Abstract
This study aimed to develop an intravesical delivery system of gemcitabine HCl for superficial bladder cancer in order to provide a controlled release profile, to prolong the residence time, and to avoid drug elimination via urination. For this aim, bioadhesive nanoparticles were prepared with thiolated chitosan (chitosan–thioglycolic acid conjugate) and were dispersed in bioadhesive chitosan gel or in an in situ gelling poloxamer formulation in order to improve intravesical residence time. In addition, nanoparticle-loaded gels were diluted with artificial urine to mimic in vivo conditions in the bladder and were characterized regarding changes in gel structure. The obtained results showed that chitosanthioglycolic acid nanoparticles with a mean diameter of 174.5±3.762 nm and zeta potential of 32.100±0.575 mV were successfully developed via ionotropic gelation and that the encapsulation efficiency of gemcitabine HCl was nearly 20%. In vitro/ex vivo characterization studies demonstrated that both nanoparticles and nanoparticle-loaded chitosan and poloxamer gels might be alternative carriers for intravesical administration of gemcitabine HCl, prolonging its residence time in the bladder and hence improving treatment efficacy. However, when the gel formulations were diluted with artificial urine, poloxamer gels lost their in situ gelling properties at body temperature, which is in conflict with the aimed formulation property. Therefore, 2% chitosan gel formulation was found to be a more promising carrier system for intravesical administration of nanoparticles.
Keywords: chitosan-TGA, nanoparticle, gemcitabine HCl, intravesical administration, chitosan, poloxamer, superficial bladder cancer
Introduction
Bladder cancer is one of the most common malignancies; it accounts for 6% of all cancer cases in men and 3% in women. More than 70% of bladder cancers are superficial at diagnosis, and transurethral resection of the tumor (TUR) is the initial treatment for such patients. TUR is generally followed by chemotherapy to reduce disease recurrence and/or progression.1 However, systemic administration of chemotherapeutic drugs offers little therapeutic benefit for patients with superficial bladder cancer, as the urothelial layer of the bladder is not vascularized.2,3 In contrast, intravesical chemotherapy provides the advantages of ensuring high drug concentrations at the tumor site, minimizing systemic side effects, and by avoiding a first pass metabolism, dose reduction would in fact be feasible.2 The success of intravesical therapy depends on direct contact between the drug and the urothelium. However, the bladder is a very well purged organ, so the periodical voiding of urine washes out the drug and reduces the residence time in the bladder. To overcome this situation, frequent treatments with repeated catheterizations are required, leading in many cases to irritation during voiding, bladder fibrosis, and infections.4 Hence, there is a need for the development of sustained intravesical drug delivery systems, which can provide prolonged contact between the drug and the affected tissues and can reduce the chance of recurrence of the disease.5
Gemcitabine hydrochloride (Gem-HCl) is a deoxycytidine analog with a broad spectrum of antitumor activity. It has been shown to be effective and well tolerated for several tumors, such as superficial bladder cancer, when given systemically. Nowadays, Gem-HCl seems to have fulfilled the requirements to be a promising new candidate for standard intravesical therapy.6 It seems to be one of the most active drugs against superficial bladder cancer, with significantly higher activity than many other drugs such as thiotepa, doxorubicin, epirubicin, or mitomycin-C that have been used intravesically so far.7,8
The aim of this study was to develop and characterize an intravesical delivery system for Gem-HCl, which was able to prolong intravesical residence time, to provide controlled drug release, and to minimize drug elimination via urination. Bioadhesive colloidal drug delivery systems such as microspheres, microparticles, and nanoparticles (NPs) have emerged as promising delivery systems for intravesical chemotherapeutic agents in the last decade.9–11 Among them, NPs came into focus, exhibiting properties such as enhancing the ability of drugs to cross the urothelium and increasing intransvesical absorption of encapsulated drugs. The efficiency of NPs is increased by bioadhesive properties, providing an intimate contact with the mucus layer. Therefore, in the current study, NPs prepared with thiolated chitosan (chitosan–thioglycolic acid [TGA]) that exhibited a comparatively high concentration of free thiol groups were chosen as an intravesical dosage form due to their higher bioadhesive, permeation-enhancing, and release-controlling properties.12 In addition, the prepared NPs were dispersed in a bioadhesive chitosan gel and in a poloxamer (Plx) gel exhibiting in situ gelling properties to increase intravesical residence time. Afterward, NP-loaded gels were diluted with Tyrode solution, which served as artificial urine to mimic the in vivo conditions when the formulations come into contact with urine in the bladder. Finally, for comparison reasons, comprehensive in vitro/ex vivo studies were carried out on Gem-HCl-loaded NPs, gels, and their dilutions with Tyrode solution.
Materials and methods
Materials
Chitosan (high molecular weight, Brookfield viscosity [1%, m/V, in 1% acetic acid solution at 25°C]; 800,000 mPa·s, >75% deacetylated), sodium tripolyphosphate (TPP), and TGA were purchased from Sigma-Aldrich Co (St Louis, MO, USA). Plx 188 and Plx 407 were kind gifts from BASF Chemicals (Ludwigshafen, Germany). Gem-HCl was purchased from Sun Pharmaceutical Industries Ltd (Mumbai, India). All other chemicals were of analytical grade.
Synthesis and characterization of chitosan–TGA
The covalent attachment of TGA to chitosan was achieved by the formation of amide bonds between the carboxylic acid groups of TGA and the primary amino groups of the polymer, as described previously by our research group.12 The amount of thiol groups immobilized on chitosan was determined photometrically with Ellman’s reagent.13
Preparation of NPs
NPs were prepared by ionotropic gelation of chitosan–TGA with TPP, according to a method described previously.12,14,15 Briefly, chitosan–TGA was dissolved in distilled water (2 mg/mL) and pH was adjusted to 4.8. TPP aqueous solution (1 mg/mL) was added to chitosan–TGA solution dropwise and was stirred at room temperature to obtain blank NPs.
To prepare Gem-HCl-loaded NPs, Gem-HCl was dissolved in TPP solution (5 mg/mL) and was then added to the chitosan–TGA solution. Spontaneously formed NPs were separated by centrifugation at 13,500 rpm for 1 hour, and the supernatant was discarded for determination of encapsulation efficiency.
Characterization of NPs
Particle size distribution and zeta potential
Mean diameters, polydispersity index values, and surface charges of NPs were determined by Malvern Zetasizer NanoZS (Malvern Instruments, Malvern, UK).
Scanning electron microscopy
Scanning electron microscopy (SEM) imaging of the NP formulations was performed with a SEM Quanta FEG-250. NP samples were dried at 40°C, fixed on metal plates, and were coated with gold (Emitech K550 X; 1.5 minutes, 15 mA, 6×10−2 mbar under vacuum). Surface morphology of the particles was observed at an accelerated voltage of 5 kV.
Encapsulation efficiency and drug loading of NPs
NPs were separated from aqueous suspension by centrifugation at 13,500 rpm for 1 hour. Supernatant was carefully removed and the amount of free Gem-HCl was determined by ultra-performance liquid chromatography (UPLC).
Encapsulation efficiency and drug loading were calculated according to the following equations:16,17
| (1) |
| (2) |
Gem-HCl was quantified via a validated UPLC method on Thermo Hypersil Gold (100×2.1 mL, 3 µm) column at 25°C by using an isocratic elution method with acetonitril:ammonium acetate buffer solution (pH 5.5) (2.5/97.5, v/v) at a flow rate of 400 µL/min. Retention time of Gem-HCl was 1.78 minutes and total analysis time was 5 minutes. The calibration curve of Gem-HCl was linear in the concentration range of 5–30 µg/mL (r2=0.9989).
Preparation of chitosan and Plx gels
For the preparation of chitosan gel, 2% (w/w) chitosan (high molecular weight) was dissolved in diluted lactic acid solution (1%, v/v).18 The gel was left at 25°C until a clear solution was obtained, and then NPs were dispersed in chitosan gel.
In situ Plx gel was prepared according to cold method.19 Briefly, Plx 407 (20%, w/w) and Plx 188 (10%, w/w) were slowly added to distilled water at 4°C with continuous agitation. The gel was left at 4°C until a clear solution was obtained, and NPs were suspended in the Plx gel base.20
Dilution of chitosan and Plx gels with artificial urine
Rheological, mechanical, and bioadhesive properties of chitosan and Plx gel formulations were evaluated after dilution with Tyrode solution21 used as artificial urine in a ratio of 1:1 to mimic the in vivo conditions in the bladder at 37°C.
Characterization of gels
Viscosity measurements
Viscosity of chitosan and Plx gels was determined with an AND Vibro viscometer (SV-10; 10.0–10,000 mPas) at 25°C and at 37°C (n=6).
Gelation temperature and gelation time of Plx gels
The sol–gel transition temperatures and gelation times of Plx gels were determined from oscillation measurements utilizing a rheometer (Haake Mars, AR 2000; Thermo Fisher Scientific, Waltham, MA, USA) and a stainless steel and plate/plate geometry probe (diameter 35 mm). The samples were heated at a rate of 2°C every 60 seconds, the temperature changed from 7°C–70°C, and the frequency was fixed to 0.01 Hz during the procedure. The sol–gel transition temperature graph was determined by plotting temperature as a function of the viscosity (η′), and the transition point was defined as the point where the viscosity was halfway between the values for the solution and the gel (n=6).22
Rheological properties of formulations
All formulations were characterized rheologically using a Haake Mars rheometer (Haake Mars, AR 2000). Continuous shear analysis of each formulation was performed at 25°C±0.1°C and 37°C±0.1°C, in flow mode, and in conjunction with parallel steel plate geometry (diameter 35 mm) and gap of 0.3 mm. Briefly, samples were carefully applied to the lower plate of the rheometer, ensuring that formulation shearing was minimized and allowing equilibration for at least 1 minute prior to analysis. Upward and downward flow curves were measured over a range of shear rates (10–1,000 s−1). The flow properties of the samples were determined with at least six replicates.23,24
Oscillatory analysis of each formulation was performed after determination of its linear viscoelastic region at 25°C±0.1°C and 37°C±0.1°C, where stress was directly proportional to strain, and the storage modulus remained constant. Frequency sweep analysis was performed over the frequency range of 0.1–10 Hz following application of a constant stress, and with a standard gap size of 0.3 mm for each sample. Storage modulus (G′) and loss modulus (G″) were determined (n=6).25,26
Mechanical properties of formulations
Mechanical properties of the formulations were determined with a software-controlled penetrometer (TA-TX Plus; Stable Micro Systems, Ltd, Godalming, UK) at 25°C and 37°C. Briefly, formulations were transferred into glass vials (20 mL), and an analytical probe was twice compressed into each formulation to a defined depth (15 mm) and at a defined rate (2 mm·s−1), allowing a delay period (15 seconds) between compressions. Force–time curves were obtained, and mechanical parameters (hardness, adhesiveness, compressibility, cohesiveness, and elasticity) were calculated from these resultant curves (n=6).27
Syringeability of formulations
The work required to expel formulations from a syringe was measured using a force transducer connected to TA-XT Plus texture analyzer. After a short time, formulations were packed into 2 mL plastic syringes connected to a catheter. The syringe was then placed in the metallic support and the plunger of the syringe was pushed with a constant force of 0.5 N. The resistance to expression of syringe contents through the catheter during plunger compression was derived from the area under the force–time curves at 25°C (n=6).28
Bioadhesive properties of formulations
The bioadhesive properties of formulations were evaluated using the TA-XT Plus texture analyzer equipped with a 5 kg load cell. Bovine mucosal bladder tissue, having been obtained fresh from a local slaughterhouse, was separated from underlying tissues, washed, cut into smaller pieces, and rinsed carefully. Sections (>2 mm in thickness) were taken from the inner part of the surface of the mucosal membrane and were attached to the lower end of the texture analyzer probe (10 mm diameter). The gels were maintained at 37°C and were placed to the lower end of the texture analyzer probe (10 mm diameter). The probe holding the gel was lowered onto surface of the bladder mucosa with a constant speed of 0.1 mm/s, and a contact force of 0.05 N was then applied for 2 minutes. The probe was then moved vertically upward at a constant speed of 0.1 mm/s, and the maximum detachment force (F) and the area under the curve (AUC, also termed mucoadhesion) were determined from the resultant force–distance graph.29
In vitro release studies
The in vitro release of Gem-HCl from chitosan–TGA NPs and chitosan–TGA NP-loaded chitosan or Plx gels were evaluated with dialysis membrane tubes (Spectra/Por Regenerated Cellulose, 6,000–8,000 molecular weight cutoff [MWCO]). Briefly, 5 mL NP suspension or NP-loaded chitosan or Plx gels were packed in dialysis bags and were then placed in 100 mL phosphate buffer pH 6.5 at 37°C. The receptor medium was continuously stirred at 300 rpm. At predetermined time intervals, samples were withdrawn, and the drug content was analyzed with UPLC (n=6).
Ex vivo permeation studies
The ex vivo permeation studies were performed using Franz-type diffusion cells across freshly excised bovine bladder mucosa. Briefly, freshly excised bovine bladder mucosa was separated from underlying tissues and was mounted on diffusion cells. Formulations were placed on a donor compartment, and the receptor compartment was filled with 20 mL pH 6.5 phosphate buffer. At predetermined time intervals, samples were taken from the receptor compartment, and the permeated amount of Gem-HCl was analyzed with UPLC (n=6).
Histopathological evaluation
At the end of the 4 hours of ex vivo permeation study, the excess amount of the formulation was removed, and the mucosa samples were fixed in 4% neutral-buffered formalin. Standard procedures were applied to prepare 4 mm thick tissue sections, and the specimens were stained with hematoxylineosin (HE).30 For each formulation, at least six independent bovine bladder mucosa samples were histopathologically evaluated with a microscope (Olympus BX50) to investigate the tissue damage of healthy mucosa.
Statistical data analysis
Statistical data analysis was performed using the Student’s t-test with P<0.05 as the minimal level of significance.
Results and discussion
Nearly 40% of all superficial carcinomas of the bladder are classified as “intermediate risk” for recurrence or progression and should be managed with prophylactic intravesical immunotherapy or chemotherapy.6,31 Most of the immunotherapy or chemotherapy agents being used are considered as effective in decreasing subsequent recurrences, but they can lead to some increase in side effects. Therefore, new treatment options for intravesical chemotherapy are needed to combine proven efficacy with good tolerability. Gem-HCl is a pyrimidine antimetabolite with a broad spectrum of antitumor activity. When given systemically, it has shown significant activity as a single agent, even against invasive bladder cancers, yielding response rates of 27%–38%.32
In addition, several characteristics make it a promising candidate for intravesical therapy for superficial bladder cancer. For instance, Gem-HCl has a molecular weight of 299 Da, which is substantially lower than that of commonly used intravesical chemotherapeutic agents such as mitomycin C (389 Da) and doxorubicin (589 Da). This comparatively smaller size may enable Gem-HCl to penetrate the bladder mucosa with beneficial effects in the treatment of early invasive bladder cancers. On the other hand, systemic absorption of chemotherapeutic drugs through the bladder wall is thought to be unlikely for agents with a molecular weight of >300 Da.2 Thus, the molecular weight of Gem-HCl is high enough to prevent significant systemic uptake in an intact bladder.6 For these reasons, Gem-HCl was chosen as a chemotherapeutic agent for intravesical therapy of non-invasive bladder cancer in the current study.
Synthesis and characterization of chitosan–TGA
Thiolated polymers (thiomers) are hydrophilic polymers (eg, polyacrylates, polycarbophil, deacetylated gellan gum, alginate, or chitosan), and are derivatized with thiol groups on their side chains. They are capable of forming covalent disulfide bonds with biological membranes. Therefore, they provide strong mucoadhesion, and they guarantee the localization of a drug delivery system at the application site. Additionally, they form intra- and inter-chain disulfide bonds within the polymeric network, and the cohesiveness, and subsequently the stability, of the carrier can be guaranteed. In addition, thiomers have enzyme inhibitory and permeation-enhancing properties.33 In this context, it was decided to use thiolated polymers for the preparation of nanoparticulate systems for intravesical administration in the present study. Previously, the suitability of thiolated chitosan–TGA for the preparation of trimethoprim-loaded NPs was evaluated for intravesical treatment of interstitial cyctitis, and the improved mucoadhesive properties of chitosan–TGA on the intravesical mucosa was proven.12 In the current study, chitosan–TGA was therefore chosen as a thiolated polymer for the preparation of Gem-HCl-loaded NPs. After the preparation of chitosan–TGA, the amount of thiol groups immobilized on chitosan was determined as 1,328±147 µmol of free SH groups per gram polymer, and this result corresponds to a coupling rate of 30.58%.
Preparation and characterization of NPs
Although intravesical administration of chemotherapeutics has many advantages such as delivering drugs in high concentration to the tumor-bearing bladder and minimizing systemic exposure, there are still some challenges to overcome. For instance, sometimes chemotherapeutic drug-induced temporary irritative voiding results in draining the drug out from the bladder and shortening the intended duration of instillation. In addition, urothelium has six to seven cellular layers, which make it impermeable to all irritants and also drugs; thus, intravesical delivery fails to provide sufficient drug concentration behind these barriers.34 Therefore, new approaches are needed to overcome the challenges caused by urine flushing/cellular barriers, and nanotechnology holds tremendous promise for the future of intravesical delivery of drugs into the bladder. Among the available options, NPs with a well-defined particle size and shape can have immense potential for intravesical delivery, as they can enhance the ability of drugs to cross the urothelium. Moreover, higher surface-to-volume ratio of NPs can be responsible for an increase in transvesical absorption of encapsulated drugs.35 The efficiency of intravesical therapy with NPs is increased by bioadhesive properties because of an intensified, close contact with the mucus layer.
Accordingly, bioadhesive chitosan–TGA NPs were chosen as the intravesical dosage form in the current study. NPs were formed due to the interaction of positive amino groups of chitosan and negative phosphate groups of TPP.14 According to several preformulation studies, a pH of 4.8 was identified as most suitable for the ionotropic gelation process, and a polymer-to-TPP ratio of 14:3 led to NPs with the most favorable properties, which were a narrow particle size distribution and a comparatively higher zeta potential.
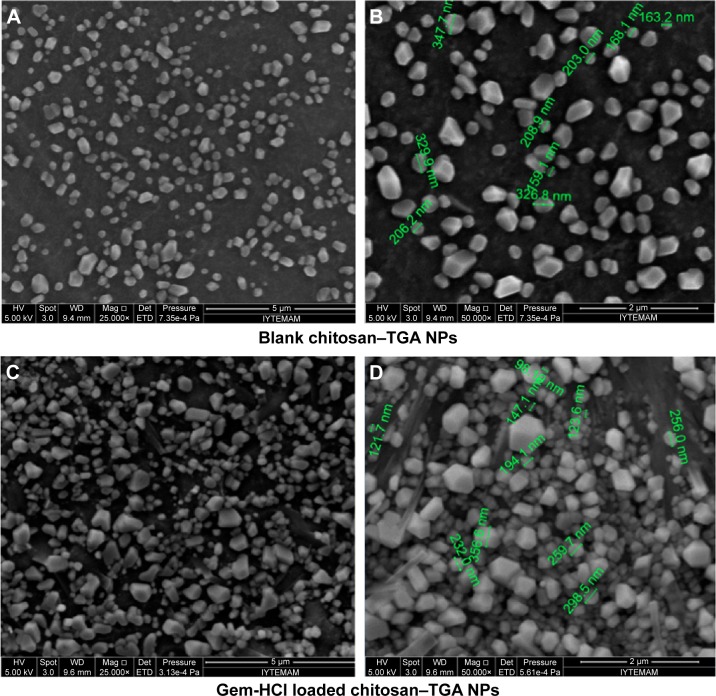
The mean diameters of blank and Gem-HCl-loaded NPs were measured according to dynamic light scattering method, and the results showed that this preparation method generates particles with a size range of 175–190 nm (Figure 1 and Table 1). The obtained particle size values were found to be advantageous, as NPs smaller than 400 nm were considered to be promising for enhancing permeation in cancerous bladder tissues.15 In addition, the size distribution of NPs might be defined as narrow, because the calculated polydispersity indices were smaller than 0.3.
Figure 1.
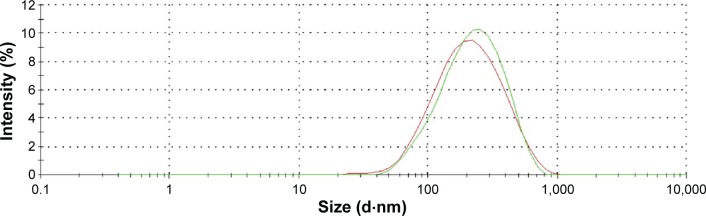
Particle size distribution of blank and Gem-HCl-loaded NPs (repeated n=6).
Notes: Green line, blank NPs; red line, Gem-HCl-loaded NPs.
Abbreviations: Gem-HCl, gemcitabine hydrochloride; NP, nanoparticle.
Table 1.
Particle size, polydispersity index, and zeta potential values of blank and Gem-HCl-loaded NPs (repeated n=6)
| Formulation | Particle size (d·nm) ± SD | Polydispersity index ± SD | Zeta potential (mV) ± SD |
|---|---|---|---|
| Chitosan–TGA NPs | 188.3±2.054 | 0.229±0.020 | 33.500±1.030 |
| Gem-HCl-loaded chitosan–TGA NPs | 174.5±3.762 | 0.239±0.012 | 32.100±0.575 |
Abbreviations: TGA, thioglycolic acid; NPs, nanoparticles; Gem-HCl, gemcitabine hydrochloride; SD, standard deviation.
Due to the free amino groups in chitosan, blank and Gem-HCl-loaded NPs displayed positive charges. Zeta potentials of the blank or Gem-HCl-loaded particles were found to be >30 mV, which shows their stability, as particles with zeta potentials > ±30 mV are considered to be more stable due to a more pronounced electric repulsion.36
The encapsulation efficiency and drug loading of Gem-HCl NPs were determined to be 19.2%±5.9% and 9.4%±2.3%, respectively. This encapsulation efficiency might be considered as low, but in the literature, similar or even lower percentages were reported for water-soluble drugs. This might be attributed to rapid partitioning of water-soluble active substances into the aqueous phase, and hence, decreased entrapment into the NPs during the ionotropic gelation process.37
SEM investigations were carried out on NPs to elucidate their morphological properties. As illustrated in Figure 2, all particles were of cornered shapes and had a smooth surface.
Figure 2.
SEM images of blank NPs and Gem-HCl loaded chitosan–TGA NPs.
Notes: Magnification ×25,000 (A and C); magnification ×50,000 (B and D).
Abbreviations: SEM, scanning electron microscopy; TGA, thioglycolic acid; NP, nanoparticle; Gem-HCl, gemcitabine hydrochloride.
Preparation of chitosan and Plx gels
Bioadhesive polymers are used for targeting a drug to a particular region of the body for extended periods, and these polymers adhere to the mucin/epithelial surface, leading to drug delivery.19 Recently; in the urological field, the application of a large variety of bioadhesive polymers such as chitosan, polycarbophil, and hydroxypropylcellulose (HPC) has been reported.38 For instance, Chiba et al39 demonstrated that the addition of 1.0% HPC effectively prolonged oxybutynin retention in the bladder compared to intravesical instillation of its solution. Among these bioadhesives, chitosan is a featured natural copolymer exhibiting various beneficial properties such as strong bioadhesion, controlled drug-releasing properties, and permeation-enhancing properties due to its cationic character and based on its primary amino groups.40
In contrast, in situ gelling liquids have recently been proved to be a convenient dosage form for application to body cavities, as they are easy to administer due to their lower viscosity values at room temperature. In addition, in response to environmental conditions such as pH, temperature, or ionic strength of the medium, these polymer solutions turn into a gel form and prolong the residence time at the application site.41 Plxs are one of the most well-known in situ triblock copolymers with thermoreversible behavior in aqueous media. They exhibit a “zigzag” configuration, transforming into a close-packed meander configuration, and they transform into a viscous gel with increasing temperature.42 Plx mixtures are often used as an alternative mucosal drug delivery platform due to their low toxicity, high solubilizing capacity, and excellent drug release characteristics.
In order to prolong the residence time in the bladder in the current study, the prepared chitosan–TGA NPs were suspended in the bioadhesive chitosan gel or in the Plx gel that exhibited in situ gelling properties. According to the literature and pre-formulation studies,18,43 chitosan of high molecular weight at a concentration of 2% was identified as the most suitable vehicle for intravesical administration of NPs, because significant increase in the work of mucoadhesion was observed as the molecular weight and viscosity of chitosan increased.
In another study completed by our research group,20 different Plx 407 and 188 combinations were evaluated according to their sol–gel transition temperature/time, and their mechanical, rheological, and bioadhesive properties. According to obtained results, a 20% Plx 407 and 10% Plx 188 mixture was identified as most appropriate in situ gelling system for mucosal administration.20 It was therefore chosen as the in situ carrier for Gem-HCl-loaded NPs and was evaluated for its suitability for intravesical administration.
Dilution of chitosan and Plx gels with artificial urine
The urine volume in a human bladder is generally 250–350 mL, differing with sexual, racial, and ethnic backgrounds.44 Due to incomplete emptying, a urine volume of nearly 50 mL generally residues even after voiding and it causes the dilution of drug concentration in bladder.45 Generally, intravesical chemotherapeutic drugs are applied in catheterized patients by installation of approximately 50 mL (range, 20–60 mL) of formulation. Therefore, in the current study, NP-loaded chitosan and Plx gel formulations were diluted with Tyrode solution were used as artificial urine in a 1:1 ratio to investigate the changes in their properties when they were mixed with urine in the bladder.
Characterization of gels
The NP-loaded chitosan and Plx gels were characterized in terms of their viscosity and Syringeability, and their rheological, mechanical, and bioadhesive properties, both at 25°C and 37°C. Characterization studies were also performed with blank gel formulations and dilutions with Tyrode solution for comparison.
Viscosity measurements
Viscosity affects many properties, such as ease of syringe-ability, spreadability, and hardness of semi-solid formulations. Therefore, viscosity of formulations was evaluated with a viscometer by vibrating at constant sine-wave vibration at the same frequency. Results are presented in Table 2 showing that the viscosity of chitosan gels significantly decreased with increasing temperature and that this decrease can be attributed to the increase in thermal motion of the polymer molecules.46 In other words, decrease in viscosity of chitosan gels was more pronounced at higher temperatures, and higher viscosities were observed at lower temperatures. In addition, incorporation of NPs into chitosan gels significantly decreased viscosity both at 25°C and 37°C.
Table 2.
Viscosity values of chitosan and Plx gels at 25°C and 37°C (n=6)
| Formulation | Viscosity [± SD (cP)]
|
|
|---|---|---|
| 25°C | 37°C | |
| Chitosan gel | 1,200±0 | 973.666±2.081 |
| NP-loaded chitosan gel | 841.333±2.516 | 736.333±2.516 |
| Chitosan gel-Tyrode solution | – | 102.666±0.577 |
| NP-loaded chitosan | – | 131.333±1.527 |
| gel-Tyrode solution | ||
| Plx gel | 636±0 | NA |
| NP-loaded Plx gel | 178.666±1.527 | 268±2.645 |
| Plx gel-Tyrode solution | – | 27.2±0.1 |
| NP-loaded Plx gel-Tyrode solution | – | 35±0.264 |
Note: –, no data.
Abbreviations: NP, nanoparticle; Plx, poloxamer; NA, not applicable; SD, standard deviation.
Viscosity of Plx gels increased at 37°C due to the thermo-gelling property of Plx molecules, as expected. At 37°C, the viscosity of blank Plx gel increased too much, and could not be measured with a vibration viscometer. On the other hand, this increase of viscosity with temperature was not so pronounced for NP-loaded Plx gel used in another study, as some additives can weaken hydrogen bonds of Plx molecules and can affect many properties, eg, by decreasing viscosity or by increasing gelation temperature/time.47 Finally, in the current study, the dilution with Tyrode solution caused significant loss of viscosity in all formulations used. Viscosities of chitosan gel, NP-loaded chitosan gel, and NP-loaded Plx gel were decreased 9.5-, 5.6-, and 7.65-fold, respectively.
Gelation temperature and time of Plx gels
Gelation temperature is the temperature at which the liquid phase turns into a gel. A suitable gelation temperature range for mucosal formulations is between 30°C–36°C.19 If the gelation temperature is high, the formulation remains in liquid form at physiological temperature. On the other hand, low gelation temperature causes the solution to become a gel at room temperature, which is in conflict with formulation requirements and may result in problems due to the viscous nature of the formulation.
In this context, gelation temperatures of Plx gel, NP-loaded Plx gel, and their dilutions with Tyrode solution were determined in the current study. The results showed that the gelation temperatures of Plx gel and NP-loaded Plx gel were 34.09°C±1.54°C and 37.86°C±0°C, respectively, and that these values were found to be suitable for intravesical administration. In contrast, the gelation temperatures of Plx gel-Tyrode solution and NP-loaded Plx gel-Tyrode solution were increased 1.5- and 1.4-fold, respectively, and were found to be 51.73°C±0.99°C and 53.66°C±1.85°C, respectively.
In addition, short gelation time was also advantageous to prevent the drainage and to prolong the retention of the formulation on the mucosal tissue. Therefore, the gelation times of Plx gel, NP-loaded Plx gel, Plx gel-Tyrode solution, and NP-loaded Plx gel-Tyrode solution were determined and were found to be 328±26 seconds, 288±0 seconds, 457±4 seconds, and 483±2 seconds, respectively. Similar to gelation temperatures, gelation times of Plx gel and NP-loaded Plx gel were increased 1.4- and 1.7-fold, respectively, when diluted with Tyrode solution. Results indicated that although Plx gel and NP-loaded Plx gel formulations were suitable carrier systems for intravesical administration, they showed significantly higher gelation temperatures and longer gelation times in the presence of Tyrode solution, and they lost their in situ gelling properties at body temperature.
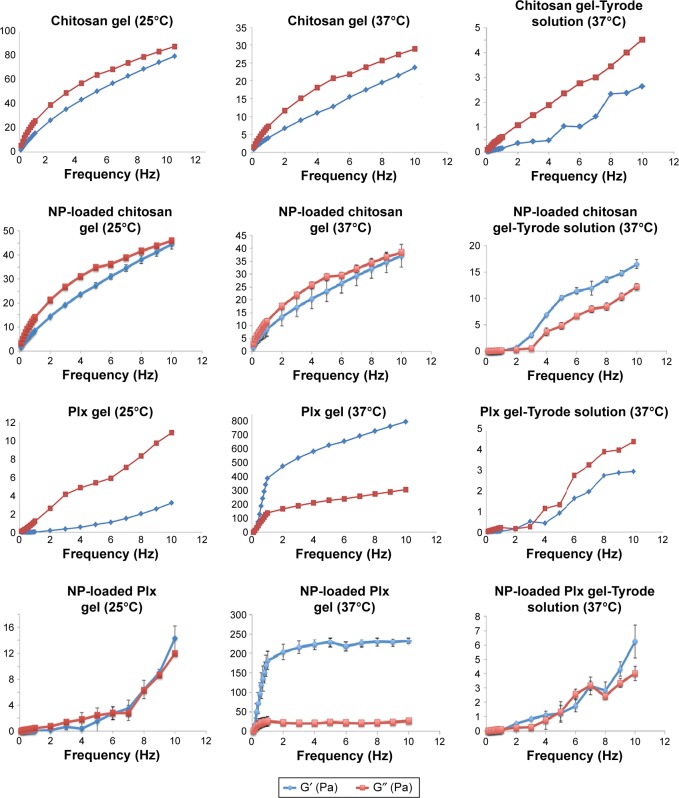
Rheological properties of formulations
The rheological properties of formulations were determined both at room temperature and at body temperature to observe any changes in gel structure. The obtained viscosity curves for chitosan formulations suggested that they behave as pseudoplastic fluids, showing decreasing viscosity with progressive increases in shear rate (data not shown). The increasing temperature and dilution with Tyrode solution also caused a significant decrease in viscosity of chitosan formulations, which exhibited the same flow type. As anticipated, each Plx formulation with or without NPs was a viscous liquid at room temperature (25°C), formed a semi-solid gel at body temperature (37°C), and returned to the liquid state when diluted with Tyrode solution (data not shown).
Furthermore, oscillatory rheological studies were performed to determine the viscoelastic properties of formulations by subjecting the samples to a sinusoidal shear stress.48 By using oscillatory rheology, it is possible to quantify both the elastic-like and viscous-like properties of formulations; it is thus a valuable tool for understanding the structural and dynamical properties of these systems. In oscillatory rheometry, the effects of oscillatory stresses on the viscoelastic properties are measured and two dynamic moduli are obtained: 1) the storage modulus (G′, a measure of the elasticity); and 2) the loss modulus (G″, representing viscous components at given frequency).49 A gel should exhibit a solid-like mechanical spectrum, that is, G′ > G″ throughout the experimentally accessible frequency range. In addition, frequency-independent behavior indicates a gel-like material, whereas the frequency dependence shows the viscous fluid.48
Figure 3 shows the plots of G′ and G″ as a function of frequency at two different temperature values. It was noticed that formulations prepared with chitosan exhibited viscoelastic properties and low gel strength. Mechanical spectra with frequency-dependence of G′ and G″ and smaller separation between the two moduli indicated that chitosan formulations could be considered as weak gels.50 As a result of increasing temperature, G′ and G″ values decreased, and this result was thought to be due to the relaxation of polymer chains. Moreover, addition of NPs caused nearly a two-fold decrease both in storage and in loss modulus.
Figure 3.
Frequency-dependent changes of the viscoelastic properties of chitosan versus Plx gels at 25°C and 37°C (n=6).
Note: G′ is the storage modulus and G″ is the loss modulus.
Abbreviations: NP, nanoparticle; Plx, poloxamer.
The elastic modulus (G′) of all Plx formulations was low at room temperature and rose significantly at body temperature. At 37°C, G′ dominated G″ for all frequency ranges, and the gap between the two moduli became wider, indicating stronger gel strength. Addition of NPs decreased G′ and G″ of the formulations compared to the blank gel. Only the NP-loaded Plx gel was found to be frequency-independent, exhibiting an elastic structure (strong gel, G′ >> G″) at 37°C. Finally, the rheological behavior of chitosan and Plx formulations mixed with Tyrode solution was evaluated, and liquid–solid behavior of macromolecular solutions was observed for all diluted gels.
Mechanical properties of formulations
Formulations intended for intravesical administration should have suitable properties for easy administration and patient compliance, such as acceptable hardness, easy removal from the container, high spreadability in the bladder, and high bioadhesion. Texture profile analyses (TPA) allow evaluation of the mechanical properties of semi-solid formulations and provide information about the physical gel structure under different environmental and physiological conditions.23 Therefore, TPA analyses were performed with formulations at 25°C and 37°C, and results are presented in Table 3.
Table 3.
Mechanical properties of chitosan and Plx gels at 25°C and 37°C (n=6)
| Formulation | Hardness (N) ± SD | Compressibility (N·sec) ± SD | Adhesiveness (N·sec) ± SD | Cohesiveness ± SD | Elasticity ± SD |
|---|---|---|---|---|---|
| Chitosan gel | |||||
| 25°C | 0.044±0.002 | 0.132±0.007 | 0.121±0.028 | 1.008±0.024 | 0.896±0.112 |
| 37°C | 0.018±0.002 | 0.075±0.011 | 0.119±0.039 | 1.016±0.005 | 1.041±0.037 |
| NP-loaded chitosan gel | |||||
| 25°C | 0.036±0.002 | 0.120±0.004 | 0.106±0.005 | 0.988±0.012 | 0.995±0.017 |
| 37°C | 0.011±0 | 0.018±0.001 | 0.054±0.007 | 1.058±0.101 | 0.944±0.031 |
| Chitosan gel-Tyrode solution | |||||
| 37°C | 0.006±0.001 | 0.011±0.002 | 0.007±0.001 | 0.987±0.012 | 0.999±0.207 |
| NP-loaded chitosan gel-Tyrode solution | |||||
| 37°C | 0.008±0 | 0.018±0.001 | 0.007±0 | 1.000±0 | 0.987±0.048 |
| Plx gel | |||||
| 25°C | 0.018±0 | 0.114±0.003 | 0.006±0.001 | 1.058±0.027 | 0.951±0.021 |
| 37°C | 0.189±0.009 | 0.355±0.019 | 0.297±0.017 | 1.008±0.005 | 0.905±0.017 |
| NP-loaded Plx gel | |||||
| 25°C | 0.013±0 | 0.064±0.004 | 0.005±0.001 | 1.032±0.056 | 0.966±0.014 |
| 37°C | 0.111±0.009 | 0.193±0.044 | 0.104±0.008 | 1.096±0.224 | 0.997±0.089 |
| Plx gel-Tyrode solution | |||||
| 37°C | 0.005±0 | 0.006±0.001 | 0.004±0 | 1.025±0.051 | 0.974±0.084 |
| NP-loaded Plx gel-Tyrode solution | |||||
| 37°C | 0.007±0 | 0.028±0 | 0.004±0 | 1.033±0.027 | 0.982±0.079 |
Abbreviations: NP, nanoparticle; Plx, poloxamer; SD, standard deviation.
Briefly, hardness value expresses the applicability of the gel to the desired site. It should be low to easily administer and to spread the formulation over the bladder mucosa. Compressibility value determines sample deformation under compression. This value should be low to easily remove the formulation from the catheter during administration and to provide high spreadability at the application site. Adhesiveness is defined as the work required to detach the probe from the sample, a process in which its cohesive bonds are broken; adhesiveness is related to bioadhesion. Elasticity value represents the rate at which the deformed sample returns to its undeformed condition. Lower numerical value in the elasticity mode indicates a greater product elasticity. Finally, cohesiveness shows the effect of repeated shearing stresses on the structural properties of the formulations.23,24
It can be seen from Table 3 that, depending on the increase in temperature, hardness and compressibility values of chitosan gels significantly decreased in the current study. This decrease was in accordance with rheological evaluation results, and it was thought to be associated with the thermal motion of the polymer molecules. No significant change was observed regarding the other three parameters, ie, temperature-dependent adhesiveness, cohesiveness, and elasticity of chitosan gels.
In contrast, it was observed that the gel structure of Plx gels strengthened and that mechanical properties were improved with the increase in temperature. Blank and NP-loaded Plx gels at 37°C exhibited the greatest hardness and compressibility values, corroborating the results obtained by oscillatory rheology, ie, that increased elastic behavior (represented by G′) was exhibited. Higher adhesiveness value could imply greater adhesion at the tissue surface, which is a desirable characteristic required to increase drug retention time.50,51 Based on the results, it appeared that NP-loaded Plx gels at 37°C could confer these desirable hardness properties, and further in vitro bioadhesion tests were performed in order to confirm initial results. The addition of NPs or the presence of Tyrode solution significantly weakened the mechanical properties of both chitosan and Plx gels, and by dilution with Tyrode solution, the most pronounced decrease was seen in the case of Plx gels.
Syringeability of formulations
Syringeability can be considered to be the ability of a formulation to be successfully administered by a syringe and appropriate catheter. Successful intravesical administration and comfortable receipt in the bladder rely on the ease of formulation syringeability. Therefore, formulation syringe-ability was tested at 25°C to optimize usability and patient comfort.
The work required to expel chitosan gel, NP-loaded chitosan gel, Plx gel, and NP-loaded Plx gel from a syringe combined with a catheter was found to be 130.1±2.9 N·mm, 82.8±0.8 N·mm, 99.8±1.5 N·mm, and 30.7±1.4 N·mm, respectively. The results showed that the syringeability values of all formulations are suitable for intravesical administration with a catheter. Previously, Jones et al52 reported that increased product viscosity leads to an increase in resistance of product deformation and to an increase in work required for compression/expulsion of the formulation from a syringe. In the current study, the highest syringe-ability value was required for the chitosan gel; chitosan gel viscosity was highest among all formulations at 25°C. In addition, significant decreases in syringeability values were observed when the chitosan and Plx gels were loaded with NPs.
Bioadhesive properties of formulations
Bioadhesive properties are essential in order to prolong the residence time of formulations in the bladder. Bioadhesion studies were therefore performed with TPA on freshly excised bovine bladder mucosa.
As a result of the current study, force–distance graphs were obtained, and the peak value of this graph corresponded to the “detachment force”, while AUC represented “bioadhesion”. In other words, the detachment force is the maximum force required to overcome the adhesive bonds between the formulations and bladder mucosa. On the other hand, bioadhesion corresponded not only to the maximum force but also to the detachment of all established bonds, and provided a wider evaluation of bioadhesive properties.53 Therefore, it was decided to evaluate bioadhesive properties of the chitosan and Plx gels by using bioadhesion values.
As can be seen from Table 4, chitosan gels came into prominence with their higher bioadhesive properties, especially when NPs were added or gels were diluted with Tyrode solution. The addition of NPs caused only a 13% decrease in bioadhesion of chitosan gels, whereas the bioadhesion of Plx gels decreased by 43%. Similarly, dilution with Tyrode solution caused a decrease of 51% and 80% in bioadhesion of NP-loaded chitosan and Plx gels, respectively. The well-known bioadhesive property of chitosan gels is based on its cationic character, because ionic interactions between the cationic primary amino groups of chitosan and the anionic substructures of mucus occur.40 Accordingly, chitosan was proposed as a promising bioadhesive polymer for hydrophilic drugs such as Gem-HCl, as it was shown to maintain its bioadhesive properties on isolated porcine urinary bladder after having been fully hydrated.35
Table 4.
Bioadhesion values and detachment forces of chitosan and Plx gels (n=6)
| Formulation | Bioadhesion mN.mm ± SD | Detachment force (mN) ± SD |
|---|---|---|
| Chitosan gel | 2,066.18±236.34 | 673.57±83.99 |
| NP-loaded chitosan gel | 1,795.901±42.771 | 1,684.092±123.612 |
| Chitosan gel-Tyrode solution | 1,406.736±39.712 | 512.834±60.238 |
| NP-loaded chitosan gel-Tyrode solution | 1,003.622±48.189 | 462.074±33.617 |
| Plx gel | 1,951.74±186.17 | 840.63±150.93 |
| NP-loaded Plx gel | 1,103.670±81.016 | 975.559±3.315 |
| Plx gel-Tyrode solution | 1,072.62±51.76 | 346.33±52.83 |
| NP-loaded Plx gel-Tyrode solution | 378.234±22.462 | 423.760±48.509 |
Abbreviations: NP, nanoparticle; Plx, poloxamer; SD, standard deviation.
In vitro release studies
In the present study, the in vitro release profiles of Gem-HCl were evaluated in phosphate buffer pH 6.5 at 37°C, and results are displayed in Figure 4A. Gem-HCl release from solution reached 100% within 150 minutes. Among the NP and NP-loaded gel formulations, the highest release rate was obtained for chitosan–TGA NPs, and the ranking of release rates was: 1) Gem-HCl solution > 2) chitosan–TGA NPs > 3) NP-loaded chitosan gel > 4) NP-loaded Plx gel. The released percentage of Gem-HCl from chitosan–TGA NPs, NP-loaded chitosan gel, and NP-loaded Plx gel reached 51.0%±3.7%, 33.4%±5.0%, and 19.6%±1.6%, respectively, within 4 hours. In addition, the release was continued up to 24 hours, and no significant change was observed in release rates at the end of 24 hours (data not shown).
Figure 4.
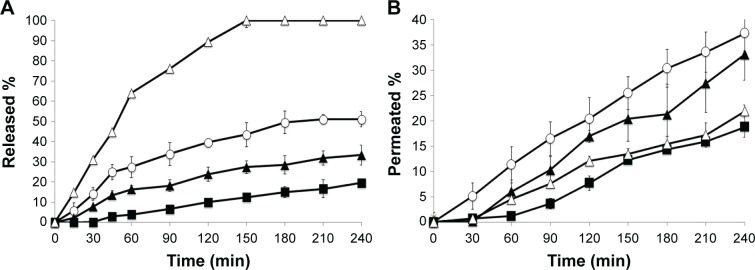
In vitro release (A) and ex vivo permeation (B) profiles of Gem-HCl from NPs and NP-loaded chitosan and Plx gels (n=6).
Notes: ∆, Gem-HCl solution; ○ Chitosan–TGA NPs; ▲, NP-loaded chitosan gel; ■, NP-loaded Plx gel. The error bars at some timepoints cannot be seen because they are smaller than the markers.
Abbreviations: Gem-HCl, gemcitabine hydrochloride; NP, nanoparticle; TGA, thioglycolic acid; Plx, poloxamer; min, minutes.
The release profile of Gem-HCl from the covalently crosslinked chitosan–TGA NPs was significantly lower in comparison to Gem-HCl solution. Covalent crosslinking hardens the particles and leads to differences in the release rate. Additionally, it provides increased resistance for penetration of artificial urine into the NP. Therefore, the diffusivity of Gem-HCl through the matrix material is lowered and allows a continuous release.12 A similar release profile for Gem-HCl loaded NPs have been obtained in a study by Derakhshandeh and Fathi.54 They observed that Gem-HCl-loaded chitosan NPs show a controlled release pattern, and approximately 45% of Gem-HCl is released from NPs during the first 4 hours, followed by continuous release.
Surprisingly, although the viscosity of NP-loaded chitosan gel is higher than Plx gel at 37°C, Gem-HCl release from chitosan gel was found to be faster than from the Plx gel. This result may be explained by the interpenetration of chitosan and TPP contents of the NPs into the Plx gel network. Similarly, in a study of Ur-Rehman et al55 the gel network formed by chitosan in the presence of TPP interpenetrated into the network of the Plx 407 gel, and this decreased the rate at which water penetrated into the Plx 407 gel, thereby delaying the unpacking of the Plx micelles and subsequent dissolution from the gel.55
In addition, the results of the current study showed that incorporation of NPs into chitosan and Plx gels significantly decreased the release rate by 1.5- and 2.6-fold, respectively. It is clear that the slow release of Gem-HCl from NP-loaded gels is exclusively based on the obstruction effect of the gel matrix due to less and narrower aqueous channels, and hence, a longer and more viscous diffusion path.56
Sustained release of intravesically administered drugs ensures continuous presence of drug in the bladder, without the need for intermittent catheterization, and it increases drug efficacy with the prolonged duration of direct contact between the drug and the abnormal urothelium.57 Although NPs and NP-loaded gel formulations showed significantly different release rates in the present study, a sustained release was obtained for all formulations during 4 hours, likely providing constant drug concentration without any peaks or troughs.
Ex vivo permeation studies
The potential permeation profiles of the formulations were determined on freshly excised bovine bladder mucosa, and the results are shown as a function of time in Figure 4B. In contrast to release profiles, when the permeation profiles of formulations were investigated, it was observed that the permeated ratio of Gem-HCl from chitosan–TGA NPs was even higher than Gem-HCl solution, and the least permeated amount was observed with NP-loaded Plx gels. The permeated percentage of Gem-HCl within 4 hours for Gem-HCl solution, chitosan–TGA NPs, NP-loaded chitosan gel, and NP-loaded Plx gel reached 21.96%±1.20%, 37.32%±3.48%, 33.16%±5.11%, and 18.78%±1.97%, respectively. This result might be explained by the permeation-enhancing effect of chitosan due to its ability to increase the paracellular route of absorption, which is important for the transport of hydrophilic compounds across the membrane. The underlying mechanism for this permeation-enhancing effect of chitosan seems to be based on its positive charge, which interacts with the negatively charged cell membrane and affects the tight junctions of umbrella cells.13 In addition, in the current study, this permeation-enhancing effect of chitosan was much more pronounced by the immobilization of thiol groups on the polymeric backbone. This improved effect of thiomers seems to be based on the inhibition of protein tyrosine phosphatase enzyme, which is involved in the opening process of tight junctions.58 Furthermore, thiomers attach on the mucosa for a comparatively more prolonged period of time as a result of improved bioadhesive properties, due to disulfide bond formation, with cysteine-rich subdomains of mucus glycoproteins favoring the opening of tight junctions and increasing paracellular transport.58
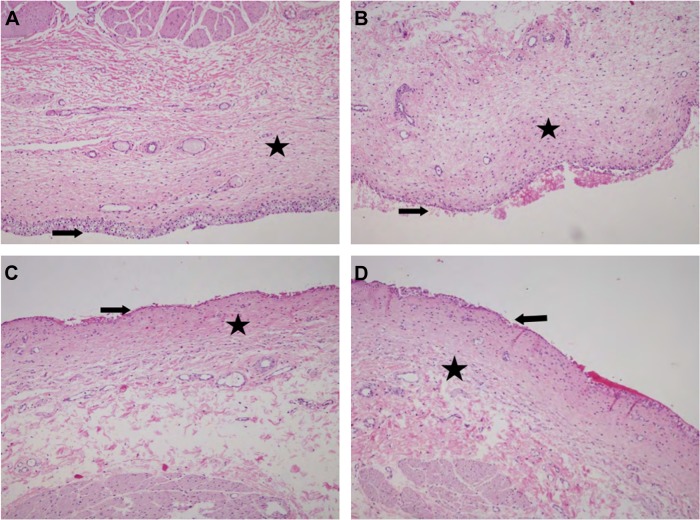
Histopathological evaluation
The results of the histopathological evaluation of the bladder mucosa are shown in Figure 5; they suggest that NPs, NP-loaded chitosan, and Plx gels do not cause any damage to healthy bladder mucosa. The formulations might therefore be regarded as safe.
Figure 5.
Microscopic images of bovine bladder mucosa.
Notes: Healthy bladder mucosa (A); bladder mucosa treated with chitosan–TGA NPs (B); bladder mucosa treated with NP-loaded chitosan gel (C); bladder mucosa treated with NP-loaded Plx gel (D). ➔, urothelium, and ★, lamina propria. H&E staining; magnification ×40.
Abbreviations: TGA, thioglycolic acid; NP, nanoparticle; Gem-HCl, gemcitabine hydrochloride; Plx, poloxamer; H&E, hematoxylin eosin.
Conclusion
Direct instillation of drugs into bladder is an efficient alternative to systemic delivery, since it reduces side effects, prevents first-pass effects, and consequently allows a more effective treatment. However, this method is limited by an excessive drug loss during voiding. To increase the residence time of drugs in the bladder and to achieve a more effective intravesi-cal treatment, chitosan–TGA NPs were prepared in the present study. The obtained results revealed that NPs composed of chitosan–TGA can be efficiently obtained by an ionotropic gelation process, and the resulting NPs showed suitable properties for intravesical administration of Gem-HCl.
Both chitosan and Plx gels might be alternative carriers for intravesical administration of Gem-HCl-loaded NPs to increase the residence time in the bladder, and subsequently, the efficacy of treatment. However, in the present study, when the gel formulations were diluted with artificial urine to mimic the conditions in bladder, Plx gels lost their in situ gelling properties at body temperature. To overcome this problem, strategies such as emptying the bladder before drug instillation, suppression of rate of urine production by the kidneys, and regulation of fluid intake before and after drug administration are recommended.
Collectively, the obtained data suggested the possibility of using both NPs and NP-dispersed chitosan gels for intravesical administration of Gem-HCl. It was also concluded that future studies, such as cell culture studies and evaluation of in vivo efficiency, are needed to determine in vivo safety and efficacy of NPs and NP-loaded chitosan gel formulations.
Acknowledgments
This study was supported by The Scientific and Technological Research Council of Turkey (grant number TUBITAK-112/S/293). The authors would also like to thank to the TR Prime Ministry State Planning Organization Foundation (Project Number 09/DPT/001).
Footnotes
Disclosure
The authors report no conflicts of interest in this work.
References
- 1.Mattioli F, Curoto A, Manfredi V, et al. Intravesical gemcitabine in superficial bladder cancer: a phase II safety, efficacy and pharmacokinetic study. Anticancer Res. 2005;25:2493–2496. [PubMed] [Google Scholar]
- 2.Hadaschik BA, ter Borg MG, Jackson J, et al. Paclitaxel and cisplatin as intravesical agents against non-muscle-invasive bladder cancer. BJU Int. 2008;101:1347–1355. doi: 10.1111/j.1464-410X.2008.07571.x. [DOI] [PubMed] [Google Scholar]
- 3.Wientjes MG, Dalton JT, Badalement RA, Drago JR, Au JL. Bladder Wall penetration of intravesical mitomycin C in dogs. Cancer Res. 1991;51:4347–4354. [PubMed] [Google Scholar]
- 4.Burjak M, Bogataj M, Velnar M, Grabnar I, Mrhar A. The study of drug release from microspheres adhered on pig vesical mucosa. Int J Pharm. 2001;224:123–130. doi: 10.1016/s0378-5173(01)00748-7. [DOI] [PubMed] [Google Scholar]
- 5.GuhaSarkar S, Banerjee R. Intravesical drug delivery: challenges, current status, opportunities and novel strategies. J Control Release. 2010;148:147–159. doi: 10.1016/j.jconrel.2010.08.031. [DOI] [PubMed] [Google Scholar]
- 6.Gontero P, Tizzani A. Intravesical Gemcitabine: state of the Art. Eur Urol. 2007;6:809–815. [Google Scholar]
- 7.Witjes JA, Vriesema JL, van der Heijden AG, Peters JA, Schalken JA. Pharmacokinetics of intravesical gemcitabine: a preclinical study in pigs. Eur Urol. 2003;44:615–619. doi: 10.1016/s0302-2838(03)00372-5. [DOI] [PubMed] [Google Scholar]
- 8.Witjes JA, van der Heijden AG, Vriesema JL, Peters GJ, Laan A, Schalken JA. Intravesical gemcitabine: a phase 1 and pharmacokinetic study. Eur Urol. 2004;45:182–186. doi: 10.1016/j.eururo.2003.09.014. [DOI] [PubMed] [Google Scholar]
- 9.Le Visage C, Rioux-Leclercq N, Haller M, Breton P, Malavaud B, Leong K. Efficacy of paclitaxel released from bio-adhesive polymer microspheres on model superficial bladder cancer. J Urol. 2004;171:1324–1329. doi: 10.1097/01.ju.0000103922.12319.59. [DOI] [PubMed] [Google Scholar]
- 10.Bogataj N, Mrhar A, Korosec A. Influence of physicochemical and biological parameters on drug release from microspheres adhered on vesical and intestinal mucosa. Int J Pharm. 1999;177:211–220. doi: 10.1016/s0378-5173(98)00341-x. [DOI] [PubMed] [Google Scholar]
- 11.Lu Z, Yeh TK, Tsai M, Au JL, Wientjes MG. Paclitaxel-loaded gelatin nanoparticles for intravesical bladder cancer therapy. Clin Cancer Res. 2004;10:7677–7684. doi: 10.1158/1078-0432.CCR-04-1443. [DOI] [PubMed] [Google Scholar]
- 12.Barthelmes J, Perera G, Hombach J, Dünnhaupt S, Bernkop-Schnürch A. Development of a mucoadhesive nanoparticulate drug delivery system for a targeted drug release in the bladder. Int J Pharm. 2011;416:339–345. doi: 10.1016/j.ijpharm.2011.06.033. [DOI] [PubMed] [Google Scholar]
- 13.Dünnhaupt S, Barthelmes J, Rahmat DK, et al. S-protected thiolated chitosan for oral delivery of hydrophilic macromolecules: evaluation of permeation enhancing and efflux pump inhibitory properties. Mol Pharmaceutics. 2012;9:1331–1341. doi: 10.1021/mp200598j. [DOI] [PubMed] [Google Scholar]
- 14.Calvo P, Remunan-Lopez C, Vila-Jato J, Alonso MJ. Novel hydrophilic chitosan polyethylene oxide nanoparticles as protein carriers. J Appl Polym Sci. 1997;63:125–132. [Google Scholar]
- 15.Bilensoy E, Sarisozen C, Esendağli G, et al. Intravesical cationic nanoparticles of chitosan and polycaprolactone for the delivery of Mitomycin C to bladder tumors. Int J Pharm. 2009;371:170–176. doi: 10.1016/j.ijpharm.2008.12.015. [DOI] [PubMed] [Google Scholar]
- 16.Sadiq AA, Abdul Rassol AA. Formulation and evaluation of silibinin loaded solid lipid nanoparticles peroral use targeting lower part of gastrointestinal tract. Int J Pharm Pharm Sci. 2014;6:56–67. [Google Scholar]
- 17.Şenyiğit T, Sonvico F, Barbieri S, Ozer O, Santi P, Colombo P. Lecithin/chitosan nanoparticles of clobetasol-17-propionate capable of accumulation in pig skin. J Control Release. 2010;142:368–373. doi: 10.1016/j.jconrel.2009.11.013. [DOI] [PubMed] [Google Scholar]
- 18.Şenyiğit ZA, Karavana SY, Eraç B, Gürsel O, Limoncu MH, Baloğlu E. Evaluation of chitosan based vaginal bioadhesive gel formulations for antifungal drugs. Acta Pharm. 2014;64:139–156. doi: 10.2478/acph-2014-0013. [DOI] [PubMed] [Google Scholar]
- 19.Choi HG, Oh YK, Kim CK. In-situ gelling and mucoadhesive liquid suppository containing acetaminophen: enhanced bioavailability. Int J Pharm. 1998;165:23–32. [Google Scholar]
- 20.Baloglu E, Karavana SY, Şenyiğit ZA, Guneri T. Rheological and mechanical properties of poloxamer mixtures as a mucoadhesive gel base. Pharm Dev Technol. 2011;16:627–636. doi: 10.3109/10837450.2010.508074. [DOI] [PubMed] [Google Scholar]
- 21.Chutipongtanate S, Thongboonkerd V. Systemic comparisons of artificial urine formulas for in vitro cellular study. Anal Biochem. 2010;402:110–112. doi: 10.1016/j.ab.2010.03.031. [DOI] [PubMed] [Google Scholar]
- 22.Karavana SY, Rençber S, Şenyiğit ZA, Baloğlu E. A new in-situ gel formulation of Itraconazole for vaginal administration. Pharmacol Pharm. 2012;3:417–426. [Google Scholar]
- 23.Jones DS, Woolfson AD, Brown AF. Textural, viscoelastic and mucoadhesive properties of pharmaceutical gels composed of cellulose polymers. Int J Pharm. 1997;151:223–233. [Google Scholar]
- 24.Jones DS, Woolfson AD, Brown AF. Textural analysis and flow rhe-ometry of novel, bioadhesive antimicrobial oral gels. Pharm Res. 1997;14:450–457. doi: 10.1023/a:1012091231023. [DOI] [PubMed] [Google Scholar]
- 25.Andrews GP, Gorman SP, Jones DS. Rheological characterisation of primary and binary interactive bioadhesive gels composed of cellulose derivatives designed as ophthalmic viscosurgical devices. Biomaterials. 2005;26:571–580. doi: 10.1016/j.biomaterials.2004.02.062. [DOI] [PubMed] [Google Scholar]
- 26.Andrews GP, Jones DS. Rheological characterization of bioadhesive binary polymeric systems designed as platforms for drug delivery implants. Biomacromolecules. 2006;7:899–906. doi: 10.1021/bm050620y. [DOI] [PubMed] [Google Scholar]
- 27.Jones DS, Woolfson AD, Djokic J. Texture profile analysis of bioadhe-sive polymeric semisolids: mechanical characterization and investigation of interactions between formulation components. J Appl Polym Sci Symp. 1996;61:2229–2234. [Google Scholar]
- 28.Jones DS, Woolfson AD, Brown AF, Coulter WA, McClelland C, Irwin CR. Design, characterisation and preliminary clinical evaluation of a novel mucoadhesive topical formulation containing tetracycline for the treatment of periodontal disease. J Control Release. 2000;67:357–368. doi: 10.1016/s0168-3659(00)00231-5. [DOI] [PubMed] [Google Scholar]
- 29.Baloglu E, Karavana SY, Şenyiğit ZA, et al. In-situ gel formulations of econazole nitrate: preparation and in-vitro and in-vivo evaluation. J Pharm Pharmacol. 2011;63:1274–1282. doi: 10.1111/j.2042-7158.2011.01315.x. [DOI] [PubMed] [Google Scholar]
- 30.Gomez P, 3rd, Gil ES, Lovett ML, et al. The effect of manipulation of silk scaffold fabrication parameters on matrix performance in a murine model of bladder augmentation. Biomaterials. 2011;32:7562–7570. doi: 10.1016/j.biomaterials.2011.06.067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Gontero P, Casetta G, Maso G, et al. Phase II study to investigate the ablative efficacy of intravesical administration of gemcitabine in intermediate-risk superficial bladder cancer (SBC) Eur Urol. 2004;46:339–343. doi: 10.1016/j.eururo.2004.05.001. [DOI] [PubMed] [Google Scholar]
- 32.Stadler WM, Kuzel T, Roth B, Raghavan D, Dorr FA. Phase II study of single-agent gemcitabine in previously untreated patients with metastatic urothelial cancer. J Clin Oncol. 1997;15:3394–3398. doi: 10.1200/JCO.1997.15.11.3394. [DOI] [PubMed] [Google Scholar]
- 33.Leitner VM, Walker GF, Bernkop-Schnürch A. Thiolated polymers: evidence for the formation of disulphide bonds with mucus glycopro-teins. Eur J Pharm Biopharm. 2003;56:207–214. doi: 10.1016/s0939-6411(03)00061-4. [DOI] [PubMed] [Google Scholar]
- 34.Liu C, Chang L, Lin K, et al. Preparatrion and characterization of gelatin-based mucoadhesive nanocomposites as intravesical gene delivery scaffolds. Biomed Res Int. 2014;2014:473823. doi: 10.1155/2014/473823. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Butte K, Monin M, Kurhade S, Kar S. Intravesical drug delivery system for bladder: An overview. IJPCBS. 2013;3:680–691. [Google Scholar]
- 36.Müller RH, Jacobs C, Kayser O. Nanosuspensions as particulate drug formulations in therapy Rationale for development and what we can expect for the future. Adv Drug Deliv Rev. 2001;47:3–19. doi: 10.1016/s0169-409x(00)00118-6. [DOI] [PubMed] [Google Scholar]
- 37.Govender T, Stolnis S, Garnett MC, Illum L, Davis SS. PLGA nanopar-ticles prepared by nanoprecipitation: drug loading and release studies of a water soluble drug. J Control Release. 1999;57:171–185. doi: 10.1016/s0168-3659(98)00116-3. [DOI] [PubMed] [Google Scholar]
- 38.Hanava T, Tsuchiya C, Endo N, et al. Formulation study of intravesical oxybutynin installation solution with enhanced retention in bladder. Chem Pharm Bull (Tokyo) 2008;56:1073–1076. doi: 10.1248/cpb.56.1073. [DOI] [PubMed] [Google Scholar]
- 39.Chiba K, Ogawa S, Hayase N, et al. Preparation and evaluation of prolonged-action oxybutynin hydrochloride solution for intravesical instillation therapy. Jpn J Hosp Pharm. 1997;23:297–307. Japanese [with English abstract] [Google Scholar]
- 40.Bernkop-Schnürch A, Dünnhaupt S. Chitosan-based drug delivery systems. Eur J Pharm Biopharm. 2012;81:463–469. doi: 10.1016/j.ejpb.2012.04.007. [DOI] [PubMed] [Google Scholar]
- 41.Peppas NA. Physiologically responsive gels. J Bioact Compat Polym. 1991;6:241–246. [Google Scholar]
- 42.Kramaric A, Resman A, Kofler B, Zmitek J, inventors. LEK Consulting, assignee Thermoreversible gel as a liquid pharmaceutical carrier for a galenic formulation. 0551626 (A1) European Patent EU. 1992 Dec 16;
- 43.Yellanki SK, Nerella NK, Goranti S, Deb SK. Development of metron-idazole intra-vaginal gel for the treatment of bacterial vaginosis: effect of mucoadhesive natural polymers on the release of metronidazole. Int J Pharm Tech Res. 2010;2:1746–1750. [Google Scholar]
- 44.Gray M. Traces: making sense of urodynamics testing – part 5: evaluation of bladder filling/storage functions. Urol Nurs. 2011;31:149–153. [PubMed] [Google Scholar]
- 45.Grabnar I, Bogataj M, Belic A, Logar V, Karba R, Mrhar A. Kinetic model of drug distribution in the urinary bladder wall following intra-vesical instillation. Int J Pharm. 2006;322:52–59. doi: 10.1016/j.ijpharm.2006.05.026. [DOI] [PubMed] [Google Scholar]
- 46.El-Hefian EA, Elgannoudi ES, Mainal A, Yahaya AH. Characterization of chitosan in acetic acid: rheological and thermal studies. Turk J Chem. 2010;34:47–56. [Google Scholar]
- 47.Yong CS, Choi JS, Quan Q, et al. Effect of sodium chloride on the release, absorption and safety of diclofenac sodium delivered by poloxamer gel. Int J Pharm. 2001;263:195–205. doi: 10.1016/s0378-5173(03)00362-4. [DOI] [PubMed] [Google Scholar]
- 48.Dumortier G, Grossiord JL, Zuber M, Couarraze G, Chaumeil JC. Rheological study of a thermoreversible morphine gel. Drug Dev Ind Pharm. 1991;17:1255–1265. [Google Scholar]
- 49.Ross-Murphy SB. Physical Techniques for the Study of Food Biopolymers. London: Blackie Academic & Professional; 1994. Rheological methods; pp. 343–392. [Google Scholar]
- 50.Ström A, Schuster E, Goh SM. Rheological characterization of acid pectin samples in the absence and presence of monovalent ions. Carbohydr Polym. 2014;113:336–343. doi: 10.1016/j.carbpol.2014.06.090. [DOI] [PubMed] [Google Scholar]
- 51.Cevher E, Sensoy D, Taha MA, Araman A. Effect of thiolated polymers to textural and mucoadhesive properties of vaginal gel formulations prepared with polycarbophil and chitosan. AAPS Pharm Sci Tech. 2008;9:953–965. doi: 10.1208/s12249-008-9132-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Jones DS, Woolfson AD, Brown AF, O’Neill MJ. Mucoadhesive, syringeable drug delivery systems for controlled application of metronidazole to the periodontal pocket: in vitro release kinetics, syringeability, mechanical and mucoadhesive properties. J Control Release. 1997;49:71–79. [Google Scholar]
- 53.das Neves J, Amaral MH, Bahia MF. Performance of an in vitro mucoadhesion testing method for vaginal semisolids: influence of different testing conditions and instrumental parameters. Eur J Pharm Biopharm. 2008;69:622–632. doi: 10.1016/j.ejpb.2007.12.007. [DOI] [PubMed] [Google Scholar]
- 54.Derakhshandeh K, Fathi S. Role of chitosan nanoparticles in the oral absorption of Gemcitabine. Int J Pharm. 2012;437(1–2):172–177. doi: 10.1016/j.ijpharm.2012.08.008. [DOI] [PubMed] [Google Scholar]
- 55.Ur-Rehman T, Tavelin S, Gröbner G. Chitosan in situ gelation for improved drug loading and retention in poloxamer 407 gels. Int J Pharm. 2011;409:19–29. doi: 10.1016/j.ijpharm.2011.02.017. [DOI] [PubMed] [Google Scholar]
- 56.Peng Q, Sun T, Gong T, et al. Injectable and biodegradable thermosen-sitive hydrogels loaded with PHBHHx nanoparticles for the sustained and controlled release of insulin. Acta Biomater. 2013;9:5063–5069. doi: 10.1016/j.actbio.2012.09.034. [DOI] [PubMed] [Google Scholar]
- 57.Tyagi P, Tyagi S, Kaufman J, Huang L, de Miguel F. Local drug delivery to bladder using technology innovations. Urol Clin North Am. 2006;33:519–530. doi: 10.1016/j.ucl.2006.06.012. [DOI] [PubMed] [Google Scholar]
- 58.Clausen A, Kast CE, Bernkop-Schnürch A. The role of glutathione in the permeation enhancing effect of thiolated polymers. Pharm Res. 2002;19:602–608. doi: 10.1023/a:1015345827091. [DOI] [PubMed] [Google Scholar]