Abstract
Background and objective:
Body weight and body mass index (BMI) are considered potentially modifiable determinants of bone mass. Therefore, the aim of this study was to explore the association between body weight and body mass index (BMI) with total hip and lumbar spine bone mineral density (BMD).
Methods:
This cross-sectional study included a population of 100 women and 32 men from Kosovo into three BMI groups. All the study subjects underwent dual-energy X-ray absorptiometry (DXA) measurements.
Results:
Total hip BMD levels of obese menopausal and premenopausal women and men were significantly higher compared to overweight or normal weight subjects, while lumbar spine BMD levels of only menopausal women and men were higher among obese subjects. Age-adjusted linear regression analysis showed that BMI is a significant independent associate of lumbar spine and total hip BMD in menopausal women and men.
Conclusion:
Despite positive association between BMI and lumbar spine and total hip BMD in menopausal women, presence of more obese and osteoporotic subjects among menopausal women represent a population at risk for fractures because of poor balance and frequent falls; therefore, both obesity and osteoporosis prevention efforts should begin early on in life.
Keywords: Weight, body mass index, bone mineral density, women, men
1. INTRODUCTION
Osteoporosis and hip and vertebral osteoporotic fractures among an ageing population are a worldwide health problem that lead to a decreased quality of life (1). Body weight and body mass index (BMI) are considered potentially modifiable determinants of bone mass (2, 3). Several studies have demonstrated an association of low body weight and BMI with low BMD and fractures (4), while several other studies showed a protective effect of higher BMI on BMD (5-8). Among most frequently cited mechanisms to explain this positive association of weight with BMD is weight-related loading on bones (9), though higher estrogen and insulin synthesis and higher plasma leptin levels are considered to play an important role (10). On the other hand, it should be acknowledged that there are studies that did not demonstrate a significant positive association between weight and BMI and BMD or demonstrated a negative association of obesity and BMD (11-13); interaction between fat mass and bones through pro-inflammatory cytokines or low levels of adiponectins are some of the proposed mechanisms (14-16).
The aim of this study was to explore the relationship between body weight and body mass index (BMI) with total hip and lumbar spine bone mineral density (BMD) in a population of 100 women and 32 men from Kosovo.
2. MATERIAL AND METHODS
Sixty postmenopausal and forty premenopausal women, and thirty two men were prospectively enrolled in this cross-sectional study. The study protocol was approved by the ethics committee, and written informed consent was obtained from all study participants before enrollment. Baseline anthropometric data (height and weight) were measured in light indoor clothing without shoes before performing DXA, and body mass index was calculated as kg/m2. The study population was classified in three categories on the basis of World Health Organization (WHO) Body Mass Index (BMI) criteria: normal weight (n=28, BMI <24.9 kg/m2), overweight (n=41, 25.0-29.9 kg/m2) and obese (n=63, BMI>30 kg/m2). Quantitative assessment of bone mineral density (BMD) at the lumbar spine and total hip was performed using dual-energy x-ray absorptiometry (DXA; STRATOS 800) technique by trained examiners. The diagnosis of osteoporosis was done according to WHO T-score criteria (osteoporosis was considered if T-score ≤ -2.5 SD, low bone mass if T-score between -2.5 SD and -1 SD, and normal BMD if T-score > -1SD).
Statistical analysis
Statistical analysis were performed with SPSS software version 16.0. The data were tested for normal distribution with Shapiro-Wilk test. Continuous variables are expressed as means ± standard deviations (median), while categorical data are presented as percentages. As the data were not normally distributed, the Kruskal-Wallis test was used to compare characteristics of the groups, while Chi square test was used for categorical variables. A p-value of <0.05 was considered statistically significant. Age-adjusted multiple linear regression analysis of independent associates (weight and BMI) of total lumbar spine and total hip BMD was calculated.
3. RESULTS
The study population consisted of 60 menopausal women with a mean age of 63.68±9.27 (SD) years, 40 premenopausal women with a mean age of 43.44±7.42 (SD) years and 32 men with mean age of 66.34±14.97 (SD) years. Distribution of the total hip and total lumbar spine BMD according to BMI groups in menopausal and premenopausal women and men is presented in Figure 1. The descriptive characteristics of the study population groups are shown in Table 1, which includes age, BMI, height, weight, lumbar spine and total BMD, as well as information regarding BMI groups and T-score groups. There were no significant differences between study groups regarding body weight (p=0.108), while BMI score was significantly higher among menopausal women compared to premenopausal women or men (p=0.001). There were no statistically significant differences in lumbar spine or total hip BMD values between three study groups. There were significantly more obese and osteoporotic subjects among menopausal women compared to premenopausal women or men (p<0.001 and p=0.002, respectively).
Figure 1.
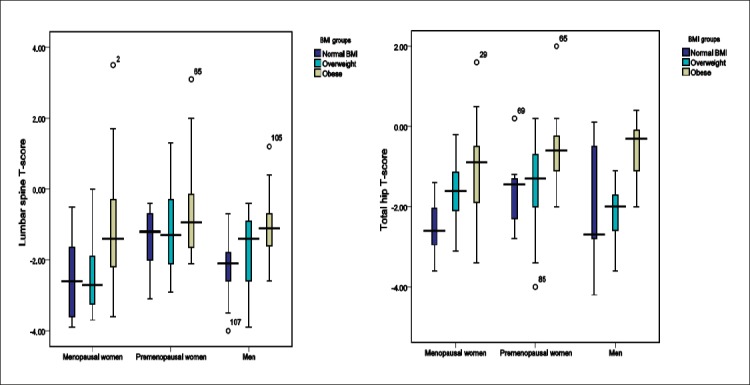
Distribution of total hip and lumbar spine BMD according to BMI groups
Table 1.
Descriptive characteristics of the study subjects. Parameters are given as mean± standard deviation, median (in the brackets), and number of cases (percentage) as appropriate; a p-values of Kruskal-Wallis test or Chi-square test as appropriate
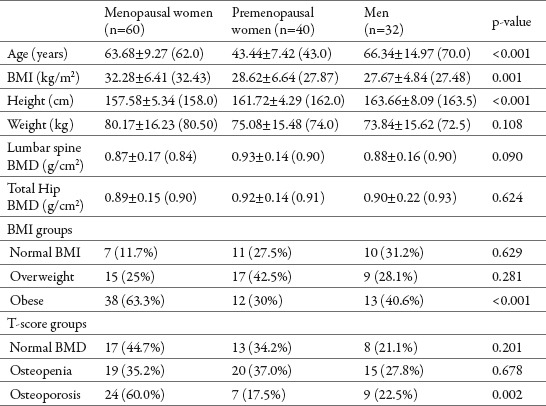
Table 2.
Age-adjusted multiple linear regression analysis of independent associates of lumbar spine and total hip BMD. BMD: Bone mineral density, BMI: Body mass index, β: Unstandardized regression coefficient
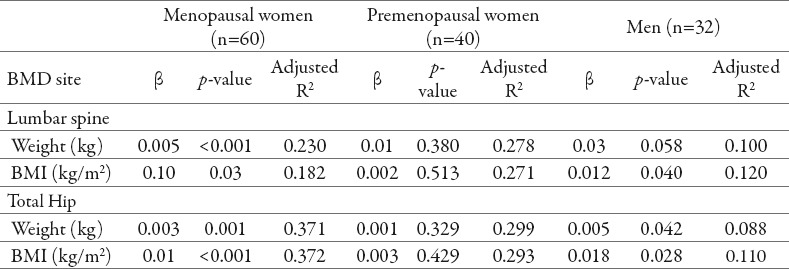
A statistically significant difference was observed in menopausal women for both total hip and lumbar spine BMD values among BMI groups (p=0.010 and p=0.003, respectively). Total hip and lumbar spine BMD values in obese women at menopause were significantly higher compared to normal weight (p=0.008 and p=0.035, respectively). Lumbar spine BMD values in obese women at menopause were significantly higher compared to overweight women at menopause (p=0.002), while no statistically significant difference was observed in total hip BMD values between obese and overweight subjects (p=0.061). No significant difference was observed between overweight and normal weight subjects in total hip and lumbar spine BMD values (p=0.091 and p=0.783, respectively). Age-adjusted multiple linear regression analysis showed that both weight and BMI were significant independent associates of lumbar spine and total hip BMD, with highest adjusted squared values in total hip BMD, where weight and BMI explained 37.1% and 37.2% of the variation, respectively.
A statistically significant difference was observed in premenopausal women for total hip BMD values among BMI groups (p=0.023). Total hip BMD values in obese premenopausal women were significantly higher compared to normal weight and overweight subjects (p=0.007 and p=0.043, respectively), while no statistically significant difference was observed in total hip BMD values between overweight and normal weight subjects (p=0.458). No statistically significant difference was found for lumbar spine BMD values among BMI groups (p=0.477). According to age-adjusted multiple linear regression analysis no significant association of weight and BMI as independent variables with total hip and lumbar spine BMD was observed.
A statistically significant difference was observed in men for total hip BMD values among BMI groups (p=0.007). Total hip BMD values in obese male subjects were significantly higher compared to normal weight and overweight subjects (p=0.03 and p=0.002, respectively), while no statistically significant difference was observed in total hip BMD values between overweight and normal weight subjects (p=0.938). No statistically significant difference was found for lumbar spine BMD values among BMI groups (p=0.060). Nevertheless, age adjusted multiple linear regression analysis showed a significant positive effect of the BMI on lumbar spine BMD in men (p=0.040), where it explains 12.0% of the variation. Though there was a positive tendency, no significant effect of weight was observed on lumbar spine BMD in men (p=0.058), while both weight and BMI showed a significant positive effect on total hip BMD in men (p=0.042 and p=0.028, respectively) according to multiple linear regression analysis.
4. DISCUSSION
In this cross-over study, we have demonstrated that total hip BMD levels of obese menopausal and premenopausal women and men were significantly higher compared to overweight or normal weight subjects, while lumbar spine BMD levels of only menopausal women and men were higher among obese subjects. We also found evidence to suggest that BMI is a significant independent associate of lumbar spine and total hip BMD in both menopausal women and men. Every unit increase in BMI among menopausal women was associated with an increase of 0.1 g/cm2 in L1-L4 BMD, and 0.01 g/cm2 in total hip BMD, while among men every unit increase in BMI was associated with an increase of 0.012 g/cm2 in L1-L4 BMD, and 0.018 g/cm2 in total hip BMD.
Our results are in agreement with some of the studies that demonstrated positive association of BMI with BMD. In this regard, Lloyd et al (5) examined variation in BMD across BMI spectrum using data from the National Health and Nutrition Examination Survey (NHANES) and found positive association of BMI with BMD in the respective sample of elderly subjects, without gender differences. Similarly, in a large retrospective cohort study in women aged 40 to 59, Morin et al (3) concluded that low weight and BMI predict osteoporosis and are associated with increased fracture risk. Our results are fully consistent with the results of Doğan et al (6) that conducted a similar study among 900 geriatric subjects and demonstrated a statistically significant difference for the lumbar spine and femur neck BMD levels among the BMI groups as well as a significant relationship between both the lumbar and the femoral BMD measurements and the BMI in women, and similarly found no significant differences in lumbar spine levels among BMI groups in men. Another recently conducted study of Hoxha et al (7) in 64 males from Kosovo compared BMI groups for L1-L4 BMD, femur neck BMD and total hip BMD levels, and reported no differences among them; nevertheless, they demonstrated a positive correlation between BMI and femur neck and total hip BMD as well as positive association of BMI with all measurement sites BMD. Due to differences in the study populations, our results are partly consistent with them, as far as we found significant differences in total hip BMD values among BMI groups in men while we failed to demonstrate a significant association of BMI with lumbar spine BMD.
On the other hand, it should be acknowledged that there are studies that did not demonstrate a significant positive association between weight and BMI and BMD, or to the contrary demonstrated a negative association of obesity and BMD, thus seriously challenging the widespread belief that obesity is protective. Paniagua et al (11) found a high prevalence of osteopenia and osteoporosis among male nursing home residents who were more likely to be classified as overweight and obese according to BMI. Similarly, Greco et al (12) demonstrated that obesity was associated with a osteoporosis and provided clinical evidence that obesity should not be considered as a protective factor.
5. CONCLUSION
In conclusion, total hip BMD values in obese menopausal and premenopausal women as well as men were significantly higher compared to overweight or normal weight subjects. BMI was shown to be a significant independent associate of lumbar spine and total hip BMD in both menopausal women and men, while such a relationship among premenopausal women did not exist. Nevertheless, significantly more obese and osteoporotic subjects among menopausal women represent a population at risk for fractures because of poor balance and frequent falls; therefore, both obesity and osteoporosis prevention efforts should begin early on in life.
Footnotes
CONFLICT OF INTEREST: NONE DECLARED
REFERENCES
- 1.Kwan P. Osteoporosis: From osteoscience to neuroscience and beyond. Mech Ageing Dev. 2015 Jan;145:26–38. doi: 10.1016/j.mad.2015.02.001. [DOI] [PubMed] [Google Scholar]
- 2.Wee J, Sng BY, Shen L, Lim CT, Singh G, Das De S. The relationship between body mass index and physical activity levels in relation to bone mineral density in premenopausal and postmenopausal women. Arch Osteoporos. 2013;8(1-2):162. doi: 10.1007/s11657-013-0162-z. [DOI] [PubMed] [Google Scholar]
- 3.Morin S, Tsang JF, Leslie WD. Weight and body mass index predict bone mineral density and fractures in women aged 40 to 59 years. Osteoporos Int. 2009 Mar;20(3):363–370. doi: 10.1007/s00198-008-0688-x. [DOI] [PubMed] [Google Scholar]
- 4.Morin S, Leslie WD. Manitoba Bone Density Program. High bone mineral density is associated with high body mass index. Osteoporos Int. 2009 Jul;20(7):1267–1271. doi: 10.1007/s00198-008-0797-6. [DOI] [PubMed] [Google Scholar]
- 5.Lloyd JT, Alley DE, Hawkes WG, Hochberg MC, Waldstein SR, Orwig DL. Body mass index is positively associated with bone mineral density in us older adults. Arch Osteoporos. 2014 Dec;9(1):175. doi: 10.1007/s11657-014-0175-2. [DOI] [PubMed] [Google Scholar]
- 6.Dogan A, Nakipoglu-Yüzer GF, Yildizgören MT, Ozgirgin N. Is age or the body mass index (BMI) more determinant of the bone mineral density (BMD) in geriatric women and men? Arch Gerontol Geriatr. 2010 Nov-Dec;51(3):338–341. doi: 10.1016/j.archger.2010.01.015. [DOI] [PubMed] [Google Scholar]
- 7.Hoxha R, Islami H, Qorraj-Bytyqi H, Thaçi S, Bahtiri E. Relationship of weight and body mass index with bone mineral density in adult men from Kosovo. Mater Sociomed. 2014 Oct;26(5):306–308. doi: 10.5455/msm.2014.26.306-308. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kang D, Liu Z, Wang Y, Zhang H, Feng X, Cao W, Wang P. Relationship of body composition with bone mineral density in northern Chinese men by body mass index levels. J Endocrinol Invest. 2014 Apr;37(4):359–367. doi: 10.1007/s40618-013-0037-6. [DOI] [PubMed] [Google Scholar]
- 9.Gonnelli S, Caffarelli C, Nuti R. Obesity and fracture risk. Clin Cases Miner Bone Metab. 2014 Jan;11(1):9–14. doi: 10.11138/ccmbm/2014.11.1.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Grumbach MM. Estrogen, bone, growth and sex: a sea change in conventional wisdom. J Pediatr Endocrinol Metab. 2000;13(Suppl 6):1439–1455. doi: 10.1515/jpem-2000-s619. [DOI] [PubMed] [Google Scholar]
- 11.Paniagua MA, Malphurs JE, Samos LF. BMI and low bone mass in an elderly male nursing home population. Clin Interv Aging. 2006;1(3):283–287. doi: 10.2147/ciia.2006.1.3.283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Greco EA, Fornari R, Rossi F, Santiemma V, Prossomariti G, Annoscia C, Aversa A, Brama M, Marini M, Donini LM, Spēra G, Lenzi A, Lubrano C, Migliaccio S. Is obesity protective for osteoporosis?Evaluation of bone mineral density in individuals with high body mass index. Int J Clin Pract. 2010 May;64(6):817–820. doi: 10.1111/j.1742-1241.2009.02301.x. [DOI] [PubMed] [Google Scholar]
- 13.Emaus N, Wilsgaard T, Ahmed LA. Impacts of Body Mass Index, Physical Activity, and Smoking on Femoral Bone Loss. The Tromsø Study. J Bone Miner Res. 2014 Sep;29(9):2080–2089. doi: 10.1002/jbmr.2232. [DOI] [PubMed] [Google Scholar]
- 14.Gómez-Ambrosi J, Rodríguez A, Catalán V, Friihbeck G. The bone-adipose axis in obesity and weight loss, obes Surg. 2008. Sep;18(9):1134–1143. doi: 10.1007/s11695-008-9548-1. [DOI] [PubMed] [Google Scholar]
- 15.Yang S, Center JR, Eisman JA, Nguyen TV. Association between fat mass, lean mass, and bone loss: the Dubbo osteoporosis epidemiology study. Osteoporos Int. 2015 Apr;26(4):1381–1386. doi: 10.1007/s00198-014-3009-6. [DOI] [PubMed] [Google Scholar]
- 16.Aguirre L, Napoli N, Waters D, Quails C, Villareal DT, Armamento-Villareal R. Increasing adiposity is associated with higher adipokine levels and lower bone mineral density in obese older adults. J Clin Endocrinol Metab. 2014 Sep;99(9):3290–3297. doi: 10.1210/jc.2013-3200. [DOI] [PMC free article] [PubMed] [Google Scholar]


