Abstract
Background
The Advisory Committee on Immunization Practice of Thailand prioritizes seasonal influenza vaccinations for populations who are at highest risk for serious complications (pregnant women, children 6 months–2 years, persons ≥65 years, persons with chronic diseases, obese persons), and health-care personnel and poultry cullers. The Thailand government purchases seasonal influenza vaccine for these groups. We assessed vaccination coverage among high-risk groups in Thailand from 2010 to 2012.
Methods
National records on persons who received publicly purchased vaccines from 2010 to 2012 were analyzed by high-risk category. Denominator data from multiple sources were compared to calculate coverage. Vaccine coverage was defined as the proportion of individuals in each category who received the vaccine. Vaccine wastage was defined as the proportion of publicly purchased vaccines that were not used.
Results
From 2010 to 2012, 8.18 million influenza vaccines were publicly purchased (range, 2.37–3.29 million doses/year), and vaccine purchases increased 39% over these years. Vaccine wastage was 9.5%. Approximately 5.7 million (77%) vaccine doses were administered to persons ≥65 years and persons with chronic diseases, 1.4 million (19%) to healthcare personnel/poultry cullers, 82,570 (1.1%) to children 6 months–2 years, 78,885 (1.1%) to obese persons, 26,481 (0.4%) to mentally disabled persons, and 17,787 (0.2%) to pregnant women. Between 2010 and 2012, coverage increased among persons with chronic diseases (8.6% versus 14%; p < 0.01) and persons ≥65 years (12%, versus 20%; p < 0.01); however, coverage decreased for mentally disabled persons (6.1% versus 4.9%; p < 0.01), children 6 months–2 years (2.3% versus 0.9%; p < 0.01), pregnant women (1.1% versus 0.9%; p < 0.01), and obese persons (0.2% versus 0.1%; p < 0.01).
Conclusions
From 2010 to 2012, the availability of publicly purchased vaccines increased. While coverage remained low for all target groups, coverage was highest among persons ≥65 years and persons with chronic diseases. Annual coverage assessments are necessary to promote higher coverage among high-risk groups in Thailand.
Keywords: Influenza, Vaccination, Influenza vaccine, Thailand
1. Introduction
Influenza is an acute, vaccine-preventable infection that annually leads to an estimated 3–5 million severe illness episodes and approximately 500,000 deaths globally [1,2]. Influenza vaccination is the most effective way to prevent influenza virus infection. The World Health Organization (WHO) recommends vaccinating those most at risk for serious complications, including young children, the elderly, those with chronic illnesses, and pregnant women [2]. Vaccination is also recommended for those who easily transmit influenza to high-risk populations (i.e., healthcare personnel) [3,4].
Although influenza vaccine is not commonly used in most countries in Southeast Asia, the burden of influenza in Southeast Asia is similar to that in other parts of the world where influenza vaccine is now routinely used [5–7]. In Thailand from 2005 to 2008, the annual incidence of influenza in young children <5 years was 236 per 100,000 and in persons aged ≥75 was 375 per 100,000 [8].
In Thailand, seasonal vaccination was first used in the public sector in 2004 to vaccinate healthcare personnel and poultry cullers in response to avian influenza A (H5N1), and its use in pandemic preparedness efforts was articulated in Thailand’s 1st National Strategy Plan for Pandemic Influenza Preparedness [9]. Currently, Thailand purchases seasonal influenza vaccines which are provided free of charge to four high-risk groups: healthcare personnel, poultry cullers, persons aged ≥65 years, and persons with chronic diseases [10,11]. Over time Thailand’s Advisory Committee on Immunization Practice (ACIP) has expanded influenza vaccine recommendations to include eight high-risk populations (Fig. 1) [12,13]. Government purchase of influenza vaccine increased over 350% between 2009 and 2011 (520,000–2.38 million doses) [14]. Here, we estimate influenza vaccine uptake and coverage among high-risk populations in Thailand’s public sector, and assess vaccine wastage. These data can be used to evaluate and inform the national vaccination program.
Fig. 1.
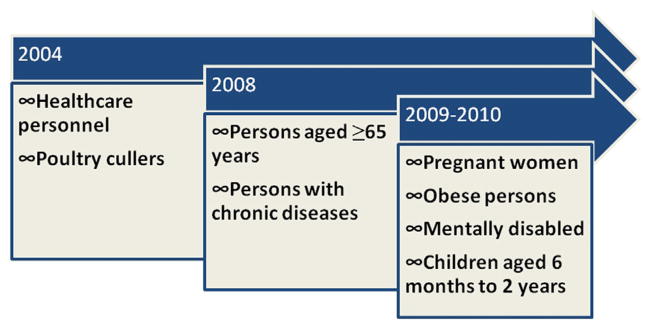
ACIP-recommended influenza vaccination target groups in Thailand by year of recommendation.
2. Methods
We conducted a retrospective review of seasonal influenza vaccine use in the public sector in Thailand from 2010 to 2012. Since this study was evaluating a national program, it was exempt from ethical review.
2.1. Study setting
Thailand is a middle-income country located in Southeast Asia that has a population of 66.0 million (est. 2010) [15]. The Thai GDP per capita is $5,318USD (est. 2012) [16], and 3.5% of Thailand’s GDP is spent on health expenditures (est. 2006) [17]. Thailand can be divided into five geographic regions (total est. 2010 population in parentheses): Metropolitan Bangkok (8.3 million), North (11.6 million), Northeast (19.0 million), Central (18.2 million), and South (8.9 million).
2.2. Influenza vaccine distribution
The Thailand National Health Security Office (NHSO) is responsible for providing health promotion activities, prevention services, treatment, and rehabilitation services to all who are enrolled in the Universal Coverage Scheme [18]. The Universal Coverage Scheme provides health insurance to nearly 75% of the Thai population, with the remainder being covered under the Social Security Scheme and the Civil Servant Medical Benefits Scheme. Following the 2008 recommendation by Thailand’s ACIP to vaccinate persons aged ≥65 years and persons with chronic diseases, NHSO began purchasing vaccine for these two high-risk groups. Vaccines purchased were inactivated, trivalent vaccines, provided to the Ministry of Public Health in multi-dose formulation (four doses per vial). Vaccines were distributed to each province based on the estimated number of persons in these two target groups (some swapping of vaccine between provinces may have occurred). Vaccination was administered in provincial and district hospitals during a 3-month campaign (or until vaccine ran out) starting in June of each year. In Thailand, outpatient clinics in hospitals serve as primary care centers. Healthcare personnel received no additional incentive for providing vaccines to the target groups. When administering vaccine, while healthcare providers prioritized the two target groups, vaccine was also administered to the other five target groups falling under the ACIP recommendation (pregnant women, obese persons weighing >100 kg and/or having a body mass index ≥35 kg/m2, mentally disabled persons, and children aged 6 months–2 years). Healthcare personnel and poultry cullers also received vaccines free of charge, although these were purchased by the Department of Disease Control of the Ministry of Public Health. For the purposes of this study, ‘publicly purchased vaccines’ refer to those purchased by the Department of Disease Control and NHSO.
2.3. Vaccine database
Each vaccination event was recorded in an electronic health record that was developed by NHSO for reimbursement purposes. After each vaccination, hospital staff entered the vaccine recipient’s 13-digit unique identification number, date of birth, date of vaccination, risk group category, province, and type of health insurance into the electronic health record. Patients not covered by the Universal Coverage Scheme could still be vaccinated and entered into this system. National data were compiled by NHSO.
2.4. High-risk group classification
In the NHSO electronic database, vaccinees were classified into pre-defined risk groups. Each vaccinee was assigned to only one risk category and some risk categories changed over time. If a vaccinee fell into >1 risk category, s/he would first be classified in either the chronic disease or aged ≥65 years groups; for the remaining risk categories, classification was at the discretion of the health-care provider. Four risk categories were consistent from 2010 to 2012: obese persons, young children aged 6 months–2 years, mentally disabled persons, and pregnant women. Three risk categories changed between 2010 and 2011–2012: persons aged ≥65 years, persons with chronic diseases and healthcare personnel/poultry cullers. Among the persons aged ≥65 years category, in 2010 all persons aged ≥65 years regardless of health status were included, whereas in 2011–2012, persons aged ≥65 years with chronic diseases were excluded from the category. In 2010, the persons with chronic diseases category excluded persons aged ≥65 years with chronic diseases; however, in 2011–2012 this category included all persons with chronic diseases regardless of age. Finally, the health-care personnel/poultry cullers category included all such workers in 2010, while in 2011–2012 poultry cullers/healthcare personnel with chronic diseases were excluded from this category.
2.5. Denominator data sources
We used three different data sources to estimate the denominator; coverage for some risk group categories was estimated using more than one approach.
2.6. National Statistical Office data
The National Statistical Office reports census data on all registered nationals [19]. We used these data to estimate the denominator for persons aged ≥65 years and young children aged 6 months–2 years. The data were reported in 1-year age increments; to estimate the number of infants aged 6 months–1 year, we calculated 50% of the 1-year age category.
2.7. National Health Examination Survey data
The National Health Examination Survey [20] is conducted every five years in Thailand to estimate the national prevalence of multiple health conditions. This nationally representative survey utilizes multi-stage random sampling to identify 30,000 participants for a health interview and examination. The most recent National Heath Examination Survey was conducted in 2009. The National Health Examination Survey data were used to estimate the denominator for young children aged 6 months–2 years, persons aged ≥65 years, obese persons, and for persons with chronic diseases. Chronic diseases included in the survey were chronic obstructive pulmonary disorder, asthma, cerebrovascular disease, diabetes mellitus, renal failure, and thalassemia.
2.8. NHSO inpatient/outpatient data
NHSO maintains databases of all persons who receive inpatient and/or outpatient care from a public hospital in Thailand. All patient visits are coded for reimbursement purposes using the 10th Revision of the International Statistical Classification of Diseases and Related Health Problems (ICD-10); codes are recorded at the time of final discharge (see Supplemental Table S1 for category definitions). Patients could receive up to two final diagnosis codes per hospital visit. The data were aggregated, and patients with more than one diagnosis were included in each illness category. For each fiscal year (October–September) that vaccines were purchased, duplicate diagnoses records for the same patient were deleted. These data were then used to estimate the denominator for persons with chronic diseases, pregnant women, obese persons, and mentally disabled persons. Chronic diseases included in the survey were heart disease, systemic lupus erythematosus, human immunodeficiency virus (HIV), and cancer.
2.9. Statistical analysis
Demographics characteristics (age, sex, and region of residence) of vaccinees are presented as number and proportion. All vaccinees were kept in their original NHSO-designated categories. However, because some risk group classifications varied by year we also combined groups to display all who were classified as persons aged ≥65 years, persons with chronic diseases, or healthcare personnel/poultry cullers. Vaccine coverage was calculated among the following groups for which we had denominator data: (1) persons aged ≥65 years; (2) persons with chronic diseases; (3) pregnant women; (4) obese persons; (5) mentally disabled persons; and (6) young children aged 6 months–2 years. In addition, we aggregated these data to present a total coverage estimate. We used the Wilson score method to calculate 95% confidence intervals (CI) for each of our coverage estimates. To graph vaccine coverage by year, we used the following denominators for each risk group: National Statistical Office census data for young children and persons aged ≥65 years, National Health Examination Survey and NHSO data for persons with chronic diseases, National Health Examination Survey data for obese persons, and NHSO data for pregnant women and persons who were mentally disabled. In the case of calculating coverage for persons with chronic diseases, NHSO data were used as the denominator source for conditions not included by the National Health Examination Survey: heart disease, immunodeficiency conditions (HIV; systemic lupus erythematosus), and cancer. National Health Examination Survey data were used as a denominator for chronic obstructive pulmonary disease, asthma, cerebrovascular disease, chronic renal failure, diabetes mellitus, and thalassemia. Sex differences in coverage within high-risk groups were calculated using Pearsons’ Chi squared test. Vaccine wastage for each year was defined as the proportion of vaccines purchased by the public sector for distribution to high-risk populations that were not used by these populations. We used Chi squared test for trend when looking at changes over the 3-year time period (Epi Info version 7.0, Centers for Disease Control and Prevention, Atlanta, GA, USA). For all other analyses, we used PASW version 18.0 (IBM, Armonk, NY, USA). A two-tailed p value <0.05 was considered statistically significant.
3. Results
From 2010 to 2012, 8.18 million doses of seasonal influenza vaccine were purchased by the Royal Thai government (Table 1). The number of vaccines purchased increased by 39% from 2.37 million doses in 2010 to 3.29 in 2012, and over the 3 years 91% of all purchased vaccines were administered. From 2010 to 2011, vaccine wastage increased (8.4% versus 10%), but decreased from 2011 to 2012 (10% versus 9.6%). Across all three years, vaccine wastage increased (trend p < 0.01), and was 9.5% per year, on average. Wastage was highest in Bangkok (42% in 2010, 26% in 2011, and 17% in 2012).
Table 1.
Number of influenza vaccine doses that were publicly purchased and used by year in Thailand, 2010–2012.
| Year | Vaccines purchased | Vaccines used, N(%) | Vaccines wasted (%) |
|---|---|---|---|
| 2010 | 2,370,678 | 2,170,813 (92) | 8.4 |
| 2011 | 2,515,880 | 2,259,614 (90) | 10 |
| 2012 | 3,294,000 | 2,976,836 (90) | 9.6 |
| Total | 8,180,558 | 7,407,263 (91) | 9.5 |
3.1. Characteristics of vaccinees
Of all vaccines that were distributed from 2010 to 2012, 29% was administered in 2010, 31% in 2011, and 40% in 2012 (Table 2). Sixty-five percent of the vaccines was administered to females and the median age of all vaccinees was 54 years in 2010, 58 years in 2011, and 59 years in 2012. The median age for persons with chronic diseases was 52 years in 2010 and 57 years in both 2011 and 2012. Across all three years, 765,984 (19%) of all persons with chronic diseases who were given a vaccine were aged ≥65 years. Among persons classified as persons aged ≥65 years, the median age was 72 years for all three years, and 2,550 (0.2%) were 60–64 years (these persons were excluded from the coverage estimates below). Among persons classified as young children aged 6 months–2 years, 693 (0.2%) were aged ≥3 years, and these persons were also excluded from coverage estimates. Of the 5 regions in Thailand, the Northeastern region administered the most vaccines (2,533,674; 34%), while Bangkok administered the least of the publicly purchased vaccines (384,560; 5.2%).
Table 2.
Descriptive characteristics of population receiving influenza vaccinea in the public sector in Thailand, 2010–2012.
| Characteristic | Total (n = 7,407,263) | 2010 (n = 2,170,813) | 2011 (n = 2,259,614) | 2012 (n = 2,976,836) |
|---|---|---|---|---|
| Sex, male, n (%) | 2,581,454 (35) | 765,585 (35) | 778,543 (35) | 1,037,326 (35) |
| Age, mean ± SD (median) | ||||
| All vaccinees | 54 ± 19 (57) | 51 ± 20 (54) | 55 ± 18 (58) | 56 ± 18 (59) |
| Chronic disease | 53 ± 17 (56) | 47 ± 16 (52) | 54 ± 17 (57) | 55 ± 16 (57) |
| Persons aged >65 years | 73 ± 6 (72) | 73 ± 6 (72) | 73 ± 6 (72) | 73 ± 6 (72) |
| Pregnant women | 27 ± 8 (26) | 27 ± 7 (26) | 27 ± 8 (26) | 27 ± 8 (26) |
| Obese | 41 ± 16 (43) | 41 ± 15 (43) | 42 ± 16 (45) | 41 ± 16 (43) |
| Mentally disabled | 33 ± 21 (30) | 33 ± 21 (30) | 34 ± 21 (31) | 32 ± 21 (28) |
| Young children (age 6 months–2 years) | 2 ± 5 (1.0) | 2 ± 6 (1.0) | 1 ± 1 (1.0) | 1 ± 1 (1.0) |
| Other | 46 ± 17 (49) | N/A | 57 ± 4 (40) | 46 ± 17 (42) |
| Place of residence, n (%) | ||||
| Northeastern region | 2,533,674 (34) | 728,231 (34) | 774,554 (34) | 1,030,889 (35) |
| Bangkok | 384,560 (5.2) | 121,003 (5.6) | 117,330 (5.2) | 146,227 (4.9) |
| Central region | 1,790,625 (24) | 520,924 (24) | 55,0518 (24) | 719,183 (24) |
| Southern region | 978,684 (13) | 303,304 (14) | 293,449 (13) | 381,931 (13) |
| Northern region | 1,718,443 (23) | 497,004 (23) | 523,342 (23) | 698,097 (23) |
Data missing on 922 (0.01%) for sex, 1,569 (0.02%) for age, and 1,277 (0.02%) for place of residence.
3.2. Vaccinees by target groups
From 2010 to 2012, 77% of vaccines were distributed to two target groups: 3,974,848 (54%) doses were administered to persons with chronic diseases and 1,721,490 (23%) to persons aged ≥65 years persons (Table 3). Additionally, 1,426,686 (19%) vaccines were administered to healthcare personnel and poultry cullers, 82,570 (1.1%) to young children aged 6 months–2 years, 78,885 (1.1%) to obese persons, 78,516 (1.1%) to persons whose risk group was listed as other (not specified), 26,481 (0.4%) to mentally disabled persons, and 17,787 (0.2%) to pregnant women. The proportion of vaccines administered to persons with chronic diseases increased from 2010 to 2011, and increased in persons aged ≥65 years from 2011 to 2012. When the two groups were combined to control for coding changes, there was only a decrease from 2011 to 2012. The proportion of vaccines that were administered to all other risk groups decreased from 2010 to 2012 (Table 3).
Table 3.
Number of influenza vaccines administered by target group and year, Thailand 2010–2012.
| Target group | Number of vaccine doses distributed
|
|||
|---|---|---|---|---|
| 2010 N (%) | 2011 N (%) | 2012 N (%) | Total N (%) | |
| Chronic disease Aged <65 yearsa Alla | 1,006,960 (46) | 1,324,662 (59) | 1,643,226 (55) | 3,974,848 (54) |
| 1,006,960 | – | – | ||
| – | 1,324,662 | 1,643,226 | ||
| Age ≥65 years | 576,035 (27) | 454,101 (20) | 691,354 (23) | 1,721,490 (23) |
| Alla | 576,035 | – | – | |
| No chronic diseasea | – | 454,101 | 691,354 | |
| Chronic disease and age ≥65 years combined | 1,582,995 (73) | 1,778,763 (79) | 2,334,580 (78) | 5,696,338 (77) |
| Healthcare personnel/poultry cullers | 487,953 (23) | 424,403 (19) | 514,330 (17) | 1,426,686 (19) |
| Alla | 487,953 | – | – | |
| No chronic diseasea | – | 424,403 | 514,330 | |
| Young children (aged 6 months–2 years)a | 43,860 (2.0) | 21,989 (1.0) | 16,721 (0.6) | 82,570 (1.1) |
| Obesea | 37,995 (1.8) | 21,701 (1.0) | 19,189 (0.7) | 78,885 (1.1) |
| Othera | – | 2 | 78,514 (2.6) | 78,516 (1.1) |
| Mentally disableda | 10,489 (0.5) | 7,884 (0.4) | 8,108 (0.3) | 26,481 (0.4) |
| Pregnant womena | 7,521 (0.4) | 4,872 (0.2) | 5,394 (0.2) | 17,787 (0.2) |
Denotes NHSO categorization for the risk groups.
3.3. Influenza vaccine coverage
Excluding healthcare personnel, poultry cullers, and those who were missing a risk group classification, overall coverage for the combined risk groups was 4.5% in 2010, 4.9% in 2011, and 6.3% in 2012 (Fig. 2). For all three years combined, coverage estimates for persons with chronic diseases ranged from 12% using the National Heath Examination Survey denominator to 30% using NHSO data. Among persons aged ≥65 years, coverage ranged from 14% using National Heath Examination Survey data to 15% using National Statistical Office data. Coverage estimates among obese persons ranged from 0.1% using National Heath Examination Survey data to 41% using NHSO data. Coverage estimates ranged from 0.8% to 0.9% in pregnant women and 1.5% to 1.6% in young children aged 6 months–2 years. Coverage among persons with mental disabilities was 4.9%.
Fig. 2.
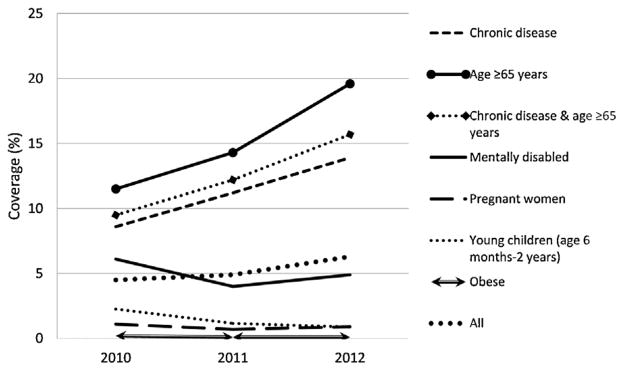
Vaccine coverage by year and target group, Thailand 2010–2012. We do not include coverage rates for healthcare personnel, poultry cullers, and those who were missing a risk group classification as we do not have denominator data for these risk groups.
From 2010 to 2012, vaccine coverage increased in persons with chronic diseases (8.6%, 11.2%, and 13.9%, respectively; p < 0.01), and persons aged ≥65 years (11.5%, 14.3%, and 19.6%, respectively; p < 0.01; see Table 4 and Fig. 2). Combined vaccine coverage for persons with chronic diseases and persons aged ≥65 years was 9.5% in 2010, 12.2% in 2011, and 15.7% in 2012. In all other target groups, vaccine coverage decreased between 2010 and 2012: 2.3–0.9% in young children aged 6 months–2 years (p < 0.01), 0.2–0.1% in obese persons (p < 0.01), 6.1% versus 4.9% in mentally disabled persons (p < 0.01), and 1.1–0.9% in pregnant women (p < 0.01).
Table 4.
Vaccine coverage by denominator source and ACIP-recommendation groups, 2010–2012.
| Target group | National Statistical Office data Coverage (95% confidence interval)
|
National Health Examination Survey data Coverage (95% confidence interval)
|
NHSO inpatient/outpatient data Coverage (95% confidence interval)
|
||||||
|---|---|---|---|---|---|---|---|---|---|
| 2010 | 2011 | 2012 | 2010 | 2011 | 2012 | 2010 | 2011 | 2012 | |
| Chronic diseases | – | 9.4 (9.3, 9.4) | 12.3 (12.3, 12.4) | 15.2 (15.2, 15.3) | 24.4 (24.4, 24.4) | 28.1 (28.1, 28.1) | 36.1 (36.0, 36.1) | ||
| 8.6 (8.6, 8.7)a | 11.2 (11.2, 11.2)a | 13.9 (13.9,13.9)a | |||||||
| Age ≥65 years | 11.5 (11.4, 11.5) | 14.3 (14.2, 14.3) | 19.6 (19.6, 19.7) | 10.4 (10.4, 10.5) | 13.0 (13.0, 13.0) | 18.0 (17.9, 18.0) | – | ||
| Chronic disease and age ≥65 years combined | – | 9.8 (9.7, 9.8) | 12.6 (12.5, 12.6) | 16.2 (16.2, 16.2) | – | ||||
| 9.5 (9.5, 9.5)a | 12.2 (12.1, 12.2)a | 15.7 (15.7, 15.7)a | |||||||
| Young children (aged 6 months–2 years) | 2.3 (2.3, 2.3) | 1.2 (1.2, 1.2) | 0.9 (0.9, 0.9) | 3.1 (3.0, 3.1) | 1.6 (1.5, 1.6) | 1.2 (1.2, 1.2) | – | ||
| Obese | – | 0.2 (0.2, 0.2) | 0.1 (0.1, 0.1) | 0.1 (0.1, 0.1) | 72.3 (71.9, 72.6) | 29.5 (29.1, 29.8) | 29.7 (29.4, 30.1) | ||
| Mentally disabled | – | – | 6.1 (6.0, 6.2) | 4.0 (3.9, 4.1) | 4.9 (4.9, 5.0) | ||||
| Pregnant | 1.0 (1.0, 1.0)b | 0.6 (0.6, 0.6)b | – | – | 1.1 (1.1, 1.1) | 0.7 (0.7, 0.7) | 0.9 (0.9, 1.0) | ||
Note: Bold indicates denominator sources deemed most reliable to estimate coverage.
NHSO inpatient and outpatient data used for denominators missing from National Heath Examination Survey (heart disease, systemic lupus erythematosus, and HIV, cancer).
Live births were reported for 2010–2011 only.
Coverage was higher among males than females among young children (male: 1.5%, female: 1.4%, p < 0.01), and mentally disabled persons (male: 8.0%, female: 5.8%, p < 0.01). In contrast, coverage was higher among females than males among obese persons (0.15% versus 0.13%, p < 0.01), persons aged ≥65 years (12.9% versus 11.1%, p < 0.01) and persons with chronic diseases (16.6% versus 9.6%, p < 0.01).
4. Discussion
This is the first vaccine coverage evaluation of the influenza vaccine program in Thailand. We found that the number of publicly purchased influenza vaccines increased 39% from 2010 to 2012, yet vaccine wastage also increased and averaged 9.5% annually. Overall vaccine coverage (excluding healthcare personnel and poultry cullers for which we had no denominator) was low (6.3% in 2012), but was highest (16% in 2012) in the two priority risk groups, persons with chronic diseases, and persons aged ≥65 years. Additionally, coverage increased among these groups from 2010 to 2012; however, in all other high-risk groups, coverage decreased. Use of different denominators generally had only a small effect on coverage estimates except among obese persons. We hypothesize that few persons are given an admission diagnosis of obesity thus underestimating the NHSO denominator.
The distribution of publicly purchased influenza vaccine to high-risk groups is a relatively new initiative in Thailand. Although vaccination of healthcare personnel and poultry cullers began in 2004, it was not until 2008 that Thailand’s NHSO began to purchase seasonal vaccines for persons aged ≥65 years and persons with chronic diseases. During the 2009 influenza pandemic, national influenza vaccine recommendations were expanded to include additional high-risk populations: pregnant women, young children aged 6 months–2 years, obese persons, and mentally disabled persons. However, persons aged ≥65 years and persons with chronic diseases have remained the priority groups for the influenza vaccine plan of the national health coverage scheme. This explains the relatively higher coverage in these two risk groups.
While influenza vaccination is increasing globally [21], coverage among high-risk groups varies between countries. One study on vaccine coverage in Germany, Spain, Italy, the United Kingdom, and France, estimated that during the 2006/2007 influenza season, vaccine coverage among persons aged ≥65 years and persons with chronic diseases ranged from 50% to 70% and 30% to 59%, respectively [22]. In the United States, vaccine coverage was estimated to be 77% (2012/2013) among children aged 6–23 months, 66% (2012/2013) among persons aged ≥65 years, and 43% (2011/2012) among pregnant women [23,24]. Higher coverage in the United States and Europe than in Thailand may reflect the maturity of these programs; for instance, the U.S. ACIP began making influenza vaccine recommendations for high-risk groups in 1984, whereas the Thai ACIP only began making recommendations in 2004. In South Korea, a country that in recent years has increased its vaccine purchases, vaccine coverage was estimated at 61% among persons aged ≥65 years and persons with chronic diseases, during the 2004/2005 influenza season. However, 17 million vaccines were available during the 2004/2005 influenza season, and 33% of the total population in South Korea received vaccine [25].
A major strength of our evaluation was our ability to use a national dataset on vaccine status for all individuals who received vaccines from public hospitals in Thailand. However, our evaluation also had several limitations. First, vaccine records were not standardized across all three years which resulted in changes in risk group classification between years making it difficult to assess temporal changes in coverage. For this reason, the coverage for combined risk groups is more likely to be accurate. Second, vaccines distributed to healthcare personnel and poultry cullers were pooled in the dataset, making it impossible to ascertain vaccine coverage in healthcare personnel separately, an important risk group. Third, there was no ideal denominator data source for persons with underlying disease and since some persons may have more than one underlying disease and therefore counted multiple times, we may have underestimated coverage. Fourth, since vaccinees could only be classified in one risk group, we may have underestimated coverage for some risk groups. Fifth, we did not have access to information on vaccines that went to a person not defined as a high-risk group (e.g., military personnel or prisoners) so the estimates of wastage are likely overestimated; despite this, wastage rates were as expected for multi-dose vials [26]. Finally, we did not include data on privately purchased influenza vaccine, which were about 1.5 times public sales in 2011 [14]. Therefore, we likely underestimate coverage estimates.
As Thailand continues to increase the use of influenza vaccine, these findings are important to establish baseline coverage and highlight programmatic challenges that can be addressed to increase coverage and reduce wastage. We hypothesize that optimal vaccine use can be achieved through better outreach to targeted population; however, future studies are needed to investigate acceptance and barriers to influenza vaccine receipt among high-risk groups in Thailand, as well as specific reasons for wastage, particularly in Bangkok (e.g., cold chain barriers or suboptimal outreach). Annual estimates of vaccine coverage will be important to assess progress toward program goals. Further, an existing effective influenza vaccine program is critical in the event of a pandemic where rapid vaccine deployment and assessment is paramount. The results of this evaluation will inform future evaluation of influenza vaccine coverage and management in Thailand.
Supplementary Material
Acknowledgments
This work was funded by the Centers for Disease Control and Prevention and the Associated Schools and Programs of Public Health (Cooperative Agreements 5U01GH00015203 and U36/CCU300430).
Appendix A. Supplementary data
Supplementary data associated with this article can be found, in the online version, at http://dx.doi.org/10.1016/j.vaccine.2014.10.029.
Footnotes
Disclaimer
The findings and conclusions in this report are those of the authors and do not necessarily represent the official position of the Centers for Disease Control and Prevention or the Associated Schools and Programs of Public Health.
References
- 1.WHO. Influenza Immunization, vaccines and biological. 2008 Available from: http://www.who.int/immunization/topics/influenza/en/index.html/ [cited 3.12.13]
- 2.WHO. Meeting of the strategic advisory group of experts on immunization, April 2012–conclusions and recommendations. Wkly Epidemiol Rec. 2012;87(21):201–16. [PubMed] [Google Scholar]
- 3.WHO. Fact sheet N 211. Influenza (Seasonal) 2009 Available from: http://who.int/mediacentre/factsheets/fs211/en/index.html/ [cited 20.06.13]
- 4.Bridges CB, Harper SA, Fukuda K, Uyeki TM, Cox NJ, Singleton JA, et al. Prevention and control of influenza. Recommendations of the advisory committee on immunization practices (ACIP) MMWR Recomm Rep. 2003;52(RR-8):1–34. (quiz CE1–4) [PubMed] [Google Scholar]
- 5.Simmerman JM, Uyeki TM. The burden of influenza in East and South-East Asia: a review of the English language literature. Influenza Other Respir Viruses. 2008;2(3):81–92. doi: 10.1111/j.1750-2659.2008.00045.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Wong CM, Yang L, Chan KP, Leung GM, Chan KH, Guan Y, et al. Influenza-associated hospitalization in a subtropical city. PLoS Med. 2006;3(4):e121. doi: 10.1371/journal.pmed.0030121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Chow A, Ma S, Ling AE, Chew SK. Influenza-associated deaths in tropical Singapore. Emerg Infect Dis. 2006;12(1):114–21. doi: 10.3201/eid1201.050826. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Simmerman JM, Chittaganpitch M, Levy J, Chantra S, Maloney S, Uyeki T, et al. Incidence, seasonality and mortality associated with influenza pneumonia in Thailand: 2005–2008. PLoS One. 2009;4(11):e7776. doi: 10.1371/journal.pone.0007776. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.The National Committee on Avian Influenza Control and The National Committee on Influenza Pandemic Control. National strategic plan for avian influenza control and influenza pandemic preparedness in Thailand, 2005–2007. 2005 Available from: http://203.157.19.193/invest/ai/bird%20flu.pdf/
- 10.Muangchana C, Thamapornpilas P, Karnkawinpong O. Immunization policy development in Thailand: the role of the Advisory Committee on Immunization Practice. Vaccine. 2010;28(Suppl 1):SA104–9. doi: 10.1016/j.vaccine.2010.02.043. [DOI] [PubMed] [Google Scholar]
- 11.Surichan S, Wirachwong P, Supachaturas W, Utid K, Theerasurakarn S, Langasanam P, et al. Development of influenza vaccine production capacity by the Government Pharmaceutical Organization of Thailand: addressing the threat of an influenza pandemic. Vaccine. 2011;29(Suppl 1):SA29–33. doi: 10.1016/j.vaccine.2011.04.120. [DOI] [PubMed] [Google Scholar]
-
12.National Vaccine Institute.
 [The guidelines of the National Vaccine Institute Steering Committee and Steering Sub-Committee] 2010 Available from: http://nvi.ddc.moph.go.th/attach/e-book/update%20file/executive/executive.pdf. [cited 09.12.2014]
[The guidelines of the National Vaccine Institute Steering Committee and Steering Sub-Committee] 2010 Available from: http://nvi.ddc.moph.go.th/attach/e-book/update%20file/executive/executive.pdf. [cited 09.12.2014]
-
13.Department of Disease Control.
 2554 [2010 guidelines for seasonal influenza vaccination facilities] 2010 Available from: http://dpc9.ddc.moph.go.th/crd/tranfers/guideline/flu_suggest.PDF. [cited 09.12.2014]
2554 [2010 guidelines for seasonal influenza vaccination facilities] 2010 Available from: http://dpc9.ddc.moph.go.th/crd/tranfers/guideline/flu_suggest.PDF. [cited 09.12.2014]
- 14.Gupta V, Dawood FS, Muangchana C, Lan PT, Xeuatvongsa A, Sovann L, et al. Influenza vaccination guidelines and vaccine sales in southeast Asia: 2008–2011. PLoS One. 2012;7(12):e52842. doi: 10.1371/journal.pone.0052842. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.National Statistical Office. The 2010 Population and Housing Census (Whole Kingdom) 2010 Available from: http://popcensus.nso.go.th/file/popcensus-10-01-56-E.pdf/ [cited 04.09.14]
- 16.United Nations Statistics Division. Country Profile: Thailand. 2013 Available from: http://www.data.un.org/CountryProfile.aspx?crName=THAILAND. [cited 18.10.13]
- 17.WHO. Total expenditure on health as a percentage of gross domestic product: Thailand. 2010 Available from: http://data.un.org/CountryProfile.aspx?crName=THAILAND/ [cited 18.10.13]
- 18.Bureau of Policy and Strategy and T.M.o.P. Health. Health policy in Thailand. 2009 Available from: http://www.bps.ops.moph.go.th/Health%20Policy%202009.pdf/ [cited 10.04.14]
- 19.National Statistical Office. 2012 Available from: web.nso.go.th/stat_theme>socpop.htm/
- 20.National Health Examination Study Group. National health examination survey IV. Nonthaburi: Health Systems Research Institute; 2009. [Google Scholar]
- 21.The macroepidemiology of influenza vaccination in 56 countries, 1997–2003. Vaccine. 2005;23(44):5133–43. doi: 10.1016/j.vaccine.2005.06.010. [DOI] [PubMed] [Google Scholar]
- 22.Blank PR, Schwenkglenks M, Szucs TD. Influenza vaccination coverage rates in five European countries during season 2006/07 and trends over six consecutive seasons. BMC Public Health. 2008;8:272. doi: 10.1186/1471-2458-8-272. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Centers for Disease Control and Prevention. Flu vaccination coverage: United States, 2012–2013 influenza season. 2013 Sep 25; Available from: www.cdc.gov/flu/fluvaxview/coverage-1213estimates.htm/ [cited 10.12.13]
- 24.Lu PJ, Santibanez TA, Williams WW, Zhang J, Ding H, Bryan L, et al. Surveillance of influenza vaccination coverage—United States: 2007–08 through 2011–12 influenza seasons. MMWR Surveill Summ. 2013;62(4):1–28. [PubMed] [Google Scholar]
- 25.Kee SY, Lee JS, Cheong HJ, Chun BC, Song JY, Choi WS, et al. Influenza vaccine coverage rates and perceptions on vaccination in South Korea. J Infect. 2007;55(3):273–81. doi: 10.1016/j.jinf.2007.04.354. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.WHO. Projected vaccine wastage. Immunization service delivery. 2014 Available from: http://apps.who.int/immunization_delivery/systems_policy/logistics_projected_wastage/en/index.html/ [cited 26.08.14]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


