Abstract
Patient: Male, 46
Final Diagnosis: Adenocarcinoma of the ascending colon
Symptoms: Anemia • diplopia • hemiparesis • slurred speech
Medication: —
Clinical Procedure: Multi-detector computed tomography • colonoscopy
Specialty: Neurology
Objective:
Rare co-existance of disease or pathology
Background:
It is rare that occult cancer presents with frequent ischemic stroke as the sole manifestation.
Case Report:
We report the case of a 46-year-old man with frequent stroke in different vascular areas, with diabetes and hypercholesterolemia identified as risk factors. The results of biochemistry, young stroke profiles, trans-cranial and extra-cranial carotid Doppler, and 24-h Holter electrocardiogram were within normal limits. The reports of transthoracic echocardiography (TTE) were unremarkable. Finally, a multi-detector computed tomography (MDCT) demonstrated a thrombus in the posterior-lateral aspect of the left atrium and non-bacterial thrombotic endocarditis (NBTE) was suspected. The results motivated the survey for occult cancer, and adenocarcinoma of the ascending colon was confirmed on colonoscopy pathology.
Conclusions:
We suggest that evaluating the possibility of occult cancer should be emphasized in patients of frequent stroke refractory to therapy, whether risk factors are already identified or not. Furthermore, we assume MDCT can be an alternative way to detect cardiogenic embolic sources in stroke patients.
MeSH Keywords: Colonic Neoplasms; Endocarditis, Non-Infective; Multidetector Computed Tomography; Stroke; Thromboembolism
Background
Central nervous system (CNS) involvements can occur in around 30% of patients with cancer. In these patients, stroke, including ischemia and hemorrhage, is the second leading cause of CNS involvement. In an autopsy study of cancer patients, 7.4% of patients presented significant clinical symptoms of stroke in life, but 14.6% of patients had pathological evidence of cerebrovascular events [1]. The hypercoagulable state, the vessels compression or infiltration, and endothelial damage are responsible for the formation of thrombus in ischemic stroke of cancer patients, whereas non-bacterial thrombotic endocarditis (NBTE), arterial tumor emboli, and septic emboli may cause cerebral embolization [2,3]. However, cerebral ischemic stroke as the first manifestation of occult cancer is very rare (0.4%) [4].
Herein, we report a rare case with frequent attacks of stroke as the initial presentation of occult colon cancer, and we review the possible mechanism of thrombo-embolism in cancer patients. We also discuss ways to detect NBTE.
Case Report
A 46-year-old man who denied any systemic disease had acute bi-ocular diplopia with right internuclear ophthalmoplegia. Stroke involving right medial longitudinal fasciculus was suspected and the report of brain computed tomography (CT) was compatible with infarction of the right pons. A survey for risk factors of stroke showed diabetes and hypercholesterolemia. He was discharged with few sequelae and took aspirin 100 mg per day with oral anti-diabetic medication and a cholesterol-lowering agent.
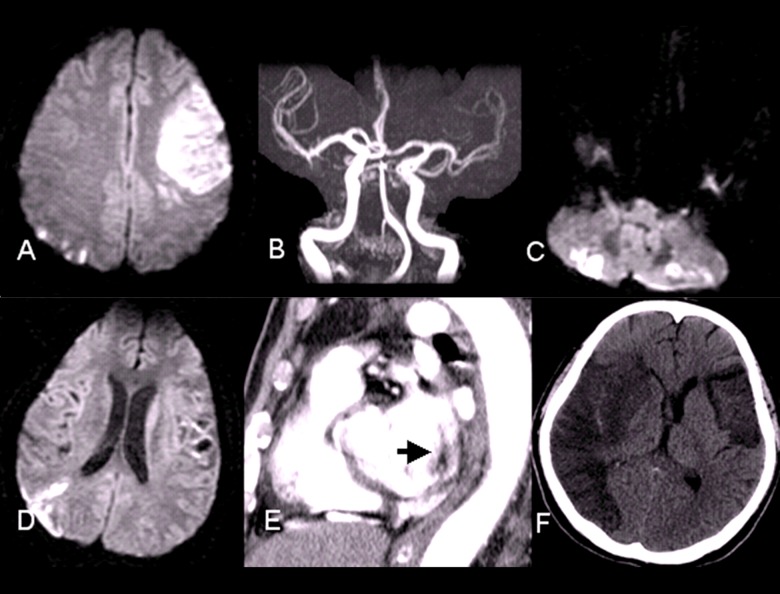
Fourteen days after discharge, he presented another episode of left tonic-gazing, Broca’s aphasia and right hemi-paresis with grade 2/5 power (Medical Research Council scale). Admission to the neurology intensive care unit was arranged initially. The brain CT was unremarkable but brain magnetic resonance imaging (MRI) disclosed acute infarcts in the left cerebellar hemisphere and in the left superior division of the middle cerebral artery (MCA) in addition to watershed infarcts of the right parietal and occipital lobes (Figure 1A). Magnetic resonance angiography (MRA) did not illustrate any focal stenosis (Figure 1B). During his stay in the intensive care unit, bedside electrocardiographic (ECG) monitoring showed sinus rhythm. The complete cell count, biochemistry studies, and laboratory tests for young stroke risk factors, including rheumatic factor, antinuclear antibody, anticardiolipin antibody, lupus anticoagulant, protein C, protein S, factor VIII, fibrinogen, viscosity, anti-thrombin III and homocysteine, were within normal limits. The reports of trans-cranial and extra-cranial Doppler, transthoracic echocardiography (TTE) and 24-h Holter electrocardiogram were unremarkable. During hospitalization, normocytic anemia (hemoglobin: 8.6 g/dl, normal range: 11–13 g/dl) and occult blood in stool were recorded. The esophago-gastroscopy demonstrated superficial gastritis with erosion, so we replaced the aspirin with clopidogrel and piracetam. Four days later, he became drowsy and brain CT showed hemorrhagic transformation of left the superior division of the MCA. Subsequent brain MRI showed multiple punctate infarcts in the right MCA territory, the splenium of the corpus callosum, the left parietal lobe, the pons, and the bilateral cerebellar hemispheres (Figure 1C, 1D).
Figure 1.
(A) MRI of the secondary episode of stroke showed infarction of left frontal and right watershed area. (B) MRA of the secondary episode of stroke did not reveal significant focal stenosis. (C, D) MRI of the third episode of stroke disclosed punctuate stroke in several territories of the cerebral artery. (E) Multidetector computed tomography showed one filling defect in the posterior-lateral aspect of left atrium (arrow). (F) CT of the fourth episode of stroke showed infarct of complete right MCA territory with brain edema.
Because cardiogenic embolus was highly suspected, we arranged another trans-thoracic cardiac echogram, but it was still unremarkable. Due to his family’s refusal, further transesophageal echocardiography (TEE) was not performed. Instead, multi-detector computed tomography (MDCT), as an alternative examination, showed a thrombus in the posterior-lateral aspect of the left atrium (Figure 1E). Three sets of serial blood cultures were negative. In addition, elevation of D-dimer (3217 ug/L, normal range: <324 ug/L) with normal prothrombin and activated pre-prothrombin time were recorded, as well as normal results of fibrinogen (297 mg/dl, normal range: 170–410 mg/dl) and fibrin-split product. Therefore, NBTE was suspected. However, anti-coagulation therapy was postponed due to active gastro-intestinal tract bleeding.
The results motivated the search for occult cancer. The level of carcinoembryonic antigen (CEA) was elevated to 100 ng/dl (normal range: <5 ng/dl) and adenocarcinoma of the ascending colon 70 cm from the anus was confirmed on colonoscopy pathology. CT abdomen demonstrated a malignant tumor in the ascending colon with multiple metastatic lymphadenopathy in the mesenteric space and aortocaval space. A cerebrospinal fluid (CSF) study excluded the possibility of leptomeningeal metastasis.
Fifty-four days after the initial neurological presentation, he had another episode of consciousness disturbance with left hemiparesis attack and brain CT showed the infarction of complete right MCA territory with brain edema (Figure 1F). His family chose conservative therapy instead of surgical intervention. A week later, he died due to intractable intracranial hypertension and septic shock.
Discussion
The relationship between thrombo-embolism and cancer was first established by Trousseau in 1865. The incidence of thrombo-embolic events in patients with cancer was 15% in clinical findings and up to 50% in post-mortem studies [5,6].
Many causes contribute to thrombo-embolism in cancer patients. While interacting with tumor cells, monocyte and macrophage lineages release tumor necrosis factor, interleukin-1, and interleukin-6, which can damage endothelium and convert the vascular lining into a thrombogenic surface. The interaction between malignant cells and macrophages can also activate platelets, factor XII, and factor X. In addition, the tumor cells themselves also have substances, including cysteine protease and tissue factor, and these materials can activate factor X (to factor Xa) and factor VII (to factor VIIa). Activation of these factors induces further thrombogenic cascades [3]. Immobility and the infectious condition of cancer patients, as well as aggressive therapy including chemotherapy, radiotherapy, and central line placement can all aggravate the thrombo-embolic events [2,3].
Of these cancer associated thrombo-embolisms, venous thrombo-embolic events are most common. Other manifestations were also reported, including arterial thrombosis, disseminated intravascular coagulation (DIC), non-bacterial thrombotic endocarditis (NBTE), migratory superficial thrombophlebitis, and thrombotic microangiopathy [6]. One previous study revealed that cerebro-vascular event, including ischemia and hemorrhage, is the second leading cause of CNS involvements in patients with cancer, just after metastasis [1]. Nevertheless, cerebral ischemic stroke is very rare as the first manifestation of concealed cancer (0.4%) [4].
We report a rare case of a man with several episodes of stroke in different vascular territories as the initial presentation of occult colon cancer. His only identified risk factors for stroke were diabetes and hypercholesteremia. The cardio-embolic source for stroke was suspected according to the classification of TOAST (Trial of Org 10172 in Acute Stroke Treatment) [7]. The finding of trans-thoracic echocardiogram was unremarkable and transesophageal echocardiography (TEE) was inaccessible. MDCT was an alternative examination and showed a thrombus in the posterior-lateral aspect of the left atrium. Finally, the diagnosis of frequent strokes secondary to NBTE was made. Based on the findings, we did further malignancy evaluation and colon adenocarcinoma was confirmed.
NBTE is the most frequent cause of cerebral ischemia in cancer patients, regardless of whether stroke is the first manifestation of cancer [1,4]. The diagnosis of NBTE should depend on the distribution of occluded vessels, identification of thrombus, and exclusion of other possible causes, such as infective endocarditis [1,6].
Transesophageal echocardiography (TEE) is the criterion standard for evaluating the left atrial appendage (LAA) and is routinely used for the assessment of atrial thrombus pre-cardio-version in patients with atrial fibrillation and in the workup of embolic stroke [8].
Conventional trans-thoracic or trans-esophageal cardio-echograms are technician-dependent and limited in different ways [9,10]. As higher spatial and temporal resolution imaging rapidly develops, MDCT can provide better visualization of heart, great vessels, and lungs [9–11], and may be an alternative way to detect the origin of cardioembolic stroke in clinical applications.
Compared with reference-standard methods for acute stroke study such as TEE, MDCT appears to be more feasible and is better tolerated. MDCT requires shorter duration, which is critical in patients with acute stroke, who may be unstable and agitated. MDCT has been reported to have good accuracy for the identification of extra- and intracranial atheromatous disease. MDCT may also yield information regarding plaque composition, including calcification and plaque attenuation characteristics, both of which may be of interest in the assessment of vulnerable plaques. Furthermore, MDCT has been demonstrated to be effective and reproducible in the detection and quantification of aortic arch atheroma [12].
The spontaneous echo contrast (SEC) as well as left atrial thrombus under transesophageal echocardiography (TEE) confers an increased risk of embolic stroke. MDCT can qualitatively and quantitatively identify and distinguish severe left atrial appendage SEC/thrombus from lesser grades of SEC [8].
Treatment consists of NBTE, including systemic anticoagulation and therapy directed at treating the underlying associated condition. Rarely, surgery with valve debridement or excision is performed.
Systemic anti-coagulation without contraindication may ameliorate symptoms and prevent further thromboembolic episodes [6]. However, the risk of anticoagulation is hemorrhagic conversion of embolic events. Anti-coagulation therapy was postponed in our patient due to active gastro-intestinal tract bleeding. Therapeutic-dose subcutaneous low molecular weight (LMW) heparin or intravenous unfractionated heparin should be used. Although no formal comparison between heparin and warfarin has been reported in patients with NBTE, studies suggest that warfarin is less effective than heparin in reducing the rate of recurrent embolization [6]. Treatment of the underlying condition (e.g., malignancy or autoimmune disease) should be attempted under appropriate conditions. Nevertheless, this strategy is often ineffective due to the advanced and metastatic deterioration in malignancy.
Surgical intervention for NBTE-associated vegetations has been reported and may be considered in select cases where the risk benefit is favorable [13]. Preservation of the valve may be possible in some NBTE cases, in contrast to infective endocarditis, where complete removal of infected tissue is important.
Conclusions
We present a rare case of a patient who had frequent ischemic stroke as the first manifestation of occult cancer. The possibility of malignancy should be emphasized in patients with frequent stroke in different vascular territories refractory to therapy, whether or not risk factors are already identified. MDCT can be an alternative way to detect cardiogenic embolic sources in stroke patients.
Reference:
- 1.Graus F, Rogers LR, Posner JB. Cerebrovascular complications in patients with cancer. Medicine. 1985;64:16–35. doi: 10.1097/00005792-198501000-00002. [DOI] [PubMed] [Google Scholar]
- 2.Rogers LR. Cerebrovascular complications in patients with cancer. Semin Neurol. 2004;24:453–60. doi: 10.1055/s-2004-861539. [DOI] [PubMed] [Google Scholar]
- 3.Bick RL. Cancer-associated thrombosis. N Engl J Med. 2003;349:109–11. doi: 10.1056/NEJMp030086. [DOI] [PubMed] [Google Scholar]
- 4.Taccone FS, Jeangette SM, Blecic SA. First-ever stroke as initial presentation of systemic cancer. J Stroke Cerebrovasc Dis. 2008;17:169–74. doi: 10.1016/j.jstrokecerebrovasdis.2008.01.007. [DOI] [PubMed] [Google Scholar]
- 5.Frenkel EP, Bick R. Issues of thrombosis and hemorrhagic events in patients with cancer. In Vivo. 1998;12:625–28. [PubMed] [Google Scholar]
- 6.el-Shami K, Griffiths E, Streiff M. Nonbacterial thrombotic endocarditis in cancer patients: pathogenesis, diagnosis, and treatment. Oncologist. 2007;12:518–23. doi: 10.1634/theoncologist.12-5-518. [DOI] [PubMed] [Google Scholar]
- 7.Adams HP, Jr, Bendixen BH, Kappelle LJ, et al. Classification of subtype of acute ischemic stroke. Definitions for use in a multicenter clinical trial. TOAST. Trial of Org 10172 in Acute Stroke Treatment. Stroke. 1993;24:35–41. doi: 10.1161/01.str.24.1.35. [DOI] [PubMed] [Google Scholar]
- 8.Kim YY, Klein AL, Halliburton SS, et al. Left atrial appendage filling defects identified by multidetector computed tomography in patients undergoing radiofrequency pulmonary vein antral isolation: a comparison with transesophageal echocardiography. Am Heart J. 2007;154:1199–205. doi: 10.1016/j.ahj.2007.08.004. [DOI] [PubMed] [Google Scholar]
- 9.Hoey ET, Mansoubi H, Gopalan D, et al. MDCT features of cardiothoracic sources of stroke. Clin Radiol. 2009;64:550–59. doi: 10.1016/j.crad.2008.11.005. [DOI] [PubMed] [Google Scholar]
- 10.Chen JJ, Manning MA, Frazier AA, et al. CT angiography of the cardiac valves: normal, diseased, and postoperative appearances. Radiographics. 2009;29:1393–412. doi: 10.1148/rg.295095002. [DOI] [PubMed] [Google Scholar]
- 11.Chen JJ, Jeudy J, Thorn EM, White CS. Computed tomography assessment of valvular morphology, function, and disease. J Cardiovasc Comput Tomogr. 2009;3:S47–56. doi: 10.1016/j.jcct.2008.10.017. [DOI] [PubMed] [Google Scholar]
- 12.Boussel L, Cakmak S, Wintermark M, et al. Ischemic stroke: etiologic work-up with multidetector CT of heart and extra- and intracranial arteries. Radiology. 2011;258:206–12. doi: 10.1148/radiol.10100804. [DOI] [PubMed] [Google Scholar]
- 13.Rabinstein AA, Giovanelli C, Romano JG, et al. Surgical treatment of non-bacterial thrombotic endocarditis presenting with stroke. J Neurol. 2005;252:352–55. doi: 10.1007/s00415-005-0660-z. [DOI] [PubMed] [Google Scholar]