Abstract
Given the heightened risk for HIV and other STIs among young men who have sex with men (YMSM) as well as the racial/ethnic disparities in HIV/STI risk, an understanding of longitudinal trends in sexual behaviors is warranted as YMSM emerge into adulthood. Drawing from an ongoing prospective cohort study, the present analysis employed latent growth curve modeling to examine trends in distinct types of sexual activity without condoms over time in sample of YMSM and examine differences by race/ethnicity and perceived familial SES. Overall, White and Mixed race YMSM reported more instances of oral sex without condom as compared to other racial/ethnic groups with rates of decline over time noted in Black YMSM. White YMSM also reported more receptive and insertive anal sex acts without a condom than Black YMSM. Declines over time in both types of anal sex acts without condoms among Black men were noted when compared to White men, while increases over time were noted for mixed race YMSM for condomless insertive anal sex. The effects for race/ethnicity were attenuated with the inclusion of perceived familial SES in these models. These findings build on previous cross sectional studies showing less frequent sex without condoms among Black YMSM despite higher rates of HIV incidence in emerging adulthood, as well as the importance of considering economic conditions in such models. Efforts to understand racial/ethnic disparities in HIV/STIs among YMSM must move beyond examination of individual-level sexual behaviors and consider both race/ethnicity and socioeconomic conditions in order to evaluate how these factors shape the sexual behaviors of YMSM.
INTRODUCTION
Among male adolescents and young adults between the ages of 13 – 24 years old, risk for HIV and other sexually transmitted infections (STIs) attributed to male-to-male sexual contact continue to increase. CDC HIV Surveillance data also note that the majority of known HIV infections among adolescent and young adult males in 2011 were among young men who reported having sex with other men; specifically, 93% of HIV diagnoses were in males between 13–19 years old while 91% were among males 20– 24 years old [1]. In New York City (NYC), new HIV (non-AIDS) diagnoses among MSM <30 years old surpassed that among MSM ≥30 years old for the first time in 2009 [2]. And by 2012, the largest proportion of new HIV infections in NYC, 46%, was among MSM between the ages of 20 – 29 [2]. Additionally, the 2011 CDC STD surveillance report indicates that the prevalence of chlamydia (CT) was approximately 14% and 12% among YMSM STD clinic patients ≤19 and 20–24 years old, respectively, across all STD Surveillance Network Sites (SSuN) [3]. In NYC, approximately 22% of individuals testing positive for gonorrhea (GC) at local SSuNs were MSM [3]. Finally, primary and secondary (P&S) syphilis has steadily increased from 2007–2011 among MSM in the US [3].
One factor underlying these alarming trends in HIV and other STIs among YMSM in the US may be engagement in sexual activity without a condom. However, the majority of studies examining sexual behaviors over time have focused on adult MSM or HIV-seropositive MSM and their partners [4–8]. A meta-analysis of such studies noted that these increases in sexual activity were not accounted for by use of combination antiretroviral therapies (cART), undetectable viral load, or HIV treatment optimism [9]. However, the application of findings around sexual behaviors among adult and older MSM to YMSM is flawed as adolescence is a time where individuals often begin to engage in sexual behaviors [10]. A recent study by Halkitis and colleagues (2011) examining differences in sexual activity by age groups found that YMSM were more likely to report engaging in sexual risk behaviors than older MSM [11]. While these reports provide important information on overall sexual behaviors and cross-sectional associations, the bulk of studies examining sexual activity among YMSM have focused on anal intercourse without disaggregating these findings by type of anal intercourse – receptive versus insertive and have virtually ignored oral sex. These gaps in knowledge are of particular concern among YMSM given the persistence, and in some cases, increased risk of STIs across sites – including oral gonorrhea, as well as penile and rectal gonorrhea and chlamydia. Furthermore, a more nuanced understanding of the trajectory of sexual behaviors as well as changes in frequency and types of sexual activity among YMSM merit additional exploration and understanding given the increased risk for HIV and other STIs as YMSM age.
In addition to the persistence of higher incidence and prevalence of HIV and other STIs among YMSM overall, are the stark racial/ethnic disparities in HIV/STIs. Specifically, among all MSM, 36% of new infections in 2010 were among Black men; furthermore, the majority of these infections (45%) occurred among those ages 13 to 24 [1]. Finally, Hispanic MSM accounted for 22% of new infections in 2010 [1]. A number of studies investigating racial/ethnic disparities in HIV and other STI risk among YMSM have often sought to examine how differences in levels of sexual behavior between racial/ethnic groups may drive these disparities [12–17]. However, the bulk of studies examining sexual behaviors across race/ethnicity have been either cross-sectional or they have ignored the multiple types of sexual behavior that may be related to HIV/STI risk among YMSM. Thus, the limited data on trajectories of sexual activity over time and by race/ethnicity prevents our ability to fully disentangle the differences in HIV/STI risk by race/ethnicity as YMSM age.
Finally, a number of reports have incorporated measures of SES in their examination of sexual behaviors [18–20]. As such, the extant empirical evidence suggests that lower SES is associated with higher rates of sexual risk behaviors in vulnerable heterosexual young men. More specifically, research with young gay and bisexual men shows that although individuals of higher SES report more sexual partners, those of lower SES were more likely to engage in receptive anal sex without a condom [21]. In an analysis conducted on a sample of 18–19 year-old YMSM, those of a lower SES were more likely to engage in 2 or more instances of unprotected anal sex than men who had a perceived middle or upper class SES [22]. These findings suggest that SES has distinct impacts on sexual activity and related behaviors among YMSM which warrant further attention. Specifically, the combined experiences of both racial and sexual discrimination coupled with economic and social disparities may manifest in the behaviors and lived experiences of YMSM of color.
Thus, the production of racial/ethnic as well as social disparities in HIV/STI risk among YMSM may be a function of the salient yet distinct impacts of race/ethnicity and socioeconomic status on HIV/STI related sexual behaviors among YMSM. In addition, as few studies have examined specific sexual behaviors longitudinally to substantiate findings from cross-sectional studies, the goal of this study is to describe changes in oral and anal, disaggregated as receptive and insertive, sexual activity without condoms in a racially/ethnically and socioeconomically diverse sample of YMSM over time.
METHODS
Study Design and Sample
The present study employs data from a prospective cohort study of YMSM – the Project 18 (P18) Study, which has been previously described in detail [23]. Briefly, participants were recruited via active and passive recruitment modalities involving approaching individuals at community based settings and events, and posting study information on social media sites between May 2009 and July 2011. Individuals were eligible for study participation if they were between 18 – 19 years old at screening, born biologically male, reported having sex with another man in the previous 6 months, and reported an HIV-negative/unknown serostatus. During the recruitment period, a total of n=2,068 participants were screened for study eligibility and n= 600 were enrolled into the P18 cohort study. Among the remaining n=1,468 screened, 49% or n=719 individuals were ineligible due to age > 19 years; this was the most common reason for lack of study eligibility.
Across baseline and semi-annual follow-up visits, data were collected via detailed, structured assessment using standardized methods to ensure adherence to study protocols and consistency of data collection across all visits. First, participants provided information on sociodemographic characteristics via audio-computer assisted self-interview (ACASI). This methodology is preferred for ascertaining information among adolescents and young adults as it can decrease the impact of differential reading ability within this group as well as reduce the likelihood of social desirability bias in responding. Next, information on recent sexual behaviors was obtained using the Timeline Followback (TLFB) calendar-based measure. The TLFB is a semi-structured, interviewer-administered assessment designed to collect detailed information on sexual activity for the 30 days preceding each study visit [24]. The TLFB allows interviewers to assist participants with the recall of recent events that can serve as a reference point to guide the recollection of sexual behaviors. By employing this technique, participants were able to report on sexual activity for each day during the past 30 days using a personalized calendar.
The present study employs data from the baseline, 6-, 12- and 18-month follow-up visits conducted onsite at the P18 research center offices. To ensure high participant retention in this study, a dedicated team of study staff members was trained to conduct follow-up and retention-related activities (e.g., regular phone calls, text message reminders, etc.) during this period. As a result of these on-going retention efforts, the present analysis includes information on n=600 (100%), n=460 (89.5%), n=446 (88.5%), and n=428 (85.9%) participants who completed the baseline and the 6-, 12- and 18-month follow-up visits, respectively. Finally, this study holds a federal certificate of confidentiality from the Department of Health and Human Services and the study protocol was approved by the New York University Institutional Review Board.
Measures
For the main dependent variable, participants reported each instance of (1) receptive oral intercourse, (2) receptive anal intercourse, and (3) insertive anal intercourse during the 30 days preceding interview via the TLFB. In addition, for each sexual activity, participants reported instances during which a condom was used as well as instances were a condom was not used. Consequently, data on sexual activity were collected as counts for each: receptive oral sex, and receptive and insertive anal sex with and without condoms. Correlations across sexual activity variables within a visit were low to moderate (r=0.14 to r=0.51, p<0.05). Across visits, there was moderate correlation in receptive oral sex (r=0.16 to r=0.47, p<0.05), low to moderate correlation in insertive (r=0.08 to r=0.37, p<0.10) and receptive anal sex (r=0.09 to r=0.42, p<0.05) (data not shown).
The main independent variables of interest include race/ethnicity and perceived familial socioeconomic status. First, using participants’ self-reported race/ethnicity, participants were grouped as Hispanic/Latino, Black, White, Asian/Pacific Islander (API), or mixed/other race. Next, perceived familial SES was used as a proxy for household-level income. This choice was made for several reasons. First, given participant age at baseline (18 – 19 years old) in combination with the large proportion (86%) who were in school full-time at baseline, it was unlikely that participants would have their own yearly income. Second, the low likelihood of accurately recalling/knowing parental household income would prevent ascertaining information on parental household income. Finally, a number of studies suggest that perceptions of socioeconomic status are as equally salient predictors of health-related behaviors and outcomes as actual income and socioeconomic status. Thus, for the present analysis, perceived familial SES was categorized as lower, middle and upper class.
Statistical Analysis
First, key sociodemographic characteristics for this cohort of sexual minority youth were compared to determine whether there were any differences between the full cohort at baseline and those who returned for follow-up visits. Chi square tests were employed to identify statistically significant differences for these key covariates. Second, exploratory data analyses were conducted to describe overall trends in sexual activity over time. This also included calculating correlations between sexual activity and predictor variables over time for this sample of sexual minority men.
Third, to examine change in sexual activity over time, a series of latent growth curve models were fit for each type of sexual activity assessed. Latent growth modeling was chosen as it offers a flexible technique for modeling systematic within- and between-individual differences in change over time. To investigate changes in number of episodes of receptive oral, insertive anal, and receptive anal intercourse without a condom between baseline and 18-months, separate latent growth models were fit which estimated a single unconditional growth model for the final level (at 18-months) and linear rate of change for each of these three sexual behaviors. Two latent constructs representing the final level and linear rate change for each sexual activity variable were estimated. Factor loadings for the growth parameters in these models were fixed and equal to either a constant value of 1 (intercept/final level) or to the values representing the point in time at which the sex use behaviors were measured (i.e., -18, -12, -6, and 0 months; rate of change). Next, to investigate between-individual differences in the final level and rate of change in receptive oral, insertive and receptive anal intercourse without a condom, separate conditional growth models were fit for each type of sexual behavior. The first set of conditional models included an indicator variable representing race/ethnicity. The second set of models included separate indicator variables for both race/ethnicity and socioeconomic status (SES). All latent growth models were fit in MPlus (version 6.1). Growth models were compared using a set of fit indices including χ2, the Comparative Fit Index (CFI) and the root mean squared error of approximation (RMSEA) statistics.
RESULTS
Descriptive Analyses
Initial exploration of sample characteristics relevant to the present analysis indicate that there were no statistically significant differences with respect to race/ethnicity or perceived familial socioeconomic status when comparing participants who completed the baseline assessment with those who returned for follow-up visits at either the 6-, 12- or 18-month follow-up visits (Table 1). Thus, there was no differential loss-to-follow up by race/ethnicity or perceived familial SES for this sample of study participants who completed study visits at the P18 research center. Next, means and standard deviations for each type of sexual episode without a condom reported in the 30 days preceding study interview are presented in Table 2. On average, mean levels of receptive oral, insertive and receptive anal sex increased in this sample of sexual minority youth over time.
Table 1.
Key covariates across baseline and follow-up visits among participants in the P18 cohort study.
| Baseline (n = 600)* |
6 month (n = 460) |
12 month (n = 445) |
18 month (n = 428) |
||||
|---|---|---|---|---|---|---|---|
| % (n) | % (n) | p | % (n) | p | % (n) | p | |
| Race | |||||||
| White | 28.9 (173) | 30.3 (139) | 0.97 | 29.1 (129) | 0.81 | 27.7 (118) | 0.91 |
| Black | 14.9 (89) | 15.9 (73) | 16.0 (71) | 16.9 (72) | |||
| Hispanic | 38.3 (229) | 37.6 (172) | 38.8 (172) | 38.7 (165) | |||
| Asian | 4.8 (29) | 4.6 (21) | 5.6 (25) | 4.9 (21) | |||
| Mixed race | 9.4 (56) | 8.1 (37) | 7.0 (31) | 8.0 (34) | |||
| Other race | 3.7 (22) | 3.5 (16) | 3.4 (15) | 3.8 (16) | |||
| Perceived Familial SES | |||||||
| Lower | 33.5 (200) | 33.1 (152) | 0.82 | 32.0 (142) | 0.94 | 33.6 (143) | 0.87 |
| Middle | 37.1 (222) | 36.9 (169) | 39.3 (174) | 38.3 (163) | |||
| Upper | 29.5 (176) | 29.9 (137) | 28.7 (127) | 28.2 (120) | |||
Baseline data on race/ethnicity and SES are missing for n=2 participants yielding an analytic sample of n = 598
Table 2.
Descriptive Statistics for sexual behaviors without a condom across baseline and follow-up visits among participants in the P18 cohort study
| Baseline (n = 598) |
6 Months (n = 460) |
12 Months (n = 445) |
18 Months (n = 428) |
|
|---|---|---|---|---|
| Mean (SD) | Mean (SD) | Mean (SD) | Mean (SD) | |
| Sexual Activity (last 30 days) | ||||
| # Episodes UAII | 0.40 (1.99) | 0.55 (2.34) | 0.70 (2.91) | 0.63 (2.27) |
| # Episodes UAIR | 0.52 (2.26) | 0.64 (2.42) | 0.57 (2.03) | 0.65 (2.06) |
| # Episodes Oral Giving | 1.85 (3.45) | 2.18 (3.89) | 2.31 (3.72) | 2.60 (3.76) |
Correlations among the sexual activity variables within each assessment were low to moderate (rs ranging from 0.14 – 0.51, p<.05). There was moderate within-individual stability in receptive oral (rs ranging from 0.16 – 0.47 across time, p<.05), and low to moderate within-individual stability in insertive anal (rs ranging from 0.08 – 0.37, p<.10) and receptive anal (rs ranging from 0.09 – 0.42, p<.05). An examination of the correlations between the race/ethnicity dummy variables and SES revealed small to moderate correlations by race/ethnicity, specifically for White, Black, Hispanic, and API YMSM but not Mixed/Other race YMSM, suggesting there may be a need to account for SES when considering racial/ethnic differences in sexual activity. Specifically, White YMSM reported higher perceived familial SES levels (r = 0.35, p<.05), while Black and Hispanic YMSM had lower perceived familial SES levels (r = −0.20, p<.05 for both groups). Finally, API YMSM reported marginally higher perceived familial SES levels (r = 0.07, p<.10).
Latent Growth Curve Modeling
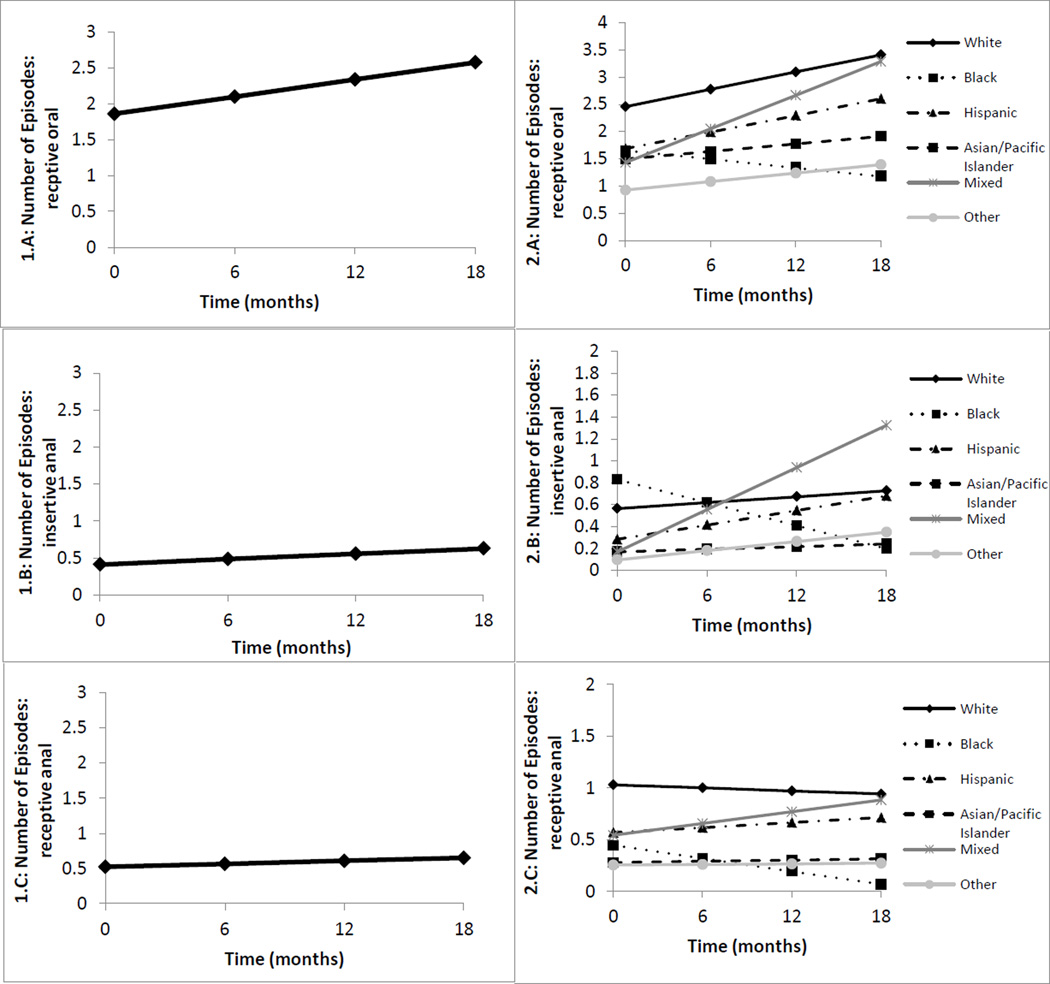
First, parameter estimates and goodness of fit statistics from the unconditional growth models investigating the simultaneous growth in receptive oral, insertive and receptive anal sex without a condom between baseline and the 18-month visit are presented in Table 3 (Model 1). Since intercepts and rates of change (slope) for all types of sexual activity were allowed to correlate, the average intercepts and rates of change for each type of sexual activity are interpreted as the average value of one type of sexual activity (e.g., receptive oral sex), controlling for the final level and rate of change in the other two types of sexual activity (e.g., insertive and receptive anal sex without a condom). Based on this modeling, all three types of sexual activity had statistically significant intercepts (p<0.001), indicating that there was engagement in receptive oral sex (b0 = 2.58, p < .001) as well as insertive anal sex ((b0 = 0.63, p < .001 and receptive anal sex (b0 = 0.65, p < .001) at the 18-month follow-up visit (i.e. the values were significant and non-zero). These results also show that there was statistically significant positive growth in the number of reported episodes of receptive oral sex as indicated by the significant slope (b1 = 0.04, p < .001) but no similar evidence of growth in the number of episodes of insertive and receptive anal sex without a condom over time (i.e., non significant slopes for the two anal sex behaviors). Trajectories for each of these unconditional growth models showing change in each type of sexual behaviors are presented in Figure 1 (panel 1.A, 1.B & 1.C).
Table 3.
Growth models for sexual behavior without a condom across time among participants in the P18 cohort study
| Model 1: Mean (SE) | Model 2: Mean (SE) | Model 3: Mean (SE) | |
|---|---|---|---|
| Receptive Oral, Intercept | 2.58***(0.167) | 3.41*** (0.307) | 2.76*** (0.630) |
| Black | - | −2.23*** (0.506) | −2.01*** (0.542) |
| Hispanic | - | −0.81* (0.405) | −0.64 (0.431) |
| API | - | −1.50+ (0.787) | −1.46+ (0.787) |
| Mixed Race | - | −0.13 (0.664) | −0.02 (0.669) |
| Other | - | −2.02* (0.898) | −1.87* (0.907) |
| SES | - | - | 0.27 (0.229) |
| Receptive Oral, Slope | 0.04***(0.011) | 0.05* (0.021) | 0.02(0.042) |
| Black | - | −0.08* (0.035) | −0.07+ (0.037) |
| Hispanic | - | −0.002 (0.028) | 0.01 (0.029) |
| API | - | −0.03 (0.054) | −0.03 (0.054) |
| Mixed Race | - | 0.05 (0.044) | 0.06 (0.044) |
| Other | - | −0.03 (0.061) | −0.02 (0.062) |
| SES | - | - | 0.01 (0.015) |
| Insertive anal, Intercept | 0.63*** (0.105) | 0.73*** (0.196) | 0.77+ (0.400) |
| Black | - | −0.53 (0.322) | −0.55 (0.344) |
| Hispanic | - | −0.05 (0.258) | −0.06 (0.274) |
| API | - | −0.49 (0.503) | −0.49 (0.504) |
| Mixed Race | - | 0.60 (0.419) | 0.59 (0.423) |
| Other | - | −0.38 (0.568) | −0.39 (0.574) |
| SES | - | - | −0.02 (0.145) |
| Insertive anal, Slope | 0.01 (0.007) | 0.01 (0.014) | −0.02 (0.028) |
| Black | - | −0.04+ (0.023) | −0.04 (0.025) |
| Hispanic | - | 0.01 (0.018) | 0.02 (0.019) |
| API | - | −0.01 (0.036) | −0.003 (0.036) |
| Mixed Race | - | 0.06+ (0.029) | 0.06* (0.029) |
| Other | - | 0.01 (0.040) | 0.01 (0.041) |
| SES | - | - | 0.01 (0.010) |
| Receptive anal, Intercept | 0.65*** (0.093) | 0.94*** (.174) | 0.87* (0.359) |
| Black | - | −0.87** (.288) | −0.85** (0.309) |
| Hispanic | - | −0.23 (.230) | −0.21 (0.245) |
| API | - | −0.63 (.447) | −0.62 (0.448) |
| Mixed Race | - | −0.06 (.378) | −0.05 (0.382) |
| Other | - | −0.67 (.510) | −0.65 (0.516) |
| SES | - | - | 0.03 (0.130) |
| Receptive anal, Slope | 0.01 (0.007) | 0.02+ (.013) | −0.01 (0.026) |
| Black | - | −0.04* (.021) | −0.03 (0.023) |
| Hispanic | - | −0.01 (.017) | −0.01 (0.018) |
| API | - | −0.02 (.033) | −0.02 (0.033) |
| Mixed Race | - | −0.002 (.027) | 0.004 (0.027) |
| Other | - | −0.02 (.037) | −0.01 (0.038) |
| SES | - | - | 0.01 (0.009) |
| Model Fit Statistics | |||
| Chi square | 1687.03*** | 583.09*** | 587.18*** |
| CFI | 0.68 | 0.69 | 0.69 |
| RMSEA | 0.13 | 0.10 | 0.10 |
p < .05;
p < .01;
p < .001;
p < .10
Figure 1.
Unconditional (panels 1.A, 1.B and 1.C) and conditional growth models (panels 2.A, 2.B and 2.C) displaying prototypical growth in receptive oral, insertive anal and receptive anal sex without a condom. Note that each trajectory controls for the final level and changes in all other sexual activities
Next, parameter estimates and goodness of fit statistics were estimated from models examining growth over time for each type of sexual activity conditioned on race/ethnicity (Table 3, Model 2). This model suggests that Black, Hispanic/Latino, API YMSM and those self-identifying as some other race reported engaging in significantly fewer episodes of oral receptive sex without a condom at the 18-month follow-up relative to White sexual minority youth (intercepts, b0 ranging from −0.81 to −2.23 with accompanying p’s raging from < .05 to < .001). Importantly, compared to White YMSM, receptive oral sexual activity without a condom for Black YMSM actually declined over time ((b1 = −0.08, p < .05). No other racial/ethnic differences in the rate of change in receptive oral sex without a condom were identified. Although there were no statistically significant racial/ethnic differences in either insertive or receptive anal sex without a condom at the 18-month follow-up, there was a marginal decline in the number of episodes of insertive anal sex without a condom over time among Black YMSM (b1 = −0.04, p < .10) while mixed race YMSM reported marginal increases in episodes of insertive anal sex without a condom between baseline and the 18-month follow-up (b1 = 0.06, p < .10). Additionally, frequency of of receptive anal sex without a condom over time significantly declined among Black YMSM (b1 = −0.04, p < .05) as compared to White MSM. No other racial/ethnic differences in insertive or receptive sexual activity were identified, suggesting that White, Hispanic, API and other race YMSM engaged in approximately equal numbers of episodes of insertive and receptive anal sex without a condom over time. Distinct prototypical growth trajectories for each type of sexual activity by race/ethnicity are displayed in Figure 1 (panels 2.A, 2.B & 2.C). These trajectories show declines for all three types of sexual activity among Black YMSM over time, while the number of sexual activity episodes (across type of activity) for all other racial/ethnic groups either increases slightly or remains relatively stable over time. It is also worth noting that in no case does a single racial/ethnic group demonstrate a higher growth trajectory for all three sexual activity variables, further supporting the notion that each group engages in very different activities across time.
Finally, an indicator for perceived familial SES was added to each latent growth model already conditioned on race/ethnicity (see Table 3, Model 3). These models show that after controlling for race/ethnicity, perceived familial socioeconomic status was not a statistically significant predictor of either final level or rate of change in receptive oral or insertive and receptive anal intercourse without a condom. However, it is interesting to note that after conditioning on perceived familial SES, the pattern of findings for race/ethnicity differed somewhat from models containing only race/ethnicity. For example, at the 18-month follow-up visit, White YMSM continued to engage in significantly higher levels of receptive oral sex relative to Black (b0 = −2.01, p < .001) and other race YMSM (b0 = −1.87, p < .05) and somewhat higher levels relative API ((b0 = −1.46, p < .10), but not Hispanic or mixed race men. In addition, after controlling for perceived familial SES, the rate of change in receptive oral sex for Black men declined relative to White YMSM as in Model 2 but the rate of decline was attenuated and become marginally significant (b1 = −0.07, p < .10). In addition, the rate of change in insertive anal sex without a condom among Black YMSM also became non-significant while increases over time were noted for mixed race YMSM (b1, = 0.06, p < .05) in models conditioned on both race/ethnicity and perceived familial SES.
Finally, controlling for perceived familial SES, there were no longer any racial/ethnic differences in receptive anal sex without a condom. As a final step, to investigate whether the effects of race/ethnicity on final level and rate of change in receptive oral, insertive and receptive anal sex without a condom over time differed by perceived familial SES, we added interaction terms between the three race/ethnicity variables and perceived familial SES to our growth models. No significant interactions were identified, suggesting the absence of effect measures modification between race/ethnicity and perceived familial SES on sexual activity among this sample of YMSM.
DISCUSSION
These longitudinal findings indicate that White and Mixed race YMSM tend to report greater likelihood of sexual behaviors without condoms compared to their Black and Hispanic/Latino counterparts [25] despite experiencing lower HIV and STI acquisition risk [26]. Further, these trends holds true over time indicating that racial/ethnic disparities in HIV and STI risk are not fully explained by sexual behaviors without condoms. As such, these longitudinal findings add greater support to those from prior, cross-sectional reports. Moreover, these findings show that declines in sexual behavior occurred across various types of sexual activity (oral sex, insertive and receptive anal sex) for Black YMSM compared to White YMSM. However, it is of interest to note that when controlling for perceived familial SES, differences in sexual activity by race/ethnicity were attenuated. Thus, these findings suggest that future studies ought to include measures of SES when assessing sexual behaviors given their association with social and financial inequalities, [27] homophobia and discrimination, [28] stigma [29] and structural inequalities [30] that are also major drivers of the HIV and STI epidemics in the US. [31]
The findings of fewer episodes of sexual behavior among YMSM of color is likely a reflection of the social and structural contexts within which these young men come of age and negotiate their sexuality. In particular, these contexts more often promote heteronormative behaviors, homophobia, and gay-related stigma and discrimination. Thus, the ability for young men of color to openly be in same-sex relationships, within which more regular or frequent sexual activity occurs, is minimized. This inability is also heightened among YMSM who come from familial backgrounds characterized by a lower SES where their familial contexts and home environments are also more likely to espouse homophobic or heteronormative attitudes and belief systems. Thus, the lack of ability to easily travel to other physical environments, beyond ones’ home environment, where experiences of gay-related stigma and discrimination are minimized, is likely to contribute to the fewer opportunities for same-sex relationships, and in turn, sexual activity. One would expect that in an urban setting, such as New York City, travel between different physical/social environments would be facilitated by the close proximity and high porosity of diverse neighborhoods as well as the availability of multiple forms of mass transit. However, for many men from lower SES backgrounds the lack of a reason to access other environments (due to fewer job options, fewer contacts/friends in other neighborhoods, a lack of familiarity with other spaces, etc) may reinforce the lack of ability to engage openly in same-sex relationships. Whereas, White YMSM and those form higher SES backgrounds, are less likely to experience gay related stigma and discrimination and consequently more able to form and maintain same-sex relationships. This, in turn, is likely to support the ability to engage in more frequent episodes of sexual activity reported by YMSM from these more advantaged groups. Thus, the overlapping and entangled forces of race/ethnicity and SES have broad reaching impact on the social, structural and behavioral realities of YMSM who are simultaneously emerging into adulthood and negotiating their sexuality and sexual experiences. When taken together, an understanding of their myriad effects allows for targeted prevention and intervention messaging that acknowledges the realities of the lived experiences of this racially/ethnically and socioeconomically diverse population.
Prior to drawing final conclusions, study limitations and strengths merit consideration. First, data on sexual activity are self-reported and subject to social desirability responding as these data were collected via interviewer-administered assessments. However, if episodes of sexual activity without a condom were more likely to be under-reported, these findings would be underestimated and biased toward the null. Second, the 30 day recall period may also lead to under-reporting of sexual activity. However, by ascertaining information on sexual activity over a shorter duration, the accuracy of recall as well as condom use during these episodes of sexual activity are likely to be greater than for longer (i.e. 3 month or 6 month) recall periods. Next, our data on condom use is per episode rather than based on generalizations or averages (i.e. all the time, less than all the time, etc.) over a period of recall. Thus, the information on unprotected sex acts is likely to be a more accurate reflection of true sexual behaviors. However, the large study sample size, high-levels of retention across study visits and the inclusion of all three sexual behaviors in LGC models minimize these concerns.
In conclusion, future investigations of HIV disparities in YMSM must move beyond the sole focus on person-level behaviors and frequency of sex acts as embodied in most social cognitive models.17 Understanding the drivers of HIV/STI risk in young sexual and racially minority is predicated on more than just behavior and must be understood in relation to the social and structural drivers that may place these young men at risk for HIV/STIs and other health disparities. In addition, prevention and intervention efforts that acknowledge these multiple and complicated forces that shape the sexual experiences of YMSM will be better suited and more effective at providing HIV/STI prevention and intervention techniques. Such efforts ought to harness this information and knowledge to positively shape the sexual health and well being of a new generation of YMSM.
Acknowledgments
This study was funded by the National Institute on Drug Abuse, Contract #R01DA025537.
References
- 1.CDC HIV Surveillance Report. http://www.cdc.gov/hiv/library/slideSets/index.html?utm_source=feedburner&utm_medium=feed&utm_campaign=Feed%3A+pkidshivnews+(PKIDs'+HIV%2FAIDS+News)
- 2.New York City Department of Health and Mental Health. HIV epidemiology & field services semiannual report. 2012;7(1):1–4. http://www.nyc.gov/html/doh/downloads/pdf/dires/2012-1st-semi-rpt.pdf. [Google Scholar]
- 3.Centers for Disease Control and Prevention. Sexually Transmitted Disease Surveillance 2011. Atlanta: U.S. Department of Health and Human Services; 2012. [Google Scholar]
- 4.Katz MH, Schwarcz SK, Kellogg TA, et al. Impact of highly active antiretroviral treatment on HIV seroincidence among men who have sex with men: San Francisco. Am J Public Health. 2002;92(3):388–394. doi: 10.2105/ajph.92.3.388. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Chen SY, Gibson S, Katz MH, et al. Continuing increases in sexual risk behavior and sexually transmitted diseases among men who have sex with men: San Francisco, CA, 1999–2001. Am J Public Health. 2002;92(9):1387–1388. [PMC free article] [PubMed] [Google Scholar]
- 6.Chen SY, Gibson S, Weide D, McFarland W. Unprotected anal intercourse between potentially HIV-serodiscordant men who have sex with men, san francisco. J Acquir Immune Defic Syndr. 2003;33(2):166–170. doi: 10.1097/00126334-200306010-00008. [DOI] [PubMed] [Google Scholar]
- 7.Ciesielski CA. Sexually transmitted diseases in men who have sex with men: An epidemiologic review. Curr Infect Dis Rep. 2003;5(2):145–152. doi: 10.1007/s11908-003-0051-5. [DOI] [PubMed] [Google Scholar]
- 8.Leichliter JS, Haderxhanaj LT, Chesson HW, Aral SO. Temporal trends in sexual behavior among men who have sex with men in the united states, 2002 to 2006–2010. JAIDS J Acquired Immune Defic Syndromes. 2013;63(2):254–258. doi: 10.1097/QAI.0b013e31828e0cfc. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Crepaz N, Marks G, Liau A, et al. Prevalence of unprotected anal intercourse among HIV-diagnosed MSM in the United States: a meta-analysis. AIDS. 2009;23:1617–1629. doi: 10.1097/QAD.0b013e32832effae. [DOI] [PubMed] [Google Scholar]
- 10.Arnett J. Reckless behavior in adolescence: A developmental perspective. Developmental review. 1992;12(4):339–373. [Google Scholar]
- 11.Halkitis PN, Brockwell S, Siconolfi DE, et al. Sexual behaviors of emerging adolescent and young adult men who have sex with men ages 13–29 in New York City. J Acquir Immune Defic Syndr. 2011;56:285–291. doi: 10.1097/QAI.0b013e318204194c. [DOI] [PubMed] [Google Scholar]
- 12.Ayala G, Bingham T, Kim J, Wheeler DP, Millett GA. Modeling the impact of social discrimination and financial hardship on the sexual risk of HIV among Latino and Black men who have sex with men. Am J Public Health. 2012;102(Suppl 2):S242–S249. doi: 10.2105/AJPH.2011.300641. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Millett GA, Peterson JL, Flores SA, et al. Comparisons of disparities and risks of HIV infection in black and other men who have sex with men in Canada, UK, and USA: a meta-analysis. Lancet. 2012;380:341–348. doi: 10.1016/S0140-6736(12)60899-X. [DOI] [PubMed] [Google Scholar]
- 14.Millett GA, Peterson JL, Wolitski RJ, Stall R. Greater risk for HIV infection of black men who have sex with men: a critical literature review. Am J Public Health. 2006;96:1007–1019. doi: 10.2105/AJPH.2005.066720. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Millett GA, Jeffries WL, Peterson JL, et al. Common roots: a contextual review of HIV epidemics in black men who have sex with men across the African diaspora. Lancet. 2012;380:411–423. doi: 10.1016/S0140-6736(12)60722-3. [DOI] [PubMed] [Google Scholar]
- 16.Garofalo R, Mustanski B, Johnson A, Emerson E. Exploring factors that underlie racial/ethnic disparities in HIV risk among young men who have sex with men. Journal of Urban Health. 2010;87(2):318–323. doi: 10.1007/s11524-009-9430-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Harawa NT, Greenland S, Bingham TA, et al. Associations of race/ethnicity with HIV prevalence and HIV-related behaviors among young men who have sex with men in 7 urban centers in the united states. JAIDS J Acquired Immune Defic Syndromes. 2004;35(5):526–536. doi: 10.1097/00126334-200404150-00011. [DOI] [PubMed] [Google Scholar]
- 18.Capaldi DM, Stoolmiller M, Clark S, Owen LD. Heterosexual risk behaviors in at-risk young men from early adolescence to young adulthood: Prevalence, prediction, and association with STD contraction. Dev Psychol. 2002;38(3):394–406. doi: 10.1037//0012-1649.38.3.394. [DOI] [PubMed] [Google Scholar]
- 19.Anderson C, Galinsky AD. Power, optimism, and risk-taking. European journal of social psychology. 2006;36(4):511–536. [Google Scholar]
- 20.Centers for Disease Control and Prevention (CDC) HIV among gay, bisexual, and other men who have sex with men: Fact sheet. [Accessed December 16, 2014]; http://www.cdc.gov/hiv/risk/gender/msm/facts/index.html. Updated September 26, 2013.
- 21.Rosario M, Schrimshaw EW, Hunter J. A model of sexual risk behaviors among young gay and bisexual men: Longitudinal associations of mental health, substance abuse, sexual abuse, and the coming-out process. AIDS education and prevention: official publication of the International Society for AIDS Education. 2006;18(5):444. doi: 10.1521/aeap.2006.18.5.444. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Halkitis PN, Figueroa RP. Sociodemographic characteristics explain differences in unprotected sexual behavior among young HIV-negative gay, bisexual, and other YMSM in new york city. AIDS Patient Care STDS. 2013;27(3):181–190. doi: 10.1089/apc.2012.0415. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Halkitis PN, Kapadia F, Siconolfi DE, et al. Individual, psychosocial, and social correlates of unprotected anal intercourse in a new generation of young men who have sex with men in New York City. Am J Public Health. 2013;103:889–895. doi: 10.2105/AJPH.2012.300963. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Robinson SM, Sobell LC, Sobell MB, Leo GI. Reliability of the Timeline Followback for cocaine, cannabis, and cigarette use. Psychol Addict Behav. 2014;28:154–162. doi: 10.1037/a0030992. [DOI] [PubMed] [Google Scholar]
- 25.Millett GA, Peterson JL, Wolitski RJ, Stall R. Greater risk for HIV infection of black men who have sex with men: a critical literature review. Am J Public Health. 2006;96:1007–1019. doi: 10.2105/AJPH.2005.066720. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Halkitis PN, Brockwell S, Siconolfi DE, et al. Sexual behaviors of adolescent emerging and young adult men who have sex with men ages 13–29 in New York City. J Acquir Immune Defic Syndr. 2011;56:285–291. doi: 10.1097/QAI.0b013e318204194c. [DOI] [PubMed] [Google Scholar]
- 27.Ayala G, Bingham T, Kim J, Wheeler DP, Millett GA. Modeling the impact of social discrimination and financial hardship on the sexual risk of HIV among Latino and Black men who have sex with men. Am J Public Health. 2012;102(Suppl 2):S242–S249. doi: 10.2105/AJPH.2011.300641. Epub@2012 Mar 8.:S242–S249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Millett GA, Jeffries WL, Peterson JL, et al. Common roots: a contextual review of HIV epidemics in black men who have sex with men across the African diaspora. Lancet. 2012;380:411–423. doi: 10.1016/S0140-6736(12)60722-3. [DOI] [PubMed] [Google Scholar]
- 29.Hatzenbuehler ML, Phelan JC, Link BG. Stigma as a fundamental cause of population health inequalities. Am J Public Health. 2013;103:813–821. doi: 10.2105/AJPH.2012.301069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Halkitis PN. Obama, marriage equality, and the health of gay men. Am J Public Health. 2012;102:1628–1629. doi: 10.2105/AJPH.2012.300940. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Halkitis PN, Wolitski RJ, Millett GA. A holistic approach to addressing HIV infection disparities in gay, bisexual, and other men who have sex with men. Am Psychol. 2013;68:261–273. doi: 10.1037/a0032746. [DOI] [PubMed] [Google Scholar]
- 32.Halkitis PN. Reframing HIV prevention for gay men in the United States. Am Psychol. 2010;65:752–763. doi: 10.1037/0003-066X.65.8.752. [DOI] [PubMed] [Google Scholar]