Abstract
AIM: To evaluate whether the prevalence of overweight and obese conditions is increased in gastro-esophageal reflux disease (GERD) patients (with 24-h pathological pH recordings) in comparison to general population.
METHODS: A total of 196 consecutive patients (103 females, age range 18-83 years) with symptoms of gastro-esophageal reflux (GER) and 24-h pathological esophageal pH-metry. Body mass index (BMI) of the patients was calculated and its distribution (%) was compared with that of the Italian general population as assessed by National Bureau of Census (ISTAT). To evaluate the association of GERD with weight categories, the binomial test was employed. P < 0.05 was considered statistically significant.
RESULTS: In males, overweightedness (BMI 25-25.9) was present in 43% of GERD patients vs 41.8% of Italian population (IP) (ns), obesity (BMI ≥ 30) in 10.9% vs 9.1% (ns). In females overweight was present in 34.9% of GERD patients vs 25.7% of IP (P < 0.01), obesity in 13.6% of GERD patients vs 9.1% of IP (P < 0.01). No statistically significant differences were noted in different age classes.
CONCLUSION: In comparison to the Italian general population, the prevalence of overweightedness and obesity is increased in female but not in male patients with ascertained gastro-esophageal reflux disease.
Keywords: Gastro-esophageal reflux, Obesity, Overweight, 24-h pH-metry, Body mass index
INTRODUCTION
Increased body weight has often been considered one of the most important risk factors for gastro-esophageal reflux disease (GERD). A recent meta-analysis concluded that overweightedness and obesity are the risk factor for GERD[1]. However, only three of the nine examined studies[2-10] showed the relationship between obesity and GERD symptoms[2].
Other studies have been performed only on patients with an exceedingly high body mass index (BMI), or even on patients requiring surgical[11-15] or intragastric balloon[16] treatment with no comparison with a normal BMI population.
Only two studies assessed the gastro-esophageal reflux (GER) by means of 24-h pH-metry but made no comparison with a reference population. Of these two studies, one was performed only on obese patients requiring intragastric balloon treatment[16], the other was performed on 70 patients, 79% of whom had abnormal BMI, indicating a biased patient selection[17].
Attempts to evaluate an improvement in gastro-esophageal reflux, or related symptoms following weight loss, in overweight and obese patients, have not led to a better understanding of the relationship between these two conditions since the data obtained are controversial[16,18,19].
MATERIALS AND METHODS
A total of 196 patients (103 females, age range 18-83 years; 93 males, age range 24-74 years) referred to our GI unit for GERD symptoms (including typical and atypical symptoms), were included in this study.
In all 196 patients, the presence of pathological gastro-esophageal reflux, according to DeMeester score, was established after a 24 h pH-metry assessment [Ingold 440 M3 glass electrode, Genesi2 RAM 8Kb LEM Electronics recorder, Casalecchio di Reno (BO), Italy]. Weight and height were measured in each patient, and their BMI was calculated [weight (kg)/ height (m2)].
Patients were then assigned to one of the four categories, according to their BMI, following the 1995 World Health Organization criteria, in which distinction between males and females is no longer considered: BMI < 18.5: underweight, BMI = 18.5-24.9: normal, BMI = 25-29.9: overweight, BMI > 30: obesity. The distribution (%) of the 196 GERD patients was compared with that of the Italian general population used, for this purpose, the data obtained in a National Bureau of Census (ISTAT) survey[20].
To evaluate the association of GERD with weight categories, we employed the binomial test, to calculate the probabilities of the estimated proportion of GERD patients in the overweight Italian population. The expected proportion of overweight individuals, in the population, was obtained from the above-mentioned ISTAT survey, based on approximately 50 000 people. This test was also performed stratifying the data according to sex and age-class. P < 0.05 was considered statistically significant. The association between smoking habit and presence of GERD was evaluated using the χ2 test.
Informed consent was obtained from patients at beginning of the study.
RESULTS
Of the patients presenting with pathological gastro-esophageal reflux, 45.9% had a normal BMI which was lower than that in the general population (53.8%) while 38.8% and 12.2% overweight and obese GERD patients had a normal BMI (exceeding 33.4% and 9.1%, respectively, in the general population) (Figure 1A).
Figure 1.
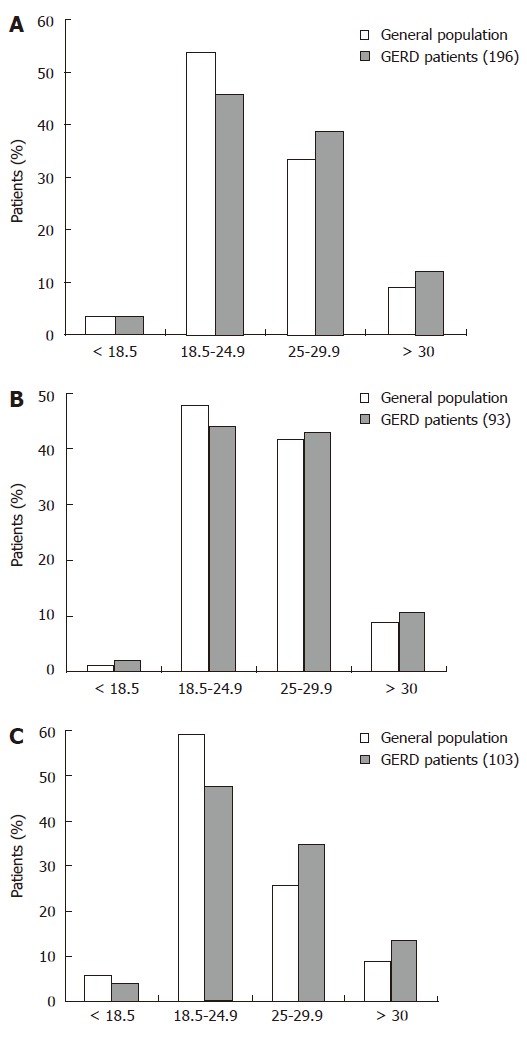
Distribution of BMI in general GERD patients (A), in male GERD patients (B), and in female GERD patients (C) after 24h esophageal pH-metry.
If the data on sex were considered, although the greater prevalence of BMI was still present in male GERD patients, the difference in the general population was less evident (overweight: 43% vs 41.8; obese: 10.8% vs 9.1%) (Figure 1B).
Conversely, the prevalence of overweightedness and obesity in female GERD patients was considerably greater than that in the general population (overweight: 34.9% vs 25.7% P < 0.01; obese: 13.6% vs 9.1% P < 0.01) (Figure 1C).
If the overweight and obese female patients were considered together, the total percentage reached 48.5% vs 35% in the general female population (P = 0.005).
No statistically significant differences were found in the analysis comparing different age classes. Likewise, statistical analysis failed to show any relationship between smoking habit and gastro-esophageal reflux in our patient population.
DISCUSSION
The most relevant finding of this study is that the prevalence of overweightedness and obesity was increased in female, but not in male Italian patients with ascertained gastro-esophageal reflux disease. Previous population-based studies considered GERD patients as those referring heartburn and acid regurgitation only[1-5] and did not assess any objective pH-metric evidence of GER.
By using typical GER symptoms as entry criteria, these studies excluded subjects with atypical GER symptoms and pathological GER and, on the other hand, included subjects with functional heartburn and no GER. It is estimated that about 10% of patients complaining of heartburn have functional heartburn, namely heartburn in endoscopy-negative, pH-metry negative patients not responding to proton pump inhibitors[21]. The prevalence of functional heartburn in patients recruited from our center is 16.5%[22]. It is also likely that the prevalence of functional heartburn is increased in obese subjects since elevated psychosomatic score is associated with reflux symptoms[10]. Moreover, some authors have advanced the hypothesis that esophageal mucosa is more sensitive in patients with functional heartburn and obese patients[23].
These limitations were not encountered in the present study which assessed BMI in patients in whom pathological gastro-esophageal reflux was confirmed by 24-h pH-metry according to DeMeester score, independently of typical or atypical GER symptoms.
Almost 45% of the Italian population have an increased BMI. Although the percentage of overweight subjects is steady, if compared with data from the ISTAT survey in 1994, the number of obese subjects has increased by 25% in the last 8 years. Elevated BMI, when accompanied with a greater intra-abdominal adipose mass, like other pathological conditions (constipation, cough and dysuria), may increase the abdominal-thoracic gradient favoring gastro-esophageal reflux episodes.
When the relationship between overweightedness or obesity and gastro-esophageal reflux is considered, it should be borne in mind that the eating habits of subjects with increased BMI values are often different from those of normal individuals, in terms of quality (particularly as lipids are concerned) and quantity of the nutrient intake. It is known that fatty foods produce a prolonged inhibitory effect on the lower esophageal sphincter (LES), particularly following intra-duodenal lipid perfusion[24]. This inhibitory effect would appear due to a cholecystokinin-mediated action on LES[25]. An epidemiological study revealed that overweightedness, but not excess fatty food intake, increases the risk of hospitalisation for GERD[26]. Gastric distension following a copious meal produces a transient increase in LES relaxation which is directly correlated to the distension volume[27] and could thus be another important factor favouring gastro-esophageal reflux. Variables such as eating habits and lifestyle were not considered in this study. The analysis of smoking failed to show any significant difference between the smoker and non-smoker groups.
Albeit, the role of LES pressure in obese patients with GERD is still controversial, and recent data[28] show that gastro-esophageal pressure gradient but not LES pressure, plays a relevant pathogenetic role in GERD patients with elevated BMI.
All the above mechanisms secondary to overweightedness and obesity would equally affect both genders and cannot explain the association between GER and overweight and obesity in females only.
The role of sex in GERD has not been clearly defined since available data from the literature are not homogeneous. In most epidemiological studies, the prevalence of GERD is greater in males than in females among symptomatic patients[29-31]. Some studies assessed the prevalence of sex primarily upon endoscopic esophagitis disregarding NERD patients, and found that low grade esophagitis is more frequent in females and high grade esophagitis in male patients[32,33]. Moreover, one study showed that longer GERD duration is correlated with the male sex[34]. It is widely known that Barrett’s esophagus is far more frequent in males[35-37].
The present study seems to indicate an association between BMI increase and gastro-esophageal reflux in female patients. Other authors have observed analogous results when studying the prevalence of male or female sex in overweight or obese patients with GERD. In fact, an association between obesity and GERD in females has been reported in some studies in which the authors are of the opinion that higher oestrogen concentration may cause more frequent transient lower esophageal sphincter relaxations[9,38].
Since high levels of circulating free oestrogens occur in obese and overweight females due to decreased concentration of oestrogen binding globulin and a concomitant increased production of oestrone from the fatty tissue, the hormonal effect can be indicated as a possible cause of GER. Although differences in gender fat distribution have not been considered, no data suggest a major risk of GER in males and a cardiovascular or metabolic risk of obesity in females. In addition, in this study the analysis of BMI and GER according to different age classes, failed to identify any significant difference, indicating that female postmenopausal distribution of visceral fat, similar to male one[39], has the same but not relevant effect on GER of the premenopausal fat distribution.
However, it an be hypothesized that the hormonal effect of increased adipose tissue increases the GER risk in overweight and obese females and makes it comparable to the GER risk in males.
In conclusion, findings of the present study suggest that overweightedness and obesity are related with an increased risk of gastro-esophageal reflux in females.
Footnotes
S- Editor Liu Y L- Editor Wang XL E- Editor Liu Y
References
- 1.Hampel H, Abraham NS, El-Serag HB. Meta-analysis: obesity and the risk for gastroesophageal reflux disease and its complications. Ann Intern Med. 2005;143:199–211. doi: 10.7326/0003-4819-143-3-200508020-00006. [DOI] [PubMed] [Google Scholar]
- 2.Andersen LI, Jensen G. Risk factors for benign oesophageal disease in a random population sample. J Intern Med. 1991;230:5–10. doi: 10.1111/j.1365-2796.1991.tb00399.x. [DOI] [PubMed] [Google Scholar]
- 3.Locke GR, Talley NJ, Fett SL, Zinsmeister AR, Melton LJ. Risk factors associated with symptoms of gastroesophageal reflux. Am J Med. 1999;106:642–649. doi: 10.1016/s0002-9343(99)00121-7. [DOI] [PubMed] [Google Scholar]
- 4.Oliveria SA, Christos PJ, Talley NJ, Dannenberg AJ. Heartburn risk factors, knowledge, and prevention strategies: a population-based survey of individuals with heartburn. Arch Intern Med. 1999;159:1592–1598. doi: 10.1001/archinte.159.14.1592. [DOI] [PubMed] [Google Scholar]
- 5.Stanghellini V. Three-month prevalence rates of gastrointestinal symptoms and the influence of demographic factors: results from the Domestic/International Gastroenterology Surveillance Study (DIGEST) Scand J Gastroenterol Suppl. 1999;231:20–28. doi: 10.1080/003655299750025237. [DOI] [PubMed] [Google Scholar]
- 6.Lagergren J, Bergström R, Nyrén O. No relation between body mass and gastro-oesophageal reflux symptoms in a Swedish population based study. Gut. 2000;47:26–29. doi: 10.1136/gut.47.1.26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Wu AH, Tseng CC, Bernstein L. Hiatal hernia, reflux symptoms, body size, and risk of esophageal and gastric adenocarcinoma. Cancer. 2003;98:940–948. doi: 10.1002/cncr.11568. [DOI] [PubMed] [Google Scholar]
- 8.Murray L, Johnston B, Lane A, Harvey I, Donovan J, Nair P, Harvey R. Relationship between body mass and gastro-oesophageal reflux symptoms: The Bristol Helicobacter Project. Int J Epidemiol. 2003;32:645–650. doi: 10.1093/ije/dyg108. [DOI] [PubMed] [Google Scholar]
- 9.Nilsson M, Johnsen R, Ye W, Hveem K, Lagergren J. Obesity and estrogen as risk factors for gastroesophageal reflux symptoms. JAMA. 2003;290:66–72. doi: 10.1001/jama.290.1.66. [DOI] [PubMed] [Google Scholar]
- 10.Diaz-Rubio M, Moreno-Elola-Olaso C, Rey E, Locke GR, Rodriguez-Artalejo F. Symptoms of gastro-oesophageal reflux: prevalence, severity, duration and associated factors in a Spanish population. Aliment Pharmacol Ther. 2004;19:95–105. doi: 10.1046/j.1365-2036.2003.01769.x. [DOI] [PubMed] [Google Scholar]
- 11.Csendes A, Burdiles P, Rojas J, Burgos A, Henríquez A. [Pathological gastroesophageal reflux in patients with severe, morbid and hyper obesity] Rev Med Chil. 2001;129:1038–1043. [PubMed] [Google Scholar]
- 12.Fisher BL, Pennathur A, Mutnick JL, Little AG. Obesity correlates with gastroesophageal reflux. Dig Dis Sci. 1999;44:2290–2294. doi: 10.1023/a:1026617106755. [DOI] [PubMed] [Google Scholar]
- 13.Mathus-Vliegen LM, Tytgat GN. Twenty-four-hour pH measurements in morbid obesity: effects of massive overweight, weight loss and gastric distension. Eur J Gastroenterol Hepatol. 1996;8:635–640. [PubMed] [Google Scholar]
- 14.Rigaud D, Merrouche M, Le Moël G, Vatier J, Paycha F, Cadiot G, Naoui N, Mignon M. [Factors of gastroesophageal acid reflux in severe obesity] Gastroenterol Clin Biol. 1995;19:818–825. [PubMed] [Google Scholar]
- 15.Lundell L, Ruth M, Sandberg N, Bove-Nielsen M. Does massive obesity promote abnormal gastroesophageal reflux? Dig Dis Sci. 1995;40:1632–1635. doi: 10.1007/BF02212682. [DOI] [PubMed] [Google Scholar]
- 16.Mathus-Vliegen EM, Tygat GN. Gastro-oesophageal reflux in obese subjects: influence of overweight, weight loss and chronic gastric balloon distension. Scand J Gastroenterol. 2002;37:1246–1252. doi: 10.1080/003655202761020498. [DOI] [PubMed] [Google Scholar]
- 17.Wajed SA, Streets CG, Bremner CG, DeMeester TR. Elevated body mass disrupts the barrier to gastroesophageal reflux; discussion 1018-1019. Arch Surg. 2001;136:1014–1018. doi: 10.1001/archsurg.136.9.1014. [DOI] [PubMed] [Google Scholar]
- 18.Fraser-Moodie CA, Norton B, Gornall C, Magnago S, Weale AR, Holmes GK. Weight loss has an independent beneficial effect on symptoms of gastro-oesophageal reflux in patients who are overweight. Scand J Gastroenterol. 1999;34:337–340. doi: 10.1080/003655299750026326. [DOI] [PubMed] [Google Scholar]
- 19.Kjellin A, Ramel S, Rössner S, Thor K. Gastroesophageal reflux in obese patients is not reduced by weight reduction. Scand J Gastroenterol. 1996;31:1047–1051. doi: 10.3109/00365529609036885. [DOI] [PubMed] [Google Scholar]
- 20.Indagine Multiscopo "condizioni di salute e ricorso ai servizi sanitari". April 2002. Available from: http//www.istat.it/dati/catalogo/20020313_01/
- 21.Galmiche JP, Clouse RE, Bálint A, Cook IJ, Kahrilas PJ, Paterson WG, Smout AJ. Functional esophageal disorders. Gastroenterology. 2006;130:1459–1465. doi: 10.1053/j.gastro.2005.08.060. [DOI] [PubMed] [Google Scholar]
- 22.Alghisi F, Piretta L. Corazziari E. Malattia da reflusso gastro-esofageo non erosiva (NERD) e pirosi funzionale. Neurogastroenterologia. 2002;8:42–46. [Google Scholar]
- 23.Barak N, Ehrenpreis ED, Harrison JR, Sitrin MD. Gastro-oesophageal reflux disease in obesity: pathophysiological and therapeutic considerations. Obes Rev. 2002;3:9–15. doi: 10.1046/j.1467-789x.2002.00049.x. [DOI] [PubMed] [Google Scholar]
- 24.Holloway RH, Lyrenas E, Ireland A, Dent J. Effect of intraduodenal fat on lower oesophageal sphincter function and gastro-oesophageal reflux. Gut. 1997;40:449–453. doi: 10.1136/gut.40.4.449. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Sturdevant RA, Kun T. Interaction of pentagastrin and the octapeptide of cholecystokinin on the human lower oesophageal sphincter. Gut. 1974;15:700–702. doi: 10.1136/gut.15.9.700. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Ruhl CE, Everhart JE. Overweight, but not high dietary fat intake, increases risk of gastroesophageal reflux disease hospitalization: the NHANES I Epidemiologic Followup Study. First National Health and Nutrition Examination Survey. Ann Epidemiol. 1999;9:424–435. doi: 10.1016/s1047-2797(99)00020-4. [DOI] [PubMed] [Google Scholar]
- 27.Scheffer RC, Akkermans LM, Bais JE, Roelofs JM, Smout AJ, Gooszen HG. Elicitation of transient lower oesophageal sphincter relaxations in response to gastric distension and meal ingestion. Neurogastroenterol Motil. 2002;14:647–655. doi: 10.1046/j.1365-2982.2002.00366.x. [DOI] [PubMed] [Google Scholar]
- 28.Pandolfino JE, El-Serag HB, Zhang Q, Shah N, Ghosh SK, Kahrilas PJ. Obesity: a challenge to esophagogastric junction integrity. Gastroenterology. 2006;130:639–649. doi: 10.1053/j.gastro.2005.12.016. [DOI] [PubMed] [Google Scholar]
- 29.Schindlbeck NE, Klauser AG, Berghammer G, Londong W, Müller-Lissner SA. Three year follow up of patients with gastrooesophageal reflux disease. Gut. 1992;33:1016–1019. doi: 10.1136/gut.33.8.1016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Voutilainen M, Sipponen P, Mecklin JP, Juhola M, Färkkilä M. Gastroesophageal reflux disease: prevalence, clinical, endoscopic and histopathological findings in 1,128 consecutive patients referred for endoscopy due to dyspeptic and reflux symptoms. Digestion. 2000;61:6–13. doi: 10.1159/000007730. [DOI] [PubMed] [Google Scholar]
- 31.Mäntynen T, Färkkilä M, Kunnamo I, Mecklin JP, Juhola M, Voutilainen M. The impact of upper GI endoscopy referral volume on the diagnosis of gastroesophageal reflux disease and its complications: a 1-year cross-sectional study in a referral area with 260,000 inhabitants. Am J Gastroenterol. 2002;97:2524–2529. doi: 10.1111/j.1572-0241.2002.06034.x. [DOI] [PubMed] [Google Scholar]
- 32.Csendes A, Maluenda F, Braghetto I, Csendes P, Henriquez A, Quesada MS. Location of the lower oesophageal sphincter and the squamous columnar mucosal junction in 109 healthy controls and 778 patients with different degrees of endoscopic oesophagitis. Gut. 1993;34:21–27. doi: 10.1136/gut.34.1.21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Garrido Serrano A, Guerrero Igea FJ, Lepe Jiménez JA, Perianes Hernández C. Clinical features and endoscopic progression of gastroesophageal reflux disease. Rev Esp Enferm Dig. 2003;95:712–716, 712-716. [PubMed] [Google Scholar]
- 34.Kulig M, Nocon M, Vieth M, Leodolter A, Jaspersen D, Labenz J, Meyer-Sabellek W, Stolte M, Lind T, Malfertheiner P, et al. Risk factors of gastroesophageal reflux disease: methodology and first epidemiological results of the ProGERD study. J Clin Epidemiol. 2004;57:580–589. doi: 10.1016/j.jclinepi.2003.10.010. [DOI] [PubMed] [Google Scholar]
- 35.Falk GW, Thota PN, Richter JE, Connor JT, Wachsberger DM. Barrett's esophagus in women: demographic features and progression to high-grade dysplasia and cancer. Clin Gastroenterol Hepatol. 2005;3:1089–1094. doi: 10.1016/s1542-3565(05)00606-3. [DOI] [PubMed] [Google Scholar]
- 36.Cook MB, Wild CP, Forman D. A systematic review and meta-analysis of the sex ratio for Barrett's esophagus, erosive reflux disease, and nonerosive reflux disease. Am J Epidemiol. 2005;162:1050–1061. doi: 10.1093/aje/kwi325. [DOI] [PubMed] [Google Scholar]
- 37.Ford AC, Forman D, Reynolds PD, Cooper BT, Moayyedi P. Ethnicity, gender, and socioeconomic status as risk factors for esophagitis and Barrett's esophagus. Am J Epidemiol. 2005;162:454–460. doi: 10.1093/aje/kwi218. [DOI] [PubMed] [Google Scholar]
- 38.Nilsson M, Lundegårdh G, Carling L, Ye W, Lagergren J. Body mass and reflux oesophagitis: an oestrogen-dependent association? Scand J Gastroenterol. 2002;37:626–630. doi: 10.1080/00365520212502. [DOI] [PubMed] [Google Scholar]
- 39.Kotani K, Tokunaga K, Fujioka S, Kobatake T, Keno Y, Yoshida S, Shimomura I, Tarui S, Matsuzawa Y. Sexual dimorphism of age-related changes in whole-body fat distribution in the obese. Int J Obes Relat Metab Disord. 1994;18:207–212. [PubMed] [Google Scholar]


