Abstract
Contemporary biological psychiatry uses experimental animal models to increase our understanding of affective disorder pathogenesis. Modern anxiolytic drug discovery mainly targets specific pathways and molecular determinants within a single phenotypic domain. However, greater understanding of the mechanisms of action is possible through animal models. Primarily developed with rats, animal models in anxiety have been adapted with mixed success for mice, easy-to-use mammals with better genetic possibilities than rats. In this review, we focus on the three most common animal models of anxiety in mice used in the screening of anxiolytics. Both conditioned and unconditioned models are described, in order to represent all types of animal models of anxiety. Behavioral studies require careful attention to variable parameters linked to environment, handling, or paradigms; this is also discussed. Finally, we focus on the consequences of re-exposure to the apparatus. Test-retest procedures can provide new answers, but should be intensively studied in order to revalidate the entire paradigm as an animal model of anxiety.
Keywords: animal anxiety test, drug development, elevated plus maze, light/dark box test, four-plate test, serotonin receptor, GABA
Abstract
La psiquiatría biológica actual emplea modelos animales experimentales para aumentar la comprensión acerca de la patogénesis del trastorno afectivo. El descubrimiento de los fármacos ansiolíticos modernos apunta principalmente a vías especificas y determinantes moleculares dentro de un dominio fenotípico único. Sin embargo, es posible una mayor comprensión de los mecanismos de acción a través de los modelos animales. Los modelos animales de ansiedad, inicialmente desarrollados en ratas, han sido adaptados con relativo éxito en ratones, un mamífero fácil de emplear y con mejores posibilidades genéticas que las ratas. Esta revisión se focaliza en los tres modelos animales de ansiedad empleados más comúnmente en ratones, que se utilizan para la evaluación de ansiolíticos. Se describen tanto los modelos condicíonados como los incondicionados con el fin de representar todos los tipos de modelos animales de ansiedad. También se analiza el gran cuidado que se debe poner en los parámetros variables relacionados con el ambiente, la manipulación o el paradigma que tienen los estudios de comportamiento. Por último se centra la atención en las consecuentias de la re-exposición al aparato. Los procedimientos de test-retest pueden proportionar nuevas respuestas, pero deben ser ampliamente estudiados para revalidar todo el paradigma como un modelo animal de ansiedad.
Abstract
La psychiatrie biologique actuelle utilise les modèles animaux expérimentaux pour mieux comprendre la pathogenèse des troubles affectifs. La recherche moderne sur les anxiolytiques cible principalement les voies spécifiques et les déterminants moléculaires dans un phénotype unique. Les modèles animaux permettent néanmoins de mieux comprendre les mécanismes d'action. D'abord développés chez le rat, les modèles animaux de l'anxiété ont été adaptés avec un succès variable chez la souris, un mammifère facile à utiliser dont les possibilités génétiques sont meilleures que celles du rat. Dans cet article, nous nous intéressons aux trois modèles d'anxiété les plus courants chez la souris, utilisés pour la sélection d'anxiolytiques. Nous décrivons à la fois les modèles conditionnés et non conditionnés afin de représenter tous les types de modèles animaux d'anxiété. Les études de comportement nécessitant une observation soigneuse des paramètres variables liés à l'environnement, aux façons de réagir ou aux modèles, sont aussi analysées. Enfin nous nous intéressons aux conséquences de la ré-exposition au dispositif. Les techniques de fiabilité test-retest peuvent fournir de nouvelles réponses mais doivent être étudiées en profondeur afin de revalider le modèle entier comme modèle animal de l'anxiété.
Introduction
The discovery of the benzodiazepines (BDZs) in the early 1960s, and their considerable commercial success in the treatment of anxiety, has fueled the development of numerous animal models of anxiety. These paradigms are widely used to search for new anxiolytic drugs and to investigate brain mechanisms underlying anxiety. Clinical classifications acknowledge the existence of different types of pathological anxiety such as generalized anxiety, social anxiety, panic, post-traumatic stress disorder, and phobia. Although attempts have been made to relate animal models to classes of anxiety disorder, the correspondence between clinical and experimental results remains an open question.1 Accordingly, anxiety defined operationally in a given model may differ from that generated by other models with respect to drug response, environmental manipulations, and/or neural substrates. Animals, like humans, express different kinds of fear/anxiety in response to different environmental conditions (eg, acute vs chronic stress, spontaneous vs conditioned responses, etc). Only restricted aspects of human psychopathology can be explored and stimulated using animal models with symptoms of these disorders, rather than a complete anxiety subtype.
Unfortunately, because BDZs were the only anxiolytic agents marketed at that time, the predictive validity of these initial models was initially mainly based on their ability to detect the pharmacological action of BDZs. This became evident in the early 1980s when non-BDZ anxiolytics, eg, serotoninergic agents, were found to be inactive in some anxiety tests.
The research into the psychopharmacological treatments of anxiety is an active area. Old drugs are being re-evaluated and their indications broadened, while important new agents, such as the selective serotonin reuptake inhibitors, (SSRIs), have been successfully added to the clinician's armory in recent years. Exciting new drugs that either have a completely different profile compared with the established ones, or promise fewer adverse effects, are currently undergoing testing.
Earlier studies on the hypothetical involvement of serotonin (5-hydroxytryptamine or 5-HT) in anxiety suggested that an increase in 5-HT transmission would promote anxiety, while a reduction would attenuate it. However, more than four decades of research have shown a complex picture. The paradoxical effects of 5-HT manipulations in animal models have been attributed either to the recognition that animal models reflect different neurobiological mechanisms, or that multiple 5-HT receptor subtypes located either pre- or postsynaptically play differential roles in various aspects of anxiety. The existence of so many 5-HT receptors and the lack of ligands with sufficient selectivity for the receptor subtypes have made it difficult to determine unequivocally whether a single 5-HT receptor subtype modulates a particular biological response, or is critically involved in a specific brain function. The specific role of 5-HT subtypes in various aspects of anxiety or in different types of animal models is still largely unknown.
Initial evidence concerning the 5-HT2 receptor in anxiety results from studies involving nonselective 5-HT2C receptor agonists and antagonists. Meta-chlorophenylpiperazine (mCPP), a 5-HT2C partial agonist, was found to possess anxiogenic-like effects in various animal and human studies. On the other hand, the nonselective 5-HT2A/2C receptor antagonists such as ritanserin and ketanserin showed potential anxiolytic-like effects in animal models and promising clinical results. The development of new compounds with 5-HT2 receptor affinities was thus of interest for potential therapeutic purposes. Lack of specificity of the available 5-HT2 agents and differential involvement of 5-HT in the various anxiety models accounted for inconclusive results and hindered the recognition of their respective roles, if any, in the etiology of anxiety. With the recent advent of dynamic brain imaging techniques and the increasing availability of new ligands, work has focused on a more systematic “teasing-out” of the pathways involved in the various forms of anxiety.
What is an anxiety model?
Animal models are experimental preparations developed in one species for the purpose of studying phenomena occurring in another species, and such models may be valid if they have the same structure as the human behavior or pathology. The use of animal models is well established in the study of the biological bases of psychiatric disorders. Despite traditional difficulties in accepting animal models for psychopathology, stemming from the argument that there is no evidence for concluding that what occurs in the brain of the animal is equivalent to what occurs in the brain of a human, these models have become an invaluable tool in the analysis of the multitude of causes—genetic, environmental, or pharmacological—that can bring about symptoms homologous to those of patients with a specific disorder.2
Currently, animal models are sought that have three types of validity:
Face validity, where the model is phenotypically similar and implies that the response observed in the animal model should be identical to the behavioral and physiological responses observed in humans. The behavioral response repertoire of mice is of course very different from the human ethogram, which includes the verbal aspect that is absent in rodents
Predictive validity entails that the model should be sensitive to clinically effective pharmacological agents, and conversely anxiogenic compounds should elicit opposite effects, while agents that have no effect in the clinic should have no effect in these tests
The criterion of construct validity relates to the similarity between the theoretical rationale underlying the animal model and the human behavior. This requires that the etiology of the behavior and the biological factors underlying the disorder be similar in animals and humans.
Often researchers fail to specify whether they are seeking a correlational model (eg, predictive validity, a model that is selectively sensitive to therapeutic agents), an isomorphic model (face validity, a model that implies that the behavioral response in the human and animal is the same) or a homologous model (true construct validity, a model that implies the “cause” of the behavioral response in the animal is sufficient to provoke the same response in humans).
Behavior can be both an event and a process, and observable behaviors are the result of the integration of all of the processes ongoing in underlying organ systems, in interaction with the external social and physical environment. Animal models can allow the study of mechanisms of specific behaviors and their pathophysiology, and can aid in developing and predicting therapeutic responses to pharmacological agents.
As previously mentioned, many animal models arose from the discovery of BZs, and non-BDZ anxiolytics eg, buspirone, were found to be inactive in some anxiety tests.3 It became evident that anxiety is not a unitary disease, but a complex phenomenon that probably involves many different neurochemical systems with varied etiological origins and may be divided into various forms including state and trait anxiety, and normal and pathological anxiety. Animals cannot model every aspect of human anxiety, but studies in animals permit detailed investigations of neurobiological and psychological processes in states in which fear might be inferred, such as responses to acute and repeated aversive stressors. The clinical acceptance of the heterogeneity of anxiety disorder suggests that there are distinct neurobiological substrates for each, and it is therefore necessary to examine whether different animal tests might reflect those differences. Assigning particular tests of anxiety to particular anxiety disorders is an extremely difficult task. Thus, various animal models may be more appropriate for one type of anxiety disorder than for another, as it is inappropriate to assume that any one model may serve to detect compounds for a disease that is mediated through multiple and diverse mechanisms.
Classification of the anxiety models
Handley4 tried to classify animal models of anxiety according to the nature of the aversive stimulus and of the response elicited, suggesting that the neuronal control of anxiety may differ according to whether the interpretation of an aversive signal is innate or learned, and whether it elicits a response or, conversely, inhibits an ongoing, rewarded behavior. Animal models of anxiety can be grouped into two main subclasses (Table I): the first involves the animal's conditioned responses to stressful and often painful events (eg, exposure to electric footshock); the second includes ethologically based paradigms and involves the animal's spontaneous or natural reactions (eg, flight, avoidance, freezing) to stress stimuli that do not explicitly involve pain or discomfort (eg, exposure to a novel highly illuminated test chamber or to a predator).
Table I. Drug effects in mouse models of anxiety.
| Conditioned responses | Unconditioned reponses |
| Geller-Seifter conflict | Elevated plus maze (zero/T maze) |
| Vogel conflict | Light/dark exploration (L/D) |
| Four-plate test | Social interaction |
| Conditioned emotional response | Open field |
| Conditioned taste aversion | Ultrasonic vocalization (pain or separation) |
| Fear-potentiated startle | Fear/anxiety-defense test batteries |
| Defensive burying | Staircase test |
| Active/passive avoidance | Holeboard |
| Electrical brain stimulation | Predator |
Ethologically based animal models of fear and anxiety attempt to approximate the natural conditions under which such emotional states are elicited. By employing nonpainful aversive stimuli to induce fear and anxiety, ethological tests are thought to minimize possible confounding effects of motivational or perceptual states arising from interference with learning/memory or hunger/thirst or nociceptive mechanisms, and allow for a truly comprehensive “behavioral profiling” of experimental interventions. When compared with conditioned models, ethologically based tests seem better qualified to be analogs of human anxiety. Ethological models, however, present individual differences and variable behavioral baseline levels. Nonetheless, ethological stimuli are diverse in nature.
Producing conditioned fear in animals requires the pairing of a previously neutral stimulus with an electric shock. Subsequent presentations of the stimulus disrapt ongoing behavior and produce avoidance or defense. Prior training of subjects to attain specific levels of response decreases individual variability. Automated evaluation of the investigated parameters, together with a rigorous control and methodological manipulation of the experimental variables, also facilitates the use of conditioned models. Nonetheless, such tests involve a time-consuming effort for their subjects. The need for some degree of motivation (food and/or water deprivation) and the involvement of painful stimuli or events often times confound results, leading to other possible interpretations.5 Furthermore, influence of prior drug experience, and often low baseline response rates, are additional difficulties encountered in conflict paradigms.6
Mouse models of anxiety
Models of rodent behavior have been optimized in the rat over the past century. Yet the mouse is far more studied as a genetic organism, because it is more easily housed (many more mice can be housed in a given space), it breeds more quickly, homologue recombination techniques are now standard for the mouse (and not yet generally available for the rat), and the mouse genome has been more completely characterized. The behavioral field has responded to this paradox by trying to adapt tests developed in the rat to the mouse. Most models involve exposure of subjects to external (eg, cues either paired with foot-shock, bright light, predator) or internal (eg, drug states) stimuli that are assumed to be capable of inducing anxiety in animals.7
Since none of these models involves pathological anxiety-related behaviors,8 they have been described as animal models of “state” anxiety. State anxiety is that seen in a response to the level of stress and to the way that stress is perceived. In such procedures subjects experience anxiety at a particular moment in time, and this is increased by the presence of an anxiogenic stimulus. Models of “pathological” anxiety are often referred to as “trait” anxiety tests. Trait anxiety is the persistent and durable feature of the individual personality that reflects the way the subject interacts with its physical and social environment. Unlike state anxiety, trait anxiety does not vary from moment to moment,and is considered to be an enduring feature of an individual.9
The choice of the three models below is linked to the author's own experience, as well as the pertinence to screening anxioly tic-like drugs. When the effect size obtained by a new drug is high, the chance of discovering a new anxiolytic is also high.
Elevated plus maze
One of the most popular behavioral tests for research on anxiety and frequently used mouse models of anxiety is the elevated plus maze (EPM)10 initially developed for rats11 and more recently, for other species such as guinea pigs, voles, hamsters, and gerbils Figure 1. 12 There has also been development of several derivatives of the EPM including the elevated T-maze, zero maze, and the unstable elevated exposed plus maze, a recently established model of extreme anxiety in rats which has all four arms exposed and oscillated in a horizontal plane.
Figure 1. Elevated plus maze apparatus.
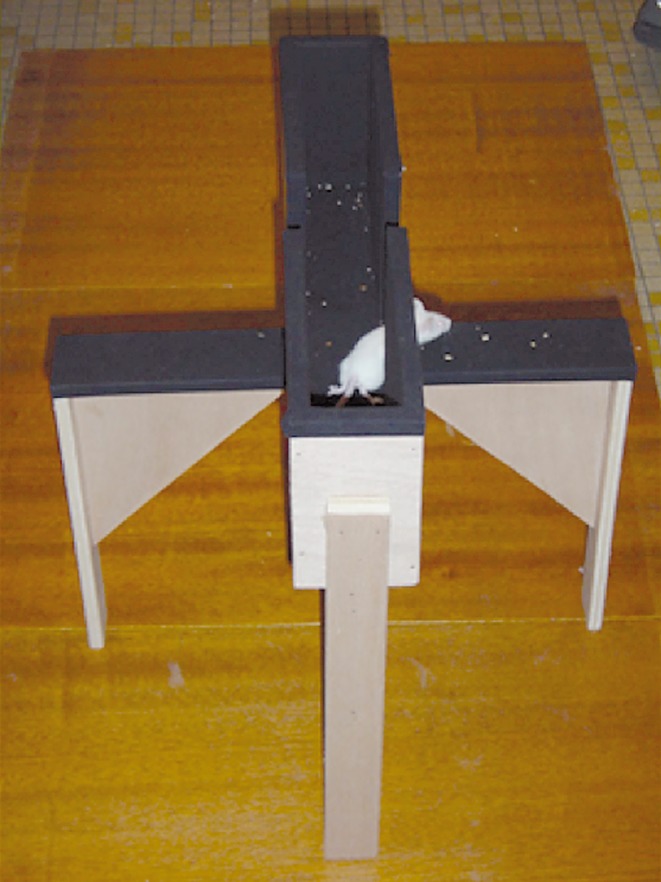
The EPM has been widely used as a tool in the investigation of the psychological and neurochemical bases of anxiety, for screening anxiety-modulating drugs or mouse genotypes13; The EPM is in the form of a plus-sign, with two open elevated arms facing each other and separated by a central square and two arms of the same dimensions, but enclosed by walls. The maze is raised off the ground so that the open arms combine elements of unfamiliarity, openness, and elevation. The EPM is based on the natural aversion of rodents to open spaces, and uses conflict between exploration and this aversion. Provoked behavior profiles in the EPM appear to include elements of neophobia, exploration, and approach/avoidance conflict, and thus the apparatus is often referred to as an unconditioned spontaneous behavioral conflict model.
Mice taken from their home cages will generally show a pattern of behavior characterized by open-arm avoidance, with a consistent preference for the closed arms. The rank order preference profile is closed → centre → open, indicative of a penchant for relatively secured sections of the maze. This tendency is suppressed by anxiolytics and potentiated by anxiogenic agents. The measures of anxiety are the number of open-arm entries and the number of closed-arm entries expressed as a percentage of the total number of arm entries and the amount of time spent on the open arms. Although automated plus-maze apparatus (eg, photobeam-based, video tracking systems) is now used in a few laboratories, most research groups still observe the behavior of their animals during testing. As such, the plus maze test has traditionally been scored either live or from a video-image by a trained observer.
Lister10 showed that the behavioral parameters in the mouse plus maze provided measures of two independent factors, one reflecting anxiety and one reflecting motor activity. The percentage of open-arm entries and the time spent on the open arms are extremely good measures of anxiety generated by this test. In contrast, the total arm entries, the measure of activity that was originally proposed, is a contaminated measure, and changes in this parameter could reflect changes in anxiety or in activity. In later factor analyses of data the same factor structure was confirmed and it was found that the number of closed-arm entries provided a better measure of motor activity.14 However, agreement as to the “pure” indicator of locomotor activity index of the EPM remains ambiguous. Some investigators report total entries as a locomotor activity indicator9,14 open entries as a mixed anxiety/ locomotor activity indicator, and closed entries as an index of protected exploration. The factor structure of the plus maze parameters in rats is changed by sex: for the male rat the strongest factor was anxiety, with motor activity being relatively unimportant. For the females, the situation was reversed, with activity being the more important factor.
The EPM permits a rapid screening of anxiety-modulating drugs or mouse genotypes (eg, CCK2 KO, 5-HT1A KO) without training or involvement of complex schedules. The test offers a number of advantages over other paradigms used to assess anxiety that involve food or water deprivation or shock administration. In particular, drug effects on appetite or sensitivity to pain are unlikely to interfere with experimental results.
5-HT modulating compounds are particularly prone to discrepancies in the plus maze, which may be explained by the EPM detecting multiple effects of drugs interacting with the 5-HT system. A number of research groups have argued that the utility and sensitivity of this model might be improved by adapting a more ethological approach. Rodgers and Johnson14 have developed and refined an “ethological” version of the mouse plus maze that incorporates specific behavioral postures (eg, risk assessment, head dipping, and stretched attend posture) together with conventional spatiotemporal measures of open-arm avoidance.
The anxiolytic efficacy of BDZs is either markedly reduced or completely abolished by prior undrugged test experience. In addition to these observations, prior test experience also appears to fundamentally alter the nature of future emotional responses to the plus maze. More specifically, the primary indices of anxiety from trials 1 and 2 load on independent factors, ie, two distinct states of anxiety are generated from the two trials.15 It seems that it is the open aspect of the arms that is the most important factor controlling behavior on trial one, whereas it is the elevation that is most important on trial two. This has two implications for research: first, it means that the same apparatus can be used to assess changes in two different states of anxiety, and it is quite likely that a change may be detected in one kind of anxiety, but not the other.16 Secondly, it means that care must be exercised if the mice are retested, and that it is not possible to test on one occasion, naive, and on a second trial after drug treatment.
The elevated plus maze test, whatever the modalities of use, is still an important tool for discovery of anxiolytics; agomelatine, for example, increases time spent in open arms.17
The light/dark box
The light/dark (L/D) exploration test is another commonly used murine model of anxiety Figure 2. 18 This test is based on the innate aversion of rodents to brightly illuminated areas, and on the spontaneous exploratory behavior of rodents in response to mild stressors, ie, novel environment and light. This model permits mice to freely explore two interconnected compartments that vary in size (2:1), color (white:black) and illumination (bright:dim). Thus, control mice placed into the brightly lit section will rapidly move into the dark area. After anxiolytic (BDZ) drug treatment the apparent apprehension of remaining in or moving to the light area is abolished. Since then the L/D test has been widely adopted as an anxiolytic screening test in mice, extended for use with rats and has been subject to several modifications. The size of the box and compartments has been adjusted Another model included the addition of a tunnel between the two compartments and the transformation of the paradigm into a corridortype runway.
Figure 2. The light/dark box apparatus.
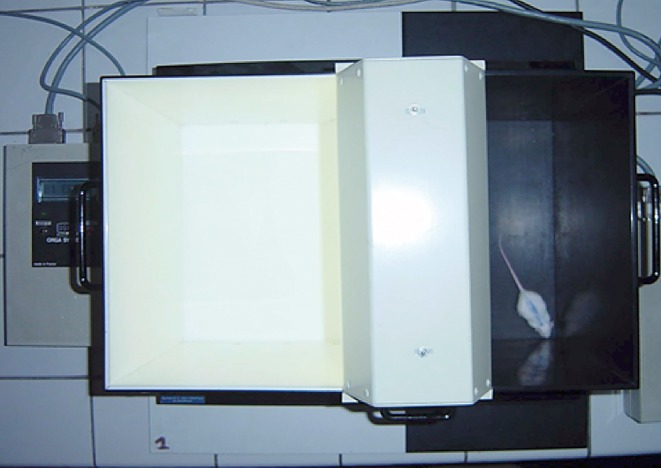
In parallel with these developments, additional indices of anxiolytic activity have been championed, eg, relative behavioral activity/time spent in each compartment.19 Five main parameters are now available to assess the anxiolytic profile of drug treatment: the latency time for the first passage from the light compartment to the dark one, the number of transitions between the two compartments, the movement in each compartment, and the time spent in each compartment. Sometimes rearing and grooming are measured. BDZs decrease the number of attempts at entry in the aversive area as mice pass directly into the lit compartment without hesitation, a profile suggested of being indicative of anxiolytic-like activity. A parameter suggested as an index of the effect of anxiogenics is the “leaning out” or “peeking out” of the dark chamber by the mouse, where a decrease in the rate of leaning out appears to be a constant effect of standard anxiety-inducing drugs. However, these behaviors are invariably ignored in favor of a simple spatiotemporal index, and the measurement found to be most consistent and useful for assessing anxiolytic-like activity action is the time spent in the lit compartment, as this parameter provides the most consistent dose-effect responses with different compounds.19
There are a number of nongenetic, nonpharmacological manipulations that lead to modulation of the general stress levels of animals, which when performed before testing have profound effects on behavior in the L/D model. Prior exposure of mice to the EPM eliminates the anxiolytic response to diazepam in the L/D paradigm,20 whereas tail suspension acute stress immediately before the test can increase the sensitivity to anxiolytic-like responses. Forced swimming suppresses general behavioral activity and increases the disinhibition effect of diazepam in both compartments, whereas foot shocks given immediately before the test significantly reduced the activity in the dark compartment and did not affect the behavior in the light compartment. Exposure of CD-1 mice to predator odor (mimicked by 2,5-dihydro-2,4,5-trimethylthiazoline, or TMT) or control odor (mimicked by butyric acid or BA) induced anxiety in the L/D test relative to saline treated mice. Mice exposed to either TMT or BA took longer to re-enter the light section of the apparatus and also spent less time in the light division relative to mice exposed to saline.21 Data indicate that prior test experience seriously compromises the anxiolytic efficacy of chloradiazepoxide (CDP) in the mouse L/D test without significantly altering behavioral baselines.22 The choice of strain and age of the animal is also an important factor. Studies by Hascoet and colleagues23 indicate the preference for the Swiss mouse strain of 4 weeks of age, as an age-related effect was observed.
The light/dark box test is still useful for discovering new targets in the field of anxiety-related disorders.24
Four-plate-test
The four-plate test Figure 3. is based on the suppression of a simple innate ongoing behavior, ie, the exploration of novel surroundings, of the mouse. The apparatus consists of a floor made of four identical rectangular metal plates.
Figure 3. Four-plate-test apparatus.

This exploration behavior is suppressed by the delivery of mild electric foot shock contingent on quadrant crossings. Every time the mouse crosses from one plate to another, the experimenter electrifies the whole floor, eliciting a clear flight reaction from the animal. BDZs increase the number of punished crossings accepted by the animal.25 Before any conclusion can be drawn for a drug tried in this test, it is necessary to verify that this drug has no analgesic effects. This is verified utilizing a hot-plate apparatus, employing morphine as the control compound.
This paradigm is not commonly used in other laboratories, making it difficult to formulate inter-laboratory comparisons. As such, the various factors potentially- influencing the behavioral response of mice has not been profoundly studied. However, its success in our laboratory and the demonstration of an anxiolytic-like effect of ADs in this model (in comparison with many of the traditional paradigms employed) emphasizes the validity of this model.26 It was reported that a single prior undrugged exposure to the FPT reduces punished responding on retest at intervals ranging from 24 hours to 42 days.27 Furthermore, prior experience attenuates the anxiolytic response to the benzodiazepines diazepam and lorazepam, similar to results observed in the EPM and L/D.20
This test is very useful to explain the mechanisms of anxiolytic drugs using agonists or antagonists at the level of 5-HT, γ-aminobutyric acid (GABA), cholecystokinin, glutamate, and corticotrophin-releasing factor receptors (Table II).28-31 The FPT is being increasingly used for the detection of the anti-anxiety activity of potentially new anxiolytics.32
Table II. Classification of animal models of anxiety. BZD, benzodiazepine; 5-HT, serotonin; CCK, cholecystokynin; AD, adrenergic; GLU, glutamate; CRF, corticotropin-releasing factor; EPM, elevated plus maze; L/D, light/dark; FP, four-plate; ++: anxiolytic-like effect; +: anxiolytic-like effect or no effect, anxiogenic effect; 0: no effect.
| Animal models | BZD agonists | 5-HT1A agonists | 5-HT2A/2C antagonists | 5-HT3 antagonists | CCK-2 antagonists | AD agents | GLU | CRF |
| EPM | ++ | + | + | + | + | ++ | ++ | |
| L/D | ++ | ++ | + | + | + | - | ++ | |
| FP | ++ | ++ | ++ | 0 | NA | ++ | ++ |
Conclusion and perspectives
For screening new compounds the zebrafish (Danio rerio) is emerging as an important new species for studying mechanisms of brain function and dysfunction.33 Focusing on selected central nervous system (CNS) disorders (brain cancer, epilepsy, and anxiety) and using them as examples, the value of zebrafish models in translational neuroscience is being evaluated. Zebrafish can also be used in research into neuroimaging, circuit levels, and drug discovery. Outlining the role of zebrafish in modeling a wide range of human brain disorders, it is possible to find new applications and existing challenges in this field. Finally, the potential of zebrafish models in behavioral phenomics and high-throughput genetic/ small molecule screening, which is critical for CNS drug discovery and identifying novel candidate genes, is on the way. It is too early to compare the screening power of this test with rodent tests.
Although animal models of anxiety have relatively good validity, anxiolytic drugs with novel mechanisms are slow to emerge.34 The reasons appear to be linked to the difficulty of studying these types of drugs in clinical trials, because of the placebo response caused by the types of patients selected.
REFERENCES
- 1.Bourin M. Animal models of anxiety: are they suitable for predicting drug action in humans? Pol J Pharmacol. 1997;49:79–84. [PubMed] [Google Scholar]
- 2.Shekhar Al., McCann UD., Meaney MJ., et al Summary of a National Institute of Mental Health workshop: developing animal models of anxiety disorders. Psychopharmacology (Berl). 2001;157:327–239. doi: 10.1007/s002130100859. [DOI] [PubMed] [Google Scholar]
- 3.Belzung C. Rodent models of anxiety-like behaviors: are they predictive for compounds acting via non-benzodiazepine mechanisms? Curr Opin Investig Drugs. 2001;2:1108–1111. [PubMed] [Google Scholar]
- 4.Handley SL. 5-Hydroxytryptamine pathways in anxiety and its treatment. Pharmacol Ther. 1995;66:103–148. doi: 10.1016/0163-7258(95)00004-z. [DOI] [PubMed] [Google Scholar]
- 5.Bourin M., Petit-Demoulière B., Dhonnchadha BN., Hascöet M. Animal models of anxiety in mice. Fundam Clin Pharmacol. 2007;21:567–574. doi: 10.1111/j.1472-8206.2007.00526.x. [DOI] [PubMed] [Google Scholar]
- 6.Bourin M., Hascoet M. Implication of 5-HT2 receptor subtypes in the mechanism of action of the GABAergic compound etifoxine in the fourplate test in Swiss mice. Behav Brain Res. 2010;208:352–328. doi: 10.1016/j.bbr.2009.11.046. [DOI] [PubMed] [Google Scholar]
- 7.Steimer T. Animal models of anxiety disorders in rats and mice: some conceptual issues. Dialogues Clin Neurosci. 2011;13:495–506. doi: 10.31887/DCNS.2011.13.4/tsteimer. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Lister RG. Ethologically-based animal models of anxiety disorders. Pharmacol Ther. 1990;46:321–340. doi: 10.1016/0163-7258(90)90021-s. [DOI] [PubMed] [Google Scholar]
- 9.Millan MJ. The neurobiology and control of anxious states. Prog Neurobiol. 2003;70:83–244. doi: 10.1016/s0301-0082(03)00087-x. [DOI] [PubMed] [Google Scholar]
- 10.Lister RG. The use of a plus-maze to measure anxiety in the mouse. Psychopharmacology (Berl). 1987;92:180–185. doi: 10.1007/BF00177912. [DOI] [PubMed] [Google Scholar]
- 11.Pellow S., Chopin P., File SE., Briley M. Validation of open:closed arm entries in an elevated plus-maze as a measure of anxiety in the rat. J Neurosci Methods. 1985;14:149–167. doi: 10.1016/0165-0270(85)90031-7. [DOI] [PubMed] [Google Scholar]
- 12.Varty GB1., Morgan CA., Cohen-Williams ME., Coffin VL., Carey GJ. The gerbil elevated plus-maze I: behavioral characterization and pharmacological validation. Neuropsychopharmacology. 2002;27:357–370. doi: 10.1016/S0893-133X(02)00312-3. [DOI] [PubMed] [Google Scholar]
- 13.Belzung C., Griebel G. Measuring normal and pathological anxiety-like behaviour in mice: a review. Behav Brain Res. 2001;125:141–149. doi: 10.1016/s0166-4328(01)00291-1. [DOI] [PubMed] [Google Scholar]
- 14.Rodgers RJ., Johnson NJ. Factor analysis of spatiotemporal and ethological measures in the murine elevated plus-maze test of anxiety. Pharmacol Biochem Behav. 1995;52:297–303. doi: 10.1016/0091-3057(95)00138-m. [DOI] [PubMed] [Google Scholar]
- 15.Kocahan S., Akillioglu K. Effects of NMDA receptor blockade during the early development period on the retest performance of adult Wistar rats in the elevated plus maze. Neurochem Res. 2013;38:1496–1500. doi: 10.1007/s11064-013-1051-y. [DOI] [PubMed] [Google Scholar]
- 16.Daher F., Mattioli R. Impairment in the aversive memory of mice in the inhibitory avoidance task but not in the elevated plus maze through intraamygdala injections of histamine. Pharmacol Biochem Behav. 2015;135:237–245. doi: 10.1016/j.pbb.2015.05.023. [DOI] [PubMed] [Google Scholar]
- 17.Papp M., Litwa E., Gruca P., Mocaer E. Anxiolytic-like activity of agomelatine and melatonin in three animal models of anxiety. Behav Pharmacol. 2006;17:9–18. doi: 10.1097/01.fbp.0000181601.72535.9d. [DOI] [PubMed] [Google Scholar]
- 18.Bourin M., Hascoet M. The mouse light/dark box test. Eur J Pharmacol. 2003;463:55–65. doi: 10.1016/s0014-2999(03)01274-3. [DOI] [PubMed] [Google Scholar]
- 19.Hascoet M., Bourin M. A new approach to the light/dark test procedure in mice. Pharmacol Biochem Behav. 1998;60:645–653. doi: 10.1016/s0091-3057(98)00031-8. [DOI] [PubMed] [Google Scholar]
- 20.Rodgers RJ., Shepherd JK. Influence of prior maze experience on behaviour and response to diazepam in the elevated plus-maze and light/ dark tests of anxiety in mice. Psychopharmacology (Berl). 1993;113:237–242. doi: 10.1007/BF02245704. [DOI] [PubMed] [Google Scholar]
- 21.Hebb AL., Zacharko RM., Dominguez H., Trudel F., Laforest S., Drolet G. Odour-induced variation in anxiety-like behaviour in mice is associated with discrete and differential effects on mesocorticolimbic cholecystokinin mRNA expression. Neuropsychopharmacology. 2002;27:744–755. doi: 10.1016/S0893-133X(02)00354-8. [DOI] [PubMed] [Google Scholar]
- 22.Holmes A., Iles JP., Mayell SJ., Rodgers RJ. Prior test experience compromises the anxiolytic efficacy of chlordiazepoxide in the mouse light/dark exploration test. Behav Brain Res. 2001;122:159–167. doi: 10.1016/s0166-4328(01)00184-x. [DOI] [PubMed] [Google Scholar]
- 23.Hascoet M., Colombel MC., Bourin M. Influence of age on behavioural response in the light/dark paradigm. Physiol Behav. 1999;66:567–570. doi: 10.1016/s0031-9384(98)00333-3. [DOI] [PubMed] [Google Scholar]
- 24.Gallo I., Rattazzi L., Piras G., et al Formyl peptide receptor as a novel therapeutic target for anxiety-related disorders. PLoS One. 2014;9(12):e114626. doi: 10.1371/journal.pone.0114626. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Hascoet M., Bourin M. The four-plate test in mice. In: Gould TD, ed. Mood and Anxiety Related Phenotypes in Mice. Characterization Using Behavioral Tests. Vol II. New York, NY: Humana Press; 2011:123–141. [Google Scholar]
- 26.Hascoet M., Bourin M., Colombel MC., Fiocco AJ., Baker GB. Anxiolytic-like effects of antidepressants after acute administration in a four-plate test in mice. Pharmacol Biochem Behav. 2000;65:339–344. doi: 10.1016/s0091-3057(99)00191-4. [DOI] [PubMed] [Google Scholar]
- 27.Hascoet M., Bourin M., Couetoux du Tertre A. Influence of prior experience on mice behaviour using the four-plate test. Pharmacol Biochem Behav. 1997;58:1131–1138. doi: 10.1016/s0091-3057(97)00093-2. [DOI] [PubMed] [Google Scholar]
- 28.Masse F., Hascoet M., Bourin M. alpha2-Adrenergic agonists antagonise the anxiolytic-like effect of antidepressants in the four-plate test in mice. Behav Brain Res. 2005;164:17–28. doi: 10.1016/j.bbr.2005.05.017. [DOI] [PubMed] [Google Scholar]
- 29.Ripoll N., Hascoet M., Bourin M. Implication of 5-HT(2A) subtype receptors in DOI activity in the four-plates test-retest paradigm in mice. Behav Brain Res. 2006;166:131–139. doi: 10.1016/j.bbr.2005.07.013. [DOI] [PubMed] [Google Scholar]
- 30.Petit-Demouliere B., Masse F., Cogrel N., Hascoet M., Bourin M. Brain structures implicated in the four-plate test in naîve and experienced Swiss mice using injection of diazepam and the 5HT2A agonist DOI. Behav Brain Res. 2009;204:200–205. doi: 10.1016/j.bbr.2009.06.006. [DOI] [PubMed] [Google Scholar]
- 31.Massé F., Nic Dhonnchadha BA., Hascoët M., Bourin M. Anxiolytic-like effect of 5-HT(2) ligands and benzodiazepines co-administration: comparison of two animal models of anxiety (the four-plate test and the elevated plus maze). Behav Brain Res. 2007;177:214–226. doi: 10.1016/j.bbr.2006.11.031. [DOI] [PubMed] [Google Scholar]
- 32.Stawińxska A., Wierońska JM., Stachowicz K., et al Anxiolytic- but not antidepressant-like activity of Lu AF21934, a novel, elective positive allosteric modulator of the mGlu4 receptor. Neuropharmacology. 2013;66:225–235. doi: 10.1016/j.neuropharm.2012.05.001. [DOI] [PubMed] [Google Scholar]
- 33.Stewart A., Gaikwad S., Kyzar E., Green J., Roth A., Kalueff AV. Modeling anxiety using adult zebrafish: a conceptual review. Neuropharmacology. 2012;62:135–143. doi: 10.1016/j.neuropharm.2011.07.037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Cryan JF., Sweeney FF. The age of anxiety: role of animal models of anxiolytic action in drug discovery. Br J Pharmacol. 2011;164:1129–1261. doi: 10.1111/j.1476-5381.2011.01362.x. [DOI] [PMC free article] [PubMed] [Google Scholar]


