Abstract
Introduction:
Tuberculosis is a single-agent infectious disease, which is the major cause of death around the world. Approximately one third of the world’s population is infected with tuberculosis (TB) bacilli and at risk of developing active TB. The purpose of this study was determined the impact of education based on health belief model in promoting behavior of smear-positive pulmonary TB among patients in Chabahar city, Iran.
Material and methods:
Of the 80 smear-positive pulmonary TB who referred to health centers in Chabahar voluntarily participated in this interventional study. The data collected using questionnaire based on health belief model. The data were analyzed by using paired t-test, independent t-test, pearson correlation and chi-square test with SPSS 16.
Results:
The cognitive skills were increased significantly from 6.10 to 6.88 after intervention. All behavioral skills were increased significantly from 2.08 to 2.88 after implementing the intervention. Perceived severity was increased from11.08to12.19 significantly. Percepted benefits were enhanced significantly from 11.48 to 12.23. Mean percepted barrier was decreased significantly from 17.52 to 16.68.
Conclusion:
Findings demonstrated that implementing educational intervention programs can increase the level of knowledge and behavior of patients regarding smear- positive pulmonary TB initiatives.
Keywords: educational intervention, positive-smear pulmonary TB, health belief model
1. INTRODUCTION
Tuberculosis is a single-agent infectious disease, which is the major cause of death around the world (1). In humans it is caused by the Mycobacterium Tuberculosis complex and in most cases is caused by Mycobacterium Tuberculosis (2). Approximately one third of the world’s population is infected with tuberculosis (TB) bacilli and at risk of developing active TB (3). Smear-positive pulmonary TB (PTB) constitutes 34% of new TB cases and is most likely a source of TB transmission in the community (4). In 2010, there were an estimated 12 million TB cases, including 8.8 million incident cases (5). The geographical location of Iran and its neighborhood, with some countries having a high prevalence of tuberculosis, require our considerable attention to this disease (6). Epidemiological data in 2010 showed that about 13.7 million people in the world were infected with tuberculosis, of which more than 80% belonged to 22 developing countries (7). Among 22 countries in Eastern Mediterranean, nine countries including Pakistan, Afghanistan, Egypt, Iraq, Iran, Morocco, Somalia, Sudan and Yemen are accounted for 95% of TB cases. In this regard, 51% of TB cases occurred in Pakistan (8). Directly observed treatment short-course (DOTS) is the strategy recommended by the World Health Organization (WHO) for controlling tuberculosis (9). The successful performance of DOTS in fighting against tuberculosis requires the collaboration of all sections giving health-clinical services including clinical health networks, hospitals and university centers and private physicians (10). Iran is at serious risk of this disease since it is adjacent to Pakistan and Afghanistan, which are the most infected areas in the world. Nowadays, Iran has the seventeenth rank with infection rate of 17.9% and incidence of 26 per hundred thousand people in the world (11, 12, 13). Chabahar city in Sistan and Baluchestan Province (Iran) is one of the major places where tuberculosis is prevalent. The highest incidence of this disease is observed in this area (14). There will be many reasons for this high incidence. This may be due to the fact that Chabahar is adjacent to Pakistan with incidence of 100-300 cases per 100 thousands individuals (15). This may also be due to high rate of traffic at the border between these two countries and poor nutritional status of people (high prevalence of malnutrition, particularly among children) (16).
Health belief model is a cognitive model attempting to identify and predict health behavior (17). Due to perform healthy behaviors, according to such model, one should initially perceive the risk of contracting the health condition of concern (perceived susceptibility) and the seriousness and severity of the consequences and complications derived from such condition with its all physical, psychological, social and economic dimensions (perceived severity) by receiving positive cues in the form of incentives from external or internal environments (cues to action) and finally take action after believing in its suitability and applicability (18). The health belief model is the first behavior change model and is accepted widely in empirical applications (19). Effectiveness of Health Belief Model (HBM) was proved by researchers in preventive behaviors such as brucellosis (16), breast cancer (20) and cervical (21) in the country. With regard to performance of HBM in promoting self-care behaviors such as smear-positive pulmonary tuberculosis, which is a health-behavioral problem that threatens public health. The present study aimed to determine the effect of health education program in promoting self-care behaviors in positive-smear pulmonary TB cases using HBM under supervision of Health Center in Chabahar city in 2013.
2. PATIENTS AND METHODS
This is a quasi-experimental study with pre-test and post-test. This was conducted on 80 smear positive TB patients under supervision of Health Center in Chabahar in 2013. Inclusion criteria were that at least one month has passed since initial diagnosis and treatment, at least 3 months of treatment remains to be completed. According to results obtained in other studies (22(, mean score of performance of patients in pre-intervention has increased from 12.6 to 14.1 after intervention. Sample size was obtained as 29 individuals with 95% certainty and 80% power of test. Finally, the sample size was calculated as 80 subjects (40 subjects per group) to increase accuracy of study and reduce effects of discarding the sample.
The study was conducted in Chabahar Health Center. Moreover, stratified random sampling method was used to select the sample. Then, two rural and two urban health centers were considered either as a class. Following rural and urban health care centers were selected from each one of the classes proportional to population of centers, number of patients and inclusion criteria. The sample was selected using systematic random sampling method. Urban health care centers included two urban centers of number four and number one in which 16 subjects as test and 16 patients as control were selected. Three rural centers were selected in which 24 subjects as test and 24 subjects as control were selected.
Initially, an extensive search was conducted in field of the main study in which studies conducted in Iran and abroad were examined. The tool used in this study, i.e. questionnaire, was developed based on HBM. This questionnaire included questions on constructs of the model, perceived severity, perceived benefits, perceived barriers, cause to action, self-efficacy, knowledge, self-care behaviors and demographic information (8 questions). Face and content validities were used to examine validity of the questionnaire while an internal consistency method with Cronbach’s alpha was used to examine reliability of the questionnaire. The questionnaire also included views of several professors and specialists in health education as well as specialists in infectious diseases and tropical medicine, epidemiology and statistics.
A number of 20 sheets questionnaires were distributed among those who were not included in our study to estimate the reliability. Tools to measure perceived severity, perceived benefits, perceived barriers, and self-efficacy: For this purpose, a scale respectively consisting of five questions, 6 questions, 7 questions and 6 questions with three-points likert scale (agree, no opinion, disagree) was designed in which the expected response was given 3 points, no opinion response was given 2 points and the wrong response was given 1 point. Tool to measure cause to action: for this purpose, a scale consisting of 6 questions with three points Likert scale was designed in which yes or there is a guide was given 3 points, I do not remember/rarely / has not happened was given 2 points, no or there is no guide was given 1 point. Tools to measure knowledge; for this purpose, 12 multiple-choice questions were designed in which the expected response was given one points and the wrong answer was given a score of zero. Tool to measure self-care behaviors: for this purpose, 6 multiple-choice questions were designed in which the expected behavior was given one score while the wrong behavior was given a score of zero. According to objectives, available resources, and results obtained from pre-test, training needs assessment was performed. Then, training methods, the number of required sessions for training were identified. Training sessions for groups were held in a face to face manner (in the case of patients living in rural areas; in the patient’s home or rural health centers or health care houses where patients were housed, and in the case of urban areas in the patient’s homes) by the researcher. They were held within two months. Each session lasted for half an hour to one-hour sessions. The control group received no intervention. Teaching materials included training booklets and pamphlets in the field of tuberculosis. Content provided by face to face trainings were exactly the same ones included within the booklets and pamphlets. After a month as an intervention period or re-training, the subjects (intervention and control) were examined in order to measure the impact of intervention at post-test.
Statistical analysis
Data collected in the second phase was analyzed. Then, the results were compared with the data collected at pre-test. Pearson correlation coefficient was used to investigate the relationship between model constructs and tuberculosis preventive behaviors. Independent t-test was used to examine differences in mean scores of constructs between the two groups. Paired t-test was used to investigate the difference in mean scores of constructs before and after the intervention in one group. P-values less than 0.05 were considered significant. Moreover, chi-square test was used to examine difference in demographic data between the two groups. The difference between variables within both groups was studied using SPSS16.
3. RESULTS
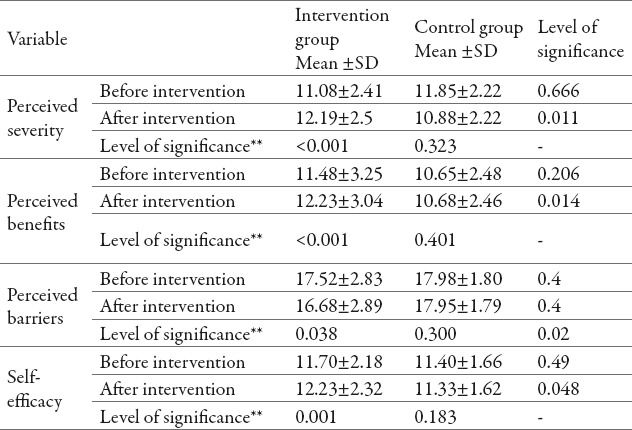
Most subjects under study were between 60 and 80 years old (30%). In addition, 47.5% of the subjects were male while 52.5% were female. Meanwhile, 67.5% of subjects were married. Moreover, 60% of the subjects were illiterate. Most of the subjects under study lived in rural areas (61.3%). Considering the number of family members, 47.5% of the subjects had between 5 and 10 family members. Incomes of majority of subjects (45%) were less than 2,000,000Rial (IRR) (currency in Iran) per month. According to chi-square test, there were no significant differences between experimental and control groups in terms of demographic data (age, sex, marital status, occupation, training level, place of residence, the number of family members and income) (P<0.05). Changes in mean scores of patients’ behaviors and knowledge in both intervention and control groups in terms of promoting self-care behaviors before and after interventions are shown in Table 1. According to contents of this table and results obtained from independent t-test, there is a significant difference between changes in mean scores of knowledge and behavior after intervention in both experimental and control groups (P<0.05). The comparison of mean scores of HBM constructs (perceived severity, perceived benefits, perceived barriers and self-efficacy) are shown in Table 2. As it is clear from contents of this table, there are no significant differences in mean scores of perceived severity, perceived benefits, perceived barriers and self-efficacy constructs between intervention and control groups before intervention according to independent t-test. However, there are significant differences in mean scores of perceived severity, perceived benefits, perceived barriers and self-efficacy constructs between Intervention and control groups after intervention (P<0.001).
Table 1.
Comparison of changes in mean and standard deviation of scores of patients’ Knowledge and behaviors in terms of promoting self-care behaviors before and after the intervention in both intervention and control groups
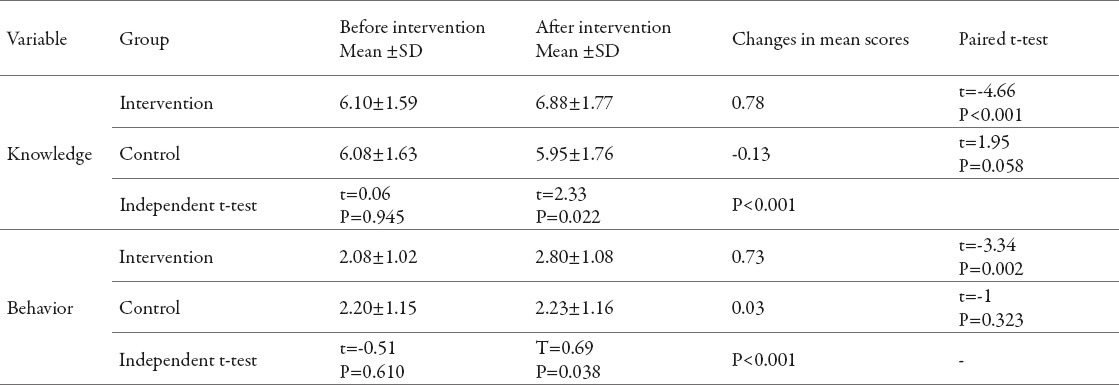
Table 2.
Comparison of mean scores of perceived severity and susceptibility, perceived benefits, perceived barriers and self-efficacy in relation to self-care behaviors in both Intervention and control groups before and after intervention. *independent t-test**paired t-test
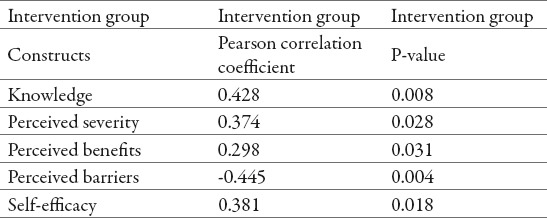
The most important cause to action for patients under study is health professionals, doctors and family members. Table 3 showed the correlation between knowledge and HBM constructs and self-care promoting behaviors in patients with positive-smear pulmonary tuberculosis. According to pearson correlation coefficient, it was observed that there is a significant relationship between knowledge and HBM constructs and self-care promoting behaviors. The relationship between knowledge and constructs of perceived severity, perceived benefits and self-efficacy was directed while the relationship between the former and perceived barriers was reversed.
Table 3.
Examining the correlation between knowledge and HBM constructs and promoting self-care behaviors in patients with smear- positive pulmonary TB in intervention group
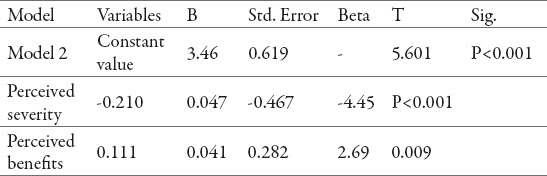
The absolute effects of changes in independent variables (perceived severity and perceived benefits) on dependent variables (behavior) in the intervention group are shown in Table 4. Examining the absolute effect of each independent variable indicated that respectively perceived severity and perceived benefits have the greatest impact on behavior. In addition, every one-unit increase in the variable perceived severity and perceived benefits changes behavior variable by -0.467 and 0.282, respectively.
Table 4.
The absolute effects of changes in independent variables (perceived severity and perceived benefits) on changes in dependent variables (behavior) in intervention group
4. DISCUSSION
The results of the present study suggested effectiveness of a training intervention in the intervention group. One of the concepts studied in this research was perceived intensity. According to contents in table 2, there was no significant difference between the two groups considering this variable both before and after intervention. However, this difference was significant in the intervention group both before and after the intervention while it was not significant in the control group. These results suggested that education was effective on health belief model constructs considering perceived severity. These findings were similar with the results obtained by Ghaffari et al. (23), Asadpour et al. (24) and Wai et al. (25), which were all based on the HBM. These study showed that an increase in mean scores of perceived intensity in training interventions. However, Austin et al. (26) conducted a study using HBM that their results showed that decreased perceived severity was a major obstacle to preventive behaviors.
The results of this study showed that construct of perceived benefits was not significantly different between the two groups before intervention (P<0.05) (Table 2). However, this difference was significant after the intervention (P=0.04). According to contents of this table, the difference between mean scores was significant both before and after intervention in the intervention group (P<0.001). However, this was not the case in the control group (P=0.07). Sarani (27) and Karimi et al. (28) showed that there was no significant difference between the two groups before education considering perceived benefits construct. But, this difference was significant after intervention in the group (P=0.0001). In addition, this difference was significant in the two groups after intervention. Considering perceived benefits construct, it was concluded that TB patients still need education about self-care behaviors, timely medication and adherence to health workers instructions in Chabahar city.
In terms of perceived barriers construct, there was no significant difference between the two groups before intervention. However, this difference was significant after intervention (Table 2). This difference was significant before and after intervention in the Intervention group in which perceived barriers were reduced. However, comparing results before and after intervention in the control group showed no significant difference (Table 2). Although Sarani (27) expected a significant reduction in perceived barriers in the intervention group, the results were conflicting. In general, perceived barriers in performing self-care behaviors regarding TB patients include a wide range of physical, psychological, environmental barriers and other factors. It is expected that training programs focus on these barriers to influence environmental factors since several number of barriers are beyond individual control. For example, the long distance between TB patients’ homes and service provider centers, not having enough time to visit these centers, especially for employed individuals, not having enough money to pay for commuting costs and experimental observation, not visiting centers because people are suspicious about them can be cited as examples of these barriers (27). In addition, Shamsi et al. (29) and Koch (30) were showed that mean scores of perceived barriers reduced in their studies. Their results were similar with obtained results in the present study. One of the implications of this study was cause to action. Most frequent cause to action was health professionals, doctors and family members of patients. Sarani (27) showed that most frequent cause to action were doctors, health workers, patients’ families, radio and books. It can be concluded that TB patients still need to be trained by health care workers, technicians, experts, practitioners and other sources considering this construct in Chabahar city.
Self-efficacy is another HBM construct. According to contents of table 2, there was no significant difference between the two groups before and after intervention in terms of this construct (P>0.05). But, there was significant difference between mean scores of self-efficacy in the intervention group both before and after intervention while this difference was not significant in the control group.
These findings was indicated the effect of training intervention in enhancing self-efficacy in the intervention group in performing and promoting self-care behaviors. This finding was likely with results obtained by Shamsi et al. (29) and Peyman et al. (31). Their results were suggested that training intervention was effective in knowledge of intervention group. Contents of table 1 showed that the two groups had no significant difference before training intervention. However, there was significant difference between the groups after intervention (P=0.001). These results were in line with results obtained by Olayemi et al. (32), Abebe et al. (33) and Shams (34). They reported that training intervention was effective in knowledge of intervention group (P=0.0001). The results also showed that self-care behaviors were significantly promoted in the intervention group after intervention in contrast to pre-intervention results, which showed no significant difference between the two groups (P>0.05). However, both groups showed significant differences after the intervention (P<0.001) (Table 2). In addition, comparison of mean scores obtained before and after intervention was showed significant difference in the intervention group after the intervention. However, this difference was not significant in the control group. Comparison of levels of self-care behaviors in the intervention group before and after intervention showed that although training intervention was effective in promoting self-care behaviors, this kind of interventions is still needed and should be repeated in this region. Olayemi et al. (32), Sarani (27) and Tahir-aziz et al. (35) also showed the effectiveness of training interventions in preventive behavior or adherence to treatment or model constructs. Based on contents in Table 3 considering pearson correlation, model constructs and knowledge are useful predictors to enhance self-care behaviors. Given these findings, we can conclude that individual self-care behaviors can be promoted by both increasing knowledge and decreasing perceived barriers. Mathuria et al. (36) illustrated significant difference between being aware of disease and symptoms patients’ behavior. Haj-amiri et al (37) reported a positive correlation between knowledge and observing treatment regimen. Furthermore, regression analysis showed that the model considered in this study was significant. In other words, the model was able to explain (predict) changes in dependent variable (behavior).
5. CONCLUSION
The results showed that educating people based on the Health Belief Model (HBM) has strong effects on knowledge, constructs of model and self-care behaviors of patients on tuberculosis. Given the high rate of illiteracy as a limitation of the study, development and application of training films based on Health Belief Model to patients about personal hygiene and health behavior recommended.
Footnotes
CONFLICT OF INTEREST: NONE DECLARED.
REFERENCES
- 1.WHO. Geneva, Switzerland: 2011. Global Tuberculosis Control Report. [Google Scholar]
- 2.Mirhaghani L, Nasehi M. Tehran: Seda. The guideline of tuberculosis prevention. 2002 [Google Scholar]
- 3.WHO. Geneva, Switzerland: 2009. Global Tuberculosis Control Report. [Google Scholar]
- 4.WHO. Geneva, Switzerland: 2010. Global Tuberculosis Control Report. [Google Scholar]
- 5.WHO. Geneva, Switzerland: 2008. WHO Three I’s Meeting Intensified Case Finding (ICF), Isoniazid Preventive Therapy (IPT) and TB Infection Control (IC) for people living with HIV, Report of a Joint World Health Organization HIV/AIDS and TB Department Meet ng. [Google Scholar]
- 6.Tuberculosis. bulletin of the national TB day. Center for Diseases Control (CDC), Iranian Ministry of Health and Medical Education. 2004 [Google Scholar]
- 7.Young DB, Perkins MD, Duncan K, Barry CE. III confornting the Scientific obstacles to global control of tuberculosis. J Clin Invest. 2008;118:1255–1265. doi: 10.1172/JCI34614. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.MosaZadeh M, Parsaie MR, Bahrami S, Mirzaei MR, Abedini N. 19th national Congress on Tuberculosis; (15-17 October 2008) Vol. 18. Zanjan: Zanjan University of Medical Sciences; 2008. Comparative study of the treatment success rate of smear positive pulmonary TB cases in the Mazandaran province and six WHO regions in the 2004-2006 years. [Google Scholar]
- 9.WHO. An expanded DOTS framework for effective tuberculosis control. WHO/CDS/TB/2002297. 2002. Available from: http://whqlib-doc.who.int/hq/2002/WHO_CDS_TB_2002297.pdf . [PubMed]
- 10.Education needs of patients with pulmonary tuberculosis admitted to Taleghani Hospital in Urmia to comply with treatment regimen. 19th National Congress of Tuberculosis. 2008 [Google Scholar]
- 11.WHO. Geneva: 2000. Global Tuberculosis Control: WHO Report 2000; p. 275. [Google Scholar]
- 12.Hatami H. Epidemiology and control of tuberculosis. In: Hatami H, Razavi SM, Eftekhar AH, Majlesi F, SayedNozadeh M, Parizadeh S.MJ, editors. Textbook of Public Health. 3rd ed. Vol. 2. Tehran: Arjomand; 2009. p. 1126. [Google Scholar]
- 13.Alavi M, Sefidgaran GH, Karami F. Comparative study on knowledge about tuberculosis in two cities with different tuberculosis epidemiological index in Khuzestan, 2004. Scientific Medical Journal. 2009;8(1):63–69. [In Persian] [Google Scholar]
- 14.Afshari M, Moein A A, Dahmardeh H, Mradqoly MR. First ed. Vol. 9. Mashhad: oroujeandisheh Publications; 2010. Analytical epidemiology of tuberculosis Zahak city. [Google Scholar]
- 15.Kiyani F. Physical problems of Tuberculosis from the point of Tuberculous patients and its relation with some demographic factors in Zahedan and Zabol, 1994. Journal of Zanjan University of Medical Sciences & Health Services. 2001;9(34):20–25. [Google Scholar]
- 16.Karimy M, Montazeri A, Araban M. The effect of an educational program based on health belief model on the empowerment of rural women in prevention of brucellosis. Arak Med Univ J (AMUJ) 2012 Winter;14(4):85–94. [Google Scholar]
- 17.Mahmoodi A, Ramazani A. Study of knowledge, attitude, and practice of presenting women to Zabol health centers with regard to breast self-examination by Using health belief model (in 2009) Modern Care. Scientific Quarterly of Birjand Nursing and Midwifery Faculty. 2011;8:65–72. [In Persian] [Google Scholar]
- 18.Bakhtariaghdam F, Nuorizade R, Sahebi L. The Role of Health Belief Model in Promotion of Beliefs and Behaviors of Breast Cancer Screening in Women Referring to Health Care Centers of Tabriz in 2010. Medical Journal of Tabriz University of Medical Sciences. 2012;33:25–31. [In Persian] [Google Scholar]
- 19.Heydariniya A. Tehran: Zamani Nasser. In the process of health education topics. 2003 [Google Scholar]
- 20.Karimy M, Hasani M, Khorram R, Gafari M, Niknami SH. The effect of education, based on health belief model on breast self examination in the Health volunteer in Zarandieh. TabibeShargh. J Zahedan Univ Med Sci. 2008;10(4):79–87. [Google Scholar]
- 21.Karimy M, Gallali M, Niknami SH, Aminshokravi F, Tavafian SS. The effect of health education based on health belief model on performance of Pap smear test among women referring to health care centers in Zarandieh. J JahromUniv Med Sci. 2012 Spring;10(1):47–53. [Google Scholar]
- 22.Heydari A. The effect of health belief model (HBM) based health education on promoting self care behaviors of patients with smear-positive pulmonary TB in Sistan region in 2011. Thesis submitted for the degree of MSc in health education Shahid Beheshti University of Medical Sciences: School of Public Health. 2011 [Google Scholar]
- 23.Ghafari M. Tarbiat Modares University; 2007. Comparing the efficacy of health belief model and it’s integrated model in AIDS education among male high school students in Tehran. Thesis for Doctorate in Health Education; pp. 187–195. [Google Scholar]
- 24.Asadpour M, Heydarnia AR. Tarbiat Modares University; Promotion and maintenance of preventive behaviors from HIV, HBV and HCV infections in health care worker with using constructs of health belief model in Precede-Proceed model. Thesis for Doctorate in Health Education; pp. 151–232. [Google Scholar]
- 25.Wai CT, Wong ML, Ng S, Cheok A, Tan MH, Chua W, Mak B, et al. Utility of Health Belief Model in predicting compliance of screening in patients with chronic hepatitis B. Aliment Pharmacol Ther. 2005 May;21(10):1255–1262. doi: 10.1111/j.1365-2036.2005.02497.x. [DOI] [PubMed] [Google Scholar]
- 26.Austin LT, Ahmad F, McNally MJ, Stewart DE. Breast and cervical cancer screening in Hispanic women: a literature review using the health belief model. Womens Health Issues. 2002 May-Jun;12(3):122–128. doi: 10.1016/s1049-3867(02)00132-9. [DOI] [PubMed] [Google Scholar]
- 27.Sarani M. The Study for Health Belief Model efficiency in adopting preventive behaviors in the Sistan region tuberculosis patients 2009-2010. Thesis submitted for the degree of MSc in health education. Medical Sciences and Health Services Zahedan: School of Public Health. 2011 [Google Scholar]
- 28.Karimi M, Zarebanlr, Montazrei A, Aminshokravi F. The Impact of Education Based On Health Belif Model In Preventive Behavior of Unwanted Pregnancy. IJOGI. 2012 Oct;15(23):18–27. [Google Scholar]
- 29.Shamsi M, Bayati A. A survey of the prevalence of self-medication and the factors affecting it in pregnant mothers referring to health centers in Arak city, 2009. Jahrom Medical Journal. 2010;7(3):34–42. [Google Scholar]
- 30.Koch J. The role of exercise in the African-American woman with type 2 diabetes mellitus:application of the health belief model. J Am Acad Nurse Pract. 2002;14(3):9–126. doi: 10.1111/j.1745-7599.2002.tb00103.x. [DOI] [PubMed] [Google Scholar]
- 31.Peyman N, Heidarnia A, Ghofranipour F, Kazemnejad A, Khodaee GH, Aminshokravi F. The relationship between perceived self-efficacy and contraceptive behaviors among Iranian women referring to health centers in Mashad in order to decrease unwanted pregnancies. J Reprodlnfertil. 2007 Apr-Jun;8(30):78–90. [Google Scholar]
- 32.Olayemi SO, Oreagba IA, Akinyede A, Adepoju GE. Educational intervention and the health seeking attitude and adherence to theraphy by tuberculosis patients from an urban slum in Lagos Niger Postgrad. Niger postgrad Medy. 2009;16(4):231–235. [PubMed] [Google Scholar]
- 33.Abebe G, Deribew A, Apers L, Woldemichael K, Shiffa J, Tesfaye M, et al. Knowledge, Health Seeking Behavior and Perceived Stigma towards Tuberculosis among Tuberculosis Suspects in a Rural Community in Southwest Ethiopia. PloS ONE. 2010;5(10):133–139. doi: 10.1371/journal.pone.0013339. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Shams SH. Study of educational needs in Tuberculosis patients and their family and self care in Urmia. Journal of Urmi a Nursing And Midwifery Faculty. 2004;2(2):62–55. [Google Scholar]
- 35.Taheri-aziz M. Tarbiatmodares university: School of medical science; 2004. Survey of effectiveness of designed health educational package on tuberculosis patients healthy behaviors at Pasteur institute spring 2004. Thesis submitted for the degree of MSc in health education. [Google Scholar]
- 36.Mathuria BL, Jain NK, Jhamaria JP, Luhadia SK, Madan A, Sharma TN, et al. Knowledge And Attitude of Tuberculous Patients Towards Their Disease And Its Management. Lung India. 1988;6(2):65–70. [Google Scholar]
- 37.Haj-amiri P, Monjamed Z, Tabari F, Bahrani N. Assessment of TB patients, Relation between their knowledge of disease and therapeutic regimers in TB/Control center, Tehran, 1998. The Journal of Faculty of Nursing & Midwifery. 2000;6(12):31–40. [Google Scholar]


