorder background (16). Meanwhile, 24% of the addicts, 15.8% of the non-addicts and 21.4% of the quitting addicts in our study patients had a mental disorder background. Similarly, in the study of Mégarbane et al., tendencies to commit suicide have been reported in the methadone poisoning patients more than the other cases (22). Brands et al., have also shown that the psychiatric problems in the methadone poisoned patients were considerably more than the other patients (23). In Mc Cowan’s study, hospitalization rate of methadone poisoned patients in the psychiatric unit has been significantly more than the normal ones (24). This comorbidity may necessitate the importance of educational programs at the community level for prevention of suicidal attempts in normal non-addict patients with psychiatric disorders and also a continuous educational program for patients with access to methadone drug especially patients on methadone maintenance treatment (25).
We also found a significant difference in the outcome in terms of gender. Most of the patients died were men. In Bernard’s study, most people who have died from methadone poisoning were men (26). Here despite the fact that this difference is statistically significant, we think due to the large difference between the number of men and women in our study, we should mention this data cautiously.
In this study there was a significant difference between the outcome with respect to co-ingestion of other medications. In a study performed by Concool and colleagues, fatality of patients had not been attributed to the mass methadone ingestion alone and alcohol abuse had been reported prominently in most of the deceased cases (27). However in our study only 4.2% of the fatal cases had ingested other medication with methadone.
In our study, patients who were received higher doses of naloxone had a better outcome of therapy. This may necessitate reconsideration of para-medical guidelines for administering naloxone by para-medic personnel or non-toxicologist health care professionals who deal with methadone intoxicated patients in Iran.
Our study had some limitations. One of them was calculating row odds ratio instead of adjusted odds ratio and we think the readers should consider this point on interpreting our results.
5. CONCLUSION
In addition to previously reported factors, GCS score at the time of hospital admission in patients with acute methadone intoxication is an important predicting factor for the outcome of therapy in these patients. Furthermore, considering the high incidence rate of fatal cases of methadone poisoning among the addicts patients under MMT programs in our region (according to our results), regulatory legislations for more restricted control on MMT facilities is recommended. Besides, considering that dose adjustment for methadone for every individual addict with different metabolisms and drug excretion activity is a must for poisoning prevention, advancement and promotion of a standard and regionally customized MMT guideline with the flexibility for patient individualization and including specialized psychiatric consultation (for prevention of methadone overdose) is also recommended.
Acknowledgments
This study is the result of a Doctor of Medicine thesis project which was financially supported by the vice-chancellery for research and technology of the Isfahan University of Medical Sciences. Authors would like to thank all personnel of the poisoning emergency ward of the Noor and Ali-Asghar [PBUH] university hospital for their sincere help.
Footnotes
CONFLICT OF INTEREST: NONE DECLARED.
REFERENCES
- 1.Dhalla IA. Opium, opioids, and an increased risk of death. BMJ. 2012;344:e2617. doi: 10.1136/bmj.e2617. PubMed PMID: 22511303. [DOI] [PubMed] [Google Scholar]
- 2.Jadidi N, Nakhaee N. Etiology of drug abuse: a narrative analysis. Journal of addiction 2014. 2014 doi: 10.1155/2014/352835. 352835. PubMed PMID: 25247105. Pubmed Central PMCID: 4160618. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Sayyah M, Sharifi M, Rokni P. Comparison of General Well-being of Patients Undergoing Methadone Maintenance Therapy (MMT) with Patients Undergoing Naltrexone Therapy. Iranian Journal of Public Health. 2013;42(2):145–148. PubMed PMID: 23515429. Pubmed Central PMCID: 3595655. [PMC free article] [PubMed] [Google Scholar]
- 4.Strain E. Treatment of opioid use disorder: Uptodate (Wolters Kluwer Health) [updated 2014/09/02; cited 2014 2014/09/29];2014 [Google Scholar]
- 5.Clark CB, Hendricks PS, Lane PS, Trent L, Cropsey KL. Methadone maintenance treatment may improve completion rates and delay opioid relapse for opioid dependent individuals under community corrections supervision. Addictive behaviors. 2014 Dec;39(12):1736–1740. doi: 10.1016/j.addbeh.2014.07.011. PubMed PMID: 25117851. [DOI] [PubMed] [Google Scholar]
- 6.Newman RG. Methadone maintenance: “interim treatment” compared to waiting lists. Journal of addiction medicine. 2014 Jul-Aug;8(4):295–296. doi: 10.1097/ADM.0000000000000046. PubMed PMID: 25089955. [DOI] [PubMed] [Google Scholar]
- 7.Aghabiklooei A, Edalatparvar M, Zamani N, Mostafazadeh B. Prognostic factors in acute methadone toxicity: a 5-year study. Journal of toxicology 2014. 2014 doi: 10.1155/2014/341826. 341826. PubMed PMID: 25197273. Pubmed Central PMCID: 4146352. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Richards-Waugh LL, Primerano DA, Dementieva Y, Kraner JC, Rankin GO. Fatal Methadone Toxicity: Potential Role of CYP3A4 Genetic Polymorphism. Journal of analytical toxicology. 2014 Oct;38(8):541–547. doi: 10.1093/jat/bku091. PubMed PMID: 25217544. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Taheri F, Yaraghi A, Sabzghabaee AM, Moudi M, Eizadi-Mood N, Gheshlaghi F, et al. Methadone toxicity in a poisoning referral center. Journal of research in pharmacy practice. 2013 Jul;2(3):130–134. doi: 10.4103/2279-042X.122387. PubMed PMID: 24991620. Pubmed Central PMCID: 4076914. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Eiden C, Leglise Y, Bertomeu L, Clavel V, Faillie JL, Petit P, et al. New formulation of methadone for opioid dependence in France: acceptability and diversion/misuse liability. Therapie. 2013 Mar-Apr;68(2):107–111. doi: 10.2515/therapie/2013020. PubMed PMID: 23773351. [DOI] [PubMed] [Google Scholar]
- 11.Centers for Disease C, Prevention. Vital signs: risk for overdose from methadone used for pain relief –United States, 1999-2010. MMWR Morbidity and mortality weekly report. 2012 Jul 6;61(26):493–497. PubMed PMID: 22763888. [PubMed] [Google Scholar]
- 12.Eizadi-Mood N, Akuchekian S, Sabzghabaee AM, Farzad G, Hessami N. General Health Status in a Cohort of Iranian Patients with Intentional Self-poisoning: A Preventive Approach. International journal of preventive medicine. 2012 Jan;3(1):36–41. PubMed PMID: 22355475. Pubmed Central PMCID: 3278867. [PMC free article] [PubMed] [Google Scholar]
- 13.LoVecchio F, Pizon A, Riley B, Sami A, D’Incognito C. Onset of symptoms after methadone overdose. The American journal of emergency medicine. 2007 Jan;25(1):57–59. doi: 10.1016/j.ajem.2006.07.006. PubMed PMID: 17157684. [DOI] [PubMed] [Google Scholar]
- 14.Shadnia S, Rahimi M, Hassanian-Moghaddam H, Soltaninejad K, Noroozi A. Methadone toxicity: comparing tablet and syrup formulations during a decade in an academic poison center of Iran. Clinical toxicology. 2013 Sep-Oct;51(8):777–782. doi: 10.3109/15563650.2013.830732. PubMed PMID: 23972442. [DOI] [PubMed] [Google Scholar]
- 15.Zamani S, Farnia M, Tavakoli S, Gholizadeh M, Nazari M, Seddighi AA, et al. A qualitative inquiry into methadone maintenance treatment for opioid-dependent prisoners in Tehran, Iran. The International journal on drug policy. 2010 May;21(3):167–172. doi: 10.1016/j.drugpo.2009.03.001. PubMed PMID: 19395250. [DOI] [PubMed] [Google Scholar]
- 16.Pilgrim JL, McDonough M, Drummer OH. A review of methadone deaths between 2001 and 2005 in Victoria, Australia. Forensic science international. 2013 Mar 10;226(1-3):216–222. doi: 10.1016/j.forsciint.2013.01.028. PubMed PMID: 23419969. [DOI] [PubMed] [Google Scholar]
- 17.Wolff K. Characterization of methadone overdose: clinical considerations and the scientific evidence. Therapeutic drug monitoring. 2002 Aug;24(4):457–470. doi: 10.1097/00007691-200208000-00001. PubMed PMID: 12142628. [DOI] [PubMed] [Google Scholar]
- 18.Hon KL, Ho JK, Hung EC, Cheung KL, Ng PC. Poisoning necessitating pediatric ICU admissions: size of pupils does matter. Journal of the National Medical Association. 2008 Aug;100(8):952–956. doi: 10.1016/s0027-9684(15)31411-5. PubMed PMID: 18717147. [DOI] [PubMed] [Google Scholar]
- 19.Caplehorn JR. Deaths in the first two weeks of maintenance treatment in NSW in 1994: identifying cases of iatrogenic methadone toxicity. Drug and alcohol review. 1998 Mar;17(1):9–17. doi: 10.1080/09595239800187551. PubMed PMID: 16203464. [DOI] [PubMed] [Google Scholar]
- 20.Afshari R, Maxwell SR, Bateman DN. Hemodynamic effects of methadone and di hydro codeine in overdose. Clinical toxicology. 2007 Oct-Nov;45(7):763–772. doi: 10.1080/15563650701502691. PubMed PMID: 17852162. [DOI] [PubMed] [Google Scholar]
- 21.Kamal F, Flavin S, Campbell F, Behan C, Fagan J, Smyth R. Factors affecting the outcome of methadone maintenance treatment in opiate dependence. Irish medical journal. 2007 Mar;100(3):393–397. PubMed PMID: 17491538. [PubMed] [Google Scholar]
- 22.Megarbane B, Buisine A, Jacobs F, Resiere D, Chevillard L, Vicaut E, et al. Prospective comparative assessment of buprenorphine overdose with heroin and methadone: clinical characteristics and response to antidotal treatment. Journal of substance abuse treatment. 2010 Jun;38(4):403–407. doi: 10.1016/j.jsat.2010.01.006. PubMed PMID: 20189341. [DOI] [PubMed] [Google Scholar]
- 23.Brands B, Blake J, Marsh DC, Sproule B, Jeyapalan R, Li S. The impact of benzodiazepine use on methadone maintenance treatment outcomes. Journal of addictive diseases. 2008;27(3):37–48. doi: 10.1080/10550880802122620. PubMed PMID: 18956528. [DOI] [PubMed] [Google Scholar]
- 24.McCowan C, Kidd B, Fahey T. Factors associated with mortality in Scottish patients receiving methadone in primary care: retrospective cohort study. Bmj. 2009;338:b2225. doi: 10.1136/bmj.b2225. PubMed PMID: 19535400. Pubmed Central PMCID: 3273784. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Schuckit MA. Comorbidity between substance use disorders and psychiatric conditions. Addiction. 2006 Sep;101(Suppl 1):76–88. doi: 10.1111/j.1360-0443.2006.01592.x. PubMed PMID: 16930163. [DOI] [PubMed] [Google Scholar]
- 26.Bernard JP, Havnes I, Slordal L, Waal H, Morland J, Khiabani HZ. Methado nere lated deaths in Norway. Forensic science international. 2013 Jan 10;224(1-3):111–116. doi: 10.1016/j.forsciint.2012.11.010. PubMed PMID: 23246070. [DOI] [PubMed] [Google Scholar]
- 27.Concool B, Smith H, Stimmel B. Mortality rates of persons entering methadone maintenance: a seven-year study. The American journal of drug and alcohol abuse. 1979;6(3):345–353. doi: 10.3109/00952997909001723. PubMed PMID: 539576. [DOI] [PubMed] [Google Scholar]


