Abstract
The authors examined racial/ethnic differences in pathways from maltreatment exposure to specialty mental health service use for youth in contact with the Child Welfare system. Participants included 1600 non-Hispanic White, African American, and Latino youth (age 4–14) who were the subjects of investigations for alleged maltreatment and participated in the National Survey of Child and Adolescent Well-Being. Maltreatment exposure, internalizing, and externalizing problems were assessed at baseline and subsequent specialty mental health service use was assessed one year later. Maltreatment exposure predicted both internalizing and externalizing problems across all racial/ethnic groups, but non-Hispanic White youth were the only group for whom maltreatment exposure was linked with subsequent service use via both internalizing and externalizing problem severity. Only externalizing problems predicted subsequent service use for African American youth and this association was significantly stronger relative to non-Hispanic White youth. Neither problem type predicted service use for Latinos. It is likely that individual, family, and system-level factors converge to link African American youth with externalizing problems to services, but not as responsive in linking African American and Latino youth with internalizing problems to services.
Keywords: child maltreatment, mental health services, children in child welfare, cultural/ethnic issues, ethnic minority populations
As many as 4 of 5 American children with mental health (MH) need do not receive services, and this unmet need is even higher for racial/ethnic minority youth compared to non-Hispanic White youth (Kataoka, Zhang, & Wells, 2002). Racial/ethnic disparities in care remain after factors such as problem severity, impairment, insurance coverage, and socioeconomic status (SES) are accounted for (Garland et al., 2005). Children in Child Welfare (CW) are of particular concern, as they are disproportionately impacted by a constellation of risk factors (e.g., maltreatment, poverty, etc.). Indeed, up to 80% of youth involved in the CW system have emotional or behavioral disorders, developmental delays, or other indications of needing mental health intervention (Farmer et al., 2001; Landsverk, Garland, & Leslie., 2002; Taussig, 2002). Although contact with CW facilitates access to care, particularly in the months following a maltreatment investigation (Leslie et al., 2005), racial/ethnic disparities in mental health services (MHS) persist. Overall, African American and Latino youth are half as likely to receive MHS compared to their non-Hispanic White counterparts, even after accounting for SES, maltreatment exposure, and indicators of MH need (Burns et al., 2004; Leslie et al., 2005).
While prior research has found these overall racial/ethnic disparities in MHS use for youth in CW, it is clear that factors beyond race/ethnicity impact service use. For example, child age and gender are key sociodemographic factors that predict service use, with older children and males being more likely to use MHS (Garland, Landsverk, Hough, & Ellis-MacLeod., 1996; Leslie et al., 2000). Perhaps more central to youth in CW, maltreatment exposure and the severity of emotional/behavioral problems are predictive of MHS use (Garland et al., 1996; Leslie et al, 2000). Interestingly, maltreatment exposure is predictive of MHS use only to the extent that it is also associated with emotional/behavioral problems (Leslie et al., 2000). Moreover, the extent to which specific child emotional/behavior problems are predictive of MHS use varies by race/ethnicity. That is, racial/ethnic disparities in MHS use may be attenuated or amplified depending on the types of child behavior problems under investigation (Gudiño, Lau, Yeh, McCabe, & Hough, 2009; Gudiño, Martinez, & Lau, 2012). Although there is substantial evidence of racial/ethnic disparities in MH care for youth in contact with CW when overall group differences are the focus and other predictors are accounted for statistically, fully understanding pathways to MHS requires an examination of complex interrelationships among various predictors in addition to an examination of potential racial/ethnic group differences.
Maltreatment Exposure and MHS Use
The type of maltreatment exposure experienced by youth in CW is one important predictor of MHS use. For example, children exposed to physical or sexual abuse were more likely to receive MHS than those that were not exposed to physical or sexual abuse, while children exposed to neglect were less likely to receive MHS compared to other forms of maltreatment (Garland et al., 1996). However, another study found that maltreatment type (physical, sexual, neglect, emotional) was not significantly related to use of outpatient mental health services (Leslie, et al., 2000). A limitation in operationalizing maltreatment by a single indicator is that it overlooks the high degree of overlap in different types of maltreatment experiences. For example, the majority of children exposed to maltreatment have been abused in multiple ways (Edwards, Holden, Felitti, & Anda, 2003), with less than 10% of child abuse cases reporting only single types of maltreatment (McGee, Wolfe, Yuen, Wilson, & Carnochan, 1995; Ney Fung, & Wickett, 1994). How cumulative exposure to multiple forms of maltreatment is related to MHS use patterns is less clear from previous research.
Regardless of how maltreatment exposure is measured, racial/ethnic disparities in MHS use remain after accounting for type of maltreatment, with numerous studies indicating that racial/ethnic minority youth in CW are less likely to receive services compared to non-Hispanic White youth (Burns et al., 2004; Garland & Besinger, 1997; Leslie et al, 2000). Racial/ethnic differences in receipt of care for youth exposed to maltreatment may be due to several contributing factors, such as cultural differences in help-seeking patterns, accessibility of service providers, and systematic bias in referral patterns within CW (Garland, Landsverk, & Lau, 2003). One study explored systematic bias of referral patterns by race/ethnicity, and found that caseworkers were more likely to recommend, and courts were more likely to order, psychotherapy for non-Hispanic White youth compared to Latino and African American youth, even after controlling for type of maltreatment exposure (Garland & Besinger, 1997). Upon further review, there was evidence that the majority of those referrals did, in fact, use services, and there were no racial/ethnic differences in rates of follow through with services (Garland et al., 2003).
Maltreatment Exposure and Emotional/Behavioral Problems
Research suggests a strong association between early maltreatment experiences and later development of emotional/behavioral problems, from internalizing to externalizing behavior problems. A 12-year prospective study found that early maltreatment exposure in children was significantly associated with later development of aggression, anxiety/depression, dissociation, delinquent behaviors, posttraumatic stress disorder (PTSD), social problems, thought problems, and social withdrawal, that were twice as high, on average, as those of their non-maltreated counterparts (Landsford et al., 2002). Notably, the effects of maltreatment exposure on all of these behavior problems could not be explained away by other ecological and child risk factors. Among children and adolescents, there is also a high degree of co-occurrence between internalizing and externalizing problems (Angold, Costello & Erkanli, 1999; Cosgrove et al., 2011). Thus, the MH needs of youth in CW may be characterized by high rates of both internalizing and externalizing problems, both of which are strongly associated with maltreatment exposure.
Given limited resources for delivering specialty MH care to youth in CW, maltreatment exposure itself is unlikely to ensure receipt of MHS. In a study of youth in foster care, Leslie and colleagues (2000) found that maltreatment history was unrelated to outpatient service use. However, children with emotional/behavioral problems were significantly more likely to use outpatient services compared to children without such problems. This makes sense given that not all children exposed to maltreatment will evidence MH problems warranting clinical intervention. Therefore, it stands to reason that maltreatment exposure is indirectly linked to MH care to the extent that it is related to presenting emotional/behavioral problems.
Racial/Ethnic Differences in the Association between MH Need and MHS Use
While the research reviewed above suggests that MH need drives MHS use, recent research suggests that the type of MH problem present may be an important determinant of who receives services. Specifically, when examining internalizing vs. externalizing problems overall, racial/ethnic disparities in MHS use appear much less pronounced among youth with externalizing problems. In a diverse sample of youth in contact with public sectors of care in San Diego county, African American (46%) and Latino (48%) youth with externalizing problems were found to have service use rates similar to non-Hispanic White (55%) youth (Gudiño, Lau, Yeh, McCabe, & Hough, 2009). Among youth surveyed from a national sample of youth in contact with CW, the National Survey of Child and Adolescent Well-Being (NSCAW I), African American youth were far more likely to receive care when they had elevated externalizing problems (45%) than when they did not (6%) relative to non-Hispanic White youth (48% vs. 27%; Gudiño, Martinez, & Lau, 2012).
In contrast, racial/ethnic disparities appear to be more pronounced among youth with internalizing problems, where non-Hispanic White youth had higher rates of service use (72%) compared to Latino (41%) and African American youth (56%; Gudiño et al., 2009). Findings from NSCAW I revealed that non-Hispanic White youth were the only group to have higher rates of service use when internalizing need was present versus absent (48% vs. 25%) when compared to African American (15% vs. 23%) and Latino (27% vs. 29%) youth (Gudiño et al., 2012). Accordingly, it is important to examine problem-specific disparities when considering issues of parity in youth MH care.
The Current Study
While previous studies have examined associations between maltreatment exposure and MH need on MHS use, these studies have focused on examining a single factor or simply controlling statistically for the presence of other predictors. However, pathways to MHS use for children in CW are likely complex and multiply determined. In the current study, we utilize structural equation modeling (SEM) to simultaneously explore interrelationships among variables and pathways to MHS use. We examined whether race/ethnicity moderates patterns of specialty MHS use as a function of maltreatment exposure and child internalizing/externalizing problems in a nationally representative sample of youth in contact with the CW system. Specifically, we tested a model whereby maltreatment exposure directly predicts the development of both internalizing and externalizing problems in youth and indirectly predicts MHS use, via internalizing and externalizing problem severity. For all racial/ethnic groups, we hypothesized that maltreatment exposure would be a strong predictor of both internalizing and externalizing problems. We also expected that there would be a strong correlation between internalizing and externalizing problem severity in this high-risk population.
The central aim of the current study, however, was to examine whether pathways from maltreatment exposure to MHS use via internalizing/externalizing problems are moderated by race/ethnicity. Our model considers the potential direct association between maltreatment exposure and MHS use. However, as prior research suggests that maltreatment exposure is likely indirectly linked to MHS use to the extent that it is related to child emotional/behavior problems, we hypothesized that 1) maltreatment exposure would be associated with increased specialty MHS use via both internalizing and externalizing child behavior problems (indirect effects). Yet, given the foregoing evidence suggesting racial/ethnic disparities in MHS use as a function of problem type for youth in contact with CW, we further hypothesized that 2) these indirect pathways to care would differ for racial/ethnic minority youth. Specifically, we predicted a stronger association (amplification) between externalizing behavior problems and MHS use for African American and Latino youth compared to non-Hispanic White youth, and a weaker association (attenuation) between internalizing problems and MHS use for African Americans and Latinos compared to non-Hispanic White youth.
Method
Participants
This study utilized data from the National Survey of Child and Adolescent Well-Being (NSCAW I), a nationally representative sample of youth in contact with the CW system. The NSCAW I sample includes 5,501 children from birth to age 14 years at the time of the initial study assessment. Participants in the current study include a subsample of families where the child who was the focus of the CW investigation was four years of age or older at the time of the initial assessment (n=3177), where the caregiver identified the child as being non-Hispanic White, African American, or Latino (n=2931), where the child remained in an in-home placement at baseline and at 12 months following the initial investigation (n=2229), and where the caregiver completed a 12-month follow-up interview reporting on specialty MHS use in the past year (n=1600). We conducted attrition analyses to determine whether the follow-up sample differed from the families who did not complete the follow-up interview reporting on specialty MHS use (n=629). There were no significant differences between the groups in terms of race/ethnicity, parental education, age, gender, maltreatment exposure, and internalizing and externalizing MH need. The final sample for analysis included 843 non-Hispanic White youth (52.7%), 449 African American youth (28.1%), and 308 Latino youth (19.1%).
Procedures
Families who had contact with the CW system in 97 counties nationwide during a 15-month period starting October 1999 were randomly selected to participate in NSCAW. Caregivers completed baseline face-to-face interviews (Wave 1) where demographic variables, child maltreatment exposure, and child behavior problems were assessed within 6 months of the close of the CW investigation. Specialty MHS use was assessed during a subsequent interview with caregivers (Wave 2) about 12 months following the close of the initial CW investigation (M = 12.18 months, SD = 1.51).
Measures
Family Demographic variables included child age (continuous), gender (0=male, 1=female), race/ethnicity (non-Hispanic White, African American, Latino), and parental education (0=no HS diploma, 1=HS diploma or above).
Youth Maltreatment Exposure In the past year was assessed using the Parent-Child Conflict Tactics Scale (CTSPC; Straus, Hamby, Finkelhor, Moore, & Runyon, 1998). The CTSPC measures the extent to which a parent reports having carried out specific acts of physical assault, psychological aggression, and neglect. The CTSPC scales were developed with a national sample matching general population representation and the CTSPC has been found to have adequate reliability, with kappa estimates above 0.75 (Straus et al., 1998). Confirmation of the factor analytic structure has been demonstrated in Latino samples (Reichenheim & Moraes, 2006) and comparable internal consistency has been reported for African American and European American families (Lau, Litrownik, Newton, Black & Everson, 2006). In the overall NSCAW sample, the internal consistency ranged from good to marginal (Total Scale α = .79, Neglect α = .39, Psychological Aggression α = .66 Minor Physical Assault α = .57, Severe Physical Assault α = .11, Very Severe Physical Assault α = .22; NSCAW Research Group, 2004). Lower internal consistency in some cases may be the result of the inclusion of items with rare occurrences (Straus, Hamby, Finkelhor, Moore, & Runyon, 1998).
We constructed a maltreatment exposure factor using the core scales of Psychological Aggression and Physical Assault, and the supplementary scale on Neglect. The Physical Assault scale is further categorized into Minor Assault, Severe Assault, and Very Severe Assault. Each scale includes past year prevalence, which is a 0–1 dichotomy (1 = one or more of the acts in the scale occurred). Chronicity, which is the number of times the acts occurred in the past year, is also measured with a continuous total score provided for all items. We explored including sexual abuse as an additional indicator of maltreatment. However, possibly due to the lower base rate of sexual abuse in the current sample (under 10%), the inclusion of sexual abuse resulted in a poorer measurement model. Model results suggested that sexual abuse reflects a dimension of maltreatment that is distinct from the other dimensions measured in the current study and sexual abuse was thus not an adequate indicator of the overall maltreatment latent variable.
In the current study we focus on maltreatment (physical assault, psychological aggression, and neglect) in the past year, as endorsed by the caregiver at the baseline interview. We analyzed the distributions of our indicator variables and their factor loadings in a measurement model. For Physical Assault, the chronicity scale was nonnormally distributed (zero-inflated), thus we opted to use a 3-level ordinal variable for Physical Assault (1 = None, 2 = Minor Assault, 3 = Severe Assault/Very Severe Assault) for past year prevalence. For the Psychological Aggression and Neglect indicators, we examined the past year chronicity total scores. Our results suggested that these variables had a skewed but fairly normal distribution, thus we elected to use the continuous scores in our model. Thus, in constructing our maltreatment exposure factor, we used a 3-level ordinal variable using subscales of Physical Assault (1= None, 2 = Minor Assault, 3 = Severe Assault/Very Severe Assault) and past year chronicity continuous scores for Psychological Aggression and Neglect.
Youth emotional/behavior problems Were assessed from the caregiver-reported Child Behavior Checklist (CBCL), a standardized measure of children’s emotional/behavioral problems. The child’s primary caregiver completed 113 items on a 3-point Likert scale (0 = not true, 1 = somewhat or sometimes true, and 2 = very true or often true). The CBCL yields eight syndrome scales: Withdrawn, Somatic Complaints, Anxious/Depressed, Social Problems, Thought Problems, Attention Problems, Delinquent Behavior, and Aggressive Behavior. We used the broadband Externalizing score, comprised of the Delinquent and Aggressive Behavior syndromes, and the broadband Internalizing score, comprised of the Withdrawn, Somatic Complaints, and Anxious /Depressed syndromes. We utilized the Internalizing and Externalizing T-scores, which are normed by gender and age from a nationally representative sample. The CBCL has well-established reliability and validity (Achenbach, 1991), as well as support for its use across cultures and racial/ethnic groups (Achenbach & Rescorla, 2001; Ivanova et al., 2007). The broadband internalizing and externalizing scales demonstrate high internal consistency (alphas ranging from .89 to .94), with strong concurrent validity for clinically-diagnosed disorders in Latino youth (Rubio-Stipec, Bird, Canino, & Gould, 1990), and support for comparable factor structures in African American and non-Hispanic White samples (Latkovich, 1996). The convergent and divergent validity of the CBCL scales has been established in multi-ethnic samples of American children (Nakamura, Ebesutani, Bernstein, & Chorpita, 2009). In the overall NSCAW sample, the internal consistency reliability of the CBCL was good (externalizing α = 0.91, internalizing α = 0.90; NSCAW Research Group, 2004). In the current sample, the internal consistency reliability of the CBCL internalizing scale by race/ethnicity (African American α = .96, Latino α = .98, non-Hispanic White α = .91) as well as the externalizing scale by race/ethnicity (African American α = .96, Latino α = .98, NHW α = .93) was also good.
Youth Specialty MHS Use Was assessed using the Child and Adolescent Services Assessment (CASA; Ascher, Farmer, Burns, & Angold, 1996). We examined past-year use of specialty outpatient MHS, including visits to MH centers, community health centers, day hospital/partial hospitalization programs, or a private practitioner (psychiatrists, psychologists, social workers, and psychiatric nurses). We were unable to calculate the internal consistency for the CASA in our sample due to unavailable item level data in the NSCAW I data set. Nevertheless, the CASA has demonstrated acceptable internal consistency for probing the number of service settings used (ICC = .76), good test-retest reliability for probing the use of outpatient services (Κ= .81), and good validity for probing the use of outpatient services (Ascher et al., 1996).
Data Analytic Procedures
Study hypotheses were examined using multi-group structural equation modeling (SEM) in Mplus, version 5.0 (Muthén & Muthén, 2007). All analyses accounted for the complex survey design (clustering and stratification) and utilized sampling weights to yield estimates that were nationally representative. Good model fit is indicated by values greater than .90 for the Comparative Fit Index (CFI), and less than .06 for the Root Mean Squared Error Approximation (RMSEA; McDonald & Ho, 2002). Full information maximum likelihood estimation was used to estimate the models, with the missing data option used to make full use of all available data. Because our study sample was restricted to those who provided follow-up data on specialty MHS use and complete CBCL data were available, missing data estimation was only relevant for the CTSPC scales. Rates of missing data were low, with minimum covariance coverage of 98%. Given the inclusion of ordinal and binary variables, we used a robust weighted least squares (WLSM) estimation procedure. To investigate whether structural paths of interest varied by race/ethnicity, the DIFFTEST command for the WLSM estimation procedure was used to test for differences in chi-square indicators of model fit between unconstrained and constrained models. Indirect effects were analyzed using the MODEL INDIRECT command, which provides results on the effect of Maltreatment Exposure on Specialty MHS use via Internalizing and Externalizing behavior problems.
Results
Table 1 presents sample descriptives for all study variables by racial/ethnic group. African American youth were less likely to receive specialty MHS relative to non-Hispanic White youth [design-based F(1.94, 160.85) = 4.42, p = .01]. Additionally, caregivers of African American youth were more likely to endorse using severe/very severe physical assaultive behavior than non-Hispanic White caregivers [design-based F(3.26, 270.76) = 3.75, p = 0.01]. Other study variables did not differ by race/ethnicity. Table 2 shows bivariate correlations between study variables.
Table 1.
Sample descriptives by race/ethnicity
| Non-Hispanic White n=843 (52.7%) |
African American n=449 (28.1%) |
Latino n=308 (19.3%) |
Total Sample N=1600 |
|||||
|---|---|---|---|---|---|---|---|---|
| N (%) | M (SE) | N (%) | M (SE) | N (%) | M (SE) | N (%) | M (SE) | |
| Youth Gender | ||||||||
| Female | 433(46.9) | 231(50.7) | 172(60.1) | 836(50.9) | ||||
| Youth Age | 8.8(0.15) | 9.1(0.28) | 8.6(0.26) | 8.8(0.11) | ||||
| Parent Education | ||||||||
| No HS diploma | 208(27.7) | 137(30.9) | 125(30.7) | 470(29.2) | ||||
| HS diploma and above | 635(72.3) | 312(69.1) | 183(69.3) | 1130(70.8) | ||||
| Maltreatment Exposure | ||||||||
| Physical Assault | ||||||||
| None | 246(28.1) | 125(22.1) | 91(26.2) | 462(26.0) | ||||
| Minor Physical Assault | 520(65.0) | 232(55.9) | 163(58.5) | 915(61.1) | ||||
| Severe/Very Severe Physical Assault | 70(7.0) a | 87(22.0) a | 51(15.3) | 208(12.9) | ||||
| Psychological Aggression | 22.0(1.50) | 21.2(1.56) | 15.8(2.20) | 20.5(1.08) | ||||
| Neglect | 3.1(0.42) | 4.7(0.71) | 3.1(0.78) | 3.5(0.34) | ||||
| Behavior Problems | ||||||||
| Internalizing behaviors | 55.1(0.70) | 53.2(0.98) | 53.2(1.26) | 54.2(0.60) | ||||
| Externalizing behaviors | 58.5(0.94) | 58.3(1.04) | 55.6(1.49) | 57.8(0.73) | ||||
|
Specialty Mental Health Service Use | ||||||||
| No | 607(78.2) | 384(89.1) | 256(87.7) | 1247(83.2) | ||||
| Yes | 236(21.8)b | 65(10.9)b | 52(12.3) | 353(16.8) | ||||
Note. Unweighted N reported. Weighted % reported in parentheses. Cells that share the same superscript are significantly different from one another (p=.01). HS=High School.
Table 2.
Correlation matrix of study variables
| Variable | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 |
|---|---|---|---|---|---|---|---|---|
| 1. Age | - | |||||||
| 2. Gender | .06* | - | ||||||
| 3. Education | .07* | −.04 | - | |||||
| 4. Physical Assault | −.17* | .08* | .04 | - | ||||
| 5. Psychological Aggression | .02 | −.04 | .09* | .45* | - | |||
| 6. Neglect | .17* | −.02 | .05* | .18* | .31* | - | ||
| 7. Internalizing behaviors | .15* | −.07* | −.02 | .15* | .25* | .19* | - | |
| 8. Externalizing behaviors | .10* | .01 | −.11* | .34* | .42* | .18* | .64* | - |
| 9. Specialty Mental Health Service Use | .27* | −.10* | .04 | .08* | .11* | .13* | .47* | .44* |
Note.
p<.05
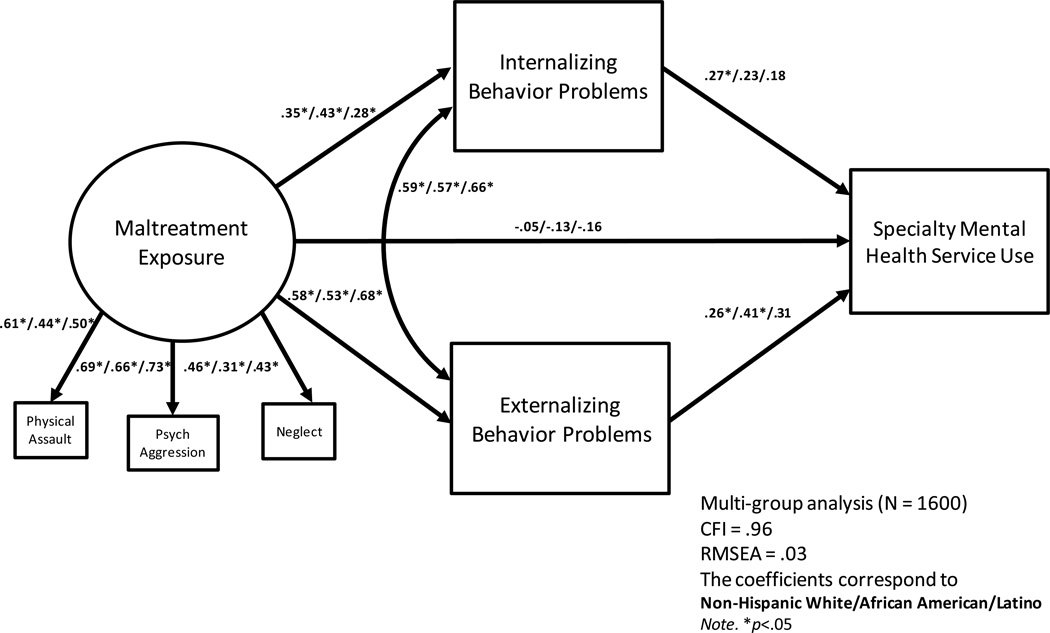
We examined our study hypotheses by fitting the model depicted in Figure 1 across racial/ethnic groups using multi-group SEM. The fit indices for this model suggested an overall good fit to the data (χ2 = 340.84, df = 25, p = .09; CFI = .96; RMSEA = .03). See Table 3 for unstandardized path estimates by race/ethnicity, and Figure 1 for all standardized path estimates for the model.
Figure 1.
Multi-group structural equation model path estimates for maltreatment exposure, child behavior problems, and specialty mental health service use by race/ethnicity.
Table 3.
Path estimates by race/ethnicity
| Non-Hispanic White | African American | Latino | ||||
|---|---|---|---|---|---|---|
| β | 95% CI | β | 95% CI | β | 95% CI | |
| Direct Effects | ||||||
| Maltreatment Internalizing |
.26 | .15 – .38 | .39 | .20 – .58 | .22 | .09 – .35 |
| Maltreatment Externalizing |
.43 | .30 – .57 | .48 | .26 – .69 | .44 | .27 – .61 |
| Maltreatment Mental Health Service Use |
−.00 | −.02 – .01 | −.01 | −.04 – .04 | −.01 | −.05 – .03 |
| Internalizing Mental Health Service Use |
.03 | .01 – .04 | .02 | .00 – .05 | .02 | −.01 – .05 |
| Externalizing Mental Health Service Use |
.02 | .01 – .04 | .04 | .02 – .06 | .03 | −.01 – .08 |
| Indirect Effects | ||||||
| Maltreatment Internalizing Mental Health Service Use |
.01 | .00 – .01 | .01 | .00 – .02 | .00 | .00 – .01 |
| Maltreatment Externalizing Mental Health Service Use |
.01 | .00 – .02 | .02 | .00 – .03 | .01 | −.01 – .04 |
Note. Unstandardized β estimates reported. See Figure 1 for standardized β estimates.
Maltreatment Exposure and Specialty MHS Use
There was no direct effect of maltreatment exposure on specialty MHS use for all racial/ethnic groups.
Maltreatment Exposure and Internalizing/Externalizing Problems
For all racial/ethnic groups, there was a significant effect of maltreatment exposure on internalizing problems. Similarly, for all racial/ethnic groups, there was a significant effect of maltreatment exposure on externalizing problems.
Racial/Ethnic Differences in Association between Internalizing/Externalizing Problems and Specialty MHS Use
For non-Hispanic White youth, both internalizing and externalizing problems significantly predicted specialty MHS use at Wave 2. Conversely, only externalizing problems predicted specialty MHS use for African American youth, whereas neither internalizing nor externalizing problems significantly predicted service use among Latinos. We formally examined moderation by race/ethnicity by comparing a constrained and unconstrained model. The constrained model included pairwise racial/ethnic group constraints on the externalizing and internalizing to specialty MHS use paths. Because our hypotheses were specific to contrasts between non-Hispanic White compared to the two racial/ethnic minority groups, we examined the relevant pairwise contrasts for the internalizing and externalizing to specialty MHS use paths. Constraining the externalizing to service use path to be equal for non-Hispanic White and African American youth produced a significantly poorer fit compared to the unconstrained model (χ2 = 7.91, df = 1, p < .01), suggesting that this path differed significantly for non-Hispanic White and African American youth. The pairwise contrast for this path was not significant for non-Hispanic White and Latino youth. Constraining the internalizing to service use path to be equal for non-Hispanic White and Latino youth produced a significantly poorer fit compared to the unconstrained model (χ2 = 6.88, df = 1, p < .01) suggesting that this path differed significantly for non-Hispanic White and Latino youth. Similarly, constraining the internalizing to service use path across non-Hispanic White and African American youth resulted in a significantly poorer fit compared to the unconstrained model (χ2 = 4.40, df = 1, p < .05), suggesting that this path differed significantly for non-Hispanic White and African American youth.
Indirect Effect of Maltreatment Exposure on Specialty MHS Use via Internalizing/Externalizing Problems
There was an indirect effect of maltreatment exposure on specialty MHS use via externalizing problems for both non-Hispanic White (β = 0.14, p < .05) and African American youth (β = 0.22, p < .05), but not for Latinos. Therefore, for non-Hispanic White and African American youth maltreatment exposure was linked to MHS use via an indirect pathway through externalizing problem severity. However, the indirect effect of maltreatment exposure on specialty MHS use via internalizing problem severity was only significant for non-Hispanic Whites (β = 0.09, p < .05). Thus, although maltreatment exposure significantly predicted both internalizing and externalizing problems for all racial/ethnic groups, non-Hispanic White youth were the only group for whom pathways through both types of problems significantly predicted subsequent MHS use. For African American youth, MHS use was predicted by a pathway linking maltreatment exposure to externalizing problem severity.
Discussion
The current study sought to examine racial/ethnic differences in pathways to specialty MHS in a nationally representative sample of youth in contact with the CW system. Consistent with prior research, we found that African American youth (10.9%) were less likely to receive specialty MHS overall relative to non-Hispanic White youth (21.8%). However, there were important differences in the pathways leading to specialty MHS use that varied as a function of youth race/ethnicity and child behavior problem type.
For all racial/ethnic groups, we hypothesized that maltreatment exposure would be a strong predictor of both internalizing and externalizing problems, which was supported by our findings. We also expected that there would be a strong correlation between internalizing and externalizing problem severity in this high-risk population, which was also supported by our data. While our model considered the potential direct association between maltreatment exposure and MHS use, we predicted that maltreatment exposure would be indirectly linked to MHS via child emotional/behavior problems. Given the foregoing evidence suggesting racial/ethnic disparities in MHS use as a function of problem type for youth in contact with CW, we further hypothesized that these indirect pathways to care would differ for racial/ethnic minority youth, which also supported by our data. Specifically, although maltreatment exposure significantly predicted both internalizing and externalizing problem severity across all racial/ethnic groups, non-Hispanic White youth were the only group for whom both types of problems significantly predicted subsequent specialty MHS use. Only externalizing problems predicted subsequent specialty MHS use for African American youth and neither type of MH problem predicted service use for Latinos. Thus, we found evidence of disparities in pathways from maltreatment exposure to mental health service use that varied by problem-type and youth race/ethnicity. Furthermore, while externalizing problem severity was a predictor of specialty MHS use for both non-Hispanic White and African American youth, it was a much stronger predictor for African American compared to non-Hispanic White youth. Conversely, internalizing problem severity was a stronger predictor of specialty MHS use for non-Hispanic White youth compared to African American and Latino youth.
Taken together, these findings suggest a more complicated association between race/ethnicity and MHS use than what is suggested by research examining disparities without considering the type of MH problem in question. These differential patterns may be explained by individual, family, and system-level factors that lead to the particular visibility of racial/ethnic minority youth with disruptive behavior as compared to internalizing problems. However, the data and design of the current study does not enable us to discern whether these racial/ethnic disparities are due to differences in responsiveness on the part of the CW system in linking certain youth with certain needs to specialty MHS, or whether individual and family factors deter families from following through with MHS receipt.
It is likely that individual, family, and system-level factors converge to influence problem-specific disparities in pathways from maltreatment exposure to MH care for different racial/ethnic groups. Ethnic minority youth are overrepresented in CW and juvenile justice (Crane & Ellis, 2004; Morton, 1999), where externalizing problems are closely scrutinized. Disruptive behavior is also a robust predictor of placement instability in CW (James, Landsverk, & Slymen, 2004), thus more resources may be directed towards youths with externalizing problems to support placement stability. CW workers may attend particularly to addressing the externalizing behaviors of African American youth who, in general, are at greater risk of placement instability and other negative CW outcomes. Data from NSCAW I suggest that externalizing problems are systematically associated with placement disruption for African American children but not for non-Hispanic White children (Foster, Hillemeier & Bai, 2011). Perhaps stronger linkages to effective care for disruptive behavior problems are all the more important for African American children who are more vulnerable to adverse system outcomes.
Yet, it may also be the case that individual and family factors work to amplify system-level determinants of MHS use. Even if a referral for MHS is made on the part of the CW system, racial/ethnic minority parents may hold culturally-influenced perceptions of child MH problems (e.g., beliefs about causes) and MHS (e.g., mistrust, stigma,) that may dissuade or encourage help-seeking (Cauce et al., 2002). These barriers may be more pronounced in the identification of and help-seeking for internalizing problems compared to externalizing problems in ethnic minority families (Gudiño et al., 2009). While child behavior that is disruptive, oppositional, or defiant may run counter to cultural values that emphasize respect, obedience, and deference to adults, internalizing problems may not necessarily be at odds with such cultural values. The adult distress threshold model of cultural influence (Weisz et al., 1988) suggests that culture may influence perceptions of how serious a problem is and decisions about what should be done. Because internalizing problems are already less likely to lead to MHS use, relative to externalizing problems (Wu et al., 1999), the presence of internalizing problems in racial/ethnic minority children may not lead to sufficient distress to overcome a higher threshold for concern and the aforementioned barriers to accessing mental health services.
Examining specialty MHS use prospectively, use of a nationally representative sample of children in contact with the CW, and the application of analytic methods to examine moderation and indirect effects are notable strengths of this study. However, our results should be interpreted in light of study limitations. First, we relied on parent-report for all study variables and it would be important to replicate these results with multi-informant methods. Second, while the use of a general maltreatment latent variable is a strength in that it accounts for the complexity of exposure to such adversity, the current study does not examine potential differences related to specific forms of maltreatment. Third, although paths from internalizing and externalizing problems to MHS use were in the predicted direction, they were not statistically significant predictor of MHS use for Latino youth. Despite the large nationally representative sample, uneven group sizes could have impacted significance levels. For example, the relatively smaller sample of Latino youth and the resulting larger standard errors for estimates may have limited our ability to identify significant effects. Additional research examining specific determinants of MHS use for Latino youth in contact with child welfare is warranted. Fourth, we were unable to verify the Missing at Random (MAR) assumption from our missing data estimation used in Mplus. However, this concern is mitigated by the fact that there were few missing data. Fifth, we defined service use as any contact with an outpatient specialty MH provider and cannot comment on the effectiveness or quality of services. Furthermore, although we assessed child behavior problems, we are unable to specify the reasons families sought services. Lastly, while we examined overall racial/ethnic group disparities in specialty MHS use, we were unable to examine more proximal indicators of culture in our model due to limitations of the NSCAW data set. Research is needed to refine our understanding of enthnocultural factors impacting MHS use. Despite these limitations, these results highlight concerning patterns of disparities that require further study.
Gatekeepers of MHS, including those within the family and the broader CW system, may be more likely to direct attention to racial/ethnic minority youth with externalizing problems who are also at risk of having poor CW system outcomes. Yet, this greater responsiveness to disruptive behavior among African American children occurs in the context of disparities whereby racial/ethnic minorities are less likely to receive services overall. It stands to reason that racial/ethnic minority youth with clinical need that does not include disruptive behavior may be driving the overall pattern of disparities (Gudiño et al., 2012). Increased awareness of these disparities as a function of problem type and increased awareness of the negative impact of untreated internalizing problems is needed within CW. While information provided to CW staff and families of children who come into the system may be one important avenue for targeting disparities, efforts must also focus on improving methods for identifying need and facilitating referral to MHS. Efforts to support the implementation of evidence-based MH assessment within CW and to examine the impact of these methods on disparities may help ensure equitable linkage of vulnerable youths to MHS.
References
- Achenbach TM. Manual for the Child Behavior Checklist/4–18 and 1991 profile. Burlington, VT: University of Vermont, Department of Psychiatry; 1991. [Google Scholar]
- Achenbach TM, Rescorla L. Manual for the ASEBA school-age forms & profiles: An integrated system of multi-informant assessment. Burlington, VT: ASEBA; 2001. [Google Scholar]
- Angold A, Costello EJ, Erkanli A. Comorbidity. Journal of Child Psychology and Psychiatry. 1999;40:57–87. [PubMed] [Google Scholar]
- Ascher BH, Farmer E, Burns BJ, Angold A. The child and adolescent services assessment (CASA): Description of psychometrics. Journal of Emotional and Behavioral Disorders. 1996;4(1):12–20. [Google Scholar]
- Burns BJ, Phillips SD, Wagner HR, Barth RP, Kolko DJ, Campbell Y, Landsverk J. Mental health need and access to mental health services by youth involved with child welfare: A national survey. Journal of the American Academy of Child and Adolescent Psychiatry. 2004;43(8):60–970. doi: 10.1097/01.chi.0000127590.95585.65. [DOI] [PubMed] [Google Scholar]
- Cauce AM, Domenech-Rodriguez M, Paradise M, Cochran BN, Shea JM, Srebnik D, Baydar N. Cultural and contextual influences in mental health help seeking: A focus on ethnic minority youth. Journal of Consulting and Clinical Psychology. 2002;70(1):44–55. doi: 10.1037//0022-006x.70.1.44. [DOI] [PubMed] [Google Scholar]
- Cosgrove VE, Rhee SH, Gelhorn HL, Boeldt D, Corley R, Ehringer M, et al. Structure and etiology of co-occurring internalizing and externalizing disorders in adolescents. Journal of Abnormal Child Psychology. 2011;39:109–123. doi: 10.1007/s10802-010-9444-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Crane KD, Ellis RA. Benevolent intervention or oppression perpetuated: Minority overrepresentation in children’s services. Journal of Human Behavior in the Social Environment. 2004;9(1–2):19–38. [Google Scholar]
- Edwards VJ, Holden GW, Felitti VJ, Anda RF. Relationship between multiple forms of childhood maltreatment and adult mental health in community respondents: Results from the adverse childhood experiences study. The American Journal of Psychiatry. 2003;160(8):1453–1460. doi: 10.1176/appi.ajp.160.8.1453. [DOI] [PubMed] [Google Scholar]
- Farmer EMZ, Burns BJ, Chapman MV, Phillips SD, Angold A, Costello EJ. Use of mental health services by youth in contact with social services. Soc Serv Rev. 2001;75:605–624. [Google Scholar]
- Foster EM, Hillemeier MM, Bai Y. Explaining the disparity in placement instability among African-American and white children in child welfare: A Blinder- Oaxaca decomposition. Children & Youth Services Review. 2011;33(1):118–125. [Google Scholar]
- Garland AF, Besinger BA. Racial/ethnic differences in court referred pathways to mental health services for children in foster care. Children and Youth Services Review. 1997;19(8):651–666. [Google Scholar]
- Garland AF, Landsverk JL, Hough RL, Ellis-MacLeod E. Type of maltreatment as a predictor of mental health service use for children in foster care. Child Abuse & Neglect. 1996;20(8):675–688. doi: 10.1016/0145-2134(96)00056-7. [DOI] [PubMed] [Google Scholar]
- Garland AF, Lau AS, Yeh M, McCabe KM, Hough RL, Landsverk JA. Racial and ethnic differences in utilization of mental health services among high-risk youths. The American Journal of Psychiatry. 2005;162:1336–1343. doi: 10.1176/appi.ajp.162.7.1336. [DOI] [PubMed] [Google Scholar]
- Gudiño OG, Lau AS, Yeh M, McCabe KM, Hough RL. Understanding racial/ethnic disparities in youth mental health services: Do disparities vary by problem type? Journal of Emotional and Behavioral Disorders. 2009;17(1):3–16. [Google Scholar]
- Gudiño OG, Martinez JI, Lau AS. tMental health service use for children in contact with Child Welfare: Racial disparities depend on problem type. Psychiatric Services. 20122012 doi: 10.1176/appi.ps.201100427. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hurlburt MS, James S, Landsverk J, Slymen DJ, Zhang J. Relationship between entry into child welfare and mental health service use. Psychiatric Services. 2005;56(8):981–987. doi: 10.1176/appi.ps.56.8.981. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ivanova MY, Dobrean A, Dopfner M, Erol N, Fombonne E, Fonseca AC, Chen WJ. Testing the 8-syndrome structure of the child behavior checklist in 30 societies. Journal Clinical Child Adolescent Psychology. 2007;36(3):405–417. doi: 10.1080/15374410701444363. [DOI] [PubMed] [Google Scholar]
- James S, Landsverk J, Slymen DJ. Placement movement in out-of-home care: Patterns and predictors. Children and Youth Services Review. 2004;26(2):185–206. [Google Scholar]
- Kataoka S, Zhang L, Wells K. Unmet need for mental health care among U. S. children: Variation by ethnicity and insurance status. American Journal of Psychiatry. 2002;159:1548–1555. doi: 10.1176/appi.ajp.159.9.1548. [DOI] [PubMed] [Google Scholar]
- Landsverk J, Garland AF, Leslie LK. Mental health services for children reported to child protective services. In: Myers JEB, Hendrix CT, Berliner L, Jenny C, Briere J, Reid T, editors. APSAC Handbook on Child Maltreatment. 2nd ed. Thousand Oaks, CA: Sage; 2002. pp. 487–507. [Google Scholar]
- Latkovich SA. An empirical test of the construct validity of the Child Behavior Checklist. Chicago, IL: Paper presented at the Annual Meeting of the Mid-Western Educational Research Association; 1996. Oct, [Google Scholar]
- Lansford JE, Dodge KA, Pettit GS, Bates JE, Crozier J, Kaplow J. A 12-year prospective study of the long-term effects of early child physical maltreatment on psychological, behavioral, and academic problems in adolescence. Archives of Pediatrics & Adolescent Medicine. 2002;156(8):824–830. doi: 10.1001/archpedi.156.8.824. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lau AS, Litrownik AJ, Newton RR, Black MM, Everson MD. Factors affecting the link between physical discipline and child externalizing problems in Black and White families. Journal of Community Psychology. 2006;34(1):89–103. [Google Scholar]
- Leslie LK, Landsverk J, Ezzet-Loftstrom R, Tschann JM, Slymen DJ, Garland AF. Children in foster care: Factors influencing outpatient mental health service use. Child Abuse & Neglect. 2000;24(4):465–476. doi: 10.1016/s0145-2134(00)00116-2. [DOI] [PubMed] [Google Scholar]
- Leslie LK, Hurlburt MS, James S, Landsverk J, Slymen DJ, Jinjin Zhang. Relationship between entry into Child Welfare and mental health service use. Psychiatric Services. 2005;56(8):981–987. doi: 10.1176/appi.ps.56.8.981. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McDonald RP, Ho MR. Principles and practice in reporting structural equation analyses. Psychological Methods. 2002;7:64–82. doi: 10.1037/1082-989x.7.1.64. [DOI] [PubMed] [Google Scholar]
- McGee RA, Wolfe DA, Yuen SA, Wilson SK, Carnochan J. The measurement of maltreatment: A comparison of approaches. Child Abuse & Neglect. 1995;19(2):233–249. doi: 10.1016/0145-2134(94)00119-f. [DOI] [PubMed] [Google Scholar]
- Morton TD. The increasing colorization of America’s child welfare system: The overrepresentation of African American children. Policy and Practic. 1999;57(4):23–30. [Google Scholar]
- Muthén LK, Muthén BO. Mplus User’s eGuide. Fifth Edition. Los Angeles, CA: Muthén & Muthén; 1998–2007. [Google Scholar]
- Nakamura BJ, Ebesutani C, Bernstein A, Chorpita BF. A psychometric analysis of the Child Behavior Checklist DSM-oriented scales. Journal of Psychopathology & Behavioral Assessment. 2009;31(3):178–189. doi: 10.1007/s10862-009-9174-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- National Survey of Child and Adolescent Well-Being, Research Group. National Data Archive on Child Abuse and Neglect. Ithaca, NY: Cornell University; 2004. Appendix Volume IIA: General Release Version. [Google Scholar]
- Ney PG, Fung T, Wickett AR. The worst combinations of child abuse and neglect. Child Abuse & Neglect. 1994;18(9):705–714. doi: 10.1016/0145-2134(94)00037-9. [DOI] [PubMed] [Google Scholar]
- Taussig HN. Risk behaviors in maltreated youth placed in foster care: a longitudinal study of protective and vulnerability factors. Child Abuse & Neglect. 2002;26:1179–1999. doi: 10.1016/s0145-2134(02)00391-5. [DOI] [PubMed] [Google Scholar]
- Reichenheim ME, Moraes CL. Psychometric properties of the Portuguese version of the Conflict Tactics Scales: Parent-Child Version (CTSPC) used to identify child abuse. Cadernos De Saúde Pública / Ministério Da Saúde, Fundacão Oswaldo Cruz, Escola Nacional De Saúde Pública. 2006;22(3):503–515. doi: 10.1590/s0102-311x2006000300005. [DOI] [PubMed] [Google Scholar]
- Rubio-Stipec M, Bird H, Canino G, Gould M. The internal consistency and concurrent validity of a Spanish translation of the Child Behavior Checklist. Journal of Abnormal Child Psychology. 1990 Jan 01;18(4):393–406. doi: 10.1007/BF00917642. [DOI] [PubMed] [Google Scholar]
- Straus MA, Hamby SL, Finkelhor D, Moore DW, Runyan D. Identification of child maltreatment with the parent-child conflict tactics scales: Development and psychometric data for a national sample of American parents. Child Abuse & Neglect. 1998;22(4):249–270. doi: 10.1016/s0145-2134(97)00174-9. [DOI] [PubMed] [Google Scholar]
- Weisz JR, Suwanlert S, Chaiyasit W, Weiss B, Walter BR, Anderson WW. Thai and American Perspectives on Over- and Undercontrolled Child Behavior Problems: Exploring the Threshold Model among Parents, Teachers, and Psychologists. Journal of Consulting and Clinical Psychology. 1988;56(4):601–609. doi: 10.1037//0022-006x.56.4.601. [DOI] [PubMed] [Google Scholar]
- Wu P, Hoven CW, Bird HR, Moore RE, Cohen P, Alegria M, …Roper MT. Depressive and disruptive disorders and mental health service utilization in children and adolescents. Journal of the American Academy of Child & Adolescent Psychiatry. 1999;38(9):1081–1090. doi: 10.1097/00004583-199909000-00010. [DOI] [PubMed] [Google Scholar]