Abstract
A 17-year-old girl with colicky abdominal pain and chronic anemia presented to the gastrointestinal service of the University Hospital of Essen. In the routine workup, there were no pathological findings despite the anemia. Because of the fluctuation of symptoms with a climax at the time of menstruation, consecutive ultrasound studies were performed revealing a visible mass inside the gallbladder. This finding was confirmed by a magnetic resonance imaging (MRI) study performed at the same time. Because of the severe anemia by that time, a cholecystectomy was performed, and histology reconfirmed the diagnosis of isolated gallbladder endometriosis. The patient recovered well and has had no recurrence of the disease to date.
Keywords: Gallbladder, Endometriosis, Bleeding, Menstrual cycle, Abdominal pain
INTRODUCTION
Endometriosis is the presence of functioning endometrial tissue outside the uterine cavity. Indeed, when this hormonally active tissue implants in the gastrointestinal tract, it can cause cyclical bleeding, resulting in anemia and pain. Herein, we describe a very rare case of an endometrial tissue manifestation in the gallbladder.
CASE REPORT
A 17-year-old girl with colicky abdominal pain and chronic anemia of unknown origin was referred to the University Hospital of Essen. The right upper quadrant pain was most severe during menstruation. Similar symptoms had occurred one year prior to admission and led to further hospital stays; however, despite extensive diagnostic efforts, a satisfying diagnosis was lacking and the treatment was for symptoms only. The patient was treated with repetitive iron replacement and blood transfusions, which led to several complications including thrombophlebitis, with the need for surgical intervention. Physical examination revealed no pathological findings apart from a local tenderness to palpation in the right upper quadrant of the abdomen. Routine laboratory studies confirmed a normocytemic hypochromic anemia. No further abnormalities were seen in routine laboratory studies; liver function tests were within normal limits, as was hepatitis serology including tests for major hepatotropic viruses.
Several diagnostic means were used to identify the cause of symptoms, including oesophago-gastro-duodenoscopy and colonoscopy as well as radiologic studies. Endoscopic examinations showed physiologic findings in the upper and lower gastrointestinal tract. Radiographic examinations, including barium follow-through, initial ultrasound (US) and magnetic resonance imaging (MRI) of the abdomen, were normal. Computed tomography (CT) of the abdomen showed a questionable radiopaque tissue in the wall of the gallbladder, with concomitant inflammation. These findings, combined with the history of complaints, led to the presumed diagnosis of gallbladder endometriosis. US examination was performed once more on d 14 of the menstrual cycle and repeated every second day, showing continual expansion of the suspected tissue. After 12 d and maximum extension of the tissue, a second MRI of the liver was performed, and the diagnosis of endometriosis of the gallbladder could be confirmed (Figure 1).
Figure 1.
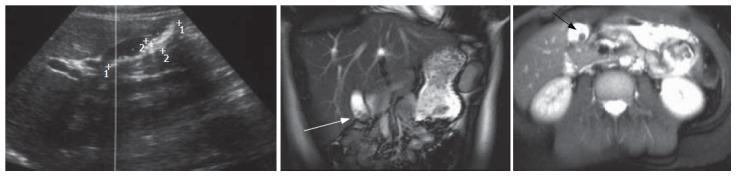
Computed tomography (CT) of the abdomen showed a radiopaque tissue in the wall of the gallbladder, with concomitant inflammation. US examination showed continual expansion of the suspected tissue. After 12 d and maximum extension of the tissue, a second MRI of the liver was performed, and the diagnosis of endometriosis of the gallbladder could be confirmed.
According to the radiologic findings and the continued abdominal complaints, laparoscopic cholecystectomy was discussed with the Department of General Surgery and finally performed. The postoperative course was uneventful. Twelve months after surgery the patient was still without any complaints, and during the laboratory follow up her hemoglobin level remained within the normal range; no further transfusions have been necessary. Histopathological examination confirmed the clinical diagnosis of endometriosis of the gallbladder.
DISCUSSION
Endometriosis, defined as the presence of endometrial tissue outside the uterine cavity and musculature, was first described by von Rokitasky in 1860. Although it usually occurs in the pelvis, endometriosis has been found in almost every region of the human body. As a response to physiologic hormonal changes that occur during the menstrual cycle, this ectopic endometrium will invade, distort and occasionally destroy normal organs. The prevalence of this abnormality has been reported to be between 8% and 18% in young women[1,2]. The majority of extrauterine endometrial tissue invades ovaries and the pelvic peritoneum. Ectopic endometriosis in other sites of the female body usually involves the gastrointestinal tract, but ectopic tissue may also present within the urinary tract[1,3,4]. In addition, symptomatic mediastinal, bronchial and pleural endometriosis have been documented[3,5-8] and the presence of endometrial tissue has been identified in thigh muscle tissue[9,10], the inguinal canal[10], nasal mucosa[11], incisional scars[12] and, in very few cases, in the gallbladder[13]. The clinical diagnosis of intestinal endometriosis may be difficult to make because of non-specific symptoms and the missing relationship between symptoms and the menstrual cycle. However, endometriosis should always be considered in women with recurrent abdominal pain and intestinal symptoms, especially in young females with gynaecologic complaints. The high prevalence of irritable bowel syndrome increases the risk of misdiagnosis in these rare cases.
According to its localization, intestinal endometriosis is often an incident finding in laparoscopic procedures[14-18]. Recognition requires a high index of suspicion. Thus, physicians should be aware of endometriosis as a differential diagnosis in female patients with recurrent periumbilical or abdominal pain and other episodic bowel symptoms.
An important component of the evaluation is a bimanual pelvic examination that includes combined rectovaginal palpitation. Because findings may vary considerably throughout the menstrual cycle, all examinations should be performed immediately before and again after menses[3,4].
In many cases, radiologic findings are useful in raising the possibility of detection of endometriosis, providing supportive evidence for a preliminary diagnosis[19-22]. Intestinal endometriosis appears radiographically as a tapered, often eccentric, constricting deformity. Although CT scanning and US are often unable to differentiate between abscesses and hematomas from endometriotic lesions[4,18,23], such indirect imaging methods may be useful in defining the anatomic extent of pelvic endometriosis[4]. MRI is useful for monitoring the response to treatment, but it cannot be relied upon as a diagnostic substitute for laparoscopy[23-26].
As intestinal endometriosis is usually nonmucosal, enteroscopy is helpful in excluding other gastrointestinal disorders, especially neoplasia[27,28]. Unequivocal diagnosis relies upon histological confirmation of the presence of the endometrium within one or several organs of the gastrointestinal tract. It is of particular importance in such morphologic interpretations to avoid confusing endometrial tissue with carcinomatous glands. In postmenopausal women in particular, less prominent stromal elements leave scattered endometrial glands, which appear similar to well-differentiated adenocarcinomas. In general, when a diagnosis of intestinal endometriosis is made, hormonal therapy is often the first therapeutic option, similar to the standard approach to pelvic endometriosis[29-31]. Low-dose estrogen-progesterone compounds can cause pseudopregnancy states that result in the decidualization of endometrial tissue and often relieve symptoms like dysmenorrhea. However, their use in more severe diseases is questionable and generally not recommended for symptomatic intestinal diseases. The most effective agents currently available are the synthetic androgen danazol and the gonadotropin-releasing hormone (GnRH) agonists. New approaches tend to use add-back estrogen replacement to improve the quality of life and reduce the side effects of these treatments[32]. Although both are effective in decreasing pelvic pain associated with endometriosis and appear to decrease the size of endometrial implants, there are no studies of these agents in intestinal disease, and there is some concern that treatment can result in increased fibrosis[33]. In cases of mucosal endometriosis, laparoscopical ablation can be accomplished using a carbon dioxide laser[34,35]. In cases of endometriosis causing partial obstruction of the colon or small intestine, segment resection of the involved area is considered to provide the best results, and it also serves to exclude any underlying carcinoma[4,36]. In patients who have failed medical therapy and who have intractable symptoms, hysterectomy and salpingo-oophorectomy can be perform-ed at the time of resective surgery to minimize the risk of symptomatic disease in the future. Similar surgery also can be performed in postmenopausal patients[37-39].
Because of the isolated endometrial manifestation in the gallbladder and the age of the patient in this case, a surgical approach and laparoscopic cholecystectomy seemed to provide the best results. Considering the long history and suffering of this patient for over one year, it appears that familiarity with this nonneoplastic process and an appropriate index of suspicion is often lacking in physicians - even for patients with typical presentations.
Footnotes
S- Editor Ma N L- Editor McGowan D E- Editor Liu Y
References
- 1.Gray LA. The management of endometriosis involving the bowel. Clin Obstet Gynecol. 1966;9:309–330. doi: 10.1097/00003081-196606000-00004. [DOI] [PubMed] [Google Scholar]
- 2.Ranney B. Endometriosis: Pathogenesis, symptoms, and findings. Clin Obstet Gynecol. 1980;23:865–874. [PubMed] [Google Scholar]
- 3.Luciano AA, Pitkin RM. Endometriosis: approaches to diagnosis and treatment. Surg Annu. 1984;16:297–312. [PubMed] [Google Scholar]
- 4.Croom RD, Donovan ML, Schwesinger WH. Intestinal endometriosis. Am J Surg. 1984;148:660–667. doi: 10.1016/0002-9610(84)90347-7. [DOI] [PubMed] [Google Scholar]
- 5.Kovarik JL, Toll GD. Thoracic endometriosis with recurrent spontaneous pneumothorax. JAMA. 1966;196:595–597. [PubMed] [Google Scholar]
- 6.Labay GR, Feiner F. Malignant pleural endometriosis. Am J Obstet Gynecol. 1971;110:478–480. doi: 10.1016/0002-9378(71)90687-9. [DOI] [PubMed] [Google Scholar]
- 7.Bednoff SL, Garfinkle BM. Endometriosis of the pleura. Obstet Gynecol. 1965;26:549–551. [PubMed] [Google Scholar]
- 8.Hibbard LT, Schumann WR, Goldstein GE. Thoracic endometriosis: a review and report of two cases. Am J Obstet Gynecol. 1981;140:227–232. doi: 10.1016/0002-9378(81)90112-5. [DOI] [PubMed] [Google Scholar]
- 9.Gitelis S, Petasnick JP, Turner DA, Ghiselli RW, Miller AW. Endometriosis simulating a soft tissue tumor of the thigh: CT and MR evaluation. J Comput Assist Tomogr. 1985;9:573–576. doi: 10.1097/00004728-198505000-00034. [DOI] [PubMed] [Google Scholar]
- 10.Strasser EJ, Davis RM. Extraperitoneal inguinal endometriosis. Am Surg. 1977;43:421–422. [PubMed] [Google Scholar]
- 11.Oner A, Karakucuk S, Serin S. Nasolacrimal endometriosis. A case report. Ophthalmic Res. 2006;38:313–314. doi: 10.1159/000095776. [DOI] [PubMed] [Google Scholar]
- 12.Ding DC, Hsu S. Scar endometriosis at the site of cesarean section. Taiwan J Obstet Gynecol. 2006;45:247–249. doi: 10.1016/S1028-4559(09)60234-5. [DOI] [PubMed] [Google Scholar]
- 13.Kasahara Y, Sonobe N, Tomiyoshi H, Imano M, Nakatani M, Urata T, Morishita A, Ueda S, Takemoto M, Yamada Y. Adenomyomatosis of the gallbladder: a clinical survey of 30 surgically treated patients. Nihon Geka Hokan. 1992;61:190–198. [PubMed] [Google Scholar]
- 14.Behera M, Vilos GA, Hollett-Caines J, Abu-Rafea B, Ahmad R. Laparoscopic findings, histopathologic evaluation, and clinical outcomes in women with chronic pelvic pain after hysterectomy and bilateral salpingo-oophorectomy. J Minim Invasive Gynecol. 2006;13:431–435. doi: 10.1016/j.jmig.2006.05.007. [DOI] [PubMed] [Google Scholar]
- 15.Michowitz M, Baratz M, Stavorovsky M. Endometriosis of the umbilicus. Dermatologica. 1983;167:326–330. doi: 10.1159/000249810. [DOI] [PubMed] [Google Scholar]
- 16.Michowitz M, Hammar B, Lazarovici I, Solowiejczky M. Endometriosis of the colon. Postgrad Med J. 1981;57:334–337. doi: 10.1136/pgmj.57.667.334. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Pillay SP, Hardie IR. Intestinal complications of endometriosis. Br J Surg. 1980;67:677–679. doi: 10.1002/bjs.1800670925. [DOI] [PubMed] [Google Scholar]
- 18.Samper ER, Slagle GW, Hand AM. Colonic endometriosis: its clinical spectrum. South Med J. 1984;77:912–914. doi: 10.1097/00007611-198407000-00029. [DOI] [PubMed] [Google Scholar]
- 19.Biscaldi E, Ferrero S, Fulcheri E, Ragni N, Remorgida V, Rollandi GA. Multislice CT enteroclysis in the diagnosis of bowel endometriosis. Eur Radiol. 2007;17:211–219. doi: 10.1007/s00330-006-0364-5. [DOI] [PubMed] [Google Scholar]
- 20.Del Frate C, Girometti R, Pittino M, Del Frate G, Bazzocchi M, Zuiani C. Deep retroperitoneal pelvic endometriosis: MR imaging appearance with laparoscopic correlation. Radiographics. 2006;26:1705–1718. doi: 10.1148/rg.266065048. [DOI] [PubMed] [Google Scholar]
- 21.Hensen JH, Van Breda Vriesman AC, Puylaert JB. Abdominal wall endometriosis: clinical presentation and imaging features with emphasis on sonography. AJR Am J Roentgenol. 2006;186:616–620. doi: 10.2214/AJR.04.1619. [DOI] [PubMed] [Google Scholar]
- 22.Marinis A, Vassiliou J, Kannas D, Theodosopoulos TK, Kondi-Pafiti A, Kairi E, Smyrniotis V. Endometriosis mimicking soft tissue tumors: diagnosis and treatment. Eur J Gynaecol Oncol. 2006;27:168–170. [PubMed] [Google Scholar]
- 23.Cavaliere D, Schirru A, Parodi A, Caristo I, Panaro F, Jarzembowski TM, Cavaliere P. Successful laparoscopic treatment of ileocecal-appendicular endometriosis. J Laparoendosc Adv Surg Tech A. 2004;14:395–398. doi: 10.1089/lap.2004.14.395. [DOI] [PubMed] [Google Scholar]
- 24.Byrne H, Ball E, Davis C. The role of magnetic resonance imaging in minimal access surgery. Curr Opin Obstet Gynecol. 2006;18:369–373. doi: 10.1097/01.gco.0000233928.19522.f0. [DOI] [PubMed] [Google Scholar]
- 25.Regadas SM, Regadas FS, Rodrigues LV, Silva FR, Lima DM, Regadas-Filho FS. Importance of the tridimensional ultrasound in the anorectal evaluation. Arq Gastroenterol. 2005;42:226–232. doi: 10.1590/s0004-28032005000400007. [DOI] [PubMed] [Google Scholar]
- 26.Robert Y, Launay S, Mestdagh P, Moisan S, Boyer C, Rocourt N, Cosson M. MRI in gynecology. J Gynecol Obstet Biol Reprod (Paris) 2002;31:417–439. [PubMed] [Google Scholar]
- 27.Farinon AM, Vadora E. Endometriosis of the colon and rectum: an indication for peroperative coloscopy. Endoscopy. 1980;12:136–139. doi: 10.1055/s-2007-1021730. [DOI] [PubMed] [Google Scholar]
- 28.Teunen A, Ooms EC, Tytgat GN. Endometriosis of the small and large bowel. Study of 18 patients and survey of the literature. Neth J Med. 1982;25:142–150. [PubMed] [Google Scholar]
- 29.Keckstein J, Ulrich U, Kandolf O, Wiesinger H, Wustlich M. Laparoscopic therapy of intestinal endometriosis and the ranking of drug treatment. Zentralbl Gynakol. 2003;125:259–266. doi: 10.1055/s-2003-42281. [DOI] [PubMed] [Google Scholar]
- 30.Régenet N, Métairie S, Cousin GM, Lehur PA. Colorectal endometriosis. Diagnosis and management. Ann Chir. 2001;126:734–742. doi: 10.1016/s0003-3944(01)00614-9. [DOI] [PubMed] [Google Scholar]
- 31.Verspyck E, Lefranc JP, Guyard B, Blondon J. Treatment of bowel endometriosis: a report of six cases of colorectal endometriosis and a survey of the literature. Eur J Obstet Gynecol Reprod Biol. 1997;71:81–84. doi: 10.1016/s0301-2115(96)02617-6. [DOI] [PubMed] [Google Scholar]
- 32.Scarselli G, Rizzello F, Cammilli F, Ginocchini L, Coccia ME. Diagnosis and treatment of endometriosis. A review. Minerva Ginecol. 2005;57:55–78. [PubMed] [Google Scholar]
- 33.Bulletti C, Flamigni C, Polli V, Giacomucci E, Albonetti A, Negrini V, Galassi A, Morselli-Labate AM. The efficacy of drugs in the management of endometriosis. J Am Assoc Gynecol Laparosc. 1996;3:495–501. doi: 10.1016/s1074-3804(05)80157-4. [DOI] [PubMed] [Google Scholar]
- 34.Nezhat C, Crowgey SR, Garrison CP. Surgical treatment of endometriosis via laser laparoscopy. Fertil Steril. 1986;45:778–783. doi: 10.1016/s0015-0282(16)49392-1. [DOI] [PubMed] [Google Scholar]
- 35.Sutton CJ, Jones KD. Laser laparoscopy for endometriosis and endometriotic cysts. Surg Endosc. 2002;16:1513–1517. doi: 10.1007/s00464-002-9060-y. [DOI] [PubMed] [Google Scholar]
- 36.Bailey HR, Ott MT, Hartendorp P. Aggressive surgical management for advanced colorectal endometriosis. Dis Colon Rectum. 1994;37:747–753. doi: 10.1007/BF02050136. [DOI] [PubMed] [Google Scholar]
- 37.Davis CJ, McMillan L. Pain in endometriosis: effectiveness of medical and surgical management. Curr Opin Obstet Gynecol. 2003;15:507–512. doi: 10.1097/00001703-200312000-00009. [DOI] [PubMed] [Google Scholar]
- 38.Davis GD, Wolgamott G, Moon J. Laparoscopically assisted vaginal hysterectomy as definitive therapy for stage III and IV endometriosis. J Reprod Med. 1993;38:577–581. [PubMed] [Google Scholar]
- 39.Urbach DR, Reedijk M, Richard CS, Lie KI, Ross TM. Bowel resection for intestinal endometriosis. Dis Colon Rectum. 1998;41:1158–1164. doi: 10.1007/BF02239439. [DOI] [PubMed] [Google Scholar]


