Abstract
Objective
Optimism has been linked with an array of positive health outcomes at the individual level. However, researchers have not examined how a spouse's optimism might impact an individual's health. We hypothesized that being optimistic (and having an optimistic spouse) would both be associated with better health.
Methods
Participants were 3,940 adults (1,970 couples) from the Health and Retirement Study, a nationally representative panel study of American adults over the age of 50. Participants were tracked for four years and outcomes included: physical functioning, self-rated health, and number of chronic illnesses. We analyzed the dyadic data using the actor partner interdependence model.
Results
After controlling for several psychological and demographic factors, a person's own optimism and their spouse's optimism predicted better self-rated health and physical functioning (b's = .08-.25, p's < .01). More optimistic people also reported better physical functioning (b = −.11, p < .01) and fewer chronic illnesses (b = −.01, p < .05) over time. Further, having an optimistic spouse uniquely predicted better physical functioning (b = −.09, p < .01) and fewer chronic illnesses (b = −.01, p < .05) over time. The strength of the relationship between optimism and health did not diminish over time.
Conclusions
Being optimistic and having an optimistic spouse were both associated with better health. Examining partner effects is important because such analyses reveal the unique role that spouses play in promoting health. These findings may have important implications for future health interventions.
Keywords: optimism, aging, relationships, successful aging, positive psychology, psychological well-being
Imagine an older adult that you know, do you think that their partner's psychological attributes can affect their health? Emerging research suggests that the people in our social networks can have profound influence on our health and well-being [1-4]. For example, a recent study of older adults showed that even after accounting for an individual's own conscientiousness, their partner's conscientiousness was a unique predictor of his or her health [5]. In a study of cardiac rehabilitation patients and their partners, patients only accepted their partner's support if the couple reported similar exercise behaviors; in couples with dissimilar exercise behaviors, patients were less receptive to their partner's supportive efforts [6]. The researchers hypothesized that a patient's awareness of a partner's efforts to modify his or her own lifestyle increases the patient's appreciation of partner involvement, which then increases exercise among cardiac patients. These two studies highlight an emerging literature that examines individual health behavior within a dyadic context—acknowledging the relationships between the psychological characteristics of people who share the same social environment. Yet, to our knowledge, the potential dyadic effects that optimism have on health have not been examined.
Dispositional optimism—the generalized expectation that good things will happen—has been linked with an array of physical health benefits ranging from reduced risk of cardiovascular disease and stroke to healthier levels of antioxidants and lipids [7–15]. Optimism is also linked with healthier behaviors. For example, optimists are more likely to exercise, eat healthier diets, manage stress better, and abstain from smoking [10,12,16–17]. Further, optimism is an individual attribute that is about 25% heritable, but can also be learned and shaped by social influences [18–23]. Therefore, optimism may provide a point of intervention for improving health outcomes. Although optimism's association with various health behaviors and outcomes has been examined at the individual level, to our knowledge, the dyadic effects of optimism on health have not been examined.
In the field of health psychology, the associations between psychological factors and health are typically conceptualized and tested at the individual level. However, it is likely that a partner's personality can impact a person's health. In the current study, we used the actor-partner interdependence model (APIM) to estimate the actor and partner/spousal effects of optimism on health while accounting for the interdependence within couples [24]. Actor effects measure the influence of a person's predictor variable on that person's own health; partner/spousal effects capture the unique influence of an actor's predictor variable on his or her spouse's health. For example, in our study, the actor effects capture the influence of a person's own level of optimism on his or her own health, while the spousal effects capture the unique influence of an actor's optimism on his or her spouse's health (above and beyond the spouse's own level of optimism).
Why might a spouse's optimism be associated with an individual's health? Past research has identified social support as a mechanism that may link optimism with health [25-28]. Social support may partly explain the link between optimism and enhanced health because optimists have several advantages when using social support for goal achievement: 1) optimists are more likely to seek social support when facing difficult situations, 2) optimists are more well liked, 3) optimists have a larger network of friends who provide social support, and 4) for optimists, these friends provide more social support during stressful times [25,28-32].
Recent research examining the dyadic effects of optimism in close relationships found that optimism plays a key role in relationship quality and how couples interact. For example, a person's own optimism predicts his or her own relationship satisfaction as well as his or her partner's relationship satisfaction in cross-sectional analyses [33]. In longitudinal analyses, higher optimism is associated with higher relationship satisfaction, and this association is mediated by enhanced cooperative problem solving [34]. Perhaps these cooperative problem solving skills help couples enhance their physical health. For example, an optimistic partner may start going to the gym more often with their spouse, who is recovering from a cardiac event and having trouble meeting exercise goals. As mentioned above, researchers found that cardiac patients are much more receptive to a partner's support of exercise behavior if the couple reports similar exercise behaviors [6]. Research has also shown that couples that collaborate efficiently cope better with illness [35]. Thus, many of the mechanisms linking partner optimism to individual health could be direct and practical (e.g., perhaps an encouraging push to go to the gym or to eat a healthier meal).
Conflict and divorce in couples can cause serious physical illness [36]. However, optimists and their partners see both themselves and each other as reaching better resolutions after conflict [37]. Another potential mechanism linking optimism with higher relationship satisfaction may be the internal belief among optimists that they are receiving more support from their partner [37]. Interestingly, optimists may not actually receive more support from a partner, but only perceive that they are receiving more support [38]. Nonetheless, the perception of social support helps buffer against stress [38]. Therefore, both social support and relationship satisfaction may help explain the dyadic effects that optimism has on health.
Based upon this prior research, we examined the following hypotheses using longitudinal data from the Health and Retirement Study, a nationally representative sample of Americans over the age of 50. The identification of factors that protect against declining health is particularly important for the expanding segment of older adults who face the dual threat of declining health and rising health care costs.
We examined the link between optimism and health over a four-year period with three hypotheses in mind. First, we examined the association between optimism and health (as measured by: self-rated health, a 23-item measure of physical functioning, and an index of eight major chronic illnesses) at the individual level. We hypothesized that higher optimism would be associated with better health. Second, we examined the possible dyadic effects of optimism. We hypothesized that higher optimism in the spouse would predict better health in the actor, above and beyond the actor's own level of optimism. Third, we hypothesized that the actor and spousal effects of optimism would prospectively predict health over a four-year period.
Most studies using the APIM adjust for a very small number of covariates, if any at all. In our analyses we controlled for traditional risk factors that predict future health including age, gender, race/ethnicity, level of education, and household wealth. Given that previous studies found a link between other personality factors (e.g., conscientiousness and neuroticism) and health, we included these personality factors as covariates [5]. The addition of these covariates helped rule out third variable explanations.
Method
Sample and Procedure
The Health and Retirement Study (HRS) is a nationally representative and prospective panel study that has surveyed more than 22,000 Americans aged 50+ every two years [39-41]. Data have been collected since 1992. We report on psychological, health, and covariate data collected in 2006, 2008, and 2010. The University of Michigan's Institute for Social Research is responsible for the study and provides extensive documentation about the protocol, instrumentation, sampling strategy, and statistical weighting procedures. The HRS is sponsored by the National Institute on Aging (grant number NIA U01AG009740).
Starting in 2006, a random 50% of HRS respondents were selected for an enhanced face-to-face interview. A random half was selected because it was not financially feasible to provide enhanced face-to-face interviews for the entire HRS sample. At the end of the interview, interviewers left behind a self-report psychological questionnaire, which respondents completed and returned by mail to the University of Michigan. Among people who were interviewed, the response rate for the leave-behind questionnaire was 90%. Although HRS interviewed all couples in a household, only data for respondents aged 50 and older is used when survey weights are applied, because HRS was intentionally created to become a nationally representative sample of adults over the age of 50. Therefore, among those who were interviewed face-to-face, 7,168 respondents were eligible for HRS. For the present study, we selected data from heterosexual couples in which both the husband and wife completed measures of optimism and health (N = 3,940 or 1,970 couples). The couples sample used for the present study (N=3,940) differed from the broader sample (N=7,168) on several variables of interest. Specifically, the present sample was more optimistic (d = .17), healthier (d = .21), had fewer conditions (d = .11), better mobility (d = .20), and was younger (d = .13) than the larger representative sample.
Measures
Optimism
Optimism was assessed during the 2006 assessment using the Life Orientation Test-Revised (LOT-R). Studies have shown that the revised LOT-R has good reliability and validity [42]. The measure has also been demonstrated to have good discriminant and convergent validity [42]. A sample item is, “In uncertain times, I usually expect the best.” Participants are asked to rate the extent to which they agree with each item on a scale ranging from 1 (strongly disagree) to 6 (strongly agree). In total, six items were used to assess optimism (α = .75). Three negatively worded items were reverse scored, then all of the items were averaged to create a scale for optimism (M = 4.52, SD = .94).
Researchers sometimes split the LOT-R into two subscales—with one scale consisting of only positively valenced items and the other scale consisting of only negatively valenced items. We chose not to create subscales for theoretical and methodological reasons [43,44]. Optimism is most accurately captured by a scale that combines both positively worded items that are endorsed and negatively worded items that are rejected [43]. It is increasingly evident that a division into subscales may be at odds with the goal of controlling for acquiescence response bias in the measurement of psychological constructs. Thus, following recent theorizing and work in this area, we used the six-item composite, rather than creating two 3-item subscales [13,44].
Health Measurements
Health was assessed at each wave (2006, 2008, 2010) using three different measurements. First, self-rated health was assessed with a single item, “Would you say your health is excellent, very good, good, fair, or poor?” Participants rated their health on a scale ranging from 1 (poor) to 5 (excellent; M = 3.21, SD = .95). Numerous studies have shown that the self-rated health measure used in this study shows good predictive validity [45,46].
Second, physical functioning was assessed using items adapted from scales developed by Rosow and Breslau [47], Nagi [48], Katz, Ford, Moskowitz, Jackson, and Jaffe [49], and Lawton and Brody [50]. Physical functioning was conceptualized as a multidimensional construct that assessed general mobility, large-muscle functioning, gross motor skills, fine motor skills, and the ability to execute a variety of activities of daily living and instrumental activities of daily living. The items asked, “Because of a health problem do you have any difficulty...?” All respondents answered yes or no to each of the questions. The items ranged from running or jogging a mile to shopping for groceries and bathing (max = 23). The present analyses used a count of reported limitations, where higher values indicate more limitations (M = 3.35, SD = 3.39).
Third, an index of eight major chronic illnesses was computed for each participant. Chronic illnesses included (1) high blood pressure, (2) diabetes, (3) cancer or a malignant tumor of any kind (excluding minor skin cancer), (4) lung disease, (5) coronary heart disease including heart attacks, angina, and congestive heart failure, (6) emotional, nervous, or psychiatric problems, (7) arthritis or rheumatism, and (8) stroke. Each participant self-reported eight physician diagnosed conditions. All health conditions in HRS are assessed via self-report of a doctor's diagnosis. Researchers have rigorously assessed these self-reported health measures, demonstrating their validity and reliability [51]. The number of major health problems were summed so that higher values reflected more health problems (M = 2.23, SD = 1.39).
Covariates Measurement
Covariates included: age, gender, race/ethnicity (European-American, African-American, Hispanic, other), educational attainment (no degree, GED or high school diploma, college degree or higher), and total household wealth (<25,000; 25,000-124,999; 125,000-299,999; 300,000-649,999; >650,000—based on quintiles of the score distribution in this sample). Each participant's total household income was assessed in U.S. dollars.
Statistical Analyses
Statistical analyses were conducted using STATA (version 12) and SPSS (version 20). To account for the interdependence of individuals within dyads, we used multilevel modeling (MLM) procedures recommended for dyadic data analysis [24]. MLM estimates both actor effects (associations between a person's optimism and his/her own health) and partner (spouse) effects (associations between a person's optimism and his/her spouse's health) while accounting for the statistical non-independence of members in a couple. The moderating effects of these variables on time enabled us to test if the relationship between actor/spouse optimism and health became stronger or weaker over time. Following recommended procedures, gender was contrast-coded (−1 = men, 1 = women) and predictor variables (spouse/actor optimism) were grand-mean centered [24]. Self-rated health, physical functioning, and number of chronic illnesses served as dependent measures in our MLM analyses.
Each model was checked for assumptions of linearity, equal variance, and normality. Analyses of residual differences between observed values and predicted values from each model indicated that these basic assumptions were satisfied. One additional assumption of dyadic data analyses (and the actor-partner model of interdependence in particular) is that the variance of the slopes of time for husbands and wives are invariant across models. Additional analyses that were run relaxing this assumption led to virtually identical results, suggesting equality of variance in the estimates of time for husbands and wives.
Results
Descriptive Statistics
Participants ranged in age from 53 to 97 (M = 68.51, SD = 8.68). Self-reported race/ethnicity was 84.2% Caucasian, 8.3% African-American, 6.2% Hispanic, and 1.3% Other. Median level of education was a high school education (16.3% had less than a high school education, 54.8% had a high school education, 28.9% reported having at least some college education). Descriptive statistics and correlations among primary study variables are presented in Table 1.
Table 1.
Correlations Among Primary Study Variables
| 2006 |
2008 |
2010 |
|||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | |
| 1. 2006 Actor Optimism | |||||||||||
| 2. 2006 Spousal Optimism | .25** | ||||||||||
| 3. 2006 Health | .30** | .17** | |||||||||
| 4. 2006 Functioning | −.25** | −.16** | −.57** | ||||||||
| 5. 2006 Conditions | −.17** | −.09** | −.45** | .44** | |||||||
| 6. 2008 Health | .28** | .16** | .67** | −.48** | −.43** | ||||||
| 7. 2008 Functioning | −.19** | −.11** | −.43** | .64** | .67** | −.54** | |||||
| 8. 2008 Conditions | −.17** | .08** | −.45** | .44** | .93** | −.46** | .45** | ||||
| 9. 2010 Health | .26** | .14** | .61** | −.44** | −.40** | .64** | −.47** | −.42** | |||
| 10. 2010 Functioning | −.17** | −.09** | −.33** | .46** | .29** | −.37** | .57** | .33** | −.57** | ||
| 11. 2010 Conditions | −.18** | −.10** | −.45** | .42** | .87** | −.45** | .43** | .93** | −.46** | .45** | |
| M | 4.52 | 4.52 | 3.30 | 3.44 | 2.04 | 3.21 | 3.27 | 2.20 | 3.25 | 3.35 | 2.40 |
| SD | .94 | .94 | 1.05 | 3.92 | 1.39 | 1.04 | 3.92 | 1.42 | 1.04 | 4.29 | 1.44 |
Preliminary Analyses
Optimism was associated with better self-rated health, better physical functioning, and fewer chronic illnesses both cross-sectionally and prospectively. Similarly, spouse optimism was associated with better self-rated health, better physical functioning, and fewer chronic illnesses both cross-sectionally and prospectively. Self-rated health, physical functioning, and chronic illnesses were significantly correlated both within each assessment point and between all assessment points. People reporting worse physical functioning and more chronic illnesses reported lower levels of self-rated health. Further, optimism (r = .25, p <.001), self-rated health (r = .26, p <.001), physical functioning (r = .26, p <.001), and chronic illnesses (r = .24, p <.001) were significantly correlated between members of each couple, indicating substantial interdependence for these measures.
Dyadic Analyses Predicting Health
We hypothesized that both actor and spousal optimism would predict better health outcomes over time. We tested these hypotheses using dyadic growth curve modeling, which enabled us to model intra-individual changes and moderators of these changes. Time (Assessment points 1, 2, 3) was treated as a within-subjects factor. Actor/spousal optimism at Time 1 was treated as time invariant. Separate multi-level models were conducted predicting self-rated health, physical functioning, and chronic illnesses from time, actor optimism, spousal optimism, and the interactions between time and actor/spousal optimism.1 We also included several covariates that are related to health including: age at Time 1, gender, race/ethnicity, education, and household wealth. The results from each of the separate multilevel models are shown in Table 2.
Table 2.
Multilevel Models Predicting Self-Rated Health, Physical Functioning, and Conditions
| Self-Rated Health |
Physical Functioning |
Conditions |
||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| b | SE (b) | Z | r | b | SE (B) | Z | r | b | SE (B) | Z | r | |
| Gender | .02 | .01 | 1.27 | .02 | .40 | .05 | 8.38** | .13 | −.01 | .02 | −.38 | .01 |
| Age | −.02 | .002 | −10.81** | .17 | .10 | .01 | 15.24** | .24 | .04 | .003 | 15.80** | .24 |
| Time | −.06 | .01 | −8.01** | .13 | −.03 | .03 | −.97 | .02 | .21 | .01 | 41.75** | .55 |
| Actor Optimism | .25 | .02 | 11.49** | .18 | −.86 | .09 | −9.93** | .16 | −.17 | .03 | −6.46** | .10 |
| Spousal Optimism | .08 | .02 | 3.77** | .06 | −.30 | .09 | −3.49** | .06 | −.03 | .03 | −1.03 | .02 |
| Actor Optimism × Time | −.01 | .01 | −1.37 | .02 | −.11 | .03 | −3.17** | .05 | −.01 | .01 | −2.42* | .04 |
| Spousal Optimism × Time | −.01 | .01 | −1.13 | .02 | −.09 | .03 | −2.63** | .04 | −.01 | .01 | −1.66† | .03 |
| Race/ethnicity | ||||||||||||
| Black | −.22 | .05 | −4.04** | .06 | .84 | .20 | 4.18** | .07 | .11 | .09 | 1.39 | .02 |
| Hispanic | −.13 | .06 | −2.14* | .03 | −.06 | .23 | −.26 | .004 | −.28 | .10 | −2.84** | .05 |
| Other | .05 | .12 | .42 | .01 | −.14 | .45 | −.30 | .005 | −.45 | .19 | −2.36* | .04 |
| Education | ||||||||||||
| High School | .20 | .04 | 4.93** | .08 | −.49 | .15 | −3.20** | .05 | −.06 | .06 | −.91 | .01 |
| College or higher | .33 | .05 | 6.95** | .11 | −.97 | .18 | −5.47** | .09 | −.17 | .07 | −2.31* | .04 |
| Wealth | ||||||||||||
| 2nd Quintile | .10 | .06 | 1.53 | .02 | −.61 | .24 | −2.54* | .04 | −.06 | .10 | −.59 | .01 |
| 3rd Quintile | .29 | .06 | 4.66** | .07 | −1.27 | .23 | −5.55** | .09 | −.36 | .10 | −3.74** | .06 |
| 4th Quintile | .44 | .06 | 7.13** | .11 | −1.61 | .23 | −6.93** | .11 | −.49 | .10 | −5.01** | .08 |
| 5th Quintile | .53 | .06 | 8.33** | .13 | −1.90 | .24 | −8.09** | .13 | −.67 | .10 | −6.69** | .11 |
Note. N = 3940; Effects are reported as unstandardized regression coefficients; Gender: −1 = men, 1 = women
< .10
p < .05
p < .01
Self-Rated Health
For self-rated health, a significant main effect of time emerged indicating that people reported lower self-rated health over time. Both actor and spousal optimism emerged as unique predictors and these effects are consistent with the pattern reported above. In other words, individual-level optimism was associated with better self-rated health. Having a spouse high in optimism was also associated with better self-rated health. The time × actor/spousal optimism interactions were not significant, suggesting that actor/spousal optimism at Time 1 continued to predict health at every assessment point of the study and did not diminish in influence.
Physical Functioning
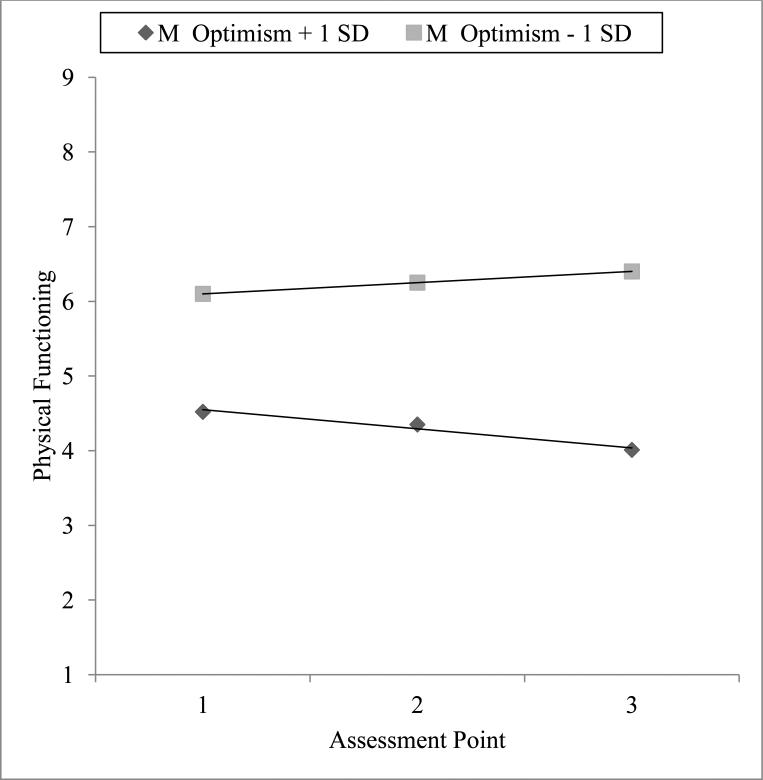
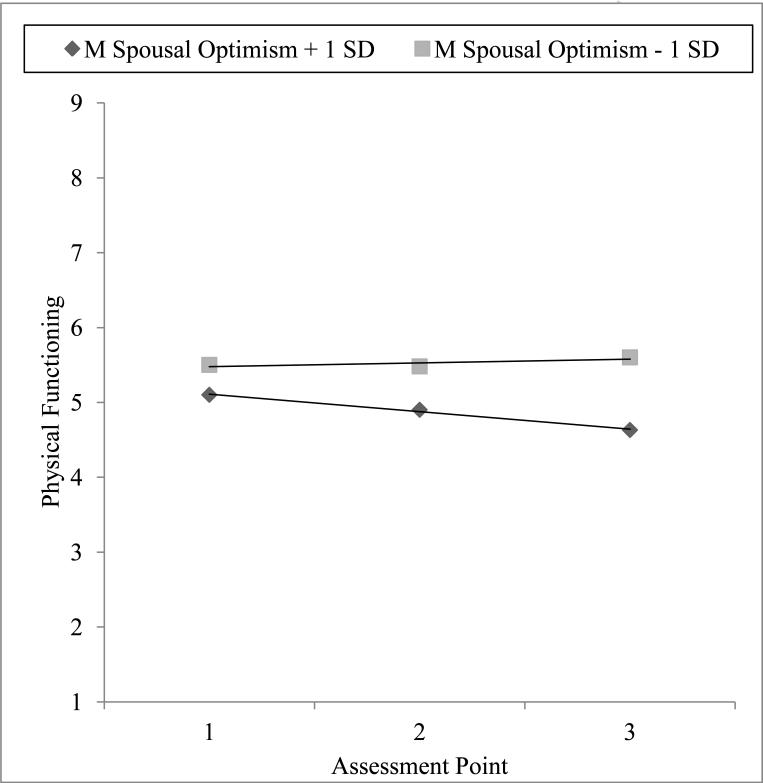
Actor and spousal optimism each uniquely predicted better physical functioning. There was a significant time × actor optimism interaction, indicating that the relationship between actor optimism and physical functioning changed over time. As seen in Figure 1, people high in optimism increased in physical functioning over time and people low in optimism decreased in physical functioning over time. Among people high in optimism, the slope of wave was b = −.13, Z = −2.94, p = .003. Among people low in optimism, the slope of wave was b = .07, Z = 1.60, p = .11. There was also a significant time × spousal optimism interaction. As seen in Figure 2, people with spouses high in optimism increased in physical functioning over time, b = −.11, Z = −2.56, p = .01. Among people with spouses low in optimism, the slope of wave was not significant, b = .05, Z = 1.22, p = .22.
Figure 1.
The effects of actor optimism on physical functioning over the duration of the study.
Figure 2.
The effects of spousal optimism on physical functioning over the duration of the study.
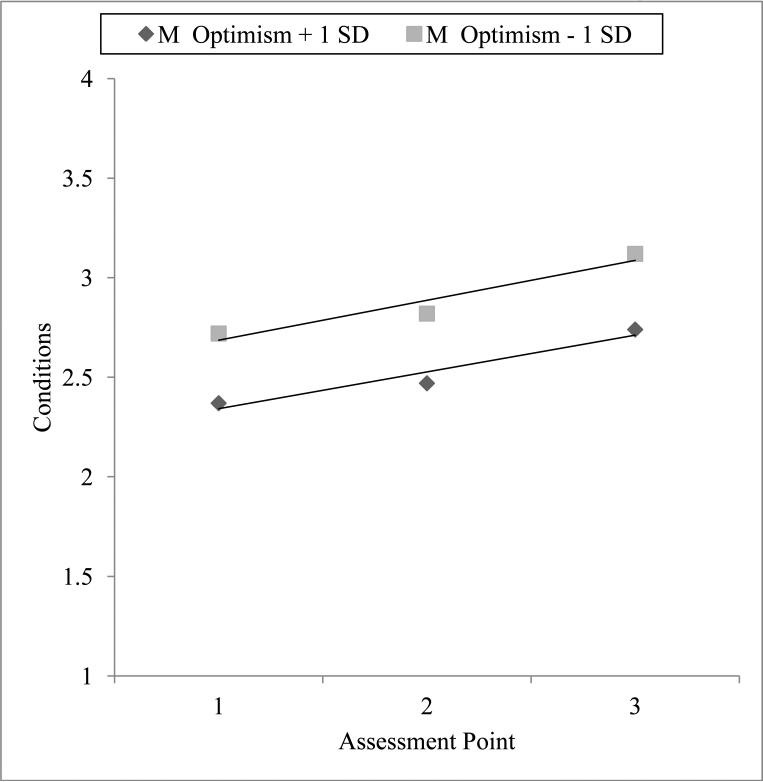
Chronic Illnesses
For chronic illnesses, there was a significant main effect of time such that people were diagnosed with more chronic illnesses over time. People high in optimism reported fewer chronic illnesses overall. However, the previous bivariate relationship between spousal optimism and chronic illnesses was no longer significant in the full multi-level model. There was a significant time × actor optimism interaction, indicating that the relationship between actor optimism and chronic illnesses changed over time. As seen in Figure 3, people high in optimism reported fewer illnesses over time than people low in optimism. Among people high in optimism, the slope of wave was b = .20, Z = 27.75, p < .001. Among people low in optimism, the slope of wave was b = .23, Z = 30.26, p <.001. Thus optimism appeared to serve a protective function and was associated with a slowed increase in the number of illnesses over time.2
Figure 3.
The effects of actor optimism on chronic health conditions over the duration of the study.
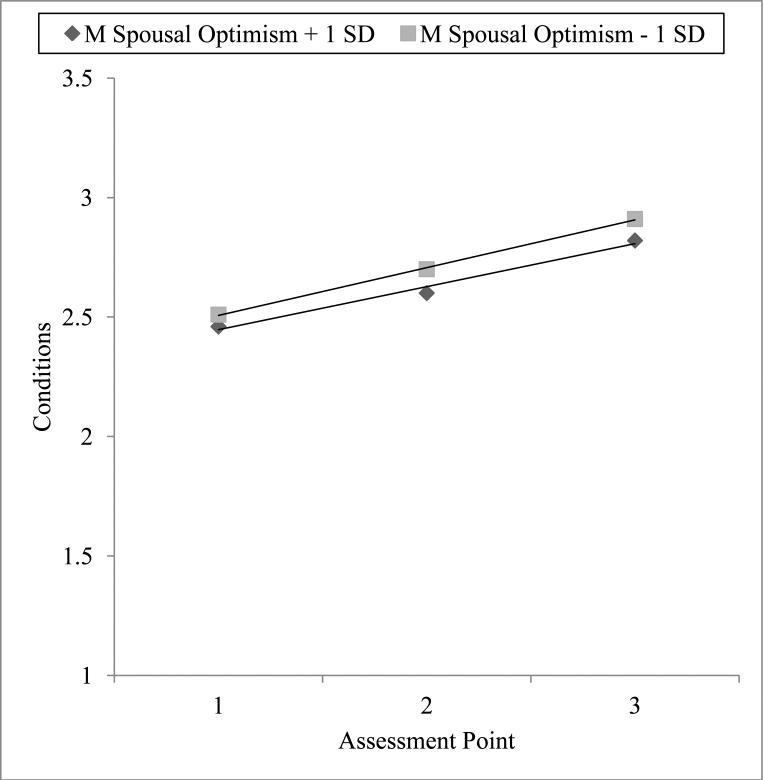
Additional Analyses
Using data from the 2006 wave of HRS, Roberts and colleagues found that higher levels of actor and spousal conscientiousness were cross-sectionally associated with better self-rated health and physical functioning [5]. The authors also controlled for the negative effects of neuroticism on health. To help temper the idea that our findings could be explained by personality traits previously linked to our dependent variables (in a subsection of our sample nonetheless), we reran each multi-level model controlling for participants’ conscientiousness and neuroticism. Although conscientiousness and neuroticism were both significant predictors of self-rated health, physical functioning, and chronic illnesses, the findings were virtually identical to those reported in Table 2 with one exception. After controlling for conscientiousness and neuroticism, a previously marginally significant spousal optimism × time interaction emerged as significant for chronic illnesses, b = −.01, Z = 1.96, p < .05. As seen in Figure 4, people with optimistic spouses reported fewer illnesses over the course of the study than people with non-optimistic spouses. Among people with spouses high in optimism, the slope of wave was b = .20, Z = 27.62, p < .001. Among people with spouses low in optimism, the slope of wave was b = .22, Z = 30.15, p < .001. Thus, optimistic spouses appear to provide a health protective effect. More specifically, compared to people who have less optimistic spouses, people who have more optimistic spouses accumulate a reduced number of illnesses over time.
Figure 4.
The effects of partner optimism on chronic health conditions over the duration of the study after controlling for conscientiousness and neuroticism.
Discussion
In a prospective and nationally representative sample of adults over the age of 50, we found that optimism was associated with three indicators of health: self-rated health, a 23-item measure of physical functioning, and a count of eight major chronic illnesses. After controlling for personality traits (i.e., conscientiousness and neuroticism) and several covariates related to health (i.e., age, gender, race/ethnicity, education, household wealth), both actor and spousal optimism predicted better self-rated health and physical functioning. Also, people with higher optimism generally fared better over time, reporting better physical functioning and fewer chronic illnesses across a four-year period. Having an optimistic spouse predicted better physical functioning and fewer chronic illnesses over time, even above and beyond a person's own level of optimism. Further, actor and spousal optimism prospectively predicted self-rated health, such that the relationship between optimism and health was just as strong at Time 1 as it was at Time 3.
Examining partner effects is important because this type of analyses reveals the unique role that partners play in promoting health. To our knowledge, this is the first study to examine the dyadic effects of optimism on health. Why might optimism enhance health? A growing number of studies suggest that the health-enhancing nature of optimism may be attributable to various direct and indirect pathways. For instance, optimists engage in healthier lifestyles that simultaneously minimize health risk factors for illness and promote health. For example, in one study having higher optimism at the outset of a cardiac rehabilitation program predicted increases in exercise and decreases in body fat, saturated fat, and an index of overall coronary risk [52]. Other studies have found that optimists are more likely to engage in health-promoting behaviors such as eating healthy diets, exercise, stress management, and smoking abstention [10,16,17]. Direct physiological effects have also been implicated. Optimism has been linked with healthier levels of interleukin (IL)-6, C-reactive protein, fibrinogen, carotid intima medial thickness, lipids, and serum antioxidants [12,13,53,54].
Psychologically, optimists are better at goal-directed behaviors and self regulation. For example, in the face of controllable stressors optimists persevere and cope by using problem-solving and planning strategies to manage the stressor [16,55]. When faced with uncontrollable stressors, however, they shift their sights to other goals and use adaptive emotion-focused coping mechanisms, such as acceptance of their current situation [55]. As discussed in more detail in the introduction section, past research has found that social support may be a mechanism that links optimism with health [25-32]. Additionally, recent dyadic research examining the role of optimism in close relationships has found that optimism plays a key role in both the quality of relationships and how couples interact [33,34]. Further studies are needed to understand the mechanisms responsible for the health-enhancing effects of optimism seen in observational studies.
Some of the effect sizes in this study were moderate or small. There are many cases, however, where small effect sizes translate into meaningful outcomes. Therefore, it is important to interpret findings based on how constructs operate in the real world and also examine if these effects accumulate across a person's lifespan [56,57]. The dyadic effects of optimism are most likely cumulative in nature, only conferring benefits after several years of daily interactions over the lifetime of the couple's relationship. Another limitation is the way in which we created the chronic illness condition score. In the current study, the eight conditions were summed, giving equal weight to each condition. However, different conditions may warrant different weights. For example, a person with heart failure may require a larger chronic illness weight than a person with a mild case of arthritis. However, there was no data on the severity of each condition. Therefore, we could not weight the conditions based on severity. This is an issue that future research should examine. Future research should also move beyond self-reported health outcomes and examine more objective biological outcomes such as blood pressure, cholesterol levels, or mortality. However, the number of chronic illnesses a person has is one of the most common methods used to predict patient mortality. Further, particularly among older adults, self-reported measures like self-rated health and physical functioning are often comparable to or even better predictors of mortality than objective biological markers [58,59].
It is unclear if people can have such high dispositional optimism that it begins harming their health. However, literature on a similar yet distinct construct (e.g., optimistic bias and unrealistic optimism) has been shown to be harmful. For example, one study found that people high in dispositional optimism knew more about cardiovascular risk factors and had higher self-awareness of their cardiovascular risk status, even after adjusting for potential confounding factors, such as level of education [60]. In the same experiment, people with high unrealistic optimism were at higher cardiovascular risk but mistakenly believed they were at lower risk. They also worried less about their risk and knew less about the risk factors for heart attacks—although they believed they knew more about risk factors. When reading information about risk factors, they also remembered less information. At the surface level, people with high in dispositional optimism and high unrealistic optimism might be mistakenly grouped into the same category. However, these two groups of people differ in very important ways that are consequential for health. Our data did not assess information about optimistic bias or unrealistic bias. Therefore, we could not investigate how these constructs were related to a spouse's health and well-being. This is an important issue that future research should address.
Finally, reverse causality is a possibility—better health may lead to higher optimism. Unfortunately, the analytic methods used in this study did not allow us to disentangle the causal direction of the association. However, a large and growing body of research suggests that optimism is at least partially responsible for better health. Further, optimism is resilient to declining health and news of impending health decline. For example, a new cancer diagnosis or people with cancer could plausibly have declining optimism over time due to declining health, the side of effects of medication, disrupted social roles, erosion of psychological resources, and declining income and wealth. Optimism, however, remains stable before and after a cancer diagnosis, as well as before and after cancer treatment [61-63].
Despite these limitations, this study has several considerable strengths. The HRS is one of the only nationally representative studies to contain extensive health and psychological information on older couples. The study is also much larger in size than typical studies examining dyadic effects. It is also one of the few to examine the dyadic effects of psychological characteristics on health longitudinally. Additionally, most studies using the APIM adjust for a very small number of covariates, if any at all. However, we controlled for age, gender, race/ethnicity, level of education, household wealth, conscientiousness, and neuroticism.
The current study suggests that the positive psychological characteristics of spouses, namely optimism, can be associated with the health of older adults. Continued research in this domain may not only enhance our knowledge of optimism's effects on health, but also increase the conceptual and physiological understanding of how mental and physical health processes interact in couples. This knowledge may then contribute to the development of more specific prevention and intervention programs for health.
Research Highlights.
Optimism has been linked with an array of positive health outcomes at the individual level.
Researchers have not examined how a spouse's optimism might impact an individual's health.
This study prospectively examined if having an optimistic spouse would impact a person's health.
It was conducted in a nationally representative sample of U.S. adults over the age of 50.
Being optimistic and having an optimistic spouse were both associated with better health.
Acknowledgements
We would like to thank Richard Gonzalez for his advice on statistical analyses. We would like to acknowledge the Health and Retirement Study, which is conducted by the Institute for Social Research at the University of Michigan, with grants from the National Institute on Aging (U01AG09740) and the Social Security Administration.
Support: The first author was supported by the Rackham Predoctoral Fellowship. The second author was supported by a National Science Foundation Graduate Research Fellowship.
Role of the Sponsor: The funding sources had no influence on the design or conduct of the study; collection, management, analysis or interpretation of the data; or preparation, review, or approval of the manuscript. Eric S. Kim and William J. Chopik had full access to all data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis. All authors contributed to the design of the study and interpretation of the findings, and have read, commented on, and approved the manuscript.
Glossary
- HRS
Health and Retirement Study
- APIM
Actor-Partner Interdependence Model
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Interactions between actor and spousal characteristics predicting health outcomes were also possible, although uncommon in dyadic research on optimism. These interaction terms would test if there was a “synergistic” effect of optimism on health. In one scenario in which this interaction term was significant, the best outcomes would be observed among couples in which if both members were high in optimism). If not significant, actor and spousal effect would be independent of each other. In this scenario, spousal optimism would predict an outcome irrespective of the individual's level of optimism (i.e., actor optimism would not moderate the association between spousal optimism and time). Although not specifically hypothesized in the current study, we reran each model including interactions between actor and partner optimism. None of these interactions were significant (p's > .26); these results were excluded in favor of a more parsimonious model.
One common practice in dyadic data analysis is to check if the dyads are “distinguishable” on a particular feature (most often gender). If gender significantly moderated any of the associations in the multi-level models, it would suggest that the actor/partner paths would differ between women and men. To assess this, reran each of the models including every possible interaction with gender. Gender did not moderate any of the associations between actor/partner optimism on health.
Disclosures: There are no conflicts of interest.
References
- 1.Smith KP, Christakis NA. Social networks and health. Ann Rev of Sociol. 2008;34:405–29. [Google Scholar]
- 2.Uchino B. Social support and health: a review of physiological processes potentially underlying links to disease outcomes. J Behav Med. 2006;29:377–87. doi: 10.1007/s10865-006-9056-5. [DOI] [PubMed] [Google Scholar]
- 3.Bolger N, Zuckerman A, Kessler RC. Invisible support and adjustment to stress. J Pers Soc Psychol. 2000;79:953–61. doi: 10.1037//0022-3514.79.6.953. [DOI] [PubMed] [Google Scholar]
- 4.Knoll N, Schwarzer R, Pfüller B, Kienle R. Transmission of depressive symptoms: a study with couples undergoing assisted-reproduction treatment. Eur Psychol. 2009;14:7–17. [Google Scholar]
- 5.Roberts BW, Smith J, Jackson JJ, Edmonds G. Compensatory conscientiousness and health in older couples. Psychol Sci. 2009;20:553–9. doi: 10.1111/j.1467-9280.2009.02339.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Hong TB, Franks MM, Gonzalez R, Keteyian SJ, Franklin BA, Artinian NT. A dyadic investigation of exercise support between cardiac patients and their spouses. Health Psychol. 2005;24:430–4. doi: 10.1037/0278-6133.24.4.430. [DOI] [PubMed] [Google Scholar]
- 7.Giltay EJ, Geleijnse JM, Zitman FG, Hoekstra T, Schouten EG. Dispositional optimism and all-cause and cardiovascular mortality in a prospective cohort of elderly Dutch men and women. Arch Gen Psychiatry. 2004;61:1126–35. doi: 10.1001/archpsyc.61.11.1126. [DOI] [PubMed] [Google Scholar]
- 8.Tindle HA, Chang Y-F, Kuller LH, Manson JE, Robinson JG, Rosal MC, Siegle GJ, Matthews KA. Optimism, cynical hostility, and incident coronary heart disease and mortality in the Women's Health Initiative. Circulation. 2009;120:656–62. doi: 10.1161/CIRCULATIONAHA.108.827642. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kim ES, Park N, Peterson C. Dispositional optimism protects older adults from stroke: the Health and Retirement Study. Stroke. 2011;42:2855–59. doi: 10.1161/STROKEAHA.111.613448. [DOI] [PubMed] [Google Scholar]
- 10.Boehm JK, Kubzansky LD. The heart's content: the association between positive psychological well-being and cardiovascular health. Psychol Bull. 2012;138:655–91. doi: 10.1037/a0027448. [DOI] [PubMed] [Google Scholar]
- 11.Peterson C, Park N, Kim ES. Can optimism decrease the risk of illness and disease among the elderly? Aging Health. 2012;8:5–8. [Google Scholar]
- 12.Boehm JK, Williams DR, Rimm EB, Ryff C, Kubzansky LD. Association between optimism and serum antioxidants in the Midlife in the United States Study. Psychosom Med. 2013;75:2–10. doi: 10.1097/PSY.0b013e31827c08a9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Boehm JK, Williams DR, Rimm EB, Ryff C, Kubzansky LD. Relation between optimism and lipids in midlife. Am J Cardiol. 2013;111:1425–1431. doi: 10.1016/j.amjcard.2013.01.292. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Rasmussen HN, Scheier MF, Greenhouse JB. Optimism and physical health: a meta-analytic review. Ann Behav Med. 2009;37:239–56. doi: 10.1007/s12160-009-9111-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Kim ES, Smith J, Kubzansky LD. A prospective study of the association between dispositional optimism and incident heart failure. Circ Heart Fail. doi: 10.1161/CIRCHEARTFAILURE.113.000644. In press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Carver CS, Scheier MF, Segerstrom SC. Optimism. Clin Psychol Rev. 2010;30:879–89. doi: 10.1016/j.cpr.2010.01.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Giltay EJ, Geleijnse JM, Zitman FG, Buijsse B, Kromhout D. Lifestyle and dietary correlates of dispositional optimism in men: the Zutphen Elderly Study. J Psychosom Res. 2007;63:483–90. doi: 10.1016/j.jpsychores.2007.07.014. [DOI] [PubMed] [Google Scholar]
- 18.Heinonen K, Räikkönen K, Matthews KA, Scheier MF, Raitakari OT, Pulkki L, Keltikangas-Järvinen L. Socioeconomic status in childhood and adulthood: associations with dispositional optimism and pessimism over a 21-year follow-up. J Pers. 2006;74:1111–26. doi: 10.1111/j.1467-6494.2006.00404.x. [DOI] [PubMed] [Google Scholar]
- 19.Plomin R, Scheier MF, Bergeman CS, Pedersen NL, Nesselroade JR, McClearn GE. Optimism, pessimism and mental health: a twin/adoption analysis. Pers Indiv Dif. 1992;13:921–30. [Google Scholar]
- 20.Peters ML, Flink IK, Boersma K, Linton SJ. Manipulating optimism: can imagining a best possible self be used to increase positive future expectancies? J Pos Psychol. 2010;5:204–11. [Google Scholar]
- 21.Meevissen YMC, Peters ML, Alberts HJEM. Become more optimistic by imagining a best possible self: effects of a two week intervention. J Behav Ther Exp Psychiatry. 2011;42:371–8. doi: 10.1016/j.jbtep.2011.02.012. [DOI] [PubMed] [Google Scholar]
- 22.Seligman ME. Learned optimism: how to change your mind and your life. Vintage; New York: 2011. [Google Scholar]
- 23.Hanssen MM, Peters ML, Vlaeyen JWS, Meevissen YMC, Vancleef LMG. Optimism lowers pain: evidence of the causal status and underlying mechanisms. Pain. 2013;154:53–5. doi: 10.1016/j.pain.2012.08.006. [DOI] [PubMed] [Google Scholar]
- 24.Kenny DA, Kashy D, Cook WL. Dyadic data analysis. Guilford Press; New York: 2006. [Google Scholar]
- 25.Brissette I, Scheier MF, Carver CS. The role of optimism in social network development, coping, and psychological adjustment during a life transition. J Pers Soc Psychol. 2002;82:102–11. doi: 10.1037//0022-3514.82.1.102. [DOI] [PubMed] [Google Scholar]
- 26.Dougall AL, Hyman KB, Hayward MC, McFeeley S, Baum A. Optimism and traumatic stress: the importance of social support and coping. J Appl Soc Psychol. 2001;31:223–45. [Google Scholar]
- 27.Shen B-J, McCreary CP, Myers HF. Independent and mediated contributions of personality, coping, social support, and depressive symptoms to physical functioning outcome among patients in cardiac rehabilitation. J Behav Med. 2004;27:39–62. doi: 10.1023/b:jobm.0000013643.36767.22. [DOI] [PubMed] [Google Scholar]
- 28.Trunzo JJ, Pinto BM. Social support as a mediator of optimism and distress in breast cancer survivors. J Consult Clin Psychol. 2003;71:805–11. doi: 10.1037/0022-006x.71.4.805. [DOI] [PubMed] [Google Scholar]
- 29.Nes LS, Segerstrom SC. Dispositional optimism and coping: a meta-analytic review. Pers Soc Psychol Rev. 2006;10:235–51. doi: 10.1207/s15327957pspr1003_3. [DOI] [PubMed] [Google Scholar]
- 30.Carver CS, Kus LA, Scheier MF. Effects of good versus bad mood and optimistic versus pessimistic outlook on social acceptance versus rejection. J Soc Clin Psychol. 1994;13:138–51. [Google Scholar]
- 31.Segerstrom SC. Optimism, goal conflict, and stressor-related immune change. J Behav Med. 2001;24:441–67. doi: 10.1023/a:1012271410485. [DOI] [PubMed] [Google Scholar]
- 32.Karademas EC. Self-efficacy, social support and well-being: the mediating role of optimism. Pers Indiv Dif. 2006;40:1281–90. [Google Scholar]
- 33.Smith TW, Ruiz JM, Cundiff JM, Baron KG, Nealey-Moore JB. Optimism and pessimism in social context: an interpersonal perspective on resilience and risk. J Res Pers. 2013;47:553–62. doi: 10.1016/j.jrp.2013.04.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Assad KK, Donnellan MB, Conger RD. Optimism: an enduring resource for romantic relationships. J Pers Soc Psychol. 2007;93:285–97. doi: 10.1037/0022-3514.93.2.285. [DOI] [PubMed] [Google Scholar]
- 35.Berg CA, Upchurch R. A developmental-contextual model of couples coping with chronic illness across the adult life span. Psychol Bull. 2007;133:920–54. doi: 10.1037/0033-2909.133.6.920. [DOI] [PubMed] [Google Scholar]
- 36.Kiecolt-Glaser JK, Newton TL. Marriage and health: his and hers. Psychol Bull. 2001;127:472. doi: 10.1037/0033-2909.127.4.472. [DOI] [PubMed] [Google Scholar]
- 37.Srivastava S, McGonigal KM, Richards JM, Butler EA, Gross JJ. Optimism in close relationships: how seeing things in a positive light makes them so. J Pers Soc Psychol. 2006;91:143–53. doi: 10.1037/0022-3514.91.1.143. [DOI] [PubMed] [Google Scholar]
- 38.Vollmann M, Antoniw K, Hartung F-M, Renner B. Social support as mediator of the stress buffering effect of optimism: The importance of differentiating the recipients’ and providers’ perspective. Eur J Pers. 2011;25:146–54. [Google Scholar]
- 39.Health and Retirement Study, (HRS Data Files; 2006, 2008, 2010) public use dataset. Produced and distributed by the University of Michigan with funding from the National Institute on Aging (grant number NIA U01AG009740) Institute for Social Research; Ann Arbor: 2014. [Google Scholar]
- 40.Wallace RB, Herzog AR. Overview of the health measures in the Health and Retirement Study. J Hum Resour. 1995;30:S84–107. [Google Scholar]
- 41.Smith J, Fisher G, Ryan L, Clarke P, House J, Weir D. Psychosocial and lifestyle questionnaire: 2006-2010. Institute for Social Research; Ann Arbor: 2013. [Google Scholar]
- 42.Scheier MF, Carver CS, Bridges MW. Distinguishing optimism from neuroticism (and trait anxiety, self-mastery, and self-esteem): A reevaluation of the Life Orientation Test. J Pers Soc Psychol. 1994;67:1063–78. doi: 10.1037//0022-3514.67.6.1063. [DOI] [PubMed] [Google Scholar]
- 43.Ryff CD, Singer B. What to do about positive and negative items in studies of psychological well-being and ill-being? Psychother Psychosom. 2007;76:61–2. [Google Scholar]
- 44.Segerstrom SC, Evans DR, Eisenlohr-Moul TA. Optimism and pessimism dimensions in the Life Orientation Test-Revised: method and meaning. J Res Pers. 2011;45:126–9. [Google Scholar]
- 45.Idler EL, Benyamini Y. Self-rated health and mortality: a review of twenty-seven community studies. J Health and Soc Behav. 1997;38:21–37. [PubMed] [Google Scholar]
- 46.Schnittker J, Bacak V. The increasing predictive validity of self-rated health. PLoS ONE. 2014;9:e84933. doi: 10.1371/journal.pone.0084933. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Rosow I, Breslau N. A Guttman health scale for the aged. J Gerontol. 1966;21:556–9. doi: 10.1093/geronj/21.4.556. [DOI] [PubMed] [Google Scholar]
- 48.Nagi SZ. An epidemiology of disability among adults in the United States. Milbank Mem Fund Q Health Soc. 1976:439–67. [PubMed] [Google Scholar]
- 49.Katz S, Ford AB, Moskowitz RW, Jackson BA, Jaffe MW. Studies of illness in the aged. The index of ADL: a standardized measure of biological and psychosocial function. JAMA. 1963;185:914–9. doi: 10.1001/jama.1963.03060120024016. [DOI] [PubMed] [Google Scholar]
- 50.Lawton MP, Brody EM. Assessment of older people: self-maintaining and instrumental activities of daily living. Gerontologist. 1969;9:179–86. [PubMed] [Google Scholar]
- 51.Fisher GG, Faul JD, Weir DR, Wallace RB. Documentation of Chronic Disease Measures in the Heath and Retirement Study (HRS/AHEAD) Survey Research Center University of Michigan; Ann Arbor, MI: 2005. [Google Scholar]
- 52.Shepperd JA, Maroto JJ, Pbert LA. Dispositional optimism as a predictor of health changes among cardiac patients. J Res Pers. 1996;30:517–34. [Google Scholar]
- 53.Roy B, Diez-Roux AV, Seeman T, Ranjit N, Shea S, Cushman M. Association of optimism and pessimism with inflammation and hemostasis in the Multi-Ethnic Study of Atherosclerosis (MESA). Psychosom Med. 2010;72:134–40. doi: 10.1097/PSY.0b013e3181cb981b. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Matthews KA, Raikkonen K, Sutton-Tyrrell K, Kuller LH. Optimistic attitudes protect against progression of carotid atherosclerosis in healthy middle-aged women. Psychosom Med. 2004;66:640–4. doi: 10.1097/01.psy.0000139999.99756.a5. [DOI] [PubMed] [Google Scholar]
- 55.Aspinwall LG, Richter L. Optimism and self-mastery predict more rapid disengagement from unsolvable tasks in the presence of alternatives. Motiv Emot. 1999;23:221–45. [Google Scholar]
- 56.Abelson RP. A variance explanation paradox: when a little is a lot. Psychol Bull. 1985;97:129–33. [Google Scholar]
- 57.Roberts BW, Kuncel NR, Shiner R, Caspi A, Goldberg LR. The power of personality: the comparative validity of personality traits, socioeconomic status, and cognitive ability for predicting important life outcomes. Perspect Psychol Sci. 2007;2:313–45. doi: 10.1111/j.1745-6916.2007.00047.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Lee SJ, Go AS, Lindquist K, Bertenthal D, Covinsky KE. Chronic conditions and mortality among the oldest old. Am J Public Health. 2008;98:1209–14. doi: 10.2105/AJPH.2007.130955. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Bopp M, Braun J, Gutzwiller F, Faeh D, Swiss National Cohort Study Group Health risk or resource? Gradual and independent association between self-rated health and mortality persists over 30 years. PLoS ONE. 2012;7:e30795. doi: 10.1371/journal.pone.0030795. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Radcliffe NM, Klein WMP. Dispositional, unrealistic and comparative optimism: differential relations with the knowledge and processing of risk information and beliefs about personal risk. Pers Soc Psychol Rev. 2002;28:836–46. [Google Scholar]
- 61.Schou I, Ekeberg Ø , Sandvik L, Ruland CM. Stability in optimism-pessimism in relation to bad news: a study of women with breast cancer. J Pers Assess. 2005;84:148–54. doi: 10.1207/s15327752jpa8402_04. [DOI] [PubMed] [Google Scholar]
- 62.Stanton AL, Snider PR. Coping with a breast cancer diagnosis: a prospective study. Health Psychol. 1993;12:16–23. doi: 10.1037//0278-6133.12.1.16. [DOI] [PubMed] [Google Scholar]
- 63.Stiegelis HE, Hagedoorn M, Sander-man R, van der Zee KI, Buunk BP, van den Bergh ACM. Cognitive adaptation: a comparison of cancer patients and healthy references. Br J Health Psychol. 2003;8:303–18. doi: 10.1348/135910703322370879. [DOI] [PubMed] [Google Scholar]