Abstract
An 83-year-old woman with no significant medical history was transferred to our tertiary hospital after being hit by a car and presenting with haemorrhagic shock. Immediate fluid resuscitation was performed; physical, chest/pelvic X-ray and echographic examinations did not detect any major sources of bleeding. However, a contrast-enhanced CT scan revealed multiple regions of significant contrast extravasation in an extensive part of the subcutaneous tissue of the patient's lower back, which is an unusual source of bleeding. Transcatheter arterial embolisation of the lumbar and internal iliac arteries and their branches was carried out. In addition, haemostatic resuscitation was performed for damage control resuscitation, which successfully resolved the patient's haemorrhagic shock.
Background
Lumbar artery injuries, which are not a major source of internal bleeding, can cause significant retroperitoneal haemorrhaging and are associated with a high mortality rate.1 2 As chest/pelvic X-ray and echographic examinations, and focused assessment with sonography for trauma (FAST) cannot exclude certain types of internal bleeding, such as retroperitoneal or non-cavitary haemorrhaging,3 clinicians should take such injuries into consideration in patients with haemorrhagic shock of unknown origin. We describe a case in which massive subcutaneous haematomas of the lower back, which are an unusual source of bleeding, occurred after blunt trauma, and were successfully treated with haemostatic resuscitation, and transcatheter arterial embolisation of the lumbar and internal iliac arteries and their branches.
Case presentation
An 83-year-old woman with no significant medical history was transferred to our tertiary hospital after being hit by a car while walking on the road. On arrival, she was pale and significantly distressed, and exhibited the following signs of shock: Glasgow Coma Scale 12 (E4V3M5), respiratory rate 25 breaths/min, heart rate 99 bpm and blood pressure 42/28 mm Hg. Fluid resuscitation was started immediately and tracheal intubation was performed due to suspected severe haemorrhagic shock. Simultaneously, a massive transfusion protocol was initiated, which enabled the infusion of red blood cells and fresh frozen plasma 30 min after the patient’s arrival. A physical examination did not reveal any obvious head, neck, chest, abdomen or pelvic traumas other than an obvious deformity of her right lower extremity associated with an open wound. Six hours after her arrival, following her recovery from haemorrhagic shock, the patient's posterior region was assessed, which resulted in the detection of multiple subcutaneous haematomas covering an extensive region of her lower back (figure 1). Chest X-ray and ultrasound examinations excluded a cavitary haemorrhage and intrathoracic, intra-abdominal or pericardial effusion, and a pelvic X-ray showed that the patient’s fractures were stable. As the patient exhibited a transient response to fluid resuscitation, she had been moved to the CT suite 40 min after her arrival to identify any major sources of bleeding. A contrast-enhanced whole-body CT scan detected multiple regions of subcutaneous contrast extravasation in her lower back (figure 2A, B). In addition, a Chance fracture of the first lumbar vertebra, a left-sided psoas haematoma associated with multiple fractures of the transverse processes of her lumbar vertebrae (figure 3A, B), and open fractures of her left lower extremities, were also identified. The pelvic fractures proved to be those of pubic and ischium bone on the left side, and third and fourth sacral bone fractures with stable pelvic ring, which were rated as 61-A by Orthopaedic Trauma Association classification (figure 4). Large retroperitoneal haematoma associated with pelvic fracture was absent on initial CT scan. The subcutaneous soft tissue of the patient’s lower back was determined to be the major source of her bleeding, and concomitant retroperitoneal haemorrhaging associated with the fractures of the transverse processes of her lumbar vertebrae was also considered to have contributed to her bleeding.
Figure 1.

An image of the patient’s posterior region taken 6 h after arrival. The patient’s shock had been resolved by the time this image was taken. Significant subcutaneous haematomas were noted in the lower back (triangle arrow) together with bruising in the iliac crest area.
Figure 2.
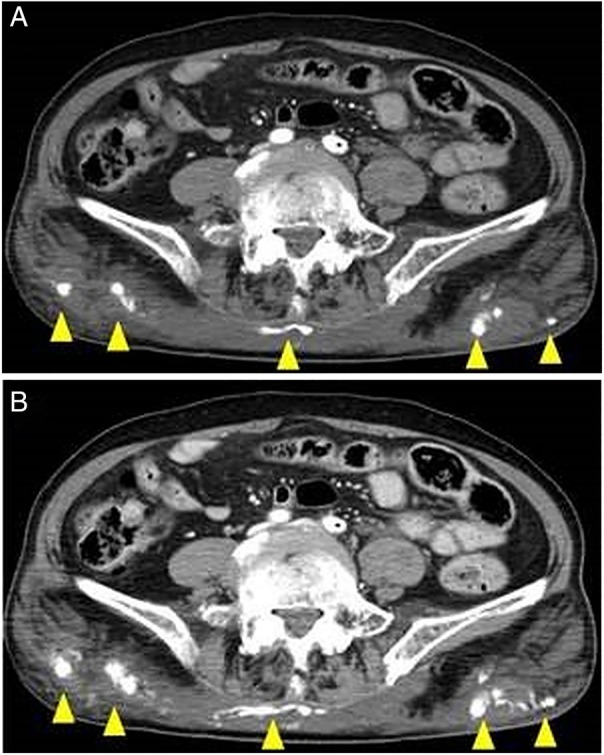
A contrast-enhanced CT scan revealing multiple regions of contrast extravasation in the subcutaneous tissue of the patient’s lower back ((A) early phase and (B) delayed phase).
Figure 3.
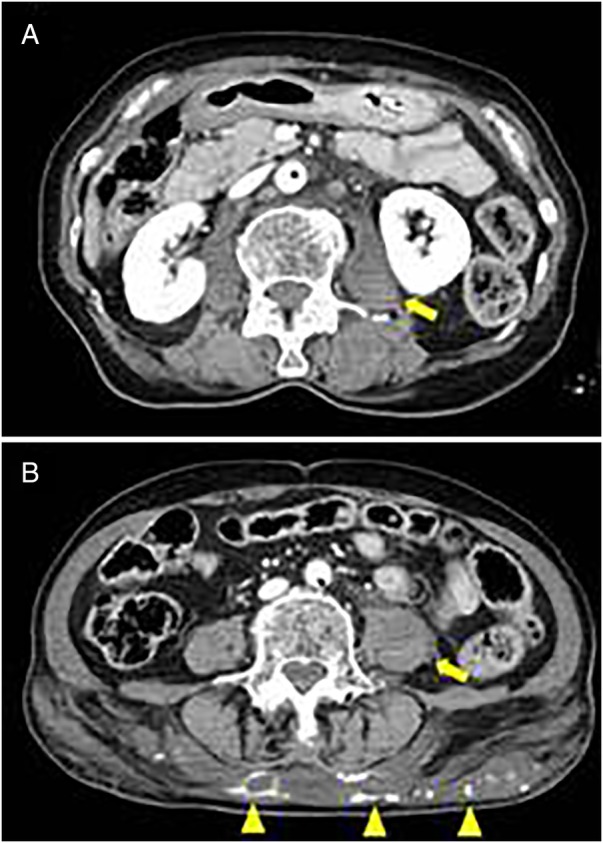
Retroperitoneal haematoma associated with fractures of the transverse processes of the lumbar, which was not significant (yellow arrow). Multiple contrast extravasations and haematoma were seen in the subcutaneous region of lower lumbar level (yellow triangle arrow) ((A) at the level of the 2nd lumbar and (B) at the level of the 4th lumbar).
Figure 4.
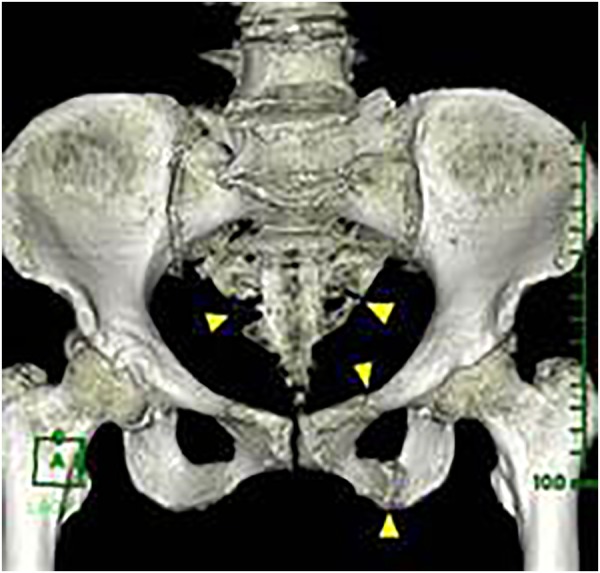
Stable-type pelvic fracture, which was classified as 61-A by Orthopaedic Trauma Association classification.
Investigations
The initial arterial blood gas analysis revealed an elevated serum lactate concentration together with the following findings: pH 7.380, PaCO2 38.3 mm Hg, PaO2 501.1 mm Hg, haemoglobin level 10.2 g/L, base excess −2.1 mmol/L and lactate 4.1 mmol/L on 10 L/min of oxygen directly prior to intubation.
The patient’s laboratory data on arrival were indicative of acute traumatic coagulopathy: platelet count 13.8×104/μL, international normalised ratio 1.22, fibrinogen 98 mg/dL and D-dimer 100.8 μg/mL.
Treatment
The patient was taken to the angiography suite soon after undergoing a CT scan so that the bleeding could be stopped. Aortography detected active contrast extravasation at multiple sites located close to the bilateral lumbar and internal iliac arteries (figure 5). The affected vessels included the first, second and fourth lumbar arteries on the right side, and the bilateral third lumbar artery and the bilateral superior gluteal arteries (left side dominant). Ultimately, to complete the haemostatic procedure, the embolisation of these affected lumbar arteries and the bilateral internal iliac arteries was successfully performed using an absorbable gelatine sponge. The patient required 18 units of red blood cell concentrate, 20 units of fresh frozen plasma and 20 units of platelets within 12 h of her arrival for haemostatic resuscitation, which successfully resolved her haemorrhagic shock. On the third day, a posterior spinal fusion procedure was performed for the Chance fracture of the first lumbar vertebra. The patient was successfully extubated on the 16th day. On the 23rd day, the open fracture of her right lower extremities was subjected to internal fixation.
Figure 5.
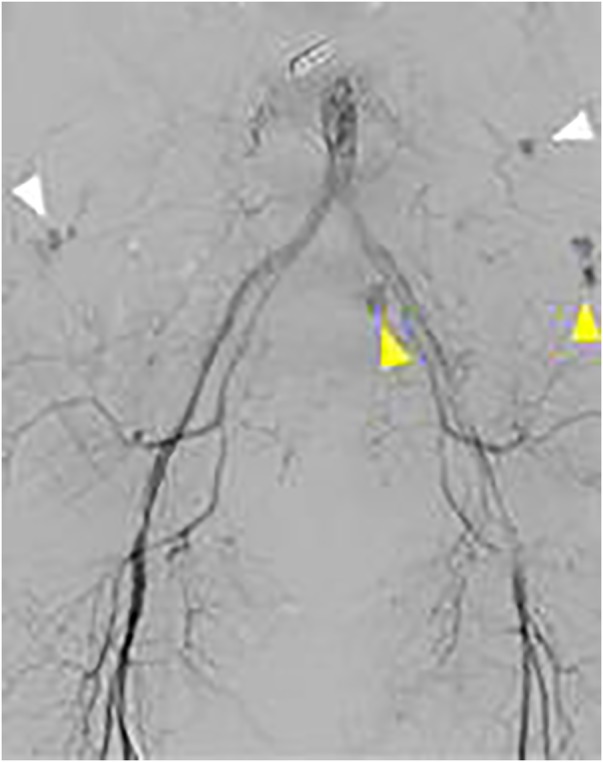
An aortographic image showing multiple regions of contrast extravasation. The lumbar and internal iliac arteries and their branches were located in the affected region (white triangle arrows describe the bilateral lower lumbar arteries, and yellow ones describe the superior gluteal artery on the left side).
Outcome and follow-up
The patient was transferred to another hospital on the 31st hospital day. At 90 days after suffering the injury, the patient was undergoing rehabilitation.
Discussion
Exsanguination is a leading cause of death in trauma patients.4 Internal bleeding after blunt trauma most commonly occurs in the intra-thoracic, intra-abdominal and retroperitoneal spaces (bleeding in the retroperitoneal space is often associated with pelvic fractures).5 Although chest/pelvic X-ray and focused assessment with sonography for trauma (FAST) examinations can identify such internal bleeding, other types of internal bleeding, for example, retroperitoneal haemorrhaging from other sources or non-cavitary haemorrhaging, cannot be detected by these techniques.2 3 Pedowitz and Shackford3 reported that about half of trauma patients who present with shock are subsequently found to be suffering from non-cavitary haemorrhaging, which is associated with long bone fractures or skin lacerations. Therefore, clinicians should recognise that less common types of internal bleeding, such as non-cavitary haemorrhaging, can also cause significant bleeding.
While pelvic fractures are a major cause of massive retroperitoneal haematomas,6 lumbar artery injuries are a rare source of post-blunt trauma bleeding.7 Lumbar artery injuries are commonly associated with transverse process fractures of the lumbar vertebrae. Our patient had stable pelvic fractures and retroperitoneal haematomas associated with transverse process fractures of the lumbar vertebrae, which are not commonly associated with major bleeding. However, she developed massive subcutaneous haematomas covering an extensive region of her lower back, which was served by the bilateral lumbar and internal iliac arteries and their branches. These kinds of injuries are difficult to identify during physical, pelvic X-ray or echographic examinations. Thus, contrast-enhanced CT scans are essential for detecting the source of bleeding in such cases. The mechanism responsible for these types of injuries is considered to involve sclerotic changes making the arteries vulnerable to injury during high-energy impacts, resulting in significant subcutaneous haematomas developing in elderly patients.
As for treatment, transcatheter arterial embolisation of the affected vessels is effective at controlling retroperitoneal and subcutaneous haemorrhaging.1 7–9 Open surgery is not recommended because it often fails to identify the source of the bleeding and can cause further bleeding due to decompression.7 In addition to controlling any haemorrhaging, haemostatic resuscitation based on the concept of damage control resuscitation is also crucial to resolving acute traumatic coagulopathy.10
We described a case in which massive subcutaneous haematomas developed in an extensive region of the lower back. The haematomas were associated with injuries to the lumbar and internal iliac arteries and their branches, which are unusual sources of bleeding after blunt trauma. The ‘historical’ or ‘traditional’ initial screening of a bleeding trauma patient (chest X-ray, pelvic X-ray and FAST) has many limitations and can often fail to determine the origin of unexteriorised bleeding. In our case, a contrast-enhanced CT scan identified the source of bleeding, and the patient was successfully treated with transcatheter arterial embolisation and haemostatic resuscitation.
Learning points.
Subcutaneous haemorrhaging in an extensive area of the lower back associated with injuries to the lumbar and internal iliac arteries and their branches can cause major bleeding in elderly patients who suffer blunt traumas.
As the ‘historical’ or ‘traditional’ initial screening of chest/pelvic X-ray and FAST cannot detect such injuries, for example, non-cavitary haemorrhaging, contrast-enhanced CT scans are necessary for identifying the source of bleeding.
Transcatheter arterial embolisation and haemostatic resuscitation are effective at resolving shock.
Footnotes
Contributors: All the authors were involved in the management and care of the patient. TY and KS prepared the manuscript.
Competing interests: None declared.
Patient consent: Obtained.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Sofocleous CT, Hinrichs CR, Hubbi B et al. Embolization of isolated lumbar artery injuries in trauma patients. Cardiovasc Intervent Radiol 2005;28:730–5. 10.1007/s00270-003-0117-7 [DOI] [PubMed] [Google Scholar]
- 2.Akpinar E, Peynircioqlu B, Turkbey B et al. Endovascular management of life-threatening retroperitoneal bleeding. ANZ J Surg 2008;78:683–7. 10.1111/j.1445-2197.2008.04148.x [DOI] [PubMed] [Google Scholar]
- 3.Pedowitz RA, Shackford SR. Non-cavitary haemorrhage producing shock in trauma patients: incidence and severity. J Trauma 1989;29:219–22. 10.1097/00005373-198902000-00012 [DOI] [PubMed] [Google Scholar]
- 4.Sauaia A, Moore FA, Moore EE et al. Epidemiology of trauma deaths: a reassessment. J Trauma 1995;38:185–93. 10.1097/00005373-199502000-00006 [DOI] [PubMed] [Google Scholar]
- 5.Lane PL, McLellan BA, Johns PD. Etiology of shock in blunt trauma. Can Med Assoc J 1985;133:199–201. [PMC free article] [PubMed] [Google Scholar]
- 6.Geeraerts T, Chhor V, Cheisson G et al. Clinical review: initial management of blunt pelvic trauma patients with haemodaynamic instability. Crit Care 2007;11:204 10.1186/cc5157 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Yuan KC, Hsu YP, Wong YC et al. Management of complicated lumbar artery injury after blunt trauma. Ann Emerg Med 2011;58:531–5. 10.1016/j.annemergmed.2011.07.002 [DOI] [PubMed] [Google Scholar]
- 8.Boufi M, Bordon S, Dona B et al. Unstable patients with retroperitoneal vascular trauma: an endovascular approach. Ann Vasc Surg 2011;25:352–8. 10.1016/j.avsg.2010.09.008 [DOI] [PubMed] [Google Scholar]
- 9.Hagiwara A, Matsuda T, Shimazaki S. Life-threatening subcutaneous haemorrhage following minor blunt trauma in an elderly patient taking ticlopidine and aspirin: a case report. Emerg Radiol 2005;12:47–9. 10.1007/s10140-005-0446-8 [DOI] [PubMed] [Google Scholar]
- 10.Jansen JO, Thomas R, Loudon MA et al. Damage control resuscitation for patients with major trauma. BMJ 2009;338:b1778 10.1136/bmj.b1778 [DOI] [PubMed] [Google Scholar]


