Abstract
Aim:
The aim of the current study was to determine the prevalence of grand multiparity and the associated risks factors.
Methods:
Four hundred thirty grandmutliparas (parity 5 or more) were compared with multiparous population (parity 2-4) with regard to maternal age, gestational age, mode of delivery, fetal and maternal outcomes and inter-current medical and obstetrical problems.
Results:
There were significant association between grand multiparity and adverse pregnancy outcomes such as cesarean delivery (OR=2.699, CI=2.072-3.515, p<0.001), fetal macrosomia (OR=1.675; 95% CI=1.004- 2.796, p=.048), Diabetes mellitus (OR=1.634, 95%CI=1.076-2.481, p=0 .021), and pregnancy induced hypertension (OR=1.838, 95% CI=1.054-3.204, p= .032). No significant associations were seen in placenta abruption, placenta previa, preterm labor, postpartum hemorrhage and the frequency of admission to neonatal intensive care unit. No prenatal or maternal mortality was reported in this study.
Conclusion:
Grand multiparty remains a major obstetrics problem. It is associated with many medical and obstetrical complications. In communities where large family is desirable it is important to address the value of family planning and conduction of meticulous antenatal care.
Keywords: Grand multiparity, Pregnancy outcome, Obstetric complications, Neonatal morbidity
1. INTRODUCTION
Grand multiparity has been considered an independent factor for increasing adverse outcome for both fetus and mother specially diabetes mellitus, antepartum hemorrhage, malpresentation, cesarean section rate, postpartum hemorrhage, iron deficiency anemia, and a high perinatal mortality rate Al JF (1). More recent reports, however, have demonstrated that in the presence of good perinatal care, grand multiparity no longer need to be considered an obstetrical risk in the presence of satisfactory health care conditions (2, 3). The majority of the studies argued that grand multiparas are more likely to be of old age which might be the reasons for increased morbidity and mortality. In our clinical practice, such factor is difficult to be removed because women’s age is the most important biological variable that influences the reproductive events which we study.
In Saudi Arabia, large family is desirable for cultural reasons; consequently, a high incidence of grand multiparity is expected. The Fertility rate in Saudi Arabia was last reported at 2.81 in 2010, according to a World Bank report published in 2012 (4). In addition, early age of marriage might be one of the reasons for this high incidence of grand multiparas. The current study was conducted in a tertiary hospital where medical care is given free of charge for all mothers. The aims of the current study were to determine the prevalence and to investigate the feto-maternal outcomes related to grand multiparity.
2. METHODS AND SUBJECTS
In this retrospective study, the data were gathered from patient’s case notes over a period of a 1-year from January 1, 2012 through December 31, 2012 at the Maternity and Children Hospital (MCH), Buraidah, Saudi Arabia in an attempt to determine the prevalence of grand multiparity and its associated risks.
The MCH is a tertiary hospital where medical care is given free of charge. Uncomplicated cases received antenatal care at the level of primary health care centers, whereas complicated and referred cases are managed at the hospital. All deliveries took place in the hospital, and no home confinements were allowed.
In this study, a grand multiparas woman was defined as a woman who gave birth to 5 and more deliveries after 24 weeks gestations (5). A total of 8040 deliveries was performed during the year, of these 430 were grand multiparas which were the actual number of grand multiparity during the whole year. They were matched to 657 multiparas (parity 1-4) women who delivered during the same time scale.
Sociodemographic factors, obstetric complications, and neonatal morbidity for both groups were recorded from the case note. Maternal variables we assessed included diabetes mellitus, hypertensive disorders of pregnancy, premature rupture membrane, placental abruption, placenta previa, medical problems (such as asthma, epilepsy and hypothyroidism), postpartum hemorrhage, tears, cesarean hysterectomy, preterm labor, mode of delivery and post term labor(diabetes was assessed separately because it is important variable for pregnancy outcomes). Each of these variables was analyzed against each group. For clarity, medical problems included (asthma, epilepsy and hypothyroidism) and diabetes included both pre-existing and gestational diabetes. Macrosomia is defined as fetal weight greater or equal to 4kg.
Fetal variables we assessed were Admission to nursery, small for gestational age, fetal death, Apgar score, fetal weight, gestational age at delivery, fetal distress and macrosomia. Each of the fetal complications was assessed against each group. This study was approved by the Ethics Committee of the College of Medicine of Qassim University.
2.1. Statistical analysis
The Statistical Package for the Social Sciences (SPSS 17 for Windows) was used for recording and statistical analyses of data. The descriptive statistics used included the mean, the frequency distribution and the standard deviation. A chi-square test was used to compare the means of qualitative data, whereas a Student’s t-test was used to compare the means of quantitative data. In multivariate analysis, all independent variables were added to the model at the same time. The results of the analysis are presented as odds ratio (OR) and 95% confidant interval (95% CI). The test of significant was set at a p<.05.
3. RESULTS
The total number of deliveries during the study period was 8040, of these 430 were grand multiparas. Thus, the prevalence of grand multiparity was 5.3 %. Of 430, grand multiparas, 28.6% (123) were below 35 years of age (younger grand multiparas), in this group the CSR was 27.2% (72). There was no significant differences in the CS rate when they were compared with those above 35 years of age 72.8 %(307) p=0.666 as show in Table 1.
Table 1.
Distribution of parity according to age group. Values were presented as number (percentage)
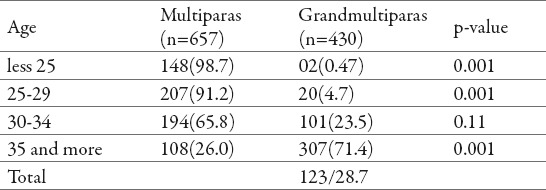
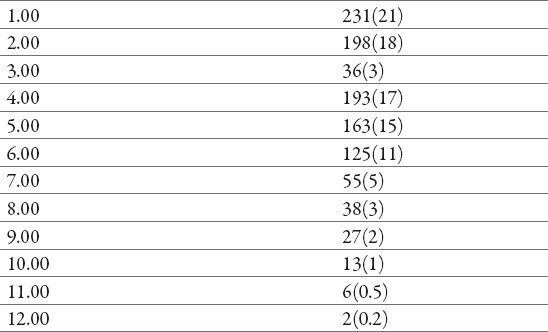
Table 2 shows the frequency of the individual parity and the associated percentage.
Table 2.
Distribution of different parities and the associated percentage. Values are presented as number (percentage)
In this study, the distribution of age according to parity showed a linear relationship with good agreement with p-p plot distribution. There were significant differences in maternal age (28.8828±5.26145 vs. 36.8488±4.40522; p<0.001), number of previous abortions (.3181±.60298 vs. .8279±1.05916; P<.001), gestational age at delivery (38.4556±1.75031 vs. 38.0695±2.00399; P=0.001) and the number of parity (2.2907±1.22442 vs. 6.3349±1.52353; P<0.001) between the study and the control groups. Fetal weight was similar between the two groups (p=.751).
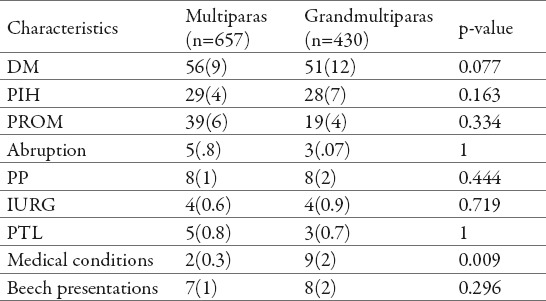
Chi-square test was used to explore the differences in the antenatal complication between the multiparas and the grand multiparas women. For clarity, PIH includes both preeclampsia and superimposed hypertension. Medical disorders reported include (bronchial asthma which constituted the majority, hypothyroidism and epilepsy). As listed in Table 3, grand multipara women had a higher frequency for medical disorders (p=009), but both groups did not differ significantly in other antenatal obstetrics complications (p>0.05).
Table 3.
Comparison of antenatal complications between multiparas and grandmultipars. Values are presented as number (percentage)
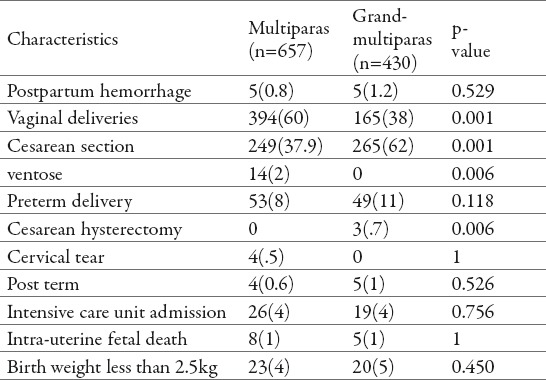
Chi-Square test and Fisher’s exact test (cell count less than 5) were used to examine the differences between some post partum obstetrical complications between multiparas and grand multiparas. Grand multiparas when compared to multiparous women they were at an increased risk of cesarean delivery (P<.001). On the other hand, multiparous women compared to grand multiparas were more likely to deliver by ventose (p=0.0062). Other postpartum complications did not differ significantly between the two groups (p>0.05) (Table 4).
Table 4.
Comparison of intrapartum complications and fetal outcome in multiparas and grandmultiparas. Values are presented as number (percentage)
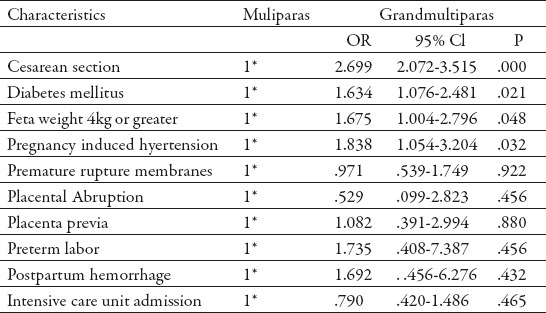
Binary logistic regression was used to explore the association of some selected antenatal and postnatal variables between multiparas and grand multiparas as presented in table 5. Grand multiparas were significantly associated with increased incidence of cesarean section (OR=2.699, CI=2.072-3.515, p<0.001), macrosomic babies (OR=1.675; 95% CI=1.004-2.796, p=.048), diabetes mellitus (OR=1.634, 95%CI=1.076-2.481, .021) and PIH (OR=1.838, 95% CI=1.054-3.204, p= .032). Logistic regression analyses demonstrated that grand multiparas were not significantly associated with increased risk of hypertensive disorders, PROM, preterm delivery, IUFD, abruption, postpartum hemorrhage and IUGR.
Table 5.
Odds ratio and 95% confidence interval for grandmultiparity and some selected pregnancy outcomes. 1* reference category, Abbreviations: OR, odds ratio; CI confident interval
4. DISCUSSION
The incidence of grand multiparity in the current study was 5.3 %. Due to the lack of consensus on the definition of grand multiparity, previous regional studies from Saudi Arabia have documented different incidence of grand multiparity (1, 6). Higher prevalence of grand multiparty was reported in developing countries (7, 8). The low prevalence rate of grand multiparity in this study can be explained by the high acceptance of family planning. Jabbar et al. in their study, which included 2675 Saudi women attending a gynecology out- patient, demonstrated that 56.0% of women were using some form of contraceptive (9).
Of the 430 grand multiparas in this study, 123(28.6) were less 35 years of age, which indicate early age of marriage leading to the concept of “younger grand multiparity” and which may constitute additional risk for further complications. There was no significant difference in the rate of CS between grand multiparity age less than 35 years compared to those greater than 35 years of age (60.0% vs. 62.3% p= 0.666).
In the current study, we found that there was a significant association between grand multiparity and adverse pregnancy outcomes (such as cesarean delivery, fetal macrosomia, Diabetes mellitus and pregnancy induced hypertension). These findings contradict with previous findings (10, 11, 12, 13) which concluded that grand multiparity is not associated with increased risk for adverse pregnancy outcomes. Certainly, our data support previous published findings (14, 15, 16, 17) which stated that grand multiparity continue to constitute potential risks for adverse pregnancy outcomes even after controlling for confounders.
The high rate of CS among grand multiparas women in this study can be explained by high frequency of fetal macrosomia, diabetes mellitus and pregnancy induced hypertension (p<0.05). All of these complications of pregnancy are well documented to increase the rate of cesarean delivery. This data showed, that within grand multiparity, 120(27.9%) of grand multiparas were less than 35 years of age, of whom 72(60%) were delivered by CS with no significant differences compared to those greater than 35 years of age, (p=0.666). This indicates that, this group of women started their reproduction before pelvic maturity and consequently resulted in high rate of CS due to feto-pelvic disproportion. While the high rate of CS among old grand multiparity, may be due to secondary contracted pelvic as a result of repeated compensatory lordosis of pregnancy (18).
This study revealed that there was no significant association between grand multiparity and placenta abruption, placenta previa, preterm labor, postpartum hemorrhage and babies admission to the intensive care unit (ICU), p>0.05. This agreed with other findings. Nassar and colleagues observed no significant differences in antepartum hemorrhage, intrauterine growth restriction and stillbirth rates (8, 19). However, Rayamajhi et al., reported stronger association of hypertensive disorders in pregnancy, preterm birth, anemia, postpartum hemorrhage in the grand multiparity (20).
In his study, 3 (.7%) cases of grand multiparity underwent hysterectomies, one for complete placenta previa and two for uncontrolled postpartum hemorrhage, giving a hospital incidence of one in 2680 deliveries, a comparable incidence of one in 2581 was reported from Tunisia (21). No maternal death was reported in this report.
In the current study, there was no significant association between grand multipara and admission to ICU, intrauterine fetal death and low birth weight babies.
The shortcomings of this study are its retrospective nature and the gathering of data from a single center rather than multicenter (the latter of which could be more reprehensive of the population).
5. CONCLUSION
In view of the results obtained in this study, we feel that grand multiparity continue to pose additional risk for pregnancy outcomes even in modern obstetrics care. In a community where large family is desirable, still there is a place for family planning. Again, conduction of good antenatal and intrapartum care will result in much reduction of these adverse outcomes for both fetus and mother. Further study is warranted to investigate the outcome of younger grand multiparty.
Footnotes
CONFLICT OF INTEREST: NONE DECLARED.
REFERENCES
- 1.Al JF. Grand multiparity: a potential risk factor for adverse pregnancy outcomes. J Reprod Med. 2012 Jan-Feb;57(1-2):53–57. [PubMed] [Google Scholar]
- 2.Kumari AS, Badrinath P. Extreme grand multiparity: is it an obstetric risk factor? EurJ Obstet Gynecol Reprod Biol. 2002 Feb 10;101(1):22–25. doi: 10.1016/s0301-2115(01)00498-5. [DOI] [PubMed] [Google Scholar]
- 3.Kaplan B, Harel L, Neri A, Rabinerson D, Goldman GA, Chayen B. Great grand multiparity - beyond the 10th delivery. Int J Gynaecol Obstet. 1995 Jul;50(1):17–19. doi: 10.1016/0020-7292(95)02417-b. [DOI] [PubMed] [Google Scholar]
- 4. http://www.tradingeconomics.com/saudi-arabia/fertility-rate-total-births-per-woman-wb-data.html .
- 5.Shahida SM, Islam MA, Begum S, Hossain MA, Azam MS. Maternal outcome of grand multipara. Mymensingh Med J. 2011 Jul;20(3):381–385. [PubMed] [Google Scholar]
- 6.Evaldson GR. The grand multipara in modern obstetrics. Gynecol Obstet Invest. 1990;30(4):217–223. doi: 10.1159/000293273. [DOI] [PubMed] [Google Scholar]
- 7.Akwuruoha E, Kamanu C, Onwere S, Chigbu B, Aluka C, Umezuruike C. Grand multiparity and pregnancy outcome in Aba, Nigeria: a case-control study. Arch Gynecol Obstet. 2011 Feb;283(2):167–172. doi: 10.1007/s00404-009-1296-5. [DOI] [PubMed] [Google Scholar]
- 8.Duria A Rayis, Abdel Aziem A Ali, Ameer O. Abbaker, Ishag Adam Maternal and perinatal outcomes of grand multiparity in Kassala hospital, eastern Sudan. Khartoum Medical Journal. 2011;4(1):554–557. [Google Scholar]
- 9.Jabbar FA, Wong SS, Al-Meshari AA. Practice and methods of contraception among Saudi women in Riyadh. Fam Pract. 1988 Jun;5(2):126–128. doi: 10.1093/fampra/5.2.126. [DOI] [PubMed] [Google Scholar]
- 10.Nordin NM, Fen CK, Isa S, Symonds EM. Is grand multiparity a significant risk factor in this new millennium? Malays J Med Sci. 2006 Jul;13(2):52–60. [PMC free article] [PubMed] [Google Scholar]
- 11.Kumari AS, Badrinath P. Extreme grand multiparity: is it an obstetric risk factor? Eur J Obstet Gynecol Reprod Biol. 2002 Feb 10;101(1):22–25. doi: 10.1016/s0301-2115(01)00498-5. [DOI] [PubMed] [Google Scholar]
- 12.Samueloff A, Schimmel MS, Eidelman AI. Grand multiparity. Is it a perinatal risk? Clin Perinatol. 1998 Sep;25(3):529–538. [PubMed] [Google Scholar]
- 13.Goldman GA, Kaplan B, Neri A, Hecht-Resnick R, Harel L, Ovadia J. The grand multipara. Eur J Obstet Gynecol Reprod Biol. 1995 Aug;61(2):105–109. doi: 10.1016/0301-2115(95)02108-j. [DOI] [PubMed] [Google Scholar]
- 14.Yasmeen S, Danielsen B, Moshesh M, Gilbert WM. Is grand multiparity an independent risk factor for adverse perinatal outcomes? J Matern Fetal Neonatal Med. 2005 Apr;17(4):277–280. doi: 10.1080/14767050500123798. [DOI] [PubMed] [Google Scholar]
- 15.Rayamajhi R, Thapa M, Pande S. The challenge of grand multi-parity in obstetric practice. Kathmandu Univ Med J (KUMJ) 2006 Jan-Mar;4(1):70–74. [PubMed] [Google Scholar]
- 16.Akwuruoha E, Kamanu C, Onwere S, Chigbu B, Aluka C, Umezuruike C. Grand multiparity and pregnancy outcome in Aba, Nigeria: a case-control study. Arch Gynecol obstet. 2011 Feb;283(2):167–172. doi: 10.1007/s00404-009-1296-5. [DOI] [PubMed] [Google Scholar]
- 17.Abasiattai AM, Utuk NM, Udoma EJ, Umoh AV. Grand multiparity: outcome of delivery in a tertiary hospital in southern Nigeria. Niger J Med. 2011 Jul-Sep;20(3):345–348. [PubMed] [Google Scholar]
- 18.Donald I. The grand multipara. In: Donald I, editor. practical obstetrical problems. 5th edition. London: L Ioyd Luke L td; 1988. pp. 138–141. [Google Scholar]
- 19.Nassar AH, Fayyumy R, Saab W, Mehio G, Usta IM. Grand multiparas in modern obstetrics. Am J Perinatol. 2006;23:345–349. doi: 10.1055/s-2006-947158. [DOI] [PubMed] [Google Scholar]
- 20.Rayamajhi R, Thapa M, Pande S. the Challenge of Grandmulti-perity in obstetric practue. Kathmandu Univ Med J (KUMJ) 2006;4:70–74. [PubMed] [Google Scholar]
- 21.Ahmadi S, Nouira M, Bibi M, Boughuizane S, Saidi H, Chaib A, Khairi H. [Uterine rupture of the unscarred uterus. About 28 cases] Gynecol Obstet Fertil. 2003 Sep;31(9):713–717. doi: 10.1016/s1297-9589(03)00212-1. [DOI] [PubMed] [Google Scholar]


