Abstract
Background
Respiratory and diarrheal diseases are leading causes of morbidity and mortality among children younger than 5 years in developing countries. Data on the burden of these diseases in Haiti are scarce.
Methods
We conducted a retrospective review of hospital admission registries during January 1, 2011–December 31, 2013 for children younger than 5 years in 6 hospitals in Haiti. We recorded the number of all-cause, respiratory and diarrheal disease admissions and deaths by epidemiologic week and age.
Results
A total of 31,565 hospital admissions and 1763 deaths were recorded among children aged <5 years during the study period. Respiratory diseases accounted for 9183 (29%) hospitalizations and 301 (17%) deaths. Children aged 6–23 months had the highest percentage of hospitalizations attributable to respiratory diseases (38%), whereas children aged 36–47 months had the highest proportion of deaths attributable to respiratory diseases (37%). Respiratory disease hospitalizations followed a bimodal seasonal pattern, with peaks during May–June and October–December. Diarrheal diseases accounted for 8063 (26%) hospitalizations and 224 (13%) deaths. Children aged 6–11 months had the highest percentage of diarrhea-associated hospitalizations (39%) and deaths (29%). Diarrheal disease admissions peaked in January–April before the rainy season.
Conclusions
Respiratory and diarrheal diseases contributed to more than half of hospitalizations and almost a third of deaths in children younger than 5 years in Haiti. These data are essential to assess the impact of pneumococcal and rotavirus vaccines and other interventions in Haiti.
Keywords: hospitalizations, diarrheal disease, respiratory disease, children, Haiti, deaths
Respiratory and diarrheal diseases are the leading causes of morbidity and mortality among children younger than 5 years in developing countries. Worldwide, respiratory diseases account for approximately 1 million deaths and diarrheal diseases for 0.6 million deaths among children aged <5 years.1–4 Rotavirus and Streptococcus pneumoniae are the most common vaccine-preventable causes of severe diarrheal and respiratory diseases in children aged <5 years, contributing to 28% and 18% of diarrheal and respiratory infections, respectively.5 The Global Enteric Multicenter Study (GEMS) showed that rotavirus is the most common cause of moderate-to-severe diarrhea among children younger than 1 year worldwide and is a leading cause of diarrheal disease in children younger than 5 years.2 In addition, rotavirus contributes to almost 30% of diarrheal deaths in children aged <5 years.3 A recent study estimated that S. pneumoniae causes around 11% (8–12%) of all deaths in children <5 years, with a global incidence of pneumococcal pneumonia of 13.8 million cases in children <5 years in the year 2000.4 Given the extensive burden of vaccine-preventable diarrheal and respiratory diseases, the World Health Organization recommends vaccination with rotavirus and pneumococcal conjugate vaccines.6,7
Haiti, located on the island of Hispaniola, is administratively divided into 10 departments and has a population of approximately 10.5 million persons.8 More than a third of the population lives in the Ouest department, which includes metropolitan Port-au-Prince.8 The number of children <5 years of age was estimated as 1.3 million in 20129; mortality for this age group is approximately 73 children per 1000 live births.10 According to the 2012 demographic and health survey, 45% of children have received all recommended vaccines in the routine immunization program (Bacillus Calmette-Guerin [BCG], Diphtheria,Tetanus, Pertussis [DTP], polio, measles and rubella [MR]) by the age of 23 months.11 Haemophilus influenzae type b (Hib) vaccine was introduced in 2012; rotavirus vaccine was introduced in April 2014, and pneumococcal conjugate vaccine will be introduced in 2016.
Nevertheless, baseline data on the burden of respiratory and diarrheal diseases among children in Haiti are scarce, particularly for those age groups targeted for vaccination. We assessed the baseline burden of respiratory and diarrheal disease hospitalizations and deaths among children aged <5 years at 6 major hospitals in Haiti during 2011–2013, before rotavirus and pneumococcal vaccine introduction. These results can be compared with future data on burden of these diseases to help evaluate the impact of vaccines targeting these diseases.
MATERIALS AND METHODS
Site Selection
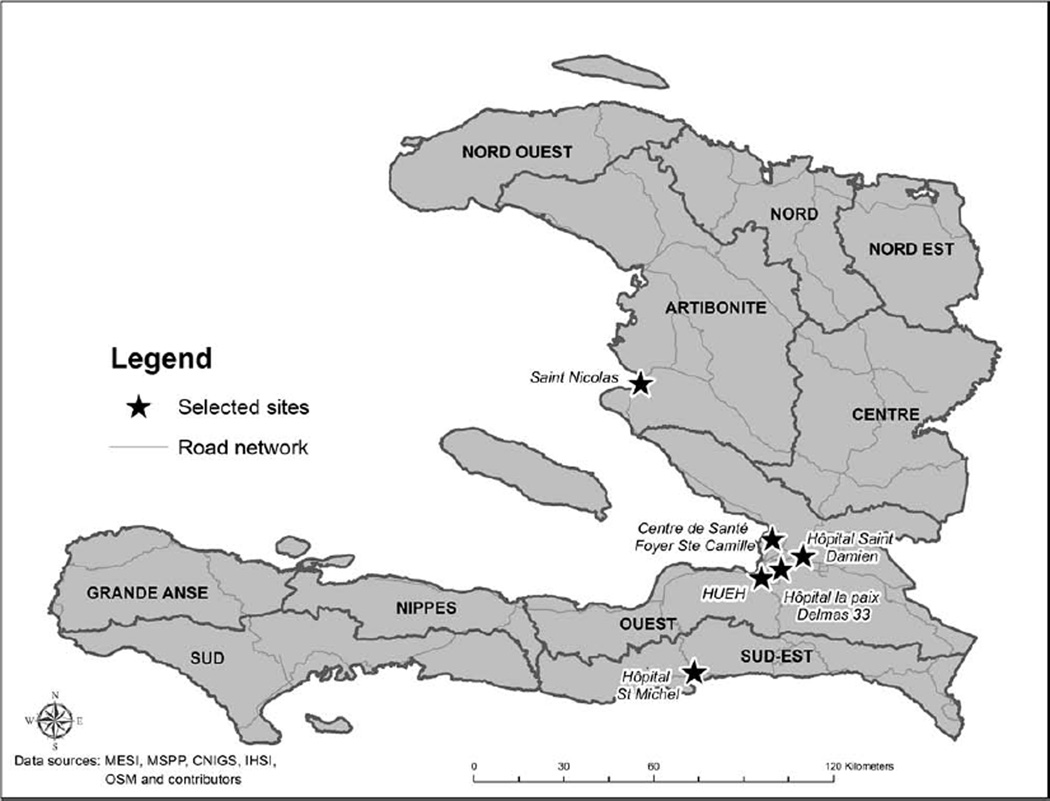
Six major hospitals were selected for this study based on their pediatric patient load and geographic distribution (Fig. 1). Four of the selected hospitals are located in Port-au-Prince where almost a third of the population resides and where patients with moderate to severe conditions get admitted: Hôpital de l’Université de l’Etat d’Haiti (HUEH, public hospital), Hôpital Saint Damien (HSD, private nonprofit hospital), Hôpital Universitaire de la Paix (public hospital) and Hôpital Saint Camille (HSC, private nonprofit hospital). Hôpital Saint Nicolas (public hospital) is in the Artibonite department and Hôpital Saint Michel de Jacmel (SMJ, public hospital) is in the South-East department. Of all the 6 sites, only HSD is an exclusively pediatric hospital.
FIGURE 1.
Location of the 6 hospitals visited for the collection of information on diarrheal and respiratory diseases in children younger than 5 years, Haiti 2011–2013.
Data Collection
We conducted a retrospective review of registries of admission to pediatric wards during January 1, 2011–December 31, 2013 in each of the selected hospitals. These registries typically include patient age (and/or date of birth), sex, admission date, discharge date, main diagnosis on admission and/or discharge and disposition (ie, deceased, discharged, transferred). In each hospital, we recorded the number of all-cause, respiratory and diarrheal admissions and deaths in children by age groups (in months: 0–5, 6–11, 12–23, 24–35, 36–47, 48–59) and epidemiologic week. Patients with both respiratory and diarrheal diagnoses were counted as both respiratory and diarrheal cases, but counted only once toward total admission numbers. When available, we used the discharge diagnosis instead of the admitting diagnosis to identify patients who fulfilled the case definitions for respiratory or diarrheal diseases. Any death associated with an admission diagnosis that met criteria for respiratory or diarrheal disease classification was coded as a death attributable to the admitting diagnosis if no other cause of death was listed.
Case Definitions
We included a number of clinical diagnoses in our definitions of respiratory and diarrheal diseases (Table 1). We used broad case definitions to capture all potential cases of respiratory and diarrheal diseases, and we consulted with hospital clinicians to ensure that we had a thorough understanding of certain diagnoses. For example, we included parasitosis in our case definition of diarrheal disease to be consistent with previous studies that assessed diarrhea-associated hospitalizations in the US12,13 and following conversations with Haitian clinicians who confirmed that parasitosis is used to describe patients with diarrhea without laboratory evidence.
TABLE 1.
Case Definitions of Respiratory and Diarrheal Diseases Used for Data Abstraction, Haiti 2011–2013
| Respiratory Disease | Diarrheal Disease |
|---|---|
| Acute respiratory illness | Diarrhea |
| Pneumonia, bronchopneumonia, viral pneumonia | Acute gastroenteritis (febrile or afebrile) |
| Pneumonitis | Gastroenteritis (febrile or afebrile) |
| Bronchitis (acute, chronic) | |
| (Acute) bronchiolitis | Dehydration |
| (Acute) sinusitis | Parasitosis |
| (Acute) epiglottitis | Cholera |
| (Acute) tracheitis | Amoebiasis |
| (Acute) viral rhinitis | Dysentery |
| Bronchiectasis | Shigellosis |
| Pharyngitis | Giardiasis |
| Laryngotracheitis | Food poisoning |
| Croup | Hypovolemic shock (unless other causes of hypovolemia were noted) |
| Diphtheria | |
| Influenza, flu-like symptoms | |
| Asthma, asthma exacerbation, status asthmaticus | |
| Pleural effusion | |
| Empyema | |
| Pleurisy | |
| Apnea | |
| Shortness of breath | |
| Tachypnea | |
| Wheezing | |
| Stridor | |
| Cough | |
| Respiratory failure, respiratory distress |
Data Analysis
Data were entered into a Microsoft Office Excel 2007 (Microsoft Corporation, Redmond, WA) database. We calculated the percentage of children who were hospitalized for and died from respiratory and diarrheal diseases by age group and hospital. For this calculation, the number of children hospitalized for each of these conditions in each age group and hospital was divided by the total number of hospitalizations in the corresponding age group and hospital, respectively. We assessed the seasonality of respiratory and diarrheal disease by presenting the number and percentage of hospitalizations associated with these syndromes by epidemiologic week during each year in the study period. Analyses for differences in percentages of hospitalizations by age, year and hospital were computed using χ2 for trend. A P value <0.05 was considered statistically significant. Analyses were computed using SAS v.9.3 (SAS Institute Inc., Cary, NC).
Ethics Statement
This study was approved by the Haiti National Bioethics Committee. The protocol was judged not to constitute human subjects research (routine surveillance activity) by the Human Subjects Protection Office at Centers for Disease Control and Prevention and therefore determined to be exempt from review by the institutional review board at Centers for Disease Control and Prevention.
RESULTS
General Characteristics of Hospitalized Children
During January 1, 2011–December 31, 2013, a total of 31,565 children <5 years of age were recorded as hospitalized at the 6 hospitals (Table 2). Of note, 1014 (3%) registry entries lacked information on age and/or diagnosis; hence, these were not included in the total count. Children aged 0–11 months accounted for 60%, and children aged <24 months accounted for 80% of hospitalized children aged <5 years. Of the 6 hospitals, HUEH and HSD had the highest numbers of hospitalized children from 2011 to 2013, accounting for 8569 (27%) and 9466 (30%) of the total hospitalizations, respectively. Among hospitalized children aged <5 years, 1763 (6%) deaths were recorded during 2011–2013.
TABLE 2.
Total Hospitalizations Among Children Aged <5 Years at 6 Major Hospitals, Haiti 2011–2013
| 2011–2013 | 2011 | 2012 | 2013 | |
|---|---|---|---|---|
| Year | n (%) | n (%) | n (%) | n (%) |
| Age (mo) | ||||
| 0–5 | 13,402 (42) | 3943 (46) | 4935 (41) | 4524 (41) |
| 6–11 | 5606 (18) | 1438 (17) | 2336 (19) | 1832 (17) |
| 12–23 | 6294 (20) | 1635 (19) | 2419 (20) | 2240 (20) |
| 24–35 | 3068 (10) | 805 (9) | 1112 (9) | 1151 (11) |
| 36–47 | 1923 (6) | 466 (5) | 736 (6) | 721 (7) |
| 48–59 | 1272 (4) | 300 (3) | 506 (4) | 466 (4) |
| Hospital | ||||
| HUEH | 8569 (27) | 2052 (24) | 3792 (31) | 2725 (25) |
| HSD | 9466 (30) | 3045 (35) | 3411 (28) | 3010 (27) |
| HUP | 1830 (6) | 328 (4) | 776 (6) | 726 (7) |
| HSC | 3749 (12) | 1030 (12) | 1434 (12) | 1285 (12) |
| HSN | 5652 (18) | 1512 (18) | 1883 (16) | 2257 (21) |
| SMJ | 2299 (7) | 620 (7) | 748 (6) | 931 (8) |
| Total | 31,565 (100) | 8587 (100) | 12,044 (100) | 10,934 (100) |
HSC indicates Hôpital Saint Camille; HSD, Hôpital Saint Damien; HSN, Hôpital Saint Nicolas; HUEH, Hôpital de l’Université de l’Etat d’Haiti; HUP, Hôpital Universitaire de la Paix; SMJ, Hôpital Saint Michel de Jacmel.
Respiratory Diseases Hospitalizations and Deaths
During 2011–2013, a total of 9183 children aged <5 years were hospitalized for respiratory diseases, accounting for 29% of the overall hospitalizations (Table 3). The overall percentage of hospitalizations attributable to respiratory diseases was 27% in 2011 and 31% in 2013. Children aged <24 months accounted for 6856 (76%) of total respiratory hospitalizations. The percentage of hospitalizations attributable to respiratory diseases was similar across age groups (33%–38%), with the exception of 0–5 month olds which had a significantly lower percentage of hospitalizations attributable to respiratory diseases (19%) compared with other age groups (P < 0.001).
TABLE 3.
Percentage of Hospitalizations Associated With Respiratory and Diarrheal Diseases* Among Children Aged <5 Years at 6 Major Hospitals, Haiti 2011–2013
| Respiratory Diseases | Diarrheal Diseases | |||||||
|---|---|---|---|---|---|---|---|---|
| 2011–2013 | 2011 | 2012 | 2013 | 2011–2013 | 2011 | 2012 | 2013 | |
| Year | n (%) | n (%) | n (%) | n (%) | n (%) | n (%) | n (%) | n (%) |
| Age (mo) | ||||||||
| 0–5 | 2482 (19) | 708 (18) | 881 (18) | 893 (20) | 1983 (15) | 537 (14) | 798 (16) | 648 (14) |
| 6–11 | 2104 (38) | 523 (36) | 883 (38) | 698 (38) | 2199 (39) | 509 (35) | 955 (41) | 735 (40) |
| 12–23 | 2370 (38) | 585 (36) | 880 (36) | 905 (40) | 2285 (36) | 516 (32) | 964 (40) | 805 (36) |
| 24–35 | 1098 (36) | 273 (34) | 405 (36) | 420 (36) | 861 (28) | 199 (25) | 328 (29) | 334 (29) |
| 36–47 | 712 (37) | 140 (30) | 278 (38) | 294 (41) | 432 (22) | 95 (20) | 182 (24) | 155 (21) |
| 48–59 | 417 (33) | 96 (32) | 174 (34) | 147 (32) | 303 (24) | 58 (19) | 129 (25) | 116 (25) |
| Hospital | ||||||||
| HUP | 525 (29) | 90 (27) | 226 (29) | 209 (29) | 702 (38) | 114 (35) | 309 (40) | 279 (38) |
| HSC | 964 (26) | 310 (30) | 366 (26) | 288 (22) | 1921 (51) | 441 (43) | 841 (59) | 639 (50) |
| HSN | 1167 (21) | 313 (21) | 365 (19) | 489 (22) | 1695 (30) | 510 (34) | 629 (33) | 556 (25) |
| SMJ | 405 (18) | 118 (19) | 152 (20) | 135 (15) | 356 (15) | 73 (12) | 125 (17) | 158 (17) |
| HUEH | 3628 (42) | 760 (37) | 1508 (40) | 1360 (50) | 2249 (26) | 486 (24) | 1040 (27) | 723 (27) |
| HSD | 2494 (26) | 734 (24) | 884 (26) | 876 (29) | 1140 (12) | 290 (10) | 412 (12) | 438 (15) |
| Total | 9183 (29) | 2325 (27) | 3501 (29) | 3357 (31) | 8063 (26) | 1914 (22) | 3356 (28) | 2293 (26) |
Percentages reflect the overall percentage of respiratory-associated or diarrhea-associated hospitalizations out of all hospitalizations in a certain age group or hospital.
HSC indicates Hôpital Saint Camille; HSD, Hôpital Saint Damien; HSN, Hôpital Saint Nicolas; HUEH, Hôpital de l’Université de l’Etat d’Haiti; HUP, Hôpital Universitaire de la Paix; SMJ, Hôpital Saint Michel de Jacmel.
The percentage of hospitalizations associated with respiratory diseases varied by hospital, ranging from 18% (405) at SMJ to 42% (3628) at HUEH (P < 0.001). Moreover, the percentage of hospitalizations attributable to respiratory disease increased from 37% in 2011 to 50% in 2013 at HUEH, the largest public hospital in Haiti. Respiratory disease hospitalizations followed a bimodal pattern, with recurrent peaks in number of admissions and percentage of respiratory-associated hospitalizations observed from May through June and October through December (Fig. 2).
FIGURE 2.
Respiratory disease hospitalization among children younger than 5 years at 6 major hospitals by epidemiologic week, Haiti 2011–2013.
Of the 9183 children admitted with a respiratory disease, 301 (3.3%) died, which represented 17% of the 1763 deaths among children aged <5 years hospitalized during 2011–2013. The percentage of deaths from respiratory diseases did not vary by year (17–18%). The percent of total deaths in each age group because of respiratory diseases was 29% for children aged 6–23 months, 32% for those aged 24–35 months and 37% for those 36–47 months. Children aged <6 months and 48–59 months had the lowest percentages of deaths attributed to respiratory disease (12% and 14%, respectively), despite making up 46% of hospital admissions and 70% of total deaths.
Diarrheal Diseases Hospitalizations and Deaths
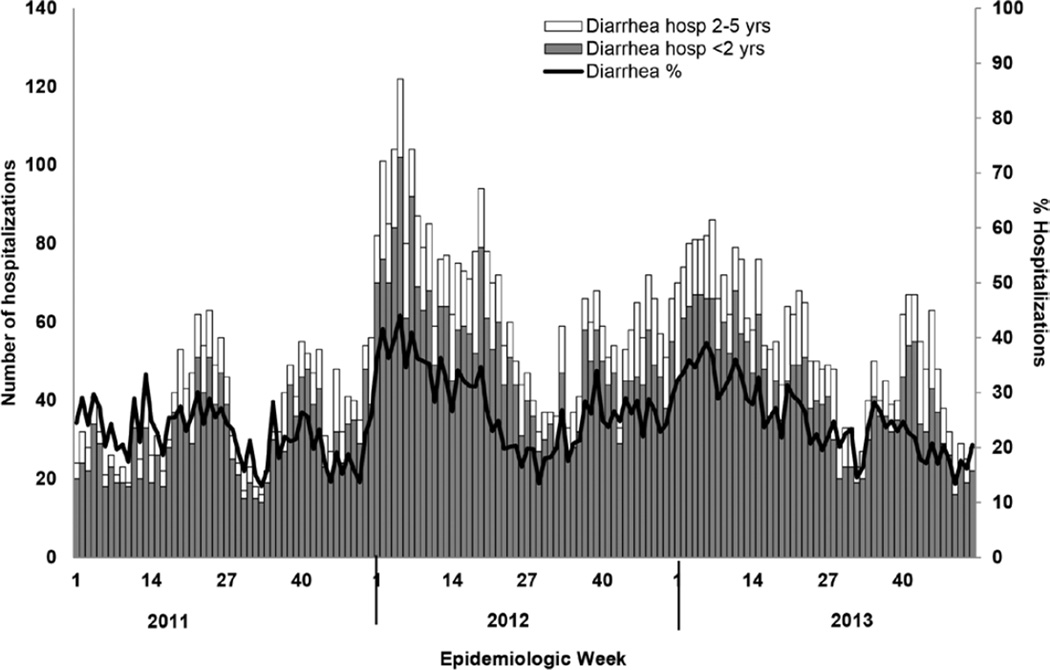
During the 3-year period, a total of 8063 children aged<5 years were hospitalized for diarrheal disease accounting for 26% of the overall hospitalizations (Table 3). This percentage varied over the study years, ranging from 22% in 2011 to 28% in 2012. Eighty percent of hospitalizations attributable to diarrheal disease occurred among children aged <24 months. Children aged 6–11 months had a significantly higher proportion of hospitalizations for diarrheal diseases (39%) compared with the other age groups (P < 0.001). Variation in the percentage of total hospitalizations attributable to diarrheal diseases was also noted between hospitals, ranging from 12% of all hospitalizations at HSD to 51% at HSC (P < 0.001; Table 3). During 2012 and 2013, the total number of diarrheal hospitalizations and the relative percentage of diarrhea-associated hospitalizations peaked from January to April (Fig. 3). In 2011, however, there were multiple small peaks in January, March, June, August and October.
FIGURE 3.
Diarrheal disease hospitalization among children younger than 5 years at 6 major hospitals by epidemiologic week, Haiti 2011–2013.
Of the 8063 children aged <5 years admitted with a diarrheal disease during 2011–2013, 224 (2.7%) died, which represented 13% of 1763 deaths reported among all age groups. The percentage of deaths because of diarrheal disease was 11%, 18% and 10% of all deaths in 2011, 2012 and 2013, respectively. The highest percentage of deaths because of diarrheal diseases occurred among children aged 6–11 months (29%) followed by children aged 12–23 months (26%) and 24–35 months (24%). The lowest percentages of deaths attributed to diarrheal disease were among children aged <6 months (7%) and 48–59 months (14%).
DISCUSSION
We found that respiratory and diarrheal diseases together contributed to more than half of hospitalizations (55%) and almost a third of deaths (30%) among children aged <5 years at 6 major hospitals in Haiti during 2011–2013. These findings are consistent with previous studies that have found diarrheal and respiratory diseases to be key contributors to pediatric morbidity and mortality in developing countries.1,5 Review of hospital records and syndromic surveillance has been shown to be useful to assess the impact of the vaccines.14 Therefore, our findings may serve as baseline for future assessment of the potential impact of Hib vaccine (introduced in 2012), rotavirus vaccine (introduced in 2014) and pneumococcal vaccine (planned introduction in 2016) in reducing the burden of hospitalizations and deaths in children in Haiti. Hib and pneumococcal vaccines resulted in significant reductions in the burden of respiratory diseases in developing countries; pneumococcal vaccine resulted in a 29% reduction in radiologically confirmed pneumonia and an 11% reduction in severe pneumonia, whereas Hib vaccine resulted in a 6% reduction in severe pneumonia and a 7% reduction in pneumonia mortality.15,16 In South Africa, pneumococcal vaccines resulted in a 69% reduction in incidence of invasive pneumococcal disease.17 Rotavirus vaccine has been shown to be 47% effective in reducing hospital admissions because of rotavirus infection and was 61% effective in reducing severe rotavirus infections based on a meta-analysis of studies conducted in several countries.15,18 In Mexico, rotavirus vaccine contributed to a 38% reduction in diarrhea-associated hospitalization19 and 50% reduction in diarrhea-related mortality.20
Although children aged 0–5 months constituted 42% of all hospitalizations, the percentage of hospitalizations attributable to respiratory and diarrheal disease in this age group was 19% and 15%, respectively, the lowest among all age groups. This finding likely reflects the burden of other perinatal infections and prematurity in the neonatal population and the protective effects of breastfeeding in decreasing diarrheal and respiratory diseases.15 In contrast, children aged 6–11 months and those aged 6–23 months had the highest percentage of respiratory and diarrheal diseases hospitalization and deaths. Therefore, the introduction of pneumococcal conjugate vaccine-13 at the schedule of 6, 10 and 14 weeks of age and rotavirus vaccine at 6 and 10 weeks of age is expected to have a major impact in reducing the burden of respiratory and diarrheal disease hospitalizations in children aged 6–23 months.
Respiratory disease hospitalizations followed a bimodal pattern, with peaks during May–June and October–December, coinciding with the rainy and cyclonic seasons, times of highest rainfall.21 This may support findings by Dowell et al22 showing increased incidence of pneumococcal disease during times of seasonal change in the US. Predominance of respiratory tract infections during the rainy season has been reported in tropical climates,23,24 and high rates of pneumonia deaths among children were also reported in Kenya during the rainy season.25 However, more years of respiratory surveillance should be undertaken to better understand the seasonality of respiratory diseases, and the addition of laboratory testing would be helpful to understand the etiologies of respiratory infections in Haiti.
Unlike cholera, which tends to peak during the rainy seasons, which corresponds to May–June and October–December in Haiti, diarrheal diseases in Haitian children aged <5 years peaked during the dry season mainly in January–April, which is similar to trends in rotavirus disease seen in other tropical countries.26 These observations might suggest the contribution of rotavirus infection to diarrheal disease hospitalizations among children in Haiti. Although cholera might have contributed to an increase in diarrheal disease hospitalizations among children in Haiti, studies have shown that hospitalizations for cholera were significantly lower in pediatric wards compared with cholera treatment centers (6% vs. 56%)27; hence, our data might not be considerably affected by the cholera epidemic as we reviewed registers of children admitted to the pediatric wards. However, the multiple peaks of diarrheal hospitalizations in 2011 might be related to the increase in cholera admissions among younger children as not all cholera treatment centers might have been operational soon after the start of the cholera outbreak.
The variation in hospitalization patterns for respiratory and diarrheal diseases between hospitals might have various reasons. Although HSD, a large private pediatric hospital in Port-au-Prince, contributed to almost a third of hospitalizations of children aged <5 years during 2011–2013, only 12% of hospitalizations were attributable to diarrheal disease. In contrast, HSC, a private hospital with a smaller pediatric ward in Port-au-Prince, contributed to only 12% of total hospitalizations, yet 51% of hospitalizations at this site were attributable to diarrheal disease. This observation might be explained by the fact that HSC is located close to the largest slum in Haiti, which has poor sanitary conditions. Similarly, the percentage of hospitalizations attributable to respiratory disease ranged from 18% at SMJ, located in South-East department, to 42% at HUEH, the largest public hospital in Haiti. Some of the largest tertiary hospitals are located in Port-au-Prince where children with severe respiratory and diarrheal diseases might get referred, leading to a relatively higher percentage of hospitalizations for these diseases in the capital. Finally, these variations might be attributable to geographic variation in respiratory or diarrheal diseases burden in Haitian children.
This study has several limitations. First, it relied on handwritten patient registries, which were inconsistently maintained and completed at different hospitals. There was also no uniformity in the way diagnoses were written; the language used to describe each diagnosis was often left to the discretion of the healthcare provider completing the registry. Second, the diagnoses used for respiratory infection are nonspecific; many might reflect noninfectious causes and several might be because of viral infection rather than bacterial pneumonias. Third, deaths were inconsistently recorded and cause of death was almost never recorded. At HUEH, one of the largest sites, patients who died soon after arrival to the hospital were almost never given a diagnosis in the registry; hence rates of diarrheal and respiratory deaths were likely underestimated at this hospital. Fourth, as most of the 6 hospitals included in the study are large tertiary hospitals located in Metropolitan-Port-au-Prince, they might not be representative of all health facilities in Haiti. Finally, the burden of respiratory and diarrheal diseases is likely underestimated as we could not account for children who died outside the hospital or who were not hospitalized. According to the 2012 demographic and health survey, 38% of children aged <5 years with acute respiratory infections and 34% of those with diarrhea were taken to a health care center for treatment.11
Despite these limitations, this study is the first to assess hospitalizations and deaths because of respiratory disease in children aged <5 years in Haiti. Although a previous study looked only at diarrheal disease hospitalizations in 4 hospitals in Haiti from 2010 to 2012 in children aged ≤2 years versus those aged 3–5 years,28 our study included information for more specific age groups at 6 major hospitals including HUEH, the largest public hospital in Haiti. Findings demonstrated that respiratory and diarrheal diseases were major contributors to hospitalizations among children aged <5 years in Haiti from 2011 to 2013 at the visited hospitals. We observed seasonal variations in respiratory and diarrheal diseases, which mirrored known seasonal patterns of respiratory and rotavirus disease infections, respectively. Therefore, introduction of Hib, pneumococcal conjugate and rotavirus vaccines could contribute to lowering of the burden of those diseases in Haiti. Continuing sentinel surveillance and conducting a similar study few years after the introduction of the vaccines in the country would help evaluate the impact of those vaccines in Haiti. In addition to vaccines, implementation of combined preventive and therapeutic interventions such as case management of pneumonia infections, improved water sources, use of oral rehydration solution and zinc supplementation could contribute to significant reductions in pneumonia and diarrheal deaths.15
ACKNOWLEDGMENTS
The authors thank Daphnel Albert, Yamileh Louis, Josué Garçon, Biaux Chety and Angelo Simon, medical students at Université Quisqueya in Port-au-Prince, Haiti for their assistance with data abstraction; Alina Choudhury, MPH student, at Emory University, for her help with the literature review and Amber Dismer, MPH, CDC for compiling the map.
This study was supported by the Centers for Disease Control and Prevention.
Footnotes
The findings and conclusions in this report are those of the authors and do not necessarily represent the official position of the Centers for Disease Control and Prevention.
The authors have no conflicts of interest or funding to disclose.
Findings in this article were presented in part at the 63rd Annual Meeting of the American Society of Tropical Medicine and Hygiene; November 2–6, 2014; New Orleans, LA.
REFERENCES
- 1.Liu L, Oza S, Hogan D, et al. Global, regional, and national causes of child mortality in 2000–13, with projections to inform post-2015 priorities: an updated systematic analysis. Lancet. 2015;385:430–440. doi: 10.1016/S0140-6736(14)61698-6. [DOI] [PubMed] [Google Scholar]
- 2.Kotloff KL, Nataro JP, Blackwelder WC, et al. Burden and aetiology of diarrhoeal disease in infants and young children in developing countries (the Global Enteric Multicenter Study, GEMS): a prospective, case-control study. Lancet. 2013;382:209–222. doi: 10.1016/S0140-6736(13)60844-2. [DOI] [PubMed] [Google Scholar]
- 3.Lanata CF, Fischer Walker CL, et al. for the Child Health Epidemiology Reference Group of the World Health Organization and UNICEF. Global causes of diarrheal disease mortality in children <5 years of age: a systematic review. PLOS One. 2013;8:e72788. doi: 10.1371/journal.pone.0072788. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.O’Brien KL, Wolfson LJ, Watt JP, et al. Hib and Pneumococcal Global Burden of Disease Study Team. Burden of disease caused by Streptococcus pneumoniae in children younger than 5 years: global estimates. Lancet. 2009;374:893–902. doi: 10.1016/S0140-6736(09)61204-6. [DOI] [PubMed] [Google Scholar]
- 5.Walker CL, Rudan I, Liu L, et al. Global burden of childhood pneumonia and diarrhoea. Lancet. 2013;381:1405–1416. doi: 10.1016/S0140-6736(13)60222-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.World Health Organization. Rotavirus vaccines WHO position paper. Wkly Epidemiol Rec. 2013;88:49–64. [PubMed] [Google Scholar]
- 7.World Health Organization. Pneumoccocal Vaccines WHO Position Paper. Wkly Epidemiol Rec. 2012;87:129–144. [PubMed] [Google Scholar]
- 8.Institut Haitien de Statistique et d’Informatique. Statistiques Demographiques et Sociales. [Accessed November 28, 2014]; Available at: http://www.ihsi.ht/produit_demo_soc.htm. [Google Scholar]
- 9.UNICEF. [Accessed November 28, 2014];Statistics at a glance: Haiti, 2013. Available at: http://www.unicef.org/infobycountry/haiti_statistics.html. [Google Scholar]
- 10.UNICEF. Levels and trends in child mortality. Report 2014: Estimates Developed by the UN Inter-agency Group for Child Mortality Estimation, 2013. [Accessed August 8, 2015]; Available at: http://www.unicef.org/media/files/Levels_and_Trends_in_Child_Mortality_2014.pdf. [Google Scholar]
- 11.Cayemittes M, Busangu MF, Bizimana JD, et al. Enquête Mortalité, Morbidité et Utilisation des Services, Haïti, 2012. Calverton, MD: MSPP, IHE et ICF International; 2013. [Accessed November 28, 2014 ]. Available at: http://mspp.gouv.ht/site/downloads/EMMUS%20V%20document%20final.pdf. [Google Scholar]
- 12.Yen C, Tate JE, Wenk JD, et al. Diarrhea-associated hospitalizations among US children over 2 rotavirus seasons after vaccine introduction. Pediatrics. 2011;127:e9–e15. doi: 10.1542/peds.2010-1393. [DOI] [PubMed] [Google Scholar]
- 13.Desai R, Haberling D, Holman RC, et al. Impact of rotavirus vaccine on diarrhea-associated disease burden among American Indian and Alaska Native children. Pediatrics. 2012;129:e907–e913. doi: 10.1542/peds.2011-2537. [DOI] [PubMed] [Google Scholar]
- 14.Ngabo F, Gatera M, Karema C, et al. Can routinely collected national data on childhood morbidity and mortality from diarrhea be used to monitor health impact of rotavirus vaccination in Africa? Examination of pre-vaccine baseline data from Rwanda. Pediatr Infect Dis J. 2014;33(Suppl 1):S89–S93. doi: 10.1097/INF.0000000000000054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Bhutta ZA, Das JK, Walker N, et al. Lancet Diarrhoea and Pneumonia Interventions Study Group. Interventions to address deaths from childhood pneumonia and diarrhoea equitably: what works and at what cost? Lancet. 2013;381:1417–1429. doi: 10.1016/S0140-6736(13)60648-0. [DOI] [PubMed] [Google Scholar]
- 16.Theodoratou E, Johnson S, Jhass A, et al. The effect of Haemophilus influenzae type b and pneumococcal conjugate vaccines on childhood pneumonia incidence, severe morbidity and mortality. Int J Epidemiol. 2010;39(Suppl 1):i172–i185. doi: 10.1093/ije/dyq033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.von Gottberg A, de Gouveia L, Tempia S, et al. GERMS-SA Investigators. Effects of vaccination on invasive pneumococcal disease in South Africa. N Engl J Med. 2014;371:1889–1899. doi: 10.1056/NEJMoa1401914. [DOI] [PubMed] [Google Scholar]
- 18.Munos MK, Walker CL, Black RE. The effect of rotavirus vaccine on diarrhoea mortality. Int J Epidemiol. 2010;39(Suppl 1):i56–i62. doi: 10.1093/ije/dyq022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Esparza-Aguilar M, Gastañaduy PA, Sánchez-Uribe E, et al. Diarrhoea-related hospitalizations in children before and after implementation of monovalent rotavirus vaccination in Mexico. Bull World Health Organ. 2014;92:117–125. doi: 10.2471/BLT.13.125286. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Gastañaduy PA, Sánchez-Uribe E, Esparza-Aguilar M, et al. Effect of rotavirus vaccine on diarrhea mortality in different socioeconomic regions of Mexico. Pediatrics. 2013;131:e1115–e1120. doi: 10.1542/peds.2012-2797. [DOI] [PubMed] [Google Scholar]
- 21.Rebaudet S, Gazin P, Barrais R, et al. The dry season in Haiti: a window of opportunity to eliminate cholera. PLOS Currents Outbreaks. (Edition 1) 2013 Jun 10; doi: 10.1371/currents.outbreaks.2193a0ec4401d9526203af12e5024ddc. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Dowell SF, Whitney CG, Wright C, et al. Seasonal patterns of invasive pneumococcal disease. Emerg Infect Dis. 2003;9:573–579. doi: 10.3201/eid0905.020556. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Shek LP, Lee BW. Epidemiology and seasonality of respiratory tract virus infections in the tropics. Paediatr Respir Rev. 2003;4:105–111. doi: 10.1016/s1526-0542(03)00024-1. [DOI] [PubMed] [Google Scholar]
- 24.Nascimento-Carvalho CM, Cardoso MR, Araujo-Neto CA, et al. Seasonal patterns of viral and bacterial infections among children hospitalized with community-acquired pneumonia in a tropical region. Scand J Infect Dis. 2010;42:839–844. doi: 10.3109/00365548.2010.498020. [DOI] [PubMed] [Google Scholar]
- 25.Ye Y, Zulu E, Mutisya M, et al. Seasonal pattern of pneumonia mortality among under-five children in Nairobi’s informal settlements. Am J Trop Med Hyg. 2009;81:770–775. doi: 10.4269/ajtmh.2009.09-0070. [DOI] [PubMed] [Google Scholar]
- 26.Levy K, Hubbard AE, Eisenberg JN. Seasonality of rotavirus disease in the tropics: a systematic review and meta-analysis. Int J Epidemiol. 2009;38:1487–1496. doi: 10.1093/ije/dyn260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Steenland MW, Joseph GA, Lucien MA, et al. Laboratory-confirmed cholera and rotavirus among patients with acute diarrhea in four hospitals in Haiti, 2012–2013. Am J Trop Med Hyg. 2013;89:641–646. doi: 10.4269/ajtmh.13-0307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Derby KS, Lucien MA, Leshem E, et al. Hospitalizations and deaths caused by diarrhea in children five years old and younger at four hospitals in Haiti, 2010–2012. Am J Trop Med Hyg. 2014;90:291–293. doi: 10.4269/ajtmh.13-0370. [DOI] [PMC free article] [PubMed] [Google Scholar]