Abstract
AIM: To study the effect of arsenic trioxide (As2O3) on rat experimental hepatocarcinoma and its renal cytotoxicity.
METHODS: The hepatocarcinoma model was established by diethaylnitrosamine perfusion in stomach of 120 Wistar rats, and the treatment began at the end of 20 weeks. Before the treatment, the rat models were randomly divided into 5 groups. In the treatment groups, three doses of As2O3 were injected into rat abdominal cavity, the total time of drug administration was 4 weeks. Cisplatin control or the blank group was injected into abdominal cavity with equal amount of cisplatin or saline at the same time, respectively. On the 7th, 14th and 28th day after the treatment, the hepatocarcinoma nodules were obtained and the morphologic changes of hepatocarcinoma cells were observed under light and electron microscopes; Immunohistochemistry (S-P methods) was employed to detect the expression of bcl-2, bax and PCNA in hepatocarcinoma tissues; flow cytometry (TUNEL assay) was used to detect the apoptosis of liver cancer cells and the change of cytokinetics. On the 28th day, the kidneys were obtained and their histologic changes were observed under light microscope, and immunohistochemistry (SP stain) was also employed to detect the expression of bcl-2 and PCNA. Cisplatin and saline solution were used as the control.
RESULTS: As2O3 could induce the apoptosis of rat liver cancer cells and exhibited typical morphologic changes. The incidence of apoptosis of hapatocarcinoma cells was elevated (P = 0.001). The elevation was the most higher in the group of middle-dose of As2O3 (1 mg·kg-1), significantly higher than that of the other arsenic groups and the controls (P = 0.001). Large dose of As2O3 (5 mg·kg-1) was able to arise the incidence of apoptosis, but also produced a large amount of necrosis and inflammatory reaction. Middle dose of As2O3 dramatically increased the cell number in G2/M phase (P = 0.0001), and apoptosis happened apparently. The expression of bcl-2 and bax was related to the dose of As2O3. With the up-regulation of apoptotic incidence, the ratio of bcl-2/bak decreased. But the incidence of apoptosis was not the highest status and the ratio of bcl-2/bax was at the lowest when the highest-dose of As2O3 was used. There was significant difference among the PCNA indexes (PCNA L1) of the five groups. Of them, three arsenic groups all showed decrease of different degrees, and this down-regulation was most obvious in group A. There was significant difference among the three groups (P = 0.016). Under the light microscope, the rat kidney in the cisplatin group exhibited tubular epithelium swelling and degeneration, protein casts in collecting tubules; While all arsenic groups didn’t show the significant changes (P = 0.013). In the arsenic groups, the expression of bcl-2 in the renal tubular epithelium was increased (P = 0.005), no obvious changes happened to PCNA L1. But in the group of cisplatin, the PCNA L1 increased significantly (P = 0.001).
CONCLUSION: As2O3 can induce apoptosis of rat hepatocellular carcinoma cells. And there is optimum dose; too high dose will induce the cytotoxic effect, while certain dose of As2O3 is able to block the cell cycle at G2/M phase. As2O3 had the most remarkable influence on G2/M cells, and it can also induce apoptosis to cells at other phases. As2O3 can restrain the proliferation of rat hepatocellular carcinoma cells, in a dose-time dependent manner. Compared with cisplatin, As2O3 didn’t show obvious renal toxicity, which was related to the increasing expression of bcl-2 in renal tubular epithelium, the inhibition of apoptosis and the anti-oxidation effects.
INTRODUCTION
Primary hepatocellular carcinoma has been found to be one of the most common malignancies worldwide. In the recent years, the diagnosis rate of early hepatocellular carcinoma has increased and the curative effect of surgery resection also improved. However, most of the early hepatocellular carcinoma is subclinical, once it is symptomatic, it is mainly in its middle or later stage. As the update statistic indicates, hepatocellular carcinoma ranked the second cause of cancer mortality since 1990s in China[1]. Presently, what challenges us most is the mid- or -late stage hepatocarcinoma, unresectable hepatocarcinoma, h igh po stoperative reoccurrence and high metastasis. Thus efficient nonsurgical methods are urgent[2,31-36].
Recently, it has been reported that arsenic (mainly arsenic trioxide, As2O3) in the treatment of leukemia has obvious curative effect through inducing tumor cell apoptosis[3,4]. But whether arsenic chemist can be used in the treatment of other malignancy such as hepatocellular carcinoma is still under the exploration. The blockage of apoptosis plays a more important role not only in the cause of malignancy but also in the out of control of proliferation. Thus in the two strategies of tumor treatment: inhabiting tumor cells’ proliferation and inducing their apoptosis, the later seems to be more preferable[5-7]. Our study is to establish a rat hepatocellular carcinoma model with the treatment of As2O3, then observe the apoptosis and proliferation of hepatocellular carcinoma cells and influence of it on the cell cycle, as well as the possibly noxious side effect on kidney of As2O3.
MATERIALS AND METHODS
Materials
Arsenic trioxide (As2O3 Sigma) was dissolved by PBS and diluted to 0.2% (m/m), kept under 4 °C. Diethaylnitrosamine (DEN Sigma) was diluted to 1% (v/v) by water solution. Cisplatin (QiLu Pharmaceutical Department) was diluted to 0.08% (m/m) by injection solution. There were also keg reagents as follows: murine monoclonal antibody against human Bcl-2 (1:50, SANTA CRUZ) and murine monoclonal antibody Bax (1: 70, SANTA CRUZ) and murine monoclonal antibody against rat proliferation cell nuclear antigen (PCNA) (1:100, Zhongshan Biotech Ltd, Beijing); HistostainTM-Plus Immunohistochemical reagent box (Zymed), DAB stain kit (Zhongshan Biotech Ltd, Beijing) APO-BRDUTM apoptosis quantitative test reagent box (Becton Dickinson).
FACS Vantage flow cytometry (Becton Dickinson), H600-4 transmission electron microscope (HITACHI) were used in this study.
Animal model, grouping and treatment
120 Wistar rats (60 males and 60 females, 6 weeks old) were supplied by the Fourth Institute of Military Medical Academy of Science. According to the method in the reference[8], the hepatocarcinoma model was established by DEN perfusion in stomach, and the treatment began at the end of 20 weeks. Before the treatment, the rat models were randomly divided into 5 groups. There were no difference in the number, sex and weight among the 5 groups. Group A: high-dose of As2O3 (5 mg·kg-1), group B: middle-dose of As2O3 (1 mg·kg-1), group C: low-dose of As2O3 (0.2 mg·kg-1), group D: cisplatin control (2 mg·kg-1), group E: blank control (saline solution).
In the treatment groups, three doses of As2O3 were injected into rat abdominal cavity, once a day, after two weeks, it is changed to twice a week, and the total time of drug administration was 4 weeks. Cisplatin control or the blank group was injected into abdominal cavity with equal amount of cisplatin or saline at the same time, respectively.
The choice of the dose of As2O3 was based on the curative dose on human leukemia (10 mg·d-1)[4], obtained by calculating the ratio of equal effective dose of body surface area between the human and rat. The dose of cisplatin was chosen according to the reference[9].
Methods
Sample preparation After the treatment, all rats were operated to obtain the liver nodules through 3 operations under anesthesia of sodium pentobarbital (abdominal cavity injection, 40-50 mg·kg-1) on the 7th, 14th and 28th day, respectively. The specimens with the formation of carcinoma proved by pathologic examination were chosen as experimental objects. At the last operation, the rats’ kidneys were obtained at the same time and the rats were killed.
The hepatocellular carcinoma nodules were divided into three parts along the center, one part (about 0.2 mg, fresh tissue) was made into monocyte suspending solution, used in the detection of flow cytometry; one part was fixed in 10% formaldehyde, embedded in paraffin with 4 μm successive section and HE staining. The pathologic changes of cancer nodules were observed under light microscope or by immunohistochemistry (IHC). The third part was processed into thin slice (< 1 mm) and immediately immersed into 2.5% glutaraldehyde phosphoric buffer. The embedded sections were made using the common electron microscope specimens. The ultrastructure of the hepatocellular carcinoma cells was observed under the transmission electron microscope[37].
Flow cytometry analysis The FACS Vantage flow cytometry was employed with the 5w argon laser as emission resource, and the wavelength of emission light was 488 nm. The variation coefficient (CV) of the machine was regulated as < 4% using chicken blood erythrocytes fixed by glutaraldehyde. 1 × 104 cells were analyzed and the data was analyzed using MODIfit LT software. Referring to the kit protocol, PI stain was used to label the cellular DNA to analyze cell cycle TdT to catalyze dUTP combined with external bromides (Br-dUTP) ligated to the 3’-OH terminal end of DNA fragments, then it was combined with anti-Br-dUTP mono-antibody labeled by FITC, and then the intensity of fluorescence of FITC was detected through the flow cytometry to estimate the number of DNA breakage points to qualitatively examine the cell apoptosis. The occurrence of apoptosis in different phases was analyzed combining with the staining result of PI.
Histology analysis The paraffin-embedded rat hepatocellular carcinoma tissues after 7 days of treatment were successively cut into 4 μm sections and the HIC (SP stain) was employed to detect the expression of bcl-2, bax and PCNA. The successive 4 μm sections were obtain from the paraffin-embedded rat hepatocellular carcinoma tissues after 28 days of treatment and stained with HE. And the histomorphologic change was observed under light microscope. IHC (SP stain) was used to detect the expression of bcl-2 and PCNA. PCNA labeling index (LI) = PCNA positive cells number/500 (using% to denote).
Statistical analysis
All the data were processed by statistical software SPSS10.0. The total VAR difference of each group was analyzed by Bartlett test. If it was the same, then analyzed by the one way ANOVA or student t test, otherwise by Kruskal-Wallis H test, or Mann Whitney U test which as for the multi-sample comparison; to the quantity material analysis, χ2 test was used (test standard: two-side α = 0.05).
RESULTS
On 7th, 14th, 28th day after the treatment, the hepatocarcinoma nodules of the rats (No. 65, 43, 34) were collected respectively (proved by pathology). The other rats were repelled out of the experiment due to the absence of carcinoma nodules. The kidneys of hepatocarcinoma rats were obtained on the 28th day after the treatment.
Morphologic change
Macroscopic observation The liver was yellow or pale with dramatically increase of the volume and weight. The liver grew as multi-nodular mass. The nodules were of variable size ranging from 3 mm to 3.5 cm. Some nodules were hemorrhagic. The liver was firm in texture, pale on section and with necrosis. Some nodules were dark red on section companied by the hemorrhagic necrosis (more obviously seen in Group A and D than in the others).
Light microscopic observation Hepatocarcinoma cells were arrayed in column or gland-like, most commonly presented middle- or highly-differentiated status, few were poorly differentiated status. In some specimens, the hepatocarcinoma cells showed patched or focal necrosis with red-stained non-structural materials. The nucleic chromatin disappeared, prominently seen in group A and D. The necrosis region and portal tracts were infiltrated by inflammatory cells with vascular dilation and hyperemia. Group B, C and E mainly exhibited point necrosis, slight inflammatory reaction in portal tracts, and vascular dilation was less obvious than the former groups. In the treated groups, some hepatocarcinoma cells presented apoptotic features, cell membrane was shrunken but intact, chromatin was condensed and accumulated at side or broken up forming nucleic bodies in different sizes within cells, without inflammatory cells invasion, seen more commonly in group A, B and D. Under microscope, group D (4/7) exhibited relatively extensive renal tubular epithelium cloudy swelling and degeneration. Protein casts was formed in the collecting tubules (4/7), there were no casts formed in group A, B, C and E (0/6, 0/6, 0/8, 0/7) without or occasionally tubular epithelium swelling and denaturalization. There was significant difference among the five groups (χ2 = 12.69, P = 0.013).
Electron microscope observation The chromatin was accumulated at the side of the nucleic membranes which was condensed. The nucleic shape was irregular and the surface of nucleic membrane was rough. The nucleus was broken but encapsuled by intact membrane, containing intact organelles and apoptotic bodies.
Flow cytometry analysis of hepatocarcinoma cells
Tumor cell apoptotic rate in each group and influence of treatment time On the 7th, 14th, 28th day of treatment, there was significant difference of tumor cell apoptotic rate presents among each group (P = 0.001). Compared with group E, apoptotic rate of group A, B, C, D all increased evidently, especialy that of group B (P = 0.000). The apoptotic rate of Group B depended on time, firstly it was increased then decreased (P = 0.004), but there was no significant difference between them on the 14th day and 28th day (P = 0.224). The relationship of apoptosis and treatment time between group A and group C was almost the same (Table 1).
Table 1.
Relationship between tumor cells apoptotic rate in each group and treatment time (-x ± s)
| Specimen | 7 days | 14 days | 28 days |
| Group A | 18.30 ± 3.43a | 20.16 ± 5.31a | 16.92 ± 4.03a |
| Group B | 40.99 ± 5.89b | 51.59 ± 7.67b | 47.49 ± 3.23b |
| Group C | 11.80 ± 7.02 | 12.24 ± 4.41a | 10.77 ± 3.45a |
| Group D | 22.41 ± 7.09a | 17.31 ± 6.16a | 13.88 ± 3.83a |
| Group E | 7.66 ± 2.23 | 6.72 ± 2.31 | 6.30 ± 1.15 |
P < 0.05, vs group E;
P < 0.001, vs group E.
Compared with group E, apoptotic rate of G0/G1, G2/M phase cell in group B was significantly increased (P < 0.05), especial that of G2/M phase cell (P = 0.001). Cell apoptosis presented during the whole cell cycle in group A, C, D, without distinct specificity (Table 2). In group B, apoptotic rate of G0/G1 phase cell is lower than that of G2/M phase cell, but the number of apoptotic cells at G0/G1 phase still accounted for a rather large proportion of the whole apoptotic cells.
Table 2.
Apoptosis distribution of tumor cells at G0/G1, G2/M phase in each group (%)
| Specimen |
7 days |
14 days |
28 days |
|||
| G0/G1 | G2/M | G0/G1 | G2/M | G0/G1 | G2/M | |
| Group A | 21.79a | 10.67 | 24.93b | 8.65 | 15.84 | 36.21a |
| Group B | 23.43a | 78.64b | 42.53b | 80.68b | 27.90a | 78.95b |
| Group C | 5.97 | 25.50a | 13.24 | 15.99 | 10.42 | 14.21 |
| Group D | 21.91a | 40.33b | 20.94a | 25.71a | 10.95 | 20.66 |
| Group E | 10.19 | 12.80 | 8.56 | 8.07 | 7.07 | 8.87 |
P < 0.05, vs group E;
P < 0.001, vs group E.
Tumor cell cycle changes in each group (Table 3)
Table 3.
Variety of tumor cells in each group (%)
| Specimen |
7 days |
14 days |
28 days |
||||||
| G0/G1 | S | G2/M | G0/G1 | S | G2/M | G0/G1 | S | G2/M | |
| Group A | 74.81a | 5.65a | 19.54a | 80.17a | 7.71a | 12.12 | 85.16a | 5.58a | 9.25 |
| Group B | 54.04 | 12.63a | 33.79a | 69.50 | 8.50a | 22.01a | 67.83 | 11.14a | 21.04a |
| Group C | 60.34 | 6.45a | 33.21a | 66.92 | 11.18a | 21.90a | 62.63 | 12.21a | 25.17a |
| Group D | 44.71a | 23.42a | 31.94a | 37.97a | 30.64a | 31.39a | 32.84a | 23.25 | 43.91a |
| Group E | 58.89 | 29.93 | 11.18 | 63.47 | 26.21 | 10.33 | 66.54 | 22.07 | 11.4 |
P < 0.05, vs group E.
The tumor cells apoptotic distribution at G0/G1, G2/M phase in each group Compared with group E, on the 7th, 14th, 28th day after the treatment, the percentage of G0/G1 phase cells in group A was increased significantly (P = 0.001), while that in group D was significantly decreased (P = 0.001), and no statistical difference in group B, C (P > 0.05); the percentage of S phase cell in group A, B, C was reduced (P = 0.001); while that of G2/M phase cell in group B, C, D was increased (P = 0.001).
Immunohistochemical analysis
Immunohistochemical result of hepatocarcinoma tissue Among the 65-rat hepatocarcinoma tissue obtained after the treatment for 7 days, bc1-2 expressed positively in 57 of them. The intensity of bc1-2 positive expression was evidently differed among the 5 groups (chi-square test, P = 0.034), it was lower expressed in group A, B, C, especial group B, which was significantly lower than that in the controls. Among the 65 specimens, 54 of them presented positive expression of bax. The intensity and rate of positive expression had significant difference among the 5 groups (chi-square test, P = 0.022 and P = 0.006). It was significantly higher in group A, B, C than that in the controls, whereas there was no statistical difference among the former. PCNA was expressed positively in 63 specimen, with significant difference among the 5 groups(Kruskal-Wallis test, P = 0.001). Compared with group E, PCNA LI expression was down regulated in group A, B, C, and D, especially in group A.
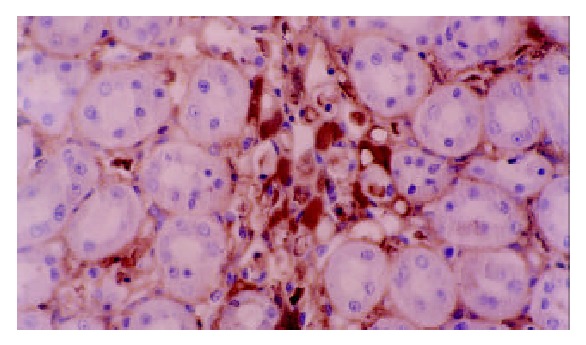
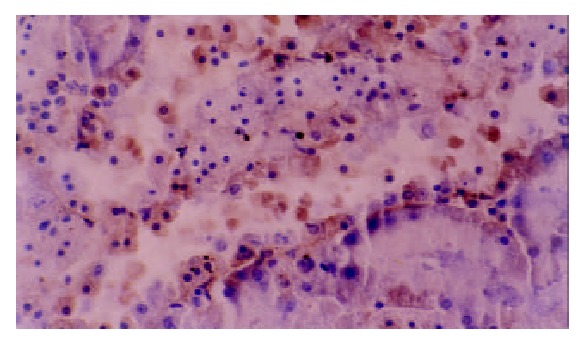
Immunohistochemical analyzing of renal tissue There was no significant difference in the expression of bcl-2 among the 5 groups, but among different positions. In group D and E, bc1-2 was positively expressed commonly in stroma cells without significant difference among the 5 groups. But in the renal tubular epithelium its positive expression was obviously enhanced (χ2 = 14.93, P = 0.005) (Figure 1, Figure 2). PCNA LI was significantly different (Kruskal-Wallis test, P = 0.001). Compared to group E, PCNA LI expression was increased evidently(Mann-Whitney, P = 0.001), without significant difference between Group A, B, C. Expression of PCNA LI renal tubular epithelium and stroma cells had significant difference among the 5 groups; while that of stroma cells, cortex-medulla cells and renal tubular epithelium all rose obviously without significant changes in Group A, B, C (Figure 3, Figure 4).
Figure 1.
Positive expression of bcl-2 in the renal stroma cell, while negative in tubular epithelium in the cisplatin group (SP, × 400).
Figure 2.
Positive expression of bc1-2 in renal tubular epithelium in medium dose arsenic group (SP, × 400).
Figure 3.
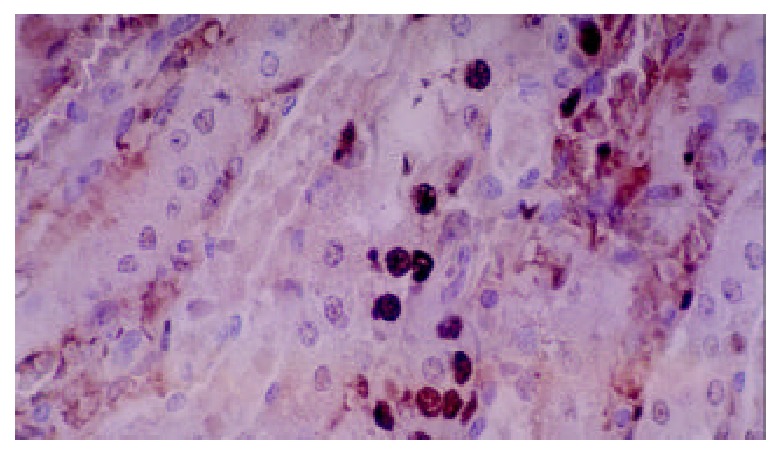
PCNA expression in renal collecting tubular epithelium and stroma cells in the cisplatin group (SP, × 400).
Figure 4.
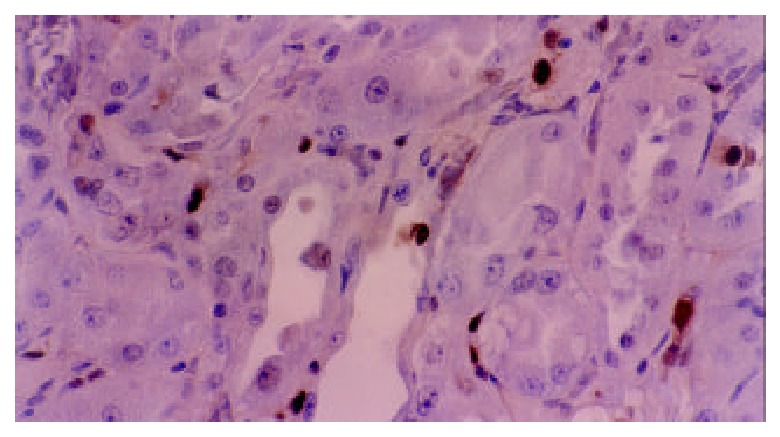
PCNA expression in renal cortex tubular cells in medium dose in arsenic group epithelium (SP, × 400).
DISCUSSION
At present, the pathogenesis and progression of tumor are thought to relate to cellular abnormal proliferation[1,16,37], and as well as the abnormal apoptosis[19,40]. Exploring the origination and development of tumor from the viewpoint of apoptosis may elucidate the pathogenesis of tumor and helpfully open a new way to the therapy of tumor.
Studies indicated that As2 O3 was able to induce hepatocarcinoma cells apoptosis[11,12,40,41], and to inhibit the growth of transplanted hepatocarcinoma of nude mice[11-14], However, there is no report on the effect of chemocarcinogen on hepatocarcinoma in vitro. The result in this study revealed that As2O3 could induce the apoptosis of hepatic carcinoma cells and inhibited the proliferation of carcinoma cells after treatment of hepatocarcinoma induced by DEN in rat. There was no apparent damage to the renal, especially to the tubular epithelial cells. Different dosages of arsenic had different effects on the apoptosis, showing a problem of an optimum dose. As for the morphologic changes, it was assumed that two death mechanisms worked at the same time when the arsenic dose was too high. Though it could induce the apoptosis in certain degree, it could also produce cellular toxic phenomena[17-23], leading to necrosis and inflammation of carcinoma cells, and kill the normal cells. While too low dose had weak cytotoxicity, it couldn’t take effect in spite of the ability to induce apoptosis of carcinoma cells. Moderate dose could induce the apoptosis of amount of cancer cells, but produce obvious cytotoxic effect[11,12,40-42].
Apoptosis has a close relationship with cell cycle. Among the current anti-cancer drugs, whether the cellular cycle-specific drugs or the non-specific ones, both of them have the first-class kinetics, which is that they cannot kill all of the tumor cells but some proportion of them. Studies showed that some carcinoma cell lines, such as human hepatocarcinoma[14,22], stomach cancer and pancreatic cancer and so on[36], may show blockage of G2/M phase after treated with As2O3 in vitro. While in human mammary carcinoma cell line, cell cycle was blocked at different phases with different dose of As2O3. The results in this study indicated that As2O3 could induce the change of cell cycle in rat. The prominent feature was that middle-dose of As2O3 would lead to G2/M blockage and large-dose of As2O3 would lead to G0/G1 blockage. It was thought that different dose of As2O3 held different influence on cell cycle of rat carcinoma cells and they correspondingly maybe had different end of cell cycle blockage. This study showed that with middle-dose of As2O3, the cells at G2/M phase had very high incidence of apoptosis, while the rate of apoptosis was low at G1 and S phase, presenting very strong cell cycle-specific manner. However, at the same time, in spite of the low incidence of apoptosis at G1 and S phase, at both of them, especially at G1 phase, the proportion of apoptotic cells to total apoptotic cells couldn’t be ignored. In the high- or low- dose of arsenic group, apoptosis didn’t present the highest sensitivity at some phase. The above results suggested that arsenic may belong to a kind of non-typical cell cycle-specific drugs, and would get better therapy effect after combination with other cell cycle-specific drugs.
PCNA is an assistant protein of DNA polymerase, directly participating in the DNA replication during the cell proliferation. PCNA is lowly expressed in rest cells, and gets its peak at G1 late phase and S phase, and then significantly descends at G2/M phase. The content and expression degree of PCNA reflect the activity of cellular proliferation, which is a main biologic index of cellular proliferation. The present study showed that PCNA LI of the rat hepatocarcinoma cells was decreased to different level after the treatment of As2O3. Different dosages of As2O3 resulted in different degree of reduction of PCNA LI. The higher dose resulted in more significant reduction, proving that there did exist certain dose effect relationship in the inhibition of proliferation of As2O3 on hepatocarcinoma cells.
Cisplatin is one of the most effective chemotherapy drugs on hepatocarcinoma at present, but the serious renal-toxicity limits its use. Under microscope the renal toxicity of cisplatin manifests acute denaturalization tubular epithelium, necrosis, interstitial edema and tubular dilation. Our study showed these changes were showed in the cisplatin group (4/7) while no significant changes happened in the As2O3 group.
Studies showed that the renal toxicity had close relation with its oxidized damage to tubules. Bcl-2 is an apoptosis inhibitor and a strong anti-oxidant[18-21]. With the action of cisplatin, the expression of bcl-2 was strikingly decreased in the renal tubular epithelium. Preliminary treatment with some medicines (Midkine, uranyl acetate) can increase the expression of bcl-2 and decrease the apoptosis resulting from cisplatin, and subsequently on low its damage on tubules[9,19]. In this study, after administration of As2O3, the expression of bcl-2 in renal tubular epithelium was increased, while PCNA LI was not significantly changed. It was supposed that with the effect of As2O3, expression of apoptosis repression gene bcl-2 was increased, resulting in the inhibition of apoptosis, meanwhile, the anti-oxidated effect of bcl-2 was able to counteract possible oxidated damage, therefore it didn’t have obvious toxic side effect on renal tubular epithelium.
In conclusion, this study indicated that As2O3 could induce apoptosis of rat hepatocarcinoma cells. And there exists optimization dose, too high dose will cause the cytotoxic effect, while proper dose of As2O3 is able to block the cell cycle at G2/M phase. As2O3 had the most remarkable influence on cells at G2/M phase, and it can also induce apoptosis to the cells at other phases. As2O3 can restrain the proliferation of rat hepatocarcinoma cells, presenting a dose-time relationship. Compared with cisplatin, As2O3 didn’t show obvious renal toxicity which maybe was related to the increase of expression of bcl-2 in renal tubular epithelium, the inhibition of apoptosis and its anti-oxidation effects[42].
Footnotes
Supported by Natural Scientific Foundation of Tianjin, No. 993703211
Edited by Xu XQ
References
- 1.Tang ZY. Hepatocellular carcinoma--cause, treatment and metastasis. World J Gastroenterol. 2001;7:445–454. doi: 10.3748/wjg.v7.i4.445. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Vucenik I, Tantivejkul K, Zhang ZS, Cole KE, Saied I, Shamsuddin AM. IP6 in treatment of liver cancer. I. IP6 inhibits growth and reverses transformed phenotype in HepG2 human liver cancer cell line. Anticancer Res. 1998;18:4083–4090. [PubMed] [Google Scholar]
- 3.Chen GQ, Zhu J, Shi XG, Ni JH, Zhong HJ, Si GY, Jin XL, Tang W, Li XS, Xong SM, et al. In vitro studies on cellular and molecular mechanisms of arsenic trioxide (As2O3) in the treatment of acute promyelocytic leukemia: As2O3 induces NB4 cell apoptosis with downregulation of Bcl-2 expression and modulation of PML-RAR alpha/PML proteins. Blood. 1996;88:1052–1061. [PubMed] [Google Scholar]
- 4.Shen ZX, Chen GQ, Ni JH, Li XS, Xiong SM, Qiu QY, Zhu J, Tang W, Sun GL, Yang KQ, et al. Use of arsenic trioxide (As2O3) in the treatment of acute promyelocytic leukemia (APL): II. Clinical efficacy and pharmacokinetics in relapsed patients. Blood. 1997;89:3354–3360. [PubMed] [Google Scholar]
- 5.Kerr JF, Winterford CM, Harmon BV. Apoptosis. Its significance in cancer and cancer therapy. Cancer. 1994;73:2013–2026. doi: 10.1002/1097-0142(19940415)73:8<2013::aid-cncr2820730802>3.0.co;2-j. [DOI] [PubMed] [Google Scholar]
- 6.Jiang MC, Yang-Yen HF, Lin JK, Yen JJ. Differential regulation of p53, c-Myc, Bcl-2 and Bax protein expression during apoptosis induced by widely divergent stimuli in human hepatoblastoma cells. Oncogene. 1996;13:609–616. [PubMed] [Google Scholar]
- 7.Fisher DE. Apoptosis in cancer therapy: crossing the threshold. Cell. 1994;78:539–542. doi: 10.1016/0092-8674(94)90518-5. [DOI] [PubMed] [Google Scholar]
- 8.Zhou H, Miyaji T, Kato A, Fujigaki Y, Sano K, Hishida A. Attenuation of cisplatin-induced acute renal failure is associated with less apoptotic cell death. J Lab Clin Med. 1999;134:649–658. doi: 10.1016/s0022-2143(99)90106-3. [DOI] [PubMed] [Google Scholar]
- 9.Chen Z, Chen GQ, Shen ZX, Sun GL, Tong JH, Wang ZY, Chen SJ. Expanding the use of arsenic trioxide: leukemias and beyond. Semin Hematol. 2002;39:22–26. doi: 10.1053/shem.2002.33611. [DOI] [PubMed] [Google Scholar]
- 10.Liao C, Zhao MJ, Zhao J, Jia D, Song H, Li ZP. Over-expression of LPTS-L in hepatocellular carcinoma cell line SMMC-7721 induces crisis. World J Gastroenterol. 2002;8:1050–1052. doi: 10.3748/wjg.v8.i6.1050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Oketani M, Kohara K, Tuvdendorj D, Ishitsuka K, Komorizono Y, Ishibashi K, Arima T. Inhibition by arsenic trioxide of human hepatoma cell growth. Cancer Lett. 2002;183:147–153. doi: 10.1016/s0304-3835(01)00800-x. [DOI] [PubMed] [Google Scholar]
- 12.Siu KP, Chan JY, Fung KP. Effect of arsenic trioxide on human hepatocellular carcinoma HepG2 cells: inhibition of proliferation and induction of apoptosis. Life Sci. 2002;71:275–285. doi: 10.1016/s0024-3205(02)01622-3. [DOI] [PubMed] [Google Scholar]
- 13.Xu HY, Yang YL, Gao YY, Wu QL, Gao GQ. Effect of arsenic trioxide on human hepatoma cell line BEL-7402 cultured in vitro. World J Gastroenterol. 2000;6:681–687. doi: 10.3748/wjg.v6.i5.681. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Zeng WJ, Liu GY, Xu J, Zhou XD, Zhang YE, Zhang N. Pathological characteristics, PCNA labeling index and DNA index in prognostic evaluation of patients with moderately differentiated hepatocellular carcinoma. World J Gastroenterol. 2002;8:1040–1044. doi: 10.3748/wjg.v8.i6.1040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Niu ZS, Li BK, Wang M. Expression of p53 and C-myc genes and its clinical relevance in the hepatocellular carcinomatous and pericarcinomatous tissues. World J Gastroenterol. 2002;8:822–826. doi: 10.3748/wjg.v8.i5.822. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Chen XP, Zhao H, Zhao XP. Alternation of AFP-mRNA level detected in blood circulation during liver resection for HCC and its significance. World J Gastroenterol. 2002;8:818–821. [PubMed] [Google Scholar]
- 17.Qiu DK, Ma X, Peng YS, Chen XY. Significance of cyclooxygenase-2 expression in human primary hepatocellular carcinoma. World J Gastroenterol. 2002;8:815–817. doi: 10.3748/wjg.v8.i5.815. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Jiang Y, Zhou XD, Liu YK, Wu X, Huang XW. Association of hTcf-4 gene expression and mutation with clinicopathological characteristics of hepatocellular carcinoma. World J Gastroenterol. 2002;8:804–807. doi: 10.3748/wjg.v8.i5.804. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Yang LJ, Wang WL. Preparation of monoclonal antibody against apoptosis-associated antigens of hepatoma cells by subtractive immunization. World J Gastroenterol. 2002;8:808–814. doi: 10.3748/wjg.v8.i5.808. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Huang J, Cai MY, Wei DP. HLA class I expression in primary hepatocellular carcinoma. World J Gastroenterol. 2002;8:654–657. doi: 10.3748/wjg.v8.i4.654. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Huang GW, Yang LY. Metallothionein expression in hepatocellular carcinoma. World J Gastroenterol. 2002;8:650–653. doi: 10.3748/wjg.v8.i4.650. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Liu L, Qin S, Chen H, Wang J, Chen H, Ma J, Liu W. [An experimental study on arsenic trioxide-selectively induced human hepatocarcinoma cell lines apoptosis and its related genes] Zhonghua Ganzangbing Zazhi. 2000;8:367–369. [PubMed] [Google Scholar]
- 23.Yang JY, Luo HY, Lin QY, Liu ZM, Yan LN, Lin P, Zhang J, Lei S. Subcellular daunorubicin distribution and its relation to multidrug resistance phenotype in drug-resistant cell line SMMC-7721/R. World J Gastroenterol. 2002;8:644–649. doi: 10.3748/wjg.v8.i4.644. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Liu LX, Jiang HC, Liu ZH, Zhou J, Zhang WH, Zhu AL, Wang XQ, Wu M. Integrin gene expression profiles of human hepatocellular carcinoma. World J Gastroenterol. 2002;8:631–637. doi: 10.3748/wjg.v8.i4.631. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Jiang HC, Liu LX, Piao DX, Xu J, Zheng M, Zhu AL, Qi SY, Zhang WH, Wu LF. Clinical short-term results of radiofrequency ablation in liver cancers. World J Gastroenterol. 2002;8:624–630. doi: 10.3748/wjg.v8.i4.624. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Su JM, Gui L, Zhou YP, Zha XL. Expression of focal adhesion kinase and alpha5 and beta1 integrins in carcinomas and its clinical significance. World J Gastroenterol. 2002;8:613–618. doi: 10.3748/wjg.v8.i4.613. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Liu H, Wang Y, Zhou Q, Gui SY, Li X. The point mutation of p53 gene exon7 in hepatocellular carcinoma from Anhui Province, a non HCC prevalent area in China. World J Gastroenterol. 2002;8:480–482. doi: 10.3748/wjg.v8.i3.480. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Li MS, Li PF, He SP, Du GG, Li G. The promoting molecular mechanism of alpha-fetoprotein on the growth of human hepatoma Bel7402 cell line. World J Gastroenterol. 2002;8:469–475. doi: 10.3748/wjg.v8.i3.469. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Wang FS, Liu MX, Zhang B, Shi M, Lei ZY, Sun WB, Du QY, Chen JM. Antitumor activities of human autologous cytokine-induced killer (CIK) cells against hepatocellular carcinoma cells in vitro and in vivo. World J Gastroenterol. 2002;8:464–468. doi: 10.3748/wjg.v8.i3.464. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Qin LX, Tang ZY, Ma ZC, Wu ZQ, Zhou XD, Ye QH, Ji Y, Huang LW, Jia HL, Sun HC, et al. P53 immunohistochemical scoring: an independent prognostic marker for patients after hepatocellular carcinoma resection. World J Gastroenterol. 2002;8:459–463. doi: 10.3748/wjg.v8.i3.459. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Liu LX, Jiang HC, Piao DX. Radiofrequence ablation of liver cancers. World J Gastroenterol. 2002;8:393–399. doi: 10.3748/wjg.v8.i3.393. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Qin LX, Tang ZY. The prognostic molecular markers in hepatocellular carcinoma. World J Gastroenterol. 2002;8:385–392. doi: 10.3748/wjg.v8.i3.385. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Zhang G, Long M, Wu ZZ, Yu WQ. Mechanical properties of hepatocellular carcinoma cells. World J Gastroenterol. 2002;8:243–246. doi: 10.3748/wjg.v8.i2.243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Zhao WH, Ma ZM, Zhou XR, Feng YZ, Fang BS. Prediction of recurrence and prognosis in patients with hepatocellular carcinoma after resection by use of CLIP score. World J Gastroenterol. 2002;8:237–242. doi: 10.3748/wjg.v8.i2.237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Zheng N, Ye SL, Sun RX, Zhao Y, Tang ZY. Effects of cryopreservation and phenylacetate on biological characters of adherent LAK cells from patients with hepatocellular carcinoma. World J Gastroenterol. 2002;8:233–236. doi: 10.3748/wjg.v8.i2.233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Hao MW, Liang YR, Liu YF, Liu L, Wu MY, Yang HX. Transcription factor EGR-1 inhibits growth of hepatocellular carcinoma and esophageal carcinoma cell lines. World J Gastroenterol. 2002;8:203–207. doi: 10.3748/wjg.v8.i2.203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Qin LX, Tang ZY. The prognostic significance of clinical and pathological features in hepatocellular carcinoma. World J Gastroenterol. 2002;8:193–199. doi: 10.3748/wjg.v8.i2.193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Wang ZX, Hu GF, Wang HY, Wu MC. Expression of liver cancer associated gene HCCA3. World J Gastroenterol. 2001;7:821–825. doi: 10.3748/wjg.v7.i6.821. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Rabe C, Pilz T, Klostermann C, Berna M, Schild HH, Sauerbruch T, Caselmann WH. Clinical characteristics and outcome of a cohort of 101 patients with hepatocellular carcinoma. World J Gastroenterol. 2001;7:208–215. doi: 10.3748/wjg.v7.i2.208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Sun BH, Zhang J, Wang BJ, Zhao XP, Wang YK, Yu ZQ, Yang DL, Hao LJ. Analysis of in vivo patterns of caspase 3 gene expression in primary hepatocellular carcinoma and its relationship to p21(WAF1) expression and hepatic apoptosis. World J Gastroenterol. 2000;6:356–360. doi: 10.3748/wjg.v6.i3.356. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Yang SM, Zhou H, Chen RC, Wang YF, Chen F, Zhang CG, Zhen Y, Yan JH, Su JH. Sequencing of p53 mutation in established human hepatocellular carcinoma cell line of HHC4 and HHC15 in nude mice. World J Gastroenterol. 1998;4:506–510. doi: 10.3748/wjg.v4.i6.506. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.45 Guo XZ, Shao XD, Liu MP, Xu JH, Ren LN, Zhao JJ, Li HY, Wang D. Effect of bax, bcl-2 and bcl-xL on regulating apoptosis in tissues of normal liver and hepatocellular carcinoma. World J Gastroenterol. 2002;8:1059–1062. doi: 10.3748/wjg.v8.i6.1059. [DOI] [PMC free article] [PubMed] [Google Scholar]


